Case Scenarios for Patient Care Seminar I
advertisement

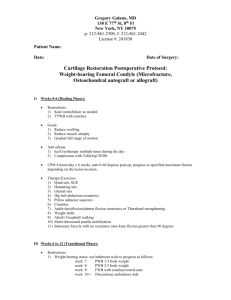
Case Scenarios for Patient Care Seminar I Spring 2014 Class of 2016 1. BPV 2. Sever’s Disease 3. ORIF ankle 4. TKA 5. CABG 6. ITB syndrome 7. Infantile Torticollis 8. ACL recon 9. GBS 10. Rib Fractures 11. Idiopathic Toe Walking PCS I Cases Katherine Deines, Jan Harting Melissa Randall, Leslie Schein, Amy McDevitt Jennifer Hide, Carrie Lamb Andy Kittelson, Danielle Sockolosky, Sharon Jordan Kyle Ridgeway, Dan Malone, Hope Yasbin Engel Bahar Shahidi, Stephanie Pascoe, Audrey Waldron Meghan Bawn, Lisa Hymes Justin Dudley, Lauren Hinrichs, Lara Canham Rebekah Griffith, Mark Manago, Angie Bruflat Guy Lev, Renee Peter, Tami Struessel Rebecca Downey, Nicole Parker Spring 2014 1 Case #1 Benign Positional Vertigo (BPV) (previously called Benign Paroxysmal Positional Vertigo or BPPV) Patient Name: Suzie Calfass Case history: Suzie Calfass is being seen in an outpatient PT clinic. Suzie is a 25 year old female who was involved in a minor car accident 4 weeks ago. She was hit from behind while sitting at a stop light. Initially she had headaches and a stiff neck. She experiences vertigo (the room spins) when she rolls over in bed to the right. When she does this she becomes nauseated and the room spins. She tries to avoid rolling to her right or sleeping on her right side. Denies any symptoms of diplopia, dysphagia, dysarthria or drop attacks. Diagnostic information No x-rays or other diagnostic tests were administered. Suzie has come into your outpatient clinic by referral from a family practice physician. Medications Birth Control Pills, daily vitamin Past Medical History Suzie is an otherwise healthy, active 25 year old. She is involved in a volleyball league at school, runs 3 miles 3 times per week, and walks her dog daily. She is single and lives in a condo near the school. Social History Suzie is a graduate student in the PT curriculum. She continues with her classes and has some difficulty in class unless she avoids bending over to pick up her books or moving her head quickly. She normally volunteers with a hippotherapy program, but has been unable to participate since the accident. Vital Signs Heart rate 66 bpm, Blood Pressure 110/82 Systems Review Cardiopulmonary: does not need further review Endocrine (Gastrointestinal): Needs monitoring Genitourinary: does not need further review Integumentary: does not need further review Musculoskeletal: needs further review Neurologic: does not need further review Needs further review. Based on the findings of the history and systems review, the following additional tests/measures were completed. Objective: Upper quarter screen reveals 2+ DTR’s, negative myotomal and sensory screening, and AROM of the cervical spine does not cause any UE pain or dizziness. PCS I Cases Spring 2014 2 MMT: MUSCLE GROUP /MOTION Elbow Flexion Elbow Extension Shld Flexion Extension Abduction Adduction Int Rotation Ext Rotation Lower trapezius Middle trapezius RIGHT SHOULDER LEFT SHOUDER Strength 5-/5 5/5 AROM 150 0 Strength 5-/5 5/5 AROM 150 0 5/5 5/5 5/5 5/5 5/5 4+/5 4/5 178 60 182 0 35 90 5/5 5/5 4/5 5/5 4/5 4+/5 4/5 180 65 175 0 40 85 4/5 4/5 Cervical Spine AROM measured with fluid inclinometer Flexion 46 Extension 52 Right lateral 38 flexion Left lateral 40 flexion Right rotation 68 Left rotation 70 Longus Colli endurance test (held chin tuck in supine without head contact on table, for up to 1 minute) 25 seconds. Suzie has a positive Dix-Hallpike to the right. She has upbeating, torsional nystagmus toward the downward ear. Vertebral artery testing is negative Palpation: Mildly increased tone with palpation in the upper trapezius and levator scapulae Dizziness Handicap Inventory: Functional subscale: 8/36 Emotional subscale: 4/28 Physical subscale: 18/30 Total Score: 30/100 PCS I Cases Spring 2014 3 Case #2: Sever’s disease Patient Name: Cal Davis Case History: It is early Spring, and Cal is an 11 year old boy referred by his family physician for bilateral heel pain due to Sever’s Disease. Cal started complaining of heel pain during his fall soccer season but essentially was able to cope until his winter/spring basketball and lacrosse practices overlapped. Cal was unable to run during either practice, nor participate in the running activities during physical education (PE 5 days per week). He reports that his heels hurt worse at the end of practice and games, especially after he is done playing. “I feel like I am having growing pains and the pressure from my gym shoes and cleats hurt my heels.” “When can I play my sports without hurting?” Cal and his parents are frustrated and very anxious to begin a rehabilitation program. They are concerned over the mention of a growth plate issue and very curious if this will impact his growth. Current Medical Status: Medications: Has taken ibuprofen 400 mg twice per day over the past 2 weeks. Diagnostic information: His family was told that x-rays indicated that the growth plate in the heel/calcaneus was still open and was likely the source of pain. Radiologist report read as “Possible widening of calcaneal apophysis with small fragmentation, correlate with history and physical examination.” Medical History: Has been healthy and active his whole life other than a Colle’s fracture after falling out of a tree when he was 10 yo. Social History: Cal is an extremely active 11 year old. He plays 3 sports: fall-soccer and lacrosse; winter-basketball and lacrosse; spring-lacrosse; summer-lacrosse. He is very stoic when it comes to his pain because he knows that pain means limiting his activity. In addition, he is in physical education classes 5 days per week. His PE teachers are quite concerned and have been in touch with the parents. Cal is concerned about his ability to play high school sports. Vitals: HR: 80 BP: 118/79 Observation: reddened area around both Achilles insertions into the calcaneous Systems Review Musculoskeletal: Needs further review Neurologic: Needs further review Cardiopulmonary: No further assessment required Integumentary: Needs further review Physical Exam: Posture: hyperextended knees bilaterally; supinated forefeet, inverted rearfoot PCS I Cases Spring 2014 4 Palpation: tender and warm around the insertions of both Achilles tendons ROM: Significant limitations in passive range: 0-degrees of dorsiflexion on right and 5 degrees on the left, full active and passive inversion, eversion and plantarflexion of the ankles bilaterally. Muscle/tendon length: Short Achilles bilaterally during standing small squat: heel unable to stay in contact with the floor Supine- hip flexion--knee extension length test for the hamstring: lacking 40 degrees of knee extension on right and 35 degrees on left Strength: Hamstrings Quadriceps Posterior tibialis Peroneals Anterior tibialis Gastrocnemious* R 5 5 5 4+ 4 5 L 5 5 5 4+ 4 5 *=pain with testing Function: Is unable to play sports or participate in PEdue to pain during and after this activity. He reports pain at the end of a school day after walking from class to class. Gait: walks with slight antalgia, limiting his push off and taking slightly shorter steps Pain: Visual analogue PCS I Cases 1-10; 10 after activity and 5 in the morning Spring 2014 5 Case # 3: Ankle fracture (ORIF) Patient Name: Sharon Olson 1) Case history: Mrs. Olson received a referral for physical therapy from her orthopedic surgeon which reads “ROM, strengthening, balance training-please note that bone scan shows moderate osteopenia., WBAT” Patient is seen at 5 pm following her workday at an outpatient practice using bilateral axillary crutches and minimally weight bearing on her right leg. a. Current Medical Status- removal of a below the knee cast yesterday from her right ankle following fracture when she slipped on ice and rolled her ankle while picking up the newspaper. She was to remain NWB while casted, but is able to WBAT at this time. Fracture occurred 10 weeks ago and surgical ORIF was performed immediately where hardware was placed in her tibia and fibula b. Medications- Actonel once per day c. Diagnostic info-The right distal tibial and fibular fractures are well healed by xray. d. Subjective- subjective report that swelling improves in the morning and is worse in the evening. She reports that her tolerance to standing is about 15 minutes, walking 5 minutes and that she wakes 1-2 times per night. She is able to perform her work duties that are primarily sitting but has difficulty walking around in the office for filing, mail distribution, and making copies and is unable to carry large files from office to office. She reports that her boss was very accommodating initially but he seems to be getting irritated that she has not been able to return to her full work duties. Pain: Numeric pain rating scale 1-10; 8 after activity and 3 in the morning 2) Past Medical History: negative except for the new diagnosis of osteopenia. 3) Vital Signs: a. HR: 76 bpm b. BP: 118/78 4) Social information- Mrs. Olson is a 52 year old divorced female legal secretary. She lives alone in a one level condo. 5) Systems Review Cardiovascular-needs further review Pulmonary- intact, does not need further review Integumentary- needs further review. Musculoskeletal-needs further review Neuromuscular-needs further review Communication/Learning- intact, does not need further review PCS I Cases Spring 2014 6 Based on the findings of the history and systems review, the following additional tests/measures were completed. 6) Additional findings i. AROM –right 0 degrees DF (knee extended), 35 degrees PF, 15 degrees inv, 5 degrees ever. Left 10 degrees DF (knee extended), 60 degrees PF, 32 degrees inv, 22 degrees ever. ii. Swelling increased by 2 cm on right by Figure 8 measurement. iii. Strength 1. Hip extension, flexion, abduction, adduction, IR/ER 4/5 bilaterally 2. Knee extension and flexion 4/5 bilaterally 3. Ankle a. Resistive testing of right ankle deferred. Able to actively move right ankle within available range (range as described above) b. Left: 4/5 DF, PF, inversion, eversion. iv. Observational- Slightly overweight, mesomorphic body type. Generalized atrophy noted in RLE. Incision is well healed. Skin dry and flaking. Scar mildly adhered along fibula, but not irritable. v. Gait-needed cueing to bear weight through the involved extremity. With cueing and axillary crutches, she demonstrated reduced right stance time, mild right circumduction, genu recurvatum on right with weight bearing during stance, but reports “less pain than I thought I would have” as she walks. PCS I Cases Spring 2014 7 Case #4 Total Knee Arthroplasty Patient Name: Roger Trenton Case history: Roger Trenton is a 75 year old male who underwent a right total knee arthroplasty one week ago and was referred to your home health agency following a 5 day stay at the local community hospital. (He spent 3 days on the acute care floor and 2 days on the transitional care unit (Skilled Nursing Facility (SNF) equivalent) for rehabilitation). The referral is for physical therapy: evaluate and treat in the home, after which he will continue with out-patient physical therapy. You are seeing him for the first time in his home where he has lived alone since his wife died 5 years ago. During the interview, Mr. Trenton reports that he was diagnosed with osteoarthritis in both of his knees 10 years ago. At that time he had x-rays taken with clear evidence of a narrowed joint space from thinning cartilage and an osteophyte at the medial joint line on the right tibia. Recent x-rays showed increased narrowing and an increased size of the osteophyte. Around that same time, he reports he was having pain with weight bearing (8/10), making walking difficult. Ambulation with a single point cane helped some but his walking tolerance was decreasing due to such severe pain on the inside of his knee. Pain even at rest was 5/10. Due to an increased sense of instability, increased varus deformity of right knee and increased mobility limitations, the physician recommended a total knee arthoplasty (TKA). One week ago the surgeon performed a right TKA, through a medial parapatellar approach. Medications: Naproxyn Low molecular weight heparin Oxycodone Beta Blocker Past Medical History: Ten year history of osteoarthritis in both knees. History of high blood pressure controlled with medication. Myocardial infarction 2 years ago with stent angioplasty. Vitals: HR: 82 bpm BP: 120/84 (right arm in sitting) RR: 16 Body temperature: 98.4° F (oral thermometer) Subjective: Mr. Trenton reports being glad to be home. He has minimal pain in the right knee since coming home. He does not like to take the pain medications. He prefers the ice and the home Continuous Passive Motion (CPM) unit. He states that he has a high pain tolerance and is ready to get up and begin moving. He is having difficulty lifting his right leg and standing on his right leg. He reported that he understood all the post-operative instructions and exercises. He was already measured at 75 degrees of knee flexion. He has been using the front wheeled walker since the surgery. He states that he is eager to get rid of the walker. He was also instructed in how to use axillary crutches prior to surgery, and has the single point cane he used regularly prior to surgery. PCS I Cases Spring 2014 8 Social information: Mr. Trenton has been an active dairy farmer all of his life. Despite his age, he remains very active, assisting his sons and grandsons with work on the farm. He is optimistic about his recovery and is eager to get back to work. Systems review: Communication /Learning: intact, does not need further review Musculoskeletal system: Needs further review Neuromuscular system: Needs further review Cardiovascular/pulmonary system: Needs further review Integumentary: Needs further review Based on the findings of the history and systems review, the following additional tests/measures were completed. Findings: 1. Pain scale (0-10) 2/10 in right knee; 1/10 in left knee. 2. Observation: no drainage, no elevated surface temperature. Incision looks to be healing well. Right knee is moderately edematous compared to the left. Wears full length elastic stockings (TED hose). 3. MMT not performed on the right knee. Observation of muscle performance indicates fair quadriceps setting. He is able to contract the muscle but unable to sustain the contraction or achieve end range knee extension. Bilateral hip MMT 4/5 abduction, 4/5 flexion, 4/5 extension. Left LE MMT 4+/5 knee flexion and extension. 4. Right knee: AROM 10° to 70°; PROM minus 5° to 75°. Left knee PROM and AROM 0-130°. 5. Bed mobility: uses hand to assist moving R leg in and out of bed. Independent with turning in bed. Minimal assistance needed in getting his right leg in and out of the CPM machine. 6. Transfers: Independent with sit<>stand from bed and dining room chair. Standby assistance for toilet and couch transfers due to lower surfaces. 7. Ambulates independently on level surfaces with a front wheeled walker with approximately 50% weight bearing from visual observation. He reports son held on to his belt the one time he went to basement stairs. “It’s awkward going downstairs with the walker.” 8. Home exercise program: patient demonstrates home program as shown to him in the SNF prior to discharge. He is performing ankle pumps, heel slides, quadriceps muscle setting independently. Requires minimal assistance with straight leg raises. 9. Self-care: currently limited in bathing and lower extremity dressing. He reports particular difficulty with donning TED hose. Occupational Therapy is scheduled to visit the day after the PT initial evaluation, so detailed assessment not completed. Home evaluation-Single level ranch style home, no stairs for entry or to reach bedroom and bathroom. Several throw rugs present. Able to maneuver into bathroom with walker. Stairs to basement, but he rarely needs to use them. PCS I Cases Spring 2014 9 Case #5 Status Post Cardiac Bypass Patient Name: Carl Bishop Case history: Mr. Bishop is 59 years old. He was diagnosed with high cholesterol and high blood pressure 15 years ago. 6 years ago he underwent angioplasty with stenting, which helped temporarily with his chest pain. Recently, he was referred by his primary care physician(PCP) to a cardiologist because he was very easily fatigued, and had begun to experience some angina again with exertion. He has been using nitroglycerin frequently, and his PCP was concerned, especially because his father died of a heart attack at 52. . The cardiologist ordered a new angiogram which showed 3 arteries in his heart that were mostly blocked, and suggested a consult with a cardiovascular surgeon. The surgeon recommended a bypass procedure. You are seeing him in the hospital one day after this procedure, with a referral stating “PT evaluate and treat. Precautions: median sternotomy”. Chart Review: You review the chart and find that he is to be on 2L oxygen by nasal cannula. Laboratory Values Glucose Potassium (K+) Ca++ Hemoglobin Hematocrit 188 mg/ dL 4.2 mEq/ L 9.7 mg/ dL 9.6 g/ dL 39% Vital Signs (taken one hours before your visit by nursing) HR BP RR SpO2 72 105/ 68 20 95% After reviewing the chart and speaking briefly with the nurse, you decide he is ready for a PT evaluation and enter his room. He is lying supine, awake, but groggy. No family/friends are present. The information below (Subjective/Social Information through Height/Weigh) is a composite from the chart and from talking to Mr. Bishop. Subjective/Social Information: Mr. Bishop is single and lives alone in a split level home with 4 steps to enter, and steps to go to his bedroom, bathroom and kitchen. He has trouble keeping up with all the things he needs to get done around the house, and he can’t really afford to pay anyone else to do the work. Before the surgery he was having trouble working as an electrician because of fatigue and occasionally from chest pain. Lifting supplies/materials at work was particularly strenuous. He is an Electrician for the IBEW Local 68, and mostly works on new construction. Since work has been scarce lately, he often works 60-80 hours per week if he gets called to a job. He must drive to his jobs, and the job requires lots of walking and carrying supplies weighing up to 50#, sometimes more. He often PCS I Cases Spring 2014 10 works in awkward spaces, including crawl spaces, and up on ladders. He has limited social support, but his sister lives nearby. In the short-term she will be helping with groceries and transportation on discharge. Medical History: Coronary artery disease (CAD), Hypertension, Hypercholesteremia Current Medications: Lipitor (statin), Propanolol (beta blocker), cardiazem (calcium channel) and aspirin. Patient controlled analgesia (PCA)/ morphine Weight 200#, Height 5’9”. Systems Review: Cognitive and communication: English speaker, communication is unimpaired Integumentary system needs further review based on history/surgery. Musculoskeletal system needs further review based on history and observation Neuromuscular system needs further review based on history Cardiopulmonary system needs further review based on history and observation Based on the findings of the history and systems review, the following additional tests/measures were completed. Observation: Mr. Bishop is lying in his hospital bed with a oxygen nasal cannula when you arrive. He is awake, but appears groggy. A PCA device is attached to IV pole and he has button in hand. On further observation, you note a median sternotomy, and mediastinal chest tube to 20 cm H2O suction. He has an IV in his right forearm, a LLE saphenous vein graft incision, and foley catheter. Pain: He reports pain in his chest and left lower leg. When asked to clarify, he reports pain from the incision and procedure, not chest pain like he had with exertion before surgery. AROM: All movements are full with the exceptions noted below: Right Left Shoulder flexion 120 125 Shoulder abduction 130 135 Strength: *mild discomfort Hip flexion Knee extension Knee flexion Dorsiflexion Gross Plantarflexion Right 4/5 4+/5 4/5 4+/5 4/5 Left 4/5 4+/5 * 4/5 * 4/5 * 4/5 * Functional Activities: Min assist for bed mobility (rolling & supine to sit). Supervision for sit to stand transfers. Instructed to limit upper extremity use to comply with sternal PCS I Cases Spring 2014 11 (sternotomy) precautions. He requires increased time and tends to hold his breath with all activities. Verbal cues for breathing sequence and sternal precautions during these tasks. Cardiopulmonary System: Heart rate Rest (supine) After moving from supine to sitting Activity (Ambulation) 74 78 Blood Pressure 100/ 66 98/ 62 Respiratory Rate 20 20 Pulse Oximetry 95 93 86 110/70 24 95 Ambulation: Able to ambulate with a 4 wheeled walker 50 feet with CGA. Vital sign response as noted in table above. Gait observation: shortened step length and decreased stance time on LLE due to pain. Timed Up and Go: 10.4 seconds PCS I Cases Spring 2014 12 Case #6 Illio-tibial band syndrome Patient Name: Isabella Benson Case history: Isabella is a 21 y/o single female college student. 4 weeks ago she began to notice pain on the outside of her right knee while biking. At the time, she was riding about 100 miles per week as she began to train for a race. In the past, she has placed in the top 10 for her age group in the amateur division of several races, and riding is her primary form of exercise. She uses clip type pedals. She continued to train and the pain became progressively more constant. She is now completely unable to ride more than 2 or so miles because near the bottom of her stroke (on the way down and way up), she gets intense pain on the outside of her knee. Standing up out of the saddle on hills seems to increase her pain. She reports an occasional grinding sensation that seems to decrease if she changes her knee/foot position while riding. Isabella reports frustration in that she doesn’t think she will be able to compete in the race in 4 weeks. She is even starting to notice pain walking between classes as the knee has become more irritated. She’s normally very active, but this injury is starting to impact her ability to stay fit. She denies trauma of any sort.. She is currently taking Ibuprofen 600 mg 3 times per day for pain. She went to the student health center where she received a referral for physical therapy. No radiographs were taken. Social history: Isabella lives in an apartment with 2 roommates. Her immediate and extended family live in a neighboring state. Previous Medical History: She is in good general health. She reports some previous right knee pain when riding long miles 2 years ago and occasional shin splints on both sides if she runs significant mileage. Because of this tendency, she’s given up running completely and only bikes. Vitals: BP 110/75, HR 65 Systems Review: No cardiovascular- intact, does not need further review Neuromuscular or integumentary systems are intact and do not require further review. Musculoskeletal system requires additional review. Communication/cognition: intact, does not need further review. Anthropometric characteristics: Ms. Matthews is 5 feet, 5 inches, 120 pounds Based on the findings of the history and systems review, the following additional tests/measures were completed. Pain: Pain is located laterally over the condyle of the right knee. On numeric pain rating scale, patient reports: 2/10 at rest 4/10 with significantly walking around campus 7/10 with riding her bike greater than 2 miles Observation: Moderate genu varum with high longitudinal arches bilaterally PCS I Cases Spring 2014 13 Lower quarter screen: negative sensation testing, AROM of the lumbar spine does not reproduce any of her symptoms, DTR’s are 2+ bilaterally. Sahrmann dynamic posture assessment: Small knee bend: drifts medially to the great toe Hip flexor length test (Thomas test): Greater hip extension when the hip is allowed to abduct Single leg stand/maximum pelvic drop: while standing on right, note an anterior pelvic tilt and medial femoral rotation. Palpation: Tenderness rated as 6/10 over the distal ITB as it crosses lateral femoral condyle Significant muscular/tendinous tension over the right ITB Muscle testing: Quadriceps Hamstrings Dorsiflexors as a group Plantar flexors Gluteus Medius Gluteus Maximus *mild discomfort lateral knee Right 5/5* 5-/5* 4+/5 5/5 4/5 4+/5 Left 5/5 5/5 4+/5 5/5 4/5 5/5 Joint Mobility: Patello-femoral, knee, ankle mobility normal Hip mobility normal except for mild decreased anterior glide of the right hip. Flexibility: Decreased length hamstrings (on right, mild lateral knee discomfort), quadriceps, plantar flexors Clinician Observation with movement: Walking, patient is noted to bear weight laterally on both feet. Gross foot mobility assessment: rigid feet bilaterally with high longitudinal arch. Noble compression test: positive on right PCS I Cases Spring 2014 14 Case # 7: Patient Name: Congenital Muscular Torticollis (CMT) Angela Dixon Case History: Angela Dixon is a 3 ½ month old baby girl. She has been diagnosed with Congenital muscular torticollis. Her parents indicate that they hope physical therapy can help Angela. They are concerned about how her head appears to tilt to the right side most of the time. They are most anxious for a remedial program. Previous Medical History: Angela was born after an uneventful full term pregnancy, and she has continued to have an uneventful perinatal period and has been healthy. She breastfeeds fairly well initially, but recently has been having difficulty. Her mother finds that both mother and baby are more comfortable when Angela is on the right breast, and therefore she is breastfed on that side more often. Recently, Angela has been spitting up frequently and her mother is concerned that she might not be getting quite enough to eat. Since she has been spitting up so frequently, her mother reports that keeping her neck skin folds clean is a challenge, and you note some skin maceration in the area. At this time, Angela has grown in a predictable pattern on the pediatric growth chart. She continues to have a rather erratic sleep schedule with occasional bouts of irritability. Her developmental milestones were screened by her Pediatric Nurse Practitioner who administered the Denver II Developmental Screening Test. The overall interpretation of the test was “Suspect,” as she had three caution items. The caution items were “hands together,” “head up to 90º,” and “sit-head steady.” At her two month well-child visit, her mother asked the pediatrician about the appearance of her head tilting to the right side. The pediatrician referred them for x-rays, and a radiological work-up did not identify any abnormalities in the cervical spine. The pediatrician then referred Angela to an orthopedic surgeon, and he has since referred her to you for outpatient physical therapy. Her vitals were reported as follows: HR: 104 bpm BP: 85/78 Social Information: Angela lives at home with her parents. Both parents work outside of the home, and she has a childcare provider (nanny) who takes care of her at home every day. The childcare provider speaks Spanish as her primary language, but she understands most of what is spoken to her in English. Angela has no siblings. Systems Review: Integumentary: requires further review Musculoskeletal: requires further review Neuromuscular: needs further review Cardiopulmonary: does not require further review Gastrointestinal: requires monitoring Cognition/Communication: needs further review Based on the findings of the history and systems review, the following additional tests/measures were completed. Additional findings: When placed in prone and in supported sitting, Angela demonstrated adequate voluntary control to hold her head against gravity, without bobbing, and look at objects and people in her visual field. However, her head stays tilted to the right (right ear to right shoulder) when PCS I Cases Spring 2014 15 in supine, when she lifted her head in prone, and when she was held out away from a supporting surface or her mother’s shoulder. She also held her head with the chin rotated to the left. When encouraged to track an object visually, she actively rotated her head approximately 90º to the left, but only about 30º to the right. Passive range of motion of cervical side bending/lateral flexion was approximately 70º to the right, and approximately 30º to the left. Passive cervical rotation to the right was limited to 45º degrees, but 90º to the left. Range of motion measurements were determined by visual estimation. There is a slight flattening of the occiput on the left side of her head. Palpation: Angela did not show any signs or symptoms of pain with palpation in any neck musculature, but a small nodule was noted in her right sternocleidomastoid muscle. Observational: Although Angela exhibits limitations in active range of motion, she does not appear to be in discomfort. She does show some resistance with passive movement of her head to the end ranges of right cervical rotation and left cervical side bending. Angela’s mother and father gently rock her as they do passive stretches with her neck to gain range of motion. Inspection of the skin folds reveal maceration, but nothing severe. You discuss how to keep those clean with her mother. PCS I Cases Spring 2014 16 Case #8: ACL reconstruction Patient Name: Ashley Smith History: Ashley is a 42 year old female with a referral for “physical therapy post left ACL reconstruction, FWB using crutches, evaluate and treat.” She injured her knee jumping out of her Fedex delivery truck holding a large package, during a snowstorm. She hit a patch of ice and fell to the ground, twisting her knee inward, at which point she felt a loud pop. One week after the injury, she underwent an ACL reconstruction using an ipsilateral patellar autograft. Today is 4 days after the surgery. She reports that her knee feels like a “toothache” and is moderately swollen, especially if she forgets to elevate her leg. She is walking most of the time with her crutches, but does walk around short distances within her home without them. She rates her pain as 5/10 on average that goes up to 7/10 at worst on a 0-10 verbal pain scale. When it gets over a 5/10, she takes Vicodin. Social history: lives alone in a 2 level townhouse Work: She has been a Courier for Fedex for 12 years, requiring lifting up to 70 pounds, frequently walking quickly on uneven surfaces, in all weather. She is currently off work due to her injury. Medical history: a. Exercise-induced asthma that seems worse in cold weather. Smokes 1 pack of cigarettes daily b. Medications-using Vicodin prn for pain, inhaler for asthma c. Diagnostic info-Pre-operatively, MRI confirmed a complete rupture of her left ACL. No other structures were involved. d. Vitals: HR 80 bpm, BP 125/85, RR 18 e. Height 5’7”, Weight 145 # Systems Review Cardiovascular-Pulmonary-requires further review Integumentary- requires further review Musculoskeletal- requires further review Neuromuscular- requires further review Communication/Learning Ability-able to respond to questioning, no issues with communication Physical Examination Findings Inspection: 3 intact scope holes, and midline patellar tendon incision left knee. No redness or drainage. Quadriceps atrophy evident left knee. MMT Right Left Quadriceps 5/5 Deferred (see below) PCS I Cases Spring 2014 17 Hamstrings 4/5 Deferred Gastrocnemius 4/5 3/5 DF 5/5 4/5 with mild knee pain Hip abduction 5/5 4/5 with mild knee pain Functional movement: unable to complete a quadset, or straight leg raise on the left. Bed Mobility/Transfers: Is independent with all transfers, but tends to use arms to support under knee during bed mobility and supine to sit and sit to supine transfers. Gait: Tends to stand in genu recurvatum on the left and bears weight in standing only through the toes of her left foot. She bears minimal weight on her left leg during gait, but uses an appropriate gait pattern. Gait is cautious and slow. AROM of her knee is -15-90 degrees with discomfort reported with overpressure into flexion. Circumference measurements: Right Left 10 cm above mid-patella 26 cm 24.8 cm Mid-patella 27 cm 28.4 cm 10 cm below mid-patella 24 cm 24.5 cm Left positive ballotable patella. No joint line tenderness. PCS I Cases Spring 2014 18 Case #9: Guillain-Barré Syndrome (GBS) Patient Name: Gary Barnes Case history: Gary is a 30-year-old male who is employed as a sales representative for a computer storage firm and reports that he was training for a marathon when his symptoms began. He experienced a significant decline in function as a result of Guillain-Barré Syndrome, and has been unable to work or exercise since shortly after his symptoms began. He has no significant medical history. He lives in a 2 story townhome with his girlfriend. The bedrooms and full bath are upstairs, with a half bath on the main level. At the time of his first visit, he was an inpatient in an acute rehabilitation unit. Initial visit: He reported an initial onset of flulike symptoms during a vacation out of state. This was followed one to two weeks later by the onset of severe myalgias and arthralgias in the legs and unexplained fatigue. He was given a diagnosis of GBS one month after the initial onset of symptoms, at which time he was unable to heel or toe walk, felt very fatigued, had experienced a 15-lb weight loss, and was experiencing difficulty walking. After three weeks in inpatient care where he received specific medical care but was not intubated, he was admitted to the acute rehabilitation unit with stabilizing condition and improving function. At the time of the initial interview, it had been 6 weeks since the initial onset of flulike symptoms. During his stay in acute rehabilitation, he hoped to return to living independently with his girlfriend and hopefully to return to walking. His ultimate goal was to return to exercising, although he admitted doubts of being able to return to training as he had in the past. At the time of the initial interview, Gary denied current fever, chills, or sweating, and his vital signs were stable with BP 120/85 and HR 82 bpm. His skin color was normal. He reported weakness and fatigue related to the GBS, and this at first limited his participation in therapy to 20 minutes. In particular, he noted goals of improving moving around in bed, eating, transfers, and walking and standing. . He did report feeling a bit depressed due to the extremely unexpected turn his life had taken. The Integumentary system: requires monitoring Musculoskeletal system: requires more review Neuromuscular system: requires more reviewe Cardiopulmonary examination: requires monitoring Psychosocial and cognitive systems: requires monitoring Based on the findings of the history and systems review, the following additional tests/measures were completed. Deep Tendon Reflexes were absent for patellar tendon and Achilles tendon reflexes, 1+ for bilateral biceps and brachioradialis and trace for bilateral triceps. Functional mobility was more specifically assessed using the Functional Independence Measure (FIM). At initial examination, the patient’s FIM score was 80/126, with a motor subscore of 45/91. FIM subscores are noted in parentheses with each functional task observed. Observation revealed that Gary required supervision and use of bed rails for bed mobility tasks of sit to supine and supine to sit.(FIM score: 5) He required supervision to transfer from bed to wheelchair when set up using a sliding board (FIM 5) He required minimal assistance without the sliding board. (FIM 4) Gary required moderate assistance for bathing and dressing (3), PCS I Cases Spring 2014 19 minimal assistance for grooming and toileting, (4), and min assist for transfers to shower and toilet(4). He was unable to ambulate but was able to propel a wheelchair 30 feet on level terrain. (3) Muscle performance was assessed using manual muscle testing (MMT) which revealed significant symmetrical weakness as listed below. See below. Sensory testing for light touch revealed that sensation was impaired in a glove-and-stocking pattern. MMT Deltoids Biceps Triceps Wrist extensors Wrist flexors Hand intrinsics Hip flexors Quadriceps Hamstrings Dorsiflexors Plantarflexors PCS I Cases Right 3/5 3/5 2/5 3/5 Left 3/5 3/5 2-/5 3/5 3/5 3/5 3/5 3/5 3-/5 2/5 2-/5 1/5 2-/5 3-/5 2/5 1/5 1/5 2/5 Spring 2014 20 Case #10 rib fx Patient Name: Ahn Ngygen History: Ahn Nguyen presents to your outpatient clinic after her husband dropped her off for the appointment. She is a right-handed 48 year old female who was involved in a motor vehicle accident 8 weeks ago. During the accident, she sustained rib fractures in ribs 3-8 on the right side and a punctured right lung, but was otherwise uninjured. She was an unrestrained passenger in a car that was struck on the passenger side, and was taken to the ER and hospitalized for 4 days. The chest tube was removed on Day 3, she was monitored for 24 hours, then discharged home using an incentive spirometer. She has had no specific issues with her lungs since that time. About 2 weeks ago, she tried to return to work, but was unsuccessful because she was in too much pain with her work activities, including lifting, reaching and carrying cleaning supplies. Not being able to work has become a major financial hardship for her family and her primary goal for PT is to be able to go back to work. She works for a large contract cleaning company cleaning offices in the evening. Specific requirements of the job include lifting/carrying up to 50#, bending, reaching, stooping and lots of time on her feet. She is able to perform her basic self-care activities, but reaching overhead to wash her hair, and reaching behind her back are mildly difficult. She is getting used to using her left hand more, but that still presents some challenges, especially with driving. She is normally very involved in taking care of the house, and her family is assisting with most of that at this time. Pain: Pain is located laterally over the rib wall, and is increased with movement like reaching and bending, and with deep breathing. On the numeric pain rating scale (0-10), patient reports: 2/10 at rest 4/10 with reaching overhead 5/10 with lifting anything heavier than a plate of food at home She denies any numbness or tingling, or pain in her arms or neck, but does report some stiffness on the right side neck muscles. Imaging: Xrays just before her failed return to work showed fully healed rib fractures. Physician medical clearance: Her physician cleared her for return to work after the xrays were read, but when return to work was unsuccessful, he referred her to Physical Therapy. Medications: Taking 400 mg ibuprofen 3 times per day for pain control Social history: Ms. Nguyen is of Vietnamese descent, immigrating to the United States at 18 yo with her parents and 3 sisters. She understands most spoken English, but has limited reading and writing ability in English. Vietnamese is her first language, and it is spoken in her home. She is married to her husband Hai Nguyen, and they have 3 sons 10, 13 and 16. They live in northern Aurora, CO in a 3 bedroom ranch home. Previous Medical History: Overall Ms. Nguyen is in good health, although she does not currently do any sort of regular exercise. She does not smoke or drink alcohol. Anthropometric characteristics: 5 feet, 2 inches, 110 pounds BP is 112/90 and HR is 75 bpm Systems Review: Cardiovascular: pulmonary requires monitoring. PCS I Cases Spring 2014 21 Neuromuscular: intact, does not require further review. Integumentary system: requires further review Musculoskeletal system: requires further review. Cognition/Communication: requires monitoring Other Systems: intact, does not need further review Based on the findings of the history and systems review, the following additional tests/measures were completed. Observation: Slightly guarded, right arm held at side, with limited use of right hand for reaching, and with limited arm swing Posture: Rounded right shoulder, slightly guarded. Uses left hand for most reaching. Upper quarter screen: negative sensation testing, AROM of the cervical spine does not reproduce any of her symptoms although left sidebending is mildly restricted with pulling through the right upper trapezius. DTR’s are 2+ bilaterally. Sahrmann dynamic assessment: Standing shoulder flexion/elevation: o ROM limited by pain on right and she tends to extend her lumbar spine to obtain motion o FMP: lacks scapular upward rotation Pectoralis major length test: o Right short clavicular and sternal portion Palpation: Tenderness along entire right rib cage laterally, but no point tenderness. Closed scar from chest tube in the axilla, intercostals space between ribs 5 and 6 Significant muscular tension right upper trapezius, infraspinatus, subscapularis Thoracic spine AROM: limited by about 25% into right rotation, left rotation, and flexion with reports of pulling and discomfort through the right ribs. Shoulder complex AROM Flexion Extension Abduction ER at 90 degrees abd IR at 90 degrees abd *mild discomfort in ribs Right *155 55 *155 85 50 Left 170 60 170 88 65 Elbow AROM Flexion Extension Right 150 0 Left 150 0 PCS I Cases Spring 2014 22 Muscle testing: Infraspinatus Supraspinatus Lower trapezius Rhomboids Pectoralis major Serratus anterior Right 4/5* 4/5* Unable to obtain position for testing 4/5* 4/5* Painful with any testing so deferred Left 5/5 5/5 4/5 5/5 4/5 4/5 *mild discomfort in ribs Joint Mobility: Hypomobile ribs 2-9 right. Mildly hypomobile right glenohumeral joint all directions. Hypomobile right scapulothoracic joint, with decreased upward rotation, elevation Flexibility: Short latissimus dorsi and pectoralis major bilaterally, more severe on the right Mild pectoralis minor shortness Clinician Observation of movement: Protective positioning of right arm, and lacks normal right arm swing with gait Reduced scapulothoracic motion with right arm elevation Reversed scapulohumeral rhythm with right arm elevation With deep inhalation and exhalation, rib expansion on right is decreased, and she reports “tightness” and mild discomfort through the right ribs. PCS I Cases Spring 2014 23 Case #11 Idiopathic Toe Walking Patient Name: Collin Brown Case History: Collin is referred to your outpatient pediatric physical therapy clinic by his PCP with the prescription reading “toe walking – ROM, strengthening, etc.” Collin is a 4-year-old male with a diagnosis of idiopathic toe walking. His mother states this has been his walking pattern since he began walking at approximately 14 months old. She was told he would outgrow this pattern but this has not occurred. The toe walking seems to be getting worse with his recent growth and he has difficulty with balance when he tries to walk flat-footed. Collin now complains of mild foot pain at the end of his preschool day. His pain resolves with rest or after a warm bath. From a communication standpoint, he is able to follow most instructions, talks in 5-6 word sentences, and seems to understand the meaning of “hurt” Social History He lives at home with his mother and step-father. He does not have trouble getting around the home. Past medical history: Collin was born prematurely at 32 weeks gestation. He was hospitalized for 6 weeks in the NICU, but has been fairly healthy since home, except for frequent respiratory illness, such as cold and coughs. Frequent upper respiratory infection. Heart rate: 108 beats/min. Respiratory rate: 30 breaths/min. Current Medical Status – Getting over croup Diagnostic Information: A foot radiograph was taken at his 3 year old check up to assess status/alignment of foot/ankle bones. No abnormalities were found. Medications – None Systems Review – Cardiovascular -Pulmonary – requires monitoring Integumentary – intact, does not require further review Musculoskeletal – needs further review Neuromuscular – needs further review Communications/ Learning ability – requires monitoring Based on the findings of the history and systems review, the following additional tests/measures were completed: Physical Examination Findings: PROM – passive ankle dorsiflexion in subtalar neutral Left Right o Knee extended -10 -5o o o Knee flexed -5 -5 Active ankle DF (knee flexed) -5° -5° Bilateral ankle plantarflexion is full. No evidence of clonus bilaterally. PCS I Cases Spring 2014 24 Modified Ashworth scores are 1 for the hamstrings, quadriceps, peroneals, posterior tibialis, toe flexors and gastrocnemius muscles. Foot position in static standing – when heels are down, he stands with his knees in mild hyperextension. Pain: Collin Tolerates his mother rubbing his feet after a bath, but otherwise hypersensitive. He appears most sensitive on his heels. He is able to point to a pain scale picture that shows 4/10 pain when he comes home from preschool. Movement and Gait: Collin is an independent community ambulator who does not use any orthotics or assistive devices. When he walks, he demonstrates an increased anterior tilt, increased lordosis with his arms often held up in a high guard position. This posture is more pronounced with running. When walking backward, Collin’s ankle dorsiflexion position does not change. When he is asked heel walk, he is able to get his feet flat on the floor with increased knee hyperextension and he lifts his toes but not his feet off the surface He uses his toe extensors to assist with active dorsiflexion to clear his feet during swing phase of gait. Collin is able to balance at least 3 seconds on each foot. He does not yet hop on one foot or gallop, but he can jump about 5 times in a row on both feet. His preschool teacher describes him as hyperactive. Resistive testing: (see chart) Not always cooperative, so +’s and –‘s may not be completely accurate. Muscles: Iliopsoas / sartorius Gluteus maximus Gluteus medius Adductors Medial Hamstrings Lateral Hamstrings Quadriceps Anterior Tibialis Gastrocnemius / soleus Peroneals Posterior Tibialis Toe extensors Toe flexors PCS I Cases Left strength 4 4+ 3+ 45 5 4 4 5 4 4 3+ 5 Right Strength 4+ 4 4+ 35 5 4 4 5 4 4 5 5 Spring 2014 25