Urinary Elimination Study Guide
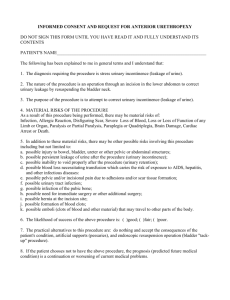
advertisement

Urinary Elimination Anatomy and Physiology Kidneys Functional unit is the nephron; remove waster products from blood and regulate fluid and electrolyte balance Glomerulus is a cluster of capillaries where the blood is filtered and urine is formed. Protein does not normally filter through, so proteinuria indicates a problem. _______________ connect kidney to bladder Bladder is a reservoir for urine Urethra connects bladder to urethral meatus; the external urethral sphincter permits voluntary flow of urine Factors Influencing Voiding Growth and Development Children cannot control urination until 18-24 months Nocturnal enuresis (is a problem if > 6 yrs old) Elders: impaired mobility affects toileting Sociocultural: privacy and social expectations Psychological: Anxiety and stress Personal habits: privacy and adequate time Positioning! Men should stand if possible and women should be in High Fowler’s if using bedpan Muscle tone: Weak abdominal and pelvic floor muscles cause incontinence Indwelling catheter causes loss of bladder tone Food and fluids Caffeine/Alcohol: mild diuretics Sodium: fluid retention Pathologic conditions: diabetes, MS, stroke, heart and renal failure, spinal cord injuries Surgery: anesthetics and narcotics can cause retention Meds: Diuretics increase output (Lasix, HCTZ); Important teaching: if ordered BID, take by 3pm to avoid nocturia Some change color of urine (Pyridium->orange urine) Terms Used Polyuria: void in abnormally lg amts Ex: Diabetes: polyuria, polydipsia, polyphagia Oliguria: Low urine output R/T Decreased fluids or impending renal failure Anuria: No urine output Dialysis: mechanism of filtering blood r/t kidney failure Hemodialysis and Peritoneal dialysis Frequency: more than usual Nocturia (2 or more per night) Urgency: feeling of need to void Dysuria: painful or difficult Hematuria: blood present Enuresis: Involuntary urination after age 4 Urinary Incontinence: Symptom, not disease; can have significant impact on life. Two types: Stress Incontinence: Leaking on coughing, laughing, sneezing, jumping Urge Incontinence: Unable to retain urine long enough after urge is felt Potential complication: _________________ Common Urinary Elimination Problems Urinary Retention: Unable to completely empty bladder -> urine accumulates-> bladder becomes distended -> risk for UTI and incontinence Potential Causes of retention: prostate gland enlargement; fecal impaction; pregnancy; anesthesia Can assess post-void residual with bladder scan or straight catheterization; >400ml is abnormal Urinary Tract Infections =40% of nosocomial infections, most due to non-asceptic catheterization; urosepsis is a life threatening complication; good handwashing and sterile technique during catheterization is essential Most common bacteria: E. coli (from colon) Causes: poor perineal hygiene; frequent sexual intercourse; bubble baths; residual urine Common symptoms: dysuria, urgency, frequency, hematuria If spreads to kidneys: fever, flank pain, chills Older adult may only show change in mental status Diagnostic tests: urinalysis; urine culture Treatment: antibiotics, antispasmodic (Pyridium) Urinary incontinence Stress Incontinence: leaking, dribbling on coughing, laughing Effective Treatment: Kegel exercises Imagine Elevator: contract up to 10th floor (count to 10) Relax and lower to 1st floor (count to 10) Repeat 10 times in a row 3-5 sets per day Urge Incontinence: incontinence after strong sense of urgency; may be in small or large amounts Effective Treatment: timed voiding (every 2 hours) and bladder retraining gradually postpone intervals between voiding to 4-6 hrs; stabilizes bladder Diversions Urinary Stoma Incontinent or continent Nephrostomy Tube placed in renal pelvis Nursing Assessment History: Voiding pattern (day and night, amount) Description of urine Any elimination symptoms, specifically: Frequency Urgency (difficulty getting to bathroom) Small amts or feeling of bladder fullness Dysuria (painful) Accidental leakage Men: hesitancy (difficulty starting stream) Hx of UTIs? Factors influencing Urinary Elimination: meds (espec diuretics), mobility and self-toileting status, fluid intake, past illness and surgery, previous dx tests) Patient Expectations PE: Percussion for _______________ tenderness, palpation of bladder Assessing Urine Assessing Input/Output and 24 hr trend Assessing characteristics (color, clarity, odor, hematuria) Measuring urine Measure in calibrated container from hat, bedpan or catheter bag Normal = 60 ml/hr * REPORT * if less than 30 ml/hr Common Diagnostic tests: To check for UTI: urine dip or urinalysis (UA) Urine culture requires sterile/”Clean catch” Identifies # and type of bacteria as well as antibiotics to which it is susceptible and resistant 24 hour urine sample Tests that evaluate kidney function: Serum Creatinine and BUN Interpreting Urinalysis (UA) Infection is indicated if: Presence of elevated WBC Presence of nitrite Presence of leukocyte esterase This is a performance standard for the course Common Nursing Diagnoses NANDA: Impaired Urinary Elimination Stress Urinary Incontinence Urge Urinary Incontinence Total urinary incontinence Urinary Retention Toileting self care deficit Nursing Diagnosis As Etiology of another issue: Risk for Infection R/T Urinary Incontinence Risk for Impaired Skin Integrity R/T Urinary Incontinence Knowledge Deficit R/T Prevention of UTI Risk for Caregiver Role Strain R/T Urinary Incontinence Social Isolation R/T Urinary Incontinence Goals Maintain or Restore Normal Voiding Regain Normal Urine Output Prevent Associated Risks: Infection, Skin Breakdown, Fluid/Electrolyte Imbalance, Decreased Self Esteem Perform toileting activities independently with assistive devices Nursing Interventions Maintaining Normal Urinary Elimination Promoting Adequate Intake (________________cc/day) Contraindicated if CHF, Kidney Failure Maintaining Normal Voiding Habits Positioning Relaxation Timing Promotion of Complete Emptying Drug Therapy Increase emptying (in retention): Urecholine (Bethanocol) Decrease hyperactivity of bladder (in urge incontinence) Tolterodine (Detrol), Oxybutinin (Ditropan) Teaching: Preventing UTI: Drink 8 8-oz glasses of water/day Void frequently; do not “hold” Void after intercourse (*evidence-based) Avoid harsh soaps, bubble baths Increase acidity of urine (Vit C, cranberry juice) Wipe front to back Managing Urinary Incontinence Maintain Skin Integrity Skin that is continually moist becomes macerated; urine converted to ammonia: irritating After incontinence, wash thoroughly with soap and water; rinse, dry thoroughly and provide dry clothing or linen Barrier creams (Zinc oxide) Absorbant draw sheets External Devices: condom, external catheter (not very effective) For Stress Incontinence: _______________ exercises For Urge Incontinence: Timed voiding or Bladder training Timed voiding has been found to significantly decrease patient falls in institutions Consider effect of socialization if living independently Managing Foley Catheterization 40% of nosocomial infections are R/T Foleys Nursing Interventions to Prevent UTIs in patients with Foley Catheters Fluids: 3000cc/day if permitted Perineal care: no special cleansing necessary but cleanse thoroughly after BM Good handwashing when working with Foley and bag Maintain sterile closed-drainage system No need to change tubing: Do not disconnect tubing unless absolutely necessary Remove catheter as soon as possible to prevent nosocomial UTI Assessments: Monitor urine output: should be at least 60cc/hr If less: check placement If still no improvement call MD; could be clogged or could indicate serious condition Monitor color, clarity, odor of urine and mental status: at high risk for developing UTI Once Foley is removed, patient should void within 6-8 hours else requires urgent assessments/interventions for urinary retention Evaluation Reassess voiding patterns and signs of alteration Inspect urine Expectations were met? Demonstrate self care skills