Nursing Care for the High Risk Newborn & Family

Nursing Care for the High Risk
Newborn & Family
High Risk Newborn
During pregnancy, screening for high is essential.
Dysmature-infant who is born before term or postterm, who is under or overweight for gestational age.
Assessment:
At birth for anomalies and gestational age (number of weeks in utero).
Monitors, 1:1nursing care, common sense.
Goals may not be full recovery.
Focus on conserving energy, temp,
Nursing Process
Minimize pain, parent teaching, support, and referrals.
Outcome Evaluation:
Long term follow up and care.
Patent airway, growth and development, temp, visits by parents, coping skills.
High Risk Newborn
Newborn Priorities in First Days of Life
Initiations and maintenance of respirations
Establishment of extrauterine circulation
Control of body temperature
Intake of adequate nourishment
Establishment of waste elimination
Prevention of infection
Establishment of an infant-parent relationship
Developmental care, balance physical and mental development.
High Risk Newborn
May require special equipment and/or care measures.
Difficulty may appear during intrapartum period, at birth or at initial APGAR.
Initiating and Maintaining Respirations:
Prognosis depends on how the first moments of life are managed.
Most deaths occur during the 1st 48 hours
Due to inability to establish or maintain adequate airway.
Cerebral hypoxia, residual neurologic dysfunction
High Risk Newborn
Most infants have some degree of respiratory acidosis.
Blood pH and bicarbonate buffer system may fail if not corrected quickly. (2 min)
May already have some degree of asphyxia due to cord compression, maternal anesthesia, placental previa or preterm separation of the placenta.
Resuscitation:
Factors – low birth wt., diabetes,
High Risk Newborn
Circulatory shunts particularly ductus arteriosus, fail to close
Infant uses available serum glucose quickly, may become hypoglycemic, compounds the problem.
Establish and maintain airway
Expanding the lungs
Initiating and maintaining effective ventilation.
If not sufficient the heart will fail. CPR
High Risk Newborn
Airway:
Suction with bulb syringe and rub back to see if skin stimulation initiates respirations.
Dry infant, may need warmed O2
Lay on back , head and shoulders elevated
Suction 10 seconds (vagus stimulation)
Laryngoscope, deep suctioning, endotracheal tube inserted, O2 100% @ 40 to
60 breaths per minute.
Primary apnea-several week gasps of air then stops breathing. Halted respirations.
High Risk Newborn
After 1 to 2 minutes of apnea the infant tries to initiate respirations with strong gasps. Can not maintain this – 4 to 5 minutes moves to secondary
apnea.
Can occur in utero.
Team-OB, Ped, neonatologist, anesthesiologist, NP
Laryngoscope size 0-1 for newborns.
Risk of hemorrhage.
High Risk Newborn
Lung Expansion:
Crying is proof that lungs have expanded.
Mask cover both nose and mouth.
Pressure needed to open lungs alveoli for 1st time is 40cm H2O then 15 to 20 cm.
Auscultate chest. Pulse ox.
If meconium do not stimulate. Wait for suction.
Watch that both sides are aerated.
High Risk Newborn
Drug Therapy:
Narcan- for respiratory depression due to Morphine. Inject into umbilical vessel or IM. 0.01 to 0.1 mg/kg body weight.
Ventilation Maintenance:
Monitor for next few hours.
Increasing respiratory rate is 1st sign.
Check for retractions, place under warmer and remove clothing from chest, elevate HOB 15 degrees, suction, O2, pulse Ox.
High Risk Newborn
Establishing Extrauterine Circulation:
Cardiac function is not so quickly restored.
If < 80 bpm do closed chest massage.
Depress sternum with 2 fingers 1 to 2 cm rate 100 / minute. Respirations
30/ minute.
Palpate femoral pulse
After not > 80/min in 30 sec. Spray in ET epinephrine 0.1 to 0.3 mL/kg.
Transport to NICU.
High Risk Newborn
Maintaining Fluid And Electrolyte Balance:
Hypoglycemia may result. Check glucose.
Dehydration-IV RL or D5%W, Na, K
Monitor closely the rate of fluid due to patent ductus arteriosus or heart failure.
Urine output < 2mL/kg/h or SG >1.015 to 1.020 (kidney or ADH secretion).
Hypotension
Hypovolemia
RL to increase blood volume.
High Risk Newborn
Regulating Temperature:
Neutral temperature environment. Less demand on infant and maintains
metabolic rate.
Give O2 to increase metabolic rate (become hypoxic)
Decreased PO2 level may open fetal right to left shunts again.
Surfactant
Risk of kernicterus (invasion of brain cells with unconjugated bilirubin).
High Risk Newborn
Radiant Heat Source:
Open beds with over head radiant heat source.
Probe is placed between umbilicus and xiphoid process of infant.(not on rib cage).
May also need a warming pad under infant.
Isolettes:
Incubator (portholes lose heat if opened for long intervals).
Check temperature frequently.
High Risk Newborn
When improved, weaning by setting temp 2 degree below infant’s temp. in 30
min check infants temp. if maintained reduce by another 2 degrees until room temp is reached.
Kangaroo Care:
Skin to skin contact to maintain body heat.
Diaper and hat on infant, cover both with a blanket, dim lights.
High Risk Newborn
Establishing Adequate Nutritional Intake
Establish respiratory rate and rule out NEC necrotizing enterocolitis.
IV fluids, gavage feedings.
Preterm breast fed if possible (express milk) can be used in gavage feeding.
Pacifier at feeding times if sucking reflex is present.
Establishing Waste Elimination
Document any voiding. Kidneys perfused.
Document any meconium or stool.
High Risk Newborn
Preventing Infection:
Infection increases metabolic demand.
Stresses immature immune system.
Can be prenatal, perinatal or postnatal.
Cytomegalovirus and toxoplasmosis viruses
Congenital anomalies
From vagina-group B strep septicemia, thrush from candida and herpes.
Postnatal is from health care personal.
High Risk Newborn
Establishing Parent Infant Bonding:
Visit NICU before birth, afterwards visit and bond.
Keep parents informed, give name and number of contact person.
See baby after death.
Developmental Needs:
Most high risk infants catch up growth occurs once stabilized from trauma.
Home care visits.
High Risk Newborn
Follow Up of High Risk Infants at Home:
Asses their level of knowledge.
Educate and refer to home care agency.
High Risk Infants and Child Abuse:
Parents become more protective.
Due to separation from the family, bonding was not complete.
Altered Gestational Age or Birth Weight
Assessed at birth and placed on growth chart.
Term infants-38 to 42 weeks pregnancy.
High Risk Newborn
Preterm infants-less than 37 weeks regardless of birth weight.
Postterm infants-after 43 weeks
AGA-appropriate for gestational age-between 10th to 90th percentile of weight.
SGA-small for gestational age-below 10th percentile of weight for their age.
LGA-large for gestational age-above 90th percentile of weight for their age.
Low birth weight-under 2500 g
Very low birth weight-less than 1500 g.
High Risk Newborn
Small for Gestational Age Infant:
IUGR-intrauterine growth restriction or retardation.
Failed to grow at expected rate in utero.
Cause:
Mother’s nutrition plays a major role
Adolescents
Placental anomaly
Systemic diseases – diabetes, hypertension
Smokers, narcotic use, infections
High Risk Newborn
Assessment:
Prenatal care; fundal height, sonogram, poor placental function,
Appearance:
Below average; weight, length, and head circumference. Overall wasted appearance. Small liver, poor skin turgor, wide sutures, dull hair, sunken abdomen, cord dry and stained yellow.
Lab Findings:
High Hct, RBC, and decreased glucose.
High Risk Newborn
Large for Gestational Age Infant:
Macrosomia
May appear healthy but exam reveals immature development.
Cause:
Over production of growth hormone in utero.
Mother with diabetes
Muitiparous women
Transposition of great vessels.
High Risk Newborn
Assessment:
Uterus unusually lg for date of pregnancy.
Sonogram
Nonstress test
Amniocentesis-lung maturity
Cesarean birth.
Appearance:
Immature reflexes, low score on gestational age exam.
Bruising, injury,extreme molding.
High Risk Newborn
Cardiovascular Dysfunction:
Cyanosis, polycythemia, hyperbilirubinemia
Hypoglycemia:
Uses up nutritional stores
High glucose levels if mother is diabetic and will increase for 24 hours, rebound.
Preterm Infant:
Before end of week 37of gestation
Birth weight < 2500g (5 lb 8 oz) at birth.
Need NICU
Preterm
Lack lung surfactant = RDS
Maturity determined by sole creases, skull firmness, ear cartilage, neurologic findings, mothers report of date of last period and sonogram.
Incidence:
7% whites, 14% African American.
Causes:
Nutrition
Testing by amniocentesis, ultrasound best.
Preterm
Assessment:
History – do not refer to smoking or working 12 hour shift contributed to preterm delivery.
Guilt may deter bonding. Support.
May not realize she is in labor.
May not feel well or have flu like symptoms.
Appearance:
Small and underdeveloped
Head lg 3 cm or more than chest, ruddy skin
Preterm
Noticeable veins, acrocyanosis.
Vernix-24 to 36 week covered, < 25 weeks none.
Lanugo extensive-back, forearms, forehead, sides of face.
Fontanelles small
Few or no creases on soles of feet.
Small eyes, pinna falls forward, ears lg, absent swallowing or sucking if <33 weeks
Reflexes poor, rarely cries (week high pitch)
Preterm
Potential Complications
Anemia of Prematurity:
Normochromic, normocytic anemia
Reticulocyte low
Pale, lethargic, anorectic
Due to hematopoietic system and destruction of RBC due to low levels of vitamin E
Give DNA recombinant erythropoietin, blood transfusion, vitamin E, iron
Preterm
Kernicterus:
Destruction of brain cells by invasion of indirect bilirubin.
More prone due to acidosis
Less serum albumin to bind indirect bilirubin (low as 12mg/100 mL)
If jaundice – phototherapy or exchange transfusion.
Persistent Patent Ductus Arteriosus:
Lack surfactant – lungs noncompliant.
Preterm
More difficult to move blood from pulmonary artery into lungs.
Causes pulmonary artery hypertension, which may interfere with closure of the ductus arteriosus.
Indomethacin given may initiate closure of patent ductus arteriosus.
Periventricular/Intraventricular Hemorrhage:
Bleeding into tissues surrounding the ventricles or into the ventricles.
Occurs in 50% of low birth wt. baby’s
Preterm
Fragile capillaries and immature cerebral vascular development.
Do cranial ultrasound to detect if hemorrhage has occurred.
Other Potential Complications
Difficulty initiating respirations
Give mother O2 by mask during birth.
Resuscitate within 2 minutes after birth.
Keep warm, periodic respirations.
Preterm
Water loss due to lg body surface
Unable to concentrate urine, excretes high proportion of fluids. 40 to 100mL
/kg/24h
Needs 160 to 200 mL of fluid /kg of body wt. (IV 27 gauge needles)
Umbilical venous catheter.
Monitor wt., urine output, specific gravity, serum electrolytes.
Blood glucose q 4-6 hours (40 to 60 mg/dl
Keep record of all blood drawn.
Preterm
Nutrition – requires lg. amount.
Immature reflexes, sm stomach,
Feeding Schedule
TPN until stable, chest x-ray before first feeding.
Needs 115 to140 calories/kilogram of body wt /day
May take 1 to 2 mL every 2 to 3 hours.
Gavage Feeding
Gag reflex not intact until 32 weeks
Preterm
Give 1 mL /hour
Introduce breast or bottle feeding gradually as infant matures.
Pacifier helps strengthen sucking reflex
Formula
Caloric concentration 24 cal/oz
Minerals and electrolytes
Vitamin K 0.5 mL, E, A.
Breast Milk
Best, mother can express. High in sodium
Preterm
Difficulty maintaining body temperature.
Baby remains extended.
Little subcutaneous fat, and brown fat.
No shivering, or sweating.(immature CNS)
Skim is easily traumatized and less resistant to infections. Has difficulty producing phagocytes and has deficient of IgM antibodies.
1st and 2nd periods of reactivity observed in 1 h and 4 hours are delayed.
Preterm
Reactivity may not appear for 12 to 18 hours, (conserve energy).
Infant needs loving attention.
Give information and support.
Sibling visitation and restrictions.
Schedule visits, procedures, rest, decrease pain.
Prepare for discharge.
Plans for beyond the immediate newborn period.
Postterm Infant
After 42 weeks of pregnancy.
Induction of labor at 2 weeks postterm.
Risks:
Placenta functions effectively for 40 weeks.
Infant develops postterm syndrome:
Dry, cracked, almost leather like skin.
Absence of vernix
Lightweight
Less amniotic fluid, meconium staining.
Long fingernails
Postterm
Alertness more like a 2 week old baby.
Sonogram
Nonstress test or biophysical profile.
Cesarean birth may be indicated.
At birth, difficulty establishing respirations.
Hypoglycemia
Low SQ fat, temperature regulation difficult
Polycythemia, dehydration.
Elevated hematocrit.
Woman becomes anxious and angry.
Postterm
Feels the baby should be extra strong and healthy since it was in utero longer.
Track developmental abilities until school age.
Neurological symptoms that become apparent when fine motor tasks attempted.
Illness In The Newborn
Respiratory Distress Syndrome RDS:
Formerly termed hyaline membrane disease
Occurs in perterm infants, infants of diabetic mothers, cesarean births, for any reason for decreased blood perfusion of the lungs.
Patho: hyaline-like (fibrous) membrane comprising products formed from an exudate of the infant’s blood that lines the terminal bronchioles, alveolar ducts, and alveoli. Prevents the exchange of oxygen
Illness In The Newborn
and carbon dioxide at the alveolar-capillary membrane.
Cause: low level or absence of surfactant.
High pressure is required to fill lungs with air for the first time and overcome the pressure of lung fluid.
Areas of hypoinflation occur and pulmonary resistance is increased,
Blood shunts through the foramen ovale and the ductus arteriosus as it did during fetal life. Surfactant decreases even further.
Illness In The Newborn
Poor O2 leads to tissue hypoxia, which causes release of lactic acid. Increased
CO2 > severe acidosis > vasoconstriction and decreased pulmonary perfusion
>decreased surfactant production > alveoli collapsing.
Assessment:
After resuscitation may seem stable or may have subtle signs:
Low body temperature
Nasal flaring
Sternal and subcostal retractions
Illness In The Newborn
Tachypnea > 60/minute
Cyanotic mucous membranes
With in several hours:
Expiratory grunting, indicates prolonged expiratory time, compensatory mechanism from closure of the glottis.
Increases pressure in alveoli on expiration
Helps keep alveoli from collapsing
Makes O2 exchange more complete
Illness In The Newborn
Disease progresses infants become cyanotic
PO2 and O2 saturation levels fall
Rales and diminished breath sounds
Exhibits:
Seesaw respirations
Heart failure
Pale gray skin
Periods of apnea
Bradycardia
Pneumothorax
Illness In The Newborn
Diagnosis made on signs of :
Grunting, cyanosis in room air, tachpnea, nasal flaring, retractions and shock.
Chest X-Ray (ground glass-haziness)
Blood gas studies (umbilicial vessel catheter- for acidosis)
Group B strep mimics RDS
Cultures of blood,CSF and skin to rule out infection.
Tx.
Administration of surfactant through
Illness In The Newborn
endotracheal tube at birth. Infant is held upright and then tilted downward.
Oxygen administration:
Necessary to maintain correct PO2 and pH levels.
CPAP or PEEP
Retinopathy is possible complication.
Ventilation:
Inspiration shorter than expiration normally
Fear of pneumothorax
Illness In The Newborn
Impaired cardiac output
Increased intracranial and arterial pressure and hemorrhage.
Indomethacin may be used to cause closure of patent ductus artheriosus
Monitor I&O and for bleeding.
Pavulon IV-muscle relaxant-allows mechanical ventilation to work. Keep
Atropine and Prostigmin immediately available.
Illness In The Newborn
EMCO-Extracorporeal Membrane Oxygenation.
For chronic severe hypoxemia in newborns with meconium aspiration, RDS, pneumonia, diaphragmatic hernia, near drowning victims or infants with severe lung infections.
Blood is removed by gravity using a venous catheter in rt. atrium of heart to
EMCO-oxygenated and rewarmed-returned to infants aortic arch.
Illness In The Newborn
ECMO is used for 4 to 7 days
Risk of intracranial hemorrhage, possibly due to anticoagulants.
Liquid Ventilation:
Use of perfluorocarbons
Weight of the fluid helps distend the lung, O2 is carried with it and spreads over the lung surfaces and O2 exchange occurs.
Nitric Oxide:
Causes pulmonary vasodilation and can
Illness In The Newborn
help increase blood flow to the alveoli when persistent pulmonary
hypertension is present.
Supportive Care:
Keep warm, hydrate, nutrition with IV fluids, glucose or gavage feedings.
Prevention:
RDS rarely occurs in mature infants.
Tocolytic agents- terbutaline,
Steroids quicken formation of lecithin production pathways.
Illness In The Newborn
2 injections of glucocorticosteroid- betamethasone to the mother at 12 and 24 hours before birth.
Sometimes there is no warning that preterm birth is imminent.
Transient Tachypnea of the Newborn
At birth a newborn may have a respiratory rate of 80breaths /min, then within
1 hour it slows to 30 to 60 breaths /min.
Rate remains high at 80 to120 breaths/min.
Illness In The Newborn
Slow absorption of lung fluid.
Occurs more often in:
Infants born cesarean,thoracic cavity is not compressed by force of vaginal birth, less lung fluid is expelled than normal.
Infants whose mothers received extensive fluid administration during labor
Preterm infants.
Monitor for fatigue, respiratory obstruction.
Peaks at 36 hours of life, fades by 72 hours.
Illness In The Newborn
Meconium Aspiration Syndrome
Meconium is present in fetal bowel at 10 weeks gestation.
Fluid at birth is green to greenish black.
Infant may aspirate meconium in utero or with first breath at birth.
Causes distress by:
1. Inflammation of bronchioles
2. Block small bronchioles by mechanical plugging.
Illness In The Newborn
3. Decrease in surfactant production through lung cell trauma.
Hypoxemia, CO2 retention, and intrapulmonary and extrapulmonary shunting occur
Secondary infection of injured tissue may lead to pneumonia.
Assessment;
Apgar score low, tachypnea, retractions, and cyanosis occur.
Suction before shoulders are delivered.
Illness In The Newborn
Intubate and suction, no O2.
Coarse bronchial sounds, retractions
Barrel chest
Blood gases
Chest X-ray-bilateral coarse infiltrates in the lungs.
Tx.
Amniotransfusion-to dilute amniotic fluid
After tracheal suction, O2
Antibiotic
Illness In The Newborn
Monitor for heart failure
Keep warm
Chest physiotherapy with clapping and vibration.
Apnea
Pause in respirations longer than 20 seconds with accompanying bradycardia.
Beginning cyanosis may be present.
Gently shake or flick the sole of foot stimulates baby to breath.
Resuscitation
Illness In The Newborn
Apnea monitor
Ventilator until mature
Keep warm and gentle handling
Never take rectal temp.
Theophylline or caffeine sodium benzoate to stimulate respirations.
High for SIDS
Monitor for 2 to 6 months.
Sudden Infant Death Syndrome
Sudden unexplained death in infancy.
Occurs:
Infants of adolescent mothers
Infants of closely spaced pregnancies
Underweight infants
Preterm infants
Infants with bronchopulmonary dysplasia
Twins
Siblings of another child with SIDS
Native American, Alaskan native infants
Sudden Infant Death Syndrome
Economically disadvantaged black infants
Infants of narcotic-dependent mothers.
Peak age 2 to 4 months.
Theories of cause:
Prolonged but unexplained apnea
Viral respiratory or botulism infection
Pulmonary edema
Brain stem abnormalities
Neurotransmitter deficiencies
Heart rate abnormalities
Sudden Infant Death Syndrome
Distorted familial breathing patterns
Decreased arousal responses
Possible lack of surfactant in alveoli
Sleeping prone
Well nourished infants, slight head cold.
After being put to bed infant is found dead a few hours later.
Autopsy often reveals petechiae in lungs and mild inflammation and congestion in respiratory tract.
Sudden Infant Death Syndrome
Put newborns to sleep on back or side.
Hard to accept by parents.
Support.
When another child is born parents are frightened.
Apnea monitor.
Apparent Life-Threatening Event
Infant discovered cyanotic and limp in bed but survived after mouth to mouth resuscitation.
Illness In The Newborn
Apnea monitoring – alarms when 20 sec or more of apnea or decreased heart rate of 80 bpm. Stressful for parents.
Parents need CPR.
Periventricular Leukomalacia
Abnormal formation of white matter of the brain.
Caused by ischemic episode that interferes with circulation to a portion of the brain.
Phagocytes and macrophages invade the area to clear away necrotic tissue.
Illness In The Newborn
Sonogram
Occurs in preterm infants with cerebral ischemia.
May have learning disabilities.
Hyperbilirubinemia
Elevated level of bilirubin in the blood
Results from destruction of RBC by normal physiologic process or abnormal destruction of RBC.
Hemolytic Disease of the Newborn
Illness In The Newborn
Destruction of RBC, mother builds antibodies against the infant’s RBC leading
to hemolysis of the cells.
Causes severe anemia and hyperbilirubinemia.
Rh Incompatibility:
Mother’s blood type is Rh (D)negative and fetal blood type is Rh positive
(contains the D antigen) the introduction of fetal blood causes sensitization to occur and the mother begins to form antibodies against the D antigen.
Illness In The Newborn
With 2nd pregnancy, a high level of antibody D circulating in mother’s blood
stream and acts to destroy the fetal RBC early in pregnancy if fetus is Rh positive.
Tx.-intrauterine transfusion
Preterm labor
ABO Incomparibility
Maternal blood type is O and fetal blood type is A (also type B or AB blood). A reaction in infant with type B blood is serious.
Illness In The Newborn
These antibodies are large (IgM) class and do not cross the placenta.
Hemolysis of blood begins with birth as the placenta is loosened and may continue for up to 2 weeks of age.
Assessment:
Preterm infants not affected.
Predicted by a rising anti-Rh titer or rising level of antibodies (indirect Coombs’ test) in mother during pregnancy.
Confirmed by detecting antibodies on the
Illness In The Newborn
fetal erythrocytes in cord blood (positive direct Coombs’ test) by umbilical blood sampling or at birth.
Mother Rh – baby Rh+
Liver and spleen may be enlarged
Edema and heart failure.
Hydrops fetalis
Edema, lethal state.
Illness In The Newborn
Management:
Initiation of Early Feeding
Sooner bowels elimination begins, sooner bilirubin removal begins.
Phototherapy
Light triggers liver to function
Quartz halogen, cool white daylight, or special blue florescent light.
Place 12 to 30 inches above newborn
Expose as much skin as possible
Total serum bilirubin 15 mg/dl at 24 to
Illness In The Newborn
28 hours of age.
Cover eyes, light harmful to retina
Stools bright green, loose
Urine dark color
Monitor temp, skin, dehydration
Home Phototherapy
To decrease physiologic jaundice rather than blood incompatability.
Phototherapy blanket.
Exchange Transfusion
When bilirubin rise rapidly
Illness In The Newborn
Baby’s stomach is aspirated
Umbilical vein is catheterized
Withdrawing small amounts of blood (2-10 mL)of infants blood and replacing it with donor blood.
Procedure lasts 1 to 3 hours.
Standards for exchange transfusion depends on indirect bilirubin concentration.
Removes 85% of sensitized cells
Keep infant warm
Administer albumin 1 to 2 hours before
Illness In The Newborn
procedure to increase number of bilirubin binding sites.
Blood type is O Rh negative
Monitor heart rate, respirations, B/P, umbilical vessel bleeding, infection.
Calcium glutamate is given after each 100 mL of blood
Blood glucose at 1 hour and bilirubin levels for 2 to 3 days.
Erythropoietin given to increase cell growth
Illness In The Newborn
Hemorrhagic Disease of the Newborn
Results from deficiency of vitamin K
Essential for formation of prothrombin by the liver >impaired blood coagulation.
K formed by action of bacteria in intestine
Begins after feeding (24 hours)
Infants with a deficiency show petechiae from superficial bleeding into the skin.
Bleeding occurs 2 to 5 days of life.
Prevention – Vitamin K 1 mg IM at birth.
Illness In The Newborn
Twin to Twin Transfusion
Occurs if twins are monozygotic (identical; share same placenta) and if abnormal arteriovenous shunts occur that direct more blood to one twin than the other.
Anemia in donor twin and polycythemia in receiving twin.
Identified by sonogram
Hemoglobin at birth has difference of 5.0 g/ 100 mL
Illness In The Newborn
Necrotizing Enterocolitis
Bowel develops necrotic patches, interfering with digestion and possibly leading to paralytic ileus.
Perforation and peritonitis may follow.
Retinopathy of Prematurity
Acquired ocular disease that leads to blindness, is due to vasoconstriction of immature retinal blood vessels.
Caused by high concentration of O2
Immature retinal blood vessels constrict
Illness In The Newborn
when exposed to high O2 concentration.
Leads to retinal detachment and blindness.
Most immature and ill infants are more exposed.
Cryosurgery or laser therapy may preserve sight.
Illness In The Newborn
Newborn at Risk because of Maternal Infections or Illness
Maternal Infection:
Newborns antibody production is immature.
Screen by TORCH assay.
Beta-Hemolytic, Group B Streptococcal Infection:
GBS, natural inhabitant of genital tract.
50 to 300 infants in 1000 births
Good handwashing spreads from baby to baby.
Illness In The Newborn
Tx. Ampicillin Iv at 28 weeks and again during labor.
Assessment:
Pneumonia 1st day of life
Late onset 2 to 4 weeks of age > meningitis
Tx.
Gentamicin, ampicillin, penicillin
Congenital Rubella
Causes extensive congenital fetal malformations if mother infected during 1st trimester.
Illness In The Newborn
A titer of less than 1:8 indicates a woman is susceptible.
Greatest risk at week 2 to 6.
Assessment:
Thrombocytopenia, cataracts, heart disease, deafness, microcephaly, motor and cognitive impairment.
Dx confirmed by identifying IgM antibodies against rubella in infants serum at birth.
Live rubella virus cultured from nasopharyngeal secretions at birth and 1 yr.
Illness In The Newborn
Women cannot be immunized during pregnancy because the vaccine used
contains a live virus.
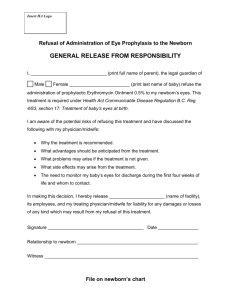
Ophthalmia Neonatorum
Occurs at birth or during 1st month.
Organisms- gonorrhea or chlamydia
Assessment:
Bilateral, conjunctiva is fiery red, thick pus, eye lids edematous.
Occurs on day 1 to 4 of life.
Illness In The Newborn
Tx:
Prophylactic erythromycin ointment into eyes.
Allow bonding period first.
If gonococci IV Rocephin or penicillin
Irrigate with sterile saline solution for discharge from eyes.
Mother and partners need treatment.
Risk of sterility or PID.
Illness In The Newborn
Hepatitis B Virus Infection HBV
Transmitted through contact with infected vaginal blood at birth. Mother
HBsAg+
70% to 90% become chronic carriers.
Develop liver cancer later in life.
Tx: HBIG immune serum globulin within 12 hours of birth.
Transmitted via breast milk, mother may feed after immune globulin given.
Illness In The Newborn
Generalized Herpesvirus Infection
Type 2 infection – multiple sexual partners
Contracted by fetus across placenta if mother has primary infection during pregnancy.
More often contracted from vaginal secretions from mother with active herpies at birth.
Assessment:
If acquired during pregnancy, infant may be born with vesicles covering skin.
Illness In The Newborn
Can have severe neurological damage.
If acquired at birth in 4 to 7 days infant has loss of appetite, low grade fever, lethargy, ulcers of mouth, vesicles on skin.
Develop dyspnea, jaundice, purpura, convulsions, and shock. Death within hours.
Survivers have permanent CNS sequelae.
Cultures to confirm
Zovirax
Cesarean birth
Crusted lesions
Illness In The Newborn
Human Immunodeficiency Virus Infection
HIV and AIDS can be caused by placental transfer or direct contact with maternal blood during birth.
Infant of a Diabetic Mother
Longer and weigh more than other babies.
Greater chance of cardiac defect, caudal regression syndrome(hypoplasia of lower extremities)
Fat and puffy appearance, lethargic or limp,
Illness In The Newborn
immature lungs, fragile giant, loses more wt. first few days.
Cesarean birth, hyperglycemic at first, hyperbilirubinemia, hypoglycemia.
Management:
Serum glucose level < 40 mg/dl
Fed early with formula or continuous infusion of glucose.
Monitor BM (smaller left colon)
Drug Dependent Mother
Tend to be SGA
Infant will show withdrawal symptoms:
Irritability
Disturbed sleep patterns
Constant movement, abrasions on elbows, knees or nose.
Tremors
Frequent sneezing.
Shrill, high pitched cry.
Possible hyperreflexia and clonus
Drug Dependent Mother
Convulsions
Tachypnea
Vomiting and diarrhea
Opiate withdrawal
Symptoms begin within 24 to 48 hours – 10 days. Last for 2 weeks.
Heroin-within 2 weeks, 72 hours. Last 8 to 16 weeks or longer.
Cocaine-no predictable withdrawal sequence. Causes long term coping behaviors. Poor sucking ability.
Drug Dependent Mother
Narcotic metabolites or quinine:
May be obtained from infants urine 1st hour after birth.
Quickly clear from the body, detection may no longer be possible.
Tx.
Firmly swaddle, decrease stimuli, darken room, pacifier.
Maintain electrolyte and fluid balance. IV
Drugs for withdrawal:
Paregoric, phenobarbital, methadone,
Drug Dependent Mother
Thorazine, valium.
No breast feeding.
Mother needs treatment.
Safe environment.
Long term neurological problems.
Fetal Alcohol Syndrome
Alcohol crosses placenta in the same concentration as in the maternal bloodstream.
Appears in 2/1000 newborns.
Newborn will have many problems.
Pre and postnatal growth restriction, CNS involvement, microcephaly, cerebral palsy, short palpebral fissures and thin upper lip.
May be tremulous, fidgety, irritable, week sucking reflex, sleep disturbances.
Fetal Alcohol Syndrome
Behavior problems, hyperactivity
Growth deficiencies
Need follow up so any future problems can be discovered.