Department of Pediatrics, Indira Gandhi Medical College, Shimla
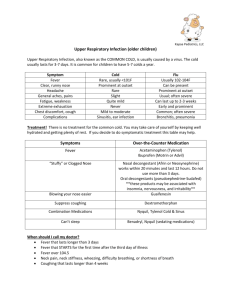
advertisement

ID/01(P) ROUND WORM INFESTATION LEADING TO MULTIPLE LIVER ABCESSES. Karuna Thapar, Renu Gupta,Ira Dhawan Dept. of Pediatrics, Govt. Medical College, Amritsar. renu.gupta31@gmail.com Introduction- The round worm (ascaris lumbroides) is one of the largest parasite that infest the human bowel and common in region with poor faecal sanitation,particularly in developing countries.Patient with ascaries can be asymtomatic or may present with different clinical features.Round worm most commonly reside in the jejunal and ilieum lumen. On occasion they migrate into duodenum and ampullary orifice,worm can then enter the hepatobiliary tree and pancreatic duct.The hepatobiliary duct system in children is smaller and thus more difficult for worm entry.The mean age of patient with hepatic ascaries is 4 to 70yrs.Here we report a case of 7 yrs male child with ascaries leading to multiple liver abscesses. Case Report- . Patient came with the complaints of vomiting, cough, pain abdomen,and fever for 4 days.Child passed worms during stay in hospital.Past history of passage of worms was also present.On examination general condition of the patient was unsatisfactory.Child was anaemic and febrile (high grade fever) with tenderness in right hypochondrium region.There was no cyanosis/icterus/lymphadenopathy/odema.Tachycardia and tachypnea were present.Respiratory distress in form of lower intercoastal and subcoastal recessions were present too.On anthropometry Wt=15Kg (against 25kg), Height=90cm (against 109cm),HC=46cm (against 53cm).Systemic examination was normal except respiratory and per abdomen examination.Chest movements were decreased on right side with diminished breath sounds. Abdomen was distended and tender, liver was 4cm below right costal margin with well defined margin. On investigation Hb 7.8gm,TLC 6500/mm3,DLC 70,26,00,000/mm,PBF showed toxic granulation in neutrophils,Mountx was negative,ESR 70mm.X Ray chest showed right lower lobe consolidation with tenting of diaphragm.On U/S abdomen multiple hypoechoiec lesion were seen,the largest lesion measured 18x17mm with irregular walls,multiple liver abscess and mesenteric lymphadenitis.Culture of microaspirate of abscess was sterile.Diagnosis of multiple liver abscess due to round worm infestation was made.Child was put on broad spectrum antibiotics for 3 weeks,recovered and then discharged.This case is being presented because of its rarity. ID/02(P) ISOLATED THROMBOCYTOPENIA : THE PRESENTING FINDING OF TYPHOID FEVER Karuna Thapar, Renu Gupta Dept. of Pediatrics, Govt. Medical College, Amritsar. renu.gupta31@gmail.com Introduction: Enteric fever, diagnosis is still made either clinically or by widal test and very rarely by blood culture. Thrombocytopenia is generally seen as a complication in typhoid fever. Platelet counts are normal to begin with and fall in some cases by second week of illness. However, it can also be encountered as a presenting sign on admission. Overall prevalence of thrombocytopenia is around 10-15%. Case Report: A 9 years female child was admitted with complaints of bleeding per rectum,petechie over the body,fever and diarrhea. On examination general condition was unsatisfactory,signs of hypovolemic shock were present.On examination of abdomen,hepatosplenomegaly and bowel sounds were present. Rest of systemic examination was normal, however petechie were present all over body.Child was not vaccinated for typhoid earlier.On investigation child was anaemic, TLC within normal limit,PBF revealed thrombocytopenia with platelet counts were just 2000/mm3. BT and CT were 7’04”, 7’21”respectivly, widal test tube method:TO 1:160;TH 1:160.All other causes of thrombocytopenia were ruled out. Platelet infusion along with enteric fever treatment was given. Child recovered and discharged.Thrombocytopenia is a rare presentation of enteric fever,so this case is being presented for its rarity. ID/03(P) CAN WE PREVENT PEDIATRIC HIV ?: EXPERIENCE AT A TERTIARY CARE HOSPITAL Maj R Praven, Col Ajay Srivastava, Col Rakesh Gupta, Brig Mukti Sharma Department of Pediatrics, AFMC Pune 411040 colrgupta@gmail.com Parent-to-child transmission (PTCT) of human immunodeficiency virus (HIV), the most common mode of acquiring HIV infection in children, vary from 25% to 45% and with effective interventions in mother and her baby, this risk can be minimized to less than 2%. This study was conducted to assess the efficacy of comprehensive PPTCT programme and outcome of infants born to HIV positive mothers at a tertiary care hospital. Patients and methods: All HIV exposed infants (babies born to HIV positive mothers) were followed up through pregnancy, delivery and after birth from Jan 2008 till Aug 2010. Mothers were given antiretroviral therapy as per institution protocol and babies were given syp Nevirapine single dose and Zidovudine till 6 weeks. All mothers were motivated not to breast feed their babies and reassured for follow up. DNA PCR was done at 6 weeks and 6 months for confirming the HIV status. Results: A total of 32 babies born to seropositive parents were evaluated in the study. Male to female ratio was 1:1. 29 mothers (90.6%) received antiretroviral therapy. 16 (50%) babies were delivered by cesarean section. 26 infants were given replacement feeding. Infant diagnosis was done by performing two HIV DNA-PCR tests at 6 weeks and 6 months. Twenty three infants were declared HIV negative after 2 negative DNA PCR tests, 7 infants yet to be confirmed, as they were below 6 months. 1 infant was found to be positive and started on HAART, and one infant lost to follow up. The Parent to child transmission rate at our center was 3.1%. CONCLUSION: PMTCT remains the best way of preventing pediatric HIV infection. In our experience, with administration of antiretroviral therapy to the mother and infant, use of breast milk substitutes and close follow up, the incidence of parent-to-child transmission (PTCT) can be reduced to negligible rates and thus pediatric HIV can be prevented significantly. ID/04(P) VISCERAL LEISHMANIASIS IN CHILDREN IN NON ENDEMIC AREA OF GARHWAL (UTTRAKHAND) N K Bhat, A Patel, A Rawat, B P Kalra, H Chandra Department of Pediatrics, Himalayan Institute of Medical Sciences, Dehradun. drnmbhat@gmail.com Introduction: During last decade adult cases of Visceral Leishmaniasis(VL) are being reported from nonendemic high altitude hilly areas of North India. We report on six children with VL from Garhwal region of Uttarakhand. To our knowledge these are first case reports of VL in children from this area. Methods: Retrospective chart review of cases diagnosed as VL Case repo rts: Case No. 1 2 3 4 5 6 The Age(years) 4 16 12 4 8 14 char acter Sex F M F F M M istics Fever(months) 3 4 3 1 1 5 of 6 Liver span(cm) 10 10 9 11 10 10 pedi Spleen(cm) 8 16 4 4 9 15 atric patie Hb(gm/dl) 5.9 5 7 6.8 3.0 7 nts TLC(/mm3) 3120 950 1630 2750 2250 810 of VL Platlet 55,000 20,000 34000 30,000 49,000 80000 are count(/mm3) tabul SGOT(U/L) 24 20 42 98 64 28 ated SGPT(U/L) 82 134 78 285 184 168 belo w. Creatinine(mg/dl) 0.5 1 0.6 0.6 0.5 0.8 These children had never visited any endemic area and were diagnosed on basis of clinical features and demonstration of leishmania donovani bodies in bone marrow. All patients were treated with sodium stibogluconate(20mg/kg/day) for 4 weeks and were declared disease free on the basis of improvement in clinical features, reduction in size of liver and spleen and lack of recurrence of symptoms during six months follow up. Conclusion: Keep high index of suspicion for VL while treating children with fever and hepatosplenomegaly from Garhwal region of Uttarakhand which is emerging as a new focus of VL. ID/05(P) PROFILE OF ENTERIC FEVER AND FEVER CLEARANCE TIME Subandhu Gupta, Meetu Rawat Gupta, Ritu Varma, Lallan Kumar Bharti 8/4 Ground Floor, Old Rajendra Nagar, New Delhi – 110060 subg2002@yahoo.com Introduction: Enteric fever is a serious public health problem in India. It leads to prolonged morbidity and school absenteeism. Hence it is vital to assess the fever clearance time in children receiving parental antibiotic therapy. Aims and Objective: To assess fever clearance time(FCT) of enteric fever in children on parental Ceftriaxone(75mg/kg/day). Material and methods: Prospective data of hospitalized patients with Enteric fever was collected from January to August 2010. Results: 225 children with clinical features suggestive of Enteric fever and Typhidot IgM positive titers were enrolled, of mean age 7.87±3.06years and male:female ratio 118:107. Mean fever duration at admission was 16.29±10.93days. Mean duration of FCT was 5.40±2.65 days with no significant difference between boys(5.37±2.85days) and girls(5.44±2.43days). There was positive correlation of FCT with Widal titers in increasing dilution of 1:80(88), 1:160(58) and 1:320(79) for somatic antigen, where FCT was 4.59±1.81, 5.31±2.84 and 6.38±3.24days respectively. 128 children had received no prior antibiotics while rest had received either Cotrimaxozole(5.33±2.77days), Amoxycillin(5.83±2.04days), Cefexime (5.74±2.75days) Ofloxacin(5.9±2.77days), or Azithromycin(3.33±1.53days). FCT in those receiving prior Amoxycillin(6) was 3.83±0.75days, Cotrimoxazole(15) was 4.60±1.96days, Ofloxacin(52) was 5.12±2.49days, Cefexime(23) was 5.43±2.87days, Azithromycin(3) was 5.33±4.16days and without antibiotics was 5.69±2.76days. Mean duration of Ceftriaxone usage was 6.92±2.02days and Azithromycin was added in 12% cases after 6.48±1.72days of parenteral Ceftriaxone. In 2%cases fever responded after stopping all parenteral drugs. Conclusions: FCT was increased with respect to rising titers of somatic antigen. FCT in patients receiving parental Ceftriaxone was 5.40±2.65days. FCT was lower in patients already receiving oral antibiotics. Drug fever should be considered in prolonged fever cases. ID/06(P) SPECTRUM OF OPPORTUNISTIC INFECTIONS & ITS CORRELATION WITH IMMUNOLOGICAL STATUS Suprita Kalra kalrasuprita@gmail.com Introduction: Opportunistic infections (OIs) are an important cause of morbidity & mortality in pediatric HIV however highly active antiretroviral therapy (HAART) has significantly reduced the incidence. There is paucity of Indian data regarding prevalence & immunological correlation of OIs. Objectives: This was a prospective study from Jan 2007 to July 2010 at Pediatric HIV clinic. All the enrolled HIV positive children were followed up for clinical & immunological status. All episodes of OIs during the study period were recorded & analysed. Results: Total 225 HIV positive were children enrolled. Mean age was 8.4 yrs. Male to female ratio was 1.39:1. Mode of transmission was vertical in 218 (96.8%).Mean age of onset 2.1 yrs. 109 children had at least one episode of OI with total 212 episodes (average 1.94 OI per child). 121 children were on HAART. The OIs were seen more frequently in immune cat III & IV than in immune cat I & II. Significant correlation of number of OIs with immunological category (p=.041). Most commonly seen OI was TB followed by serious bacterial infections.Oral/mucosal candidiasis,Herpes ,Chickenpox, chronic parotitis & Pneumocystis carinnii pneumonia were also common. An extremely low incidence of OIs in children on HAART (10%) as compared to HAART naïve HIV positive children (89%). Conclusions: The children in immunological stages III & IV had a significantly higher incidence of OIs with TB, serious bacterial infections.Oral/mucosal candidiasis,Herpes ,Chickenpox chronic parotitis & Pneumocystis carinnii pneumonia being common. Extremely low incidence of OIs is seen in children on HAART. ID/07(P) A CLINICAL STUDY OF SPECTRUM OF TUBERCULOSIS IN BCG VACCINATED CHILDREN AND EFFICACY OF DOTS UNDER RNTCP Jahnavi Konwar, Harpreet Singh, P.Biswanath Dept. of Paediatrics, Assam Medical College, Assam jahnavikonwar@gmail.com Introduction: Tuberculosis is a common problem in developing countries like India with increasing morbidity and mortality. Inspite of BCG vaccination and efforts of RNTCP the incidence of TB in children has not come down to the expectation. Aims And Objectives: To observe the incidence, various presenting features and pattern of TB in BCG vaccinated children and to study the efficacy of DOTS regimen under RNTCP in vaccinated pediatric patient. Materials And Methods: Study consisted of 68 patients both Male and Female, 1-12 years of age suffering from TB, attending the OPD of pediatrics, AMCH, Dibrugarh. Data was collected using pretested proforma. Adetailed history, physical examination and appropriate investigation including Montoux test were done in all cases. All statistical analysis were done by student t test. Efficacy and compliance of DOTS for those patients treated under RNTCP analysed. Results And Observation: The majority of patients (55.87%) were less than 6 years of age, Male:Female (3:1), 79.39% of patients were suffering from various degree of malnutrition. BCG scar present was 88.23% cases. Montoux test was positive in 79.41%cases. Pulmonary TB was commonest type [57.35%], followed by TB meningitis [7.35%], pleural effusion [8.82%], TB lymphadenitis (11.76%), Abdominal TB and disseminated TB (4.4%). Favourable treatment outcome in children treated under DOTS was noted in 94.11%. Conclusion: In pediatric age group,TB is more common among poor socio-economic status. Fever, cough and loss of weight and appetite are common presenting complains. Compliance is high with short course standardized chemotherapy regimen given under a programme of direct observation. ID/08(P) SPECTRUM OF CHILDHOOD TUBERCULOSIS IN HIV COINFECTED AND NON HIV INFECTED CHILDREN Maj Sanjeev Khera, Col Rakesh Gupta, Brig Mukti Sharma Department of Pediatrics, AFMC Pune 411040 kherakherakhera@gmail.com Introduction: The global impact of the converging dual epidemics of tuberculosis (TB) and human immunodeficiency virus (HIV) is one of the major public health challenges of our time. The World Health Organization (WHO) reports 9.2 million new cases of TB in 2006 of whom 7.7% were HIV-infected. HIV infection is associated with an increased risk of extrapulmonary tuberculosis, and the risk increases as the CD4+ lymphocyte count declines. Aims and objective: This study was conducted to evaluate the impact of HIV coinfection on spectrum of childhood tuberculosis and evaluate underlying risk factors. Materials and Methods: A total number of 176 consecutive children below 18 yrs of age suffering from various forms of tuberculosis attending pediatric OPD/ receiving inpatient care at a tertiary care service hospital since Jan 2007 constituted the study population of this prospective study. The diagnosis of tuberculosis was based on the WHO criteria and IAP consensus statement on tuberculosis . After a detailed history, thorough clinical examination and informed consent diagnosis of HIV was confirmed. The cases were divided into two groups. “Group A” having HIV & TB coinfection and “Group B” comprising HIV negative TB. Clinicoepidemiological characters, Monteux test and the distribution of pulmonary and EPTB and their relation with immune categories was compared in two groups. Results: 61 children out of total 176 were found to be coinfected with HIV, making the prevalence of HIV coinfection in our study to be 35%. HIV coinfection was seen more frequently in children more than 5 years of age and in male sex. Monteux test was found positive in 50% of the HIV negative TB cases as compared to 8% of the HIV coinfected cases. Amongst the HIV coinfected cases extra pulmonary TB was seen in 36(59%) cases as compared to 48(42%) in HIV negative TB group. Amongst extra pulmonary TB abdominal TB, and disseminated TB were predominant in HIV coinfection group while CNS TB was more common in HIV negative TB group. Extra pulmonary TB was significantly associated with immune category III & IV stating underlying severe immunodeficiency as a risk factor. All the above observations were statistically significant ( Chi square test, p< 0.05). Conclusion: The prevalence of HIV coinfection in this study (35%) was substantially higher than that reported in previous studies. The study showed a high incidence of extrapulmonary form of tuberculosis in HIV/TB coinfection which was significantly associated with higher immune category. In the extra pulmonary group, abdominal TB and disseminated TB were seen more frequently in HIV/TB coinfection. ID/09(O) PROFILE OF COMMUNITY AND HOSPITAL ASSOCIATED MRSA INFECTION CHILDREN TREATED AT A TERTIARY CARE TEACHING HOSPITAL Anu Puthanveethil, Leni G Mathew C/o. Dr. Leni G Mathew, Professor, Dept of Child Health, CMC, Vellore 632004 lenigm@yahoo.com Introduction: The aim of this exercise was to study the profile of MRSA infections in children, identify risk factors and to look at the difference between community (CA-MRSA) and hospital associated (HA-MRSA) infection. Materials & Methods: Clinical records of 82 children with MRSA infection, treated at the pediatric department of CMC, Vellore from June’03 till May2008 were analyzed. There were 48 boys and 34 girls; mean age was 33.6 months. MRSA infection was classified as HA-MRSA if the child was admitted or had visited a health care set up more than 48 hours before obtaining culture material or there was documented previous hospital acquired infection. Those who didn’t fulfill above criteria were classified as CA-MRSA.Results: 38 cases of CA-MRSA and 44 cases of HA-MRSA were identified. 32% of CA-MRSA and 61% of HA-MRSA cases had at least one risk factor; these were skin diseases (13), CVA(7), invasive procedures(7) immunosuppression(7), malnutrition(4). 70% of HA-MRSA was isolated from ICU. All isolates of MRSA were susceptible to Vancomycin, Teicoplanin and Linezolid. 87% of CA-MRSA was susceptible to Netilmicin. 70 children recovered completely from the infection. Of the remaining 12, four died, 6 were DAR and 2 had persistent infection as per their clinical records. The ratio of CA vs HA- MRSA infections has increased from 1:4 in 2003 to 7:3 in 2008. Conclusion: 60% of CA-MRSA had no identified risk factor. There was a steady increase in the number of CA-MRSA during the study period, which could possibly be attributed to widespread antibiotic use in the community. ID/10(P) ASSESSMENT OF POLICIES AND PRACTICES REGARDING IMPLEMENTATION OF EVIDENCE BASED USE OF ANTIBIOTICS FOR NEONATAL SEPSIS. Reeta Bora, S. Apong Neonatal Unit, Dept. of Pediatrics, Assam Medical College, Dibrugarh apong_l@rediffmail.com Introduction: Neonatal Sepsis (NNS) is a leading cause of mortality among neonates. NMR in India is 37/1000 live births (WHO 2008) with Assam having NMR of 44/1000 LB. Neonatal Sepsis accounts for 18.6% of all neonatal mortality (NNPD 2003 ) Aims and objectives: To find out prevailing policies and practices on use of Antibiotics among pediatricians in NNS. Methods: Voluntary participants (30 Pediatricians of 15/27 districts) were surveyed by telephonic interview based on set questions by one doctor. Data compiled and analyzed by another Doctor blind to identity of participants. Result: Sepsis screen (S/S) is done by 54% of Pediatricians before starting antibiotic. Blood culture is available to 36%. Perinatal score was considered by 83% for starting antibiotic. S/S was taken to be positive when only one parameter was positive by 30% while 43.3% considered if only CRP was +ve. Clinical experience was basis for choosing antibiotic in 90% and duration of Antibiotic in 56%. GroupBStreptococci was considered a prevailing organism by 54% Conclusions: No standard protocol is followed by Pediatricians while managing NNS .Treatment is based on individual clinical decisions. Disscusion: Compulsory Programs to assess knowledge, updating pediatricians on current management with certification by NNF/IAP with short period validity, setting up regional centers with facility for blood culture and maintaining data base will improve present status. ID/11(P) EVALUATE OCCURRENCE OF TUBERCULOSIS IN CHILDREN LIVING WITH SPUTUM POSITIVE ADULT OF PULMONARY TUBERCULOSIS N L Phuljhele, Virendra Kurrey, Rajendra Binkar C/o. Dr Virendra Kumar Kurrey, Dawada Colony, DI School,Infront Of Reliance Tower ,Pachpedi Naka Raipur ,Chhatishgarh virendra_k7@rediffmail.com Introduction- mortality due to tuberculosis can be prevented with proper screening, diagnosis and treatment. Present study is proposed to propagate screening of all children in families of all adult with sputum positive for AFB by relevant test available locally. This will help in early detection childhood infection Aim & objective: To identify the prevalence of tuberculosis in children of sputum positive adult of pulmonary tuberculosis living in same household if the findings are statistically significant routine screening should be recommended as part of RNTCP Material & method: Prospective, hospital plus community based study during a period of February 2007 to November 2008, inclusion criteria -children 5-15year, should have contact with sputum positive adult, exclusion criteria - children who treated with antitubercular, TB with concurrent immunosupression, Detail history, clinical examination, and investigation done to find out tubercular infection or disease. Observation: We observed that among 218 children 40% children had tubercular infection out of which 23 children had tubercular disease. Data of different parameter is observed and analyzed which is found statistically significant Conclusion – this study argue strongly in favors of routine screening of all children in contact with sputum positive adult of PTB and identify this group of child at high risk who should be screened on a priority basis if there of resources and time to screen all family contact. ID/12(P) FATAL PARALYTIC RABIES DESPITE ADEQUATE PROPHYLAXIS WITH INTRADERMAL VACCINE SCHEDULE Dheeraj Shah, Arvind Jhajharia, Piyush Gupta Department of Pediatrics, University College of Medical Sciences and GTB Hospital, Dilshad Garden, Delhi. shahdheeraj@hotmail.com Introduction: Prompt wound care and the administration of rabies immune globulin (RIG) and vaccine are highly effective in preventing human rabies following exposure. In view of its low price and documented efficacy, intradermal regimen of rabies vaccine has replaced the intramuscular regimen in Government sector catering to the poorest segment of the population. Further, the number of doses have also been reduced from five to four. We report a case of fatal paralytic form of rabies in a child adequately and timely immunized with intradermal rabies vaccine (IDRV) along with rabies immunoglobulin (RIG). Case Report: A 5 year old male child presented to us with complaints of paralysis of left lower limb of one day duration along with history of irrelevant talks and irritability. There was a history of dog bite with laceration and oozing of blood on the involved limb 25 days prior to presentation. Wound cleansing with soap and water was done and the child had received 20 IU/Kg of human RIG on the same day. The child also received three doses of IDRV as per schedule and the fourth dose was due two days after the presentation. At initial examination, the child was found to be conscious but irritable with acute flaccid paralysis of left lower limb. There was no hydrophobia, aerophobia or meningeal signs. Over next day, the paralysis progressed to involve the right lower limb along with deterioration in sensorium. A differential diagnoses of rabies and acute demyelinating encephalomyelitis (ADEM) were considered. MRI of brain showed extensive involvement of the grey matter; bilateral hyperintensities in the hippocampus, thalami, brainstem and basalganglia on T2 weighted and FLAIR images, findings strongly suggestive of rabies encephalitis. Child’s general condition deteriorated rapidly and the child expired after two days. Conclusion: Rabies can occur despite adequate prophylaxis with vaccine and RIG. The settings where intramuscular and reduced dose schedule is being followed, must develop strong mechanisms of follow up and reporting of any adverse events in order to document the efficacy of such a program. ID/13(P) EFFECT OF SIMULTANEOUS THERAPY ON THE SURVIVAL OF HIVTUBERCULOSIS COINFECTED PAEDIATRIC PATIENTS Tripti Pensi, Alok Hemal, Rohit Khurana, Tanushree Baneerjee Associate Professor, Dept of Paediatric &Neonatology, Dr RML Hospital, New Delhi 110001 drpensi@gmail.com; triptipensi@rediffmail.com Introduction: Diagnosis and treatment of TB in HIV infected children in resource limited setting is complicated and challenging. In countries where the prevalence of TB is high, the difficulties become more pronounced. The objective of this study was to assess the outcome of the current treatment guidelines and the effect of HAART on the survival of patients diagnosed with TB along with HIVin resource-limited setting. Material & Methods: An observational, cohort study was undertaken at the paediatric HIV Outpatient Clinic, Dr Ram Manohar Lohia Hospital, New Delhi, India a tertiary care centre. We selected all HIV paediatric patients who visited the HIV clinic with the diagnosis of TB during 2003-2006 and were observed until 31st March, 2010. TB was diagnosed either at the time of enrollment or during the follow-up visits. Clinical and epidemiological data were registered. We compared children who were given HAART along with Anti TB treatment at the time of diagnosis [simultaneous therapy (ST)] and children who completed TB treatment before starting HAART. Survival was assessed by the Kaplan-Meier Method (univariate) and Cox proportional hazards regression model. Results: Among the 298 HIV paediatric patients included in the cohort, 119 (40%) patients had TB. At the time of TB diagnosis, 96 (32%) of them were given HAART along with anti TB treatment (ST). In our cohort, amongst the TB patients 23 (19%) had completed treatment for TB before starting HAART. There were no differences between the two groups regarding basal characteristics, except for a lower CD4 cell count in ST patients. ST therapy was associated with improved survival (hazard ratio 0.35; 95% confidence interval 0.20 to 0.74, P = 0.002). By univariate analysis, survival was also associated with year of TB diagnosis and other AIDS defining conditions. Multivariate analysis including all significant variables revealed ST therapy was a powerful predictor of survival (hazard ratio 0.30; 95% confidence interval 0.14 to 0.68, P = 0.003). After adjusting for other prognostic variables such as age, gender, CD4 cell count at the time of TB diagnosis, by Cox multivariate analysis, ST remained robustly associated with improved survival (hazard ratio 0.32; 95% confidence interval 0.17 to 0.71, P = 0.001). Conclusions: Simultaneous HAART and TB treatment in HIV paediatric patients with TB is associated with improved survival. ID/14(P) HRQOL IN HIV-INFECTED CHILDREN USING PEDSQLTM 4.0 AND COMPARISON WITH NON-INFECTED CHILDREN Tripti Pensi, Alok Haemal, Rohit Khurana Associate Professor, Dept of Paediatric &Neonatology, Dr RML Hospital, New Delhi 110001 drpensi@gmail.com; triptipensi@rediffmail.com Aims : To assess the reliability and validity of Pediatric Quality of Life Inventory 4.0 (PedsQLTM 4.0) in children living with HIV. Also to determine the association of HIV infection,treatment regimens and type of care received on quality of life (QoL) in paediatric patients. Methods: Study was conducted from January to December 2008 at Dr. Ram Manohar Lohia Hospital, New Delhi, India at the HIV paediatric outpatient department (OPD). PedsQLTM 4.0 was administered to 100 HIV-infected and 200 uninfected children aged 8-12 years and their primary caregivers. Results: Internal consistency reliability exceeded 0.70 for both proxy-reported and self-reported scales. Intraclass correlation coefficient demonstrated mainly larger values for parent proxyreport (interval of 0.926 to 0.952 with 95% confidence) than for child self-report (interval of 0.891 to 0.928 with 95% confidence). Factor analysis was performed and it indicated that five factors were extracted from the PedsQLTM 4.0 and these five factors correspond mainly to the five scales. HIV infection was associated with a negative impact on QoL among children with lower scores for physical, school, and emotional functioning and health symptoms. In contrast, uninfected children had lower social functioning scores. Our results showed antiretroviral treatment to be associated with improved QoL among HIV-infected children. We even identified infected children living at home to be at a higher distress of psychosocial functioning and health symptoms when compared with children living in care homes. Conclusions: PedsQLTM is an acceptable and valid measure of health related quality of life (HRQoL) for HIV infected children and uninfected group. Application of this data will be helpful for programmes managers to devise care and support programme for both infected and uninfected children. ID/15(P) ANTIMICROBIAL SENSITIVITY PATTERN IN BACTERIA CAUSING URINARY TRACT INFECTION IN CHILDREN ATTENDING OUTPATIENT DEPARTMENT K. BalaGanesh, Mohan Reddy, Arun Prasath, Padmasani Venkat Ramanan Dept of Pediatrics and College of Pharmacy, Sri Ramachandra Medical College, Porur, Chennai bhangrascores@gmail.com Introduction: UTI is one of the most common infections in childhood. Early diagnosis and appropriate treatment significantly decreases the risk of late serious complications. Knowledge of the common organisms responsible and the sensitivity and resistance pattern of these uropathogens in specific geographical locations is an important factor in choosing suitable antimicrobial treatment. Aim of the study: This study was conducted to evaluate the antibacterial sensitivity pattern of pathogens responsible for urinary tract infections at Sri Ramachandra Medical College and Research Institute, Chennai Material &Methods: Between December 2009March 2010 all children coming to our out patient department with symptoms of UTI were evaluated. Urine culture was performed in urine samples obtained by sterile precautions. Antimicroibial sensitivity was measured by disc diffusion method. Results: Out of 100 children with suggestive symptoms 63 (63%) had a positive urine culture with significant colony count. The most prevalent urinary pathogen was E.coli (39 cases, 62%). Overall the lowest antibiotic resistance of micro organisms was against imipenem (4.65%) and nitrofurantoin (10.25%) and the highest resistance was against ampicillin and cotrimoxazole (84.6% for both). Conclusion: Most organism causing community acquired UTI in suburban Chennai are resistant to the commonly used antibiotics-cotrimoxazole and ampicillin.Therefore the selection of antibiotics and empirical therapy should be based on sensitivity and resistance pattern of uropathogens ID/16(P) CLINICAL PROFILE OF CHILDREN WITH STAPHYLOCOCCUS AUREUS SEPSIS IN A REFERRAL HOSPITAL Ashwani Sood, Mangla Sood. Department of Pediatrics, Indira Gandhi Medical College, Shimla drkumarashw@hotmail.com Aims: Staphylococcus aureus is an important pathogen causing clinical disease in children ranging from non-invasive skin infections to severe, life-threatening sepsis. This study review all children<16years of age with Staphylococcus aureus sepsis (SAS) admitted to paediatric ward of IGMC, Shimla in last 5 years (April 2005 to March 2010) with their clinical presentation and outcome. Methods: Retrospective case study. Results: Out of total 21,600 admissions 4,464 were culture positive. 134 patients (0.6% of total admissions) were identified with SAS. 116 were community acquired,of which 5 (3.7%) were Methicillin resistant Staphylococcal aureus (MRSA).18 were hospital acquired SAS, out of which 12(8.9%) were MRSA. Predisposing conditions were pustules (36%), blunt trauma (12%) and injections (5%). Fever (98%) and respiratory distress (71%) were commonest presentation followed by skin abscess, restriction of limb mobility and joint pain (12% each). Disease spectrum included multifocal disease (67%), pleuro-pulmonary disease (44%), skin and soft tissue infections (28%) , osteo-articular disease (20%). Clustering was seen during hot and humid months. An aggressive search for foci and surgical drainage of infective foci was required in 50% of children. The median length of stay in hospital was 15 (mean 21, SD 22.7, range 2–149) days. Mortality due to SAS was 15.6% compared with the overall mortality for hospital admissions of 3.7%. Morbidity was present in10 (5.9%) children after discharge. Conclusions: SAS is largely community acquired, affects healthy children, is multifocal, and has high morbidity and mortality. Management should include thorough clinical evaluation, appropriate and frequent imaging studies to look for dissemination, antibiotic as per sensitivity pattern in that area and to drain and debride foci to minimise morbidity and mortality. ID/17(P) EFFICACY OF INTRAVENOUS ANTI D (IV ANTI D) IN MANAGEMENT OF REFRACTORY THROMBOCYTOPENIA IN DENGUE HEMORRHAGIC FEVER (DHF) Kharya G, Katewa S, Sachdeva A, Yadav SP Pediatric Hematology Oncology Unit, Center for Child Health, Sir Ganga Ram Hospital, Delhi, 110060 gauravkharya@rediffmail.com Introduction: DHF is a potentially lethal complication of dengue fever. Bleeding in DHF is due to thrombocytopenia and/or coagulopathy. Previous study by De Castro et al showed efficacy of IV Anti-D for management of thrombocytopenia < 50000/mm3 in DHF. We present our experience of usage of IV Anti-D in DHF with refractory thrombocytopenia. Aims and objectives: To test efficacy of IV Anti-D for management of refractory thrombocytopenia in DHF. Methods: This is a retrospective study of children with DHF (WHO criteria). Children were managed as per WHO guidelines. IV Anti-D@50-75 mcg/kg was given to children with refractory thrombocytopenia <10000/mm3 defined as no increase in platelet counts 1 hour after administration of platelet concentrate. Results: There were 5 patients in this study with M:F ratio of 1.5:1. Average age at presentation was 10.2 years. Mean PC before administration of IV antiD was 6800/mm3. Average number of platelet units given to each patient prior to anti D administration was 20. Mean PC at 24, 48 and 72 hours post IV Anti-D were 33600, 44600, 79000/mm3 respectively. Average increase in PC at 48 hrs after administration of anti D was 37800/mm3. Average duration of hospital stay post anti D was 3.8 days. Average drop in hemoglobin after administration of anti D was 2.28 gm/dl. No major adverse effects were noted. Conclusion: Intravenous Anti D is safe and effective in management of severe refractory thrombocytopenia in DHF. ID/18(P) CONGENITAL VARICELLA SYNDROME VS CONGENITAL VARICELLA INFECTION M. Jhancy, CH.N.Raju, R.P.Bindu, P.V.Subba Rao Department of pediatrics, R.M.C, Kakinada, A.P jhansimalay@yahoo.com Case – 1: 16 days neonate presented to pediatric op for URI. On examination child had hypopigmented and hypoplastic skin over neck, upper&lower limbs. Mother had primary varicella infection at 16 weeks of pregnancy. Child diagnosed as having congenital varicella syndrome. CONGENITAL VARICELLA SYNDROME Case-2 Newborn admitted with respiratory distress. Mother had primary varicella infection 5days prior to delivery. X-ray chest showed pneumonia. On 10th day he developed vesicular rash, general condition deteriorated, expired on 15th day. Blood for varicella IgM became positive. NICU Postgraduate acquired varicella infection on 14th day. Child considered expired due to varicella pneumonia as a complication of congenital varicella infection. CONGENITAL VARICELLA INFECTION CXR SHOWING PNEUMONIA Discussion: Primary varicella is highly communicable with an attack rate of 90%. 10% of women of childbearing age are still susceptible to varicella and thought to occur 1 in 10000, (0.01%) of all pregnancies. In first 20 weeks of pregnancy maternal infection can result in the congenital varicella syndrome, rare complication of maternal varicella, which includes limb hypoplasia, microcephaly, cataracts, growth retardation and skin scarring. Maternal infection from 5 days before to 2 days after delivery is associated with a significant risk of severe neonatal infection, with dissemination which can cause serious infection of the lungs and brain This type of infection referred to as neonatal varicella with 30% mortality. Diagnosis by Detection of VZV specific IgM MANAGEMENT: Infants whose mothers develop chickenpox (but not zoster) from 5 days before to 2 days after delivery should receive VZIG. ID/19(P) RAT BITE FEVER: A CASE REPORT Manish K. Arya, Payal Shah, Pallavi Saple, AD Rathod, Rizwan, Praneet Dept. Of Paediatrics, Grant Medical College And Sir J.J. Group Of Hospitals, Mumbai 8. manjioo7@yahoo.co.in Introduction: Rat Bite fever is a rare disease by rodent bites associated with infection by Streptobacillus moniliformis & Spirillum minus presenting with Fever,Migratory Polyarthritis,Rash. Case Report: Three months old female child presented with sudden onset, high grade continuous fever with erythematous rash over palms & soles since 3 days. Mother complained of bilateral knee and ankle swelling & excessive crying on handling. Child had history of rat bite over face 15 days back for which she received oral antibiotic, bite healed completely without secondary complications. On Examination baby was febrile, tachycardia with HR 180/min, pallor, bilateral pedal edema & Knee joint swelling with tenderness.Maculopapular erythematous rash was present on extremities involving palms & soles. Healed rat bite marks were seen on the face near left eye & nose. Baby had hepatomegaly with Liver span of 12 cms. There was no lymphadenopathy. Rest Systemic examination was normal. CBC showed Hb of 6.8 gm/dl, TLC 13,700/mm3, platelets of 2,64,000/mm3 with microcytic hypochromic picture on smear. LFT, RFT, Sr.Electrolytes were normal. CSF had 10 cells with 90% lymphocytes, 10% polymorphs, proteins 68 mg%, sugar 52 mg%. CSF culture was negative. Blood culture and Culture for Streptobacillus moniliformis was negative. USG abdomen had mild hepatomegaly. 2 Decho was normal. Baby responded to IV Penicillin G for 14 days, rash disappeared on 6th day of illness & knee swelling & pain subsided after 10 days. So based on clinical features diagnosis of rat bite fever was considered. ID/20(O) METHICILLIN RESISTANT COAGULASE NEGATIVE STAPHYLOCOCCAL SEPTICEMIA IN NEONATES – CLINICAL EXPERIENCE OF A TERTIARY CARE HOSPITAL M.R.Savitha, G.M Kumar, B.L Venugopal Department of Pediatrics, Mysore Medical College and Research Institute, Mysore drsavithamr@yahoo.com Introduction: Methicillin resistant coagulase negative Staphylococci(MRCoNS) is the most frequent nosocomial blood stream infection in neonatal intensive care unit(NICU). Indwelling central vascular catheters are the greatest risk factor for MRCoNS sepsis AIMS AND OBJECTIVES: To study the incidence, clinical features and outcome of MRCoNS septicemia amongst neonates admitted to NICU Materials And Methods: Neonates with MRCoNS septicemia admitted to NICU from January 2010 to July 2010 were studied. The diagnosis of MRCoNS septicemia(ruling out contamination) was defined by clinical features of septicemia with positive blood culture for MRCoNS which was performed using a defined protocol Results: 32 cases(Male:female=2.2:1) of MRCoNS were isolated with an incidence of 4.25%. 29 cases had early onset sepsis. 26 were term neonates. 12 cases(37.5%) were low birth weight. None of them were on central vascular catheters. They were only on peripheral vascular catheters and on nasogastric tube. The most common presentations were lethargy, refusal of feeds in 7 cases each(21.88%), feed intolerance in 5 cases(15.63%), abdominal distension and tachypnea in 4 cases each(12.5%). 24 cases(75%) had positive C-reactive protein. 18 cases(56.25%) had band neutrophil ratio>0.2. Thrombocytopenia was seen in 3 cases. 31 cases were sensitive to Linezolid, 10 to Clindamycin and 4 to Ciprofloxacin. None of the cases died. Culture of hands of all the NICU personnel(except one) and NICU equipments yielded MRCoNS with similar sensitivity pattern Conclusions: MRCoNS is a nosocomial nursery infection Though mortality is uncommon in MRCoNS septicemia, there can be significant morbidity which may prolong NICU stay. ID/21(P) REEMERGENCE OF PERTUSSIS IN KERALA Abraham Paulose, Isac Mathai, Mathew Ma, C Chitralekha Dept. of Pediatrics, Malankara Orthodox Syrian Church Medical College and Hospital, Kolenchery, Kerala drabrahampaulose@hotmail.com Introduction: In India, only 44180 cases of Pertussis were reported in 2009, clearly an underestimation of the true incidence of the disease. Aims & Objectives: To describe the clinical presentation and course of pertussis in hospitalised children. Design: Retrospective study. Subjects: Children admitted to Malankara Orthodox Syrian Church Medical College, Department of Paediatrics, in Kerala with a clinical diagnosis of pertussis from January 2009 to August 2010. Results: A total of 23 cases were identified with clinical pertussis (mean age, 58 months old; range, 2 to 132 months old). All the described patients had prolonged paroxysmal cough (100%), lasting for 4 ± 3.6 weeks. 16 (70%) patients had the classic whoop. All three (13%) infants had apnoea. Five (22%) patients had severe pneumonia secondary to pertussis. The mean WBC count was 19,837 cells/cmm and the lymphocyte count was 70± 12%.Twenty (87%) had received 1 dose of DPT & 6 (26%) 5 doses of DPT. Conclusions: There is an increase in pertussis cases both in young infants and adolescents in Kerala, despite high vaccination coverage. With pertussis continuing to pose a serious threat to infants and greatly affecting adolescent, there remains a need to (a) Increase the awareness of the lay public and among doctors as to the growing pertussis problem (b) Standardize diagnostic techniques (c) Implement newer acellular low dose vaccine strategies to enhance its control. ID/22(P) EARLY DIAGNOSIS OF CNS TUBERCULOSIS WITH CSF PCR IN A PATIENT WITH NO ETIOLOGICAL OR BIOCHEMICAL EVIDENCE OF TUBERCULOUS MENINGITIS Tanmay Toteja,Vikas Bhambhani,Jacob Puliyel,Suman Lata Department of Pediatrics,St. Stephen's Hospital,Tis Hazari,Delhi-54 Introduction / Background: In stage I of TBM no cytological or biochemical changes are seen in the CSF, though bacilli are present. Early diagnosis can be made by CSF PCR for TB. CSF PCR positivity for TB without evidence of TBM or systemic tuberculosis has been reported in 5 cases of HIV positive individuals. We here report a case of focal seizures, granuloma, a normal CSF picture and culture, HIV ELISA negative but PCR CSF for TB positive CASE REPORT: A 3 year 9 month old boy with left complex partial seizures ; no history of Koch’s contact ; an unremarkable clinical examination , no neurological deficit, no features of raised ICP and meningism. CECT HEAD – Ring-enhancing lesions with perilesional edema; no evidence of abnormal meningeal enhancement or hydrocephalus. ESR 8 mm in I hour, Mantoux test 15 x 10 mm CSF – Normal cytology and biochemistry; Gram’s and AFB staining and culture inconclusive HIV ELISA – negative; Chest X- ray – Normal; PCR ASSAY for TB - POSITIVE Treatment – ATT (2HRZE + 10 HRE) with steroids and anti-epileptics RESULTS: On follow up – No seizures and resolution of the granuloma over 1 year on CECT head. DISCUSSION: Granulomatous lesions are common findings in a patient with focal seizures. Neurocysticercosis and tuberculoma being the most common differential diagnosis of the above in the Indian subcontinent. Gold standard for diagnosis is stereotactic biopsy and histology. In early TBM diagnosis can be established by CSF PCR ASSAY before cytological or biochemical changes are seen in CSF thus preventing extensive damage and neurological sequale. CONCLUSION: Early diagnosis of tubercular etiology in Granulomatous lesions can be established by CSF PCR ASSAY ID/23(P) CONGENITAL TUBERCULOSIS Rajiv Kumar, Nomeeta Gupta Department of Pediatrics, Batra Hospital & Medical Research Centre, New Delhi-110062. Congenital tuberculosis is a rare disease with a high mortality and less than 300 cases have been reported so far in the literature. Only about 10 cases reported so far in India. A timely diagnosis is difficult because the symptoms in the infants are often non-specific and mothers are often asymptomatic. A primary complex in the liver can be regarded as strong evidence of congenital tuberculosis.We report a case of congenital tuberculosis diagnosed by liver biopsy in a 2 months old infant presented with acute abdomen. Case Report: A 8 weeks old infant presented with fever, excessive cry, vomiting, gradual abdominal distension and refusal of feeds for five days. The child was sick, toxic-look, irritable and had mild pallor with no icterus or superficial lymphadenopathy. Systemic examination revealed abdominal distension, hepatosplenomegaly, reducible umbilical hernia and right hydrocele. Late onset septicemia, intrauterine congenital infections and intestinal obstruction with paralytic ileus were considered in the differential diagnosis. Laboratory investigations revealed Hb 8.1 gm%, TLC 16600/mm3 with 73% neutrophils, 24% lymphocytes, 2% monocytes and 1% eosinophil, ESR 58mm and platelet count 80,000/mm3. PT and PTT were normal. Liver enzymes were elevated. Serological tests for TORCH, syphilis and HIV were negative. Alpha- fetoprotein was normal. Hepatitis B surface antigen and hepatitis C antibody were negative. Chest X-ray showed ill-defined homogenous opacity in the right paracardiac region. Abdominal X-rays revealed gaseous distension of bowel loops. Abdominal ultrasound revealed hepatosplenomegaly, portal adenopathy and minimal free fluid in the Morrison’s pouch. CT abdomen revealed ascites with hepatosplenomegaly with mutiple hypodense lesions in liver and spleen with necrotic retroperitoneal or intra-abdominal lymphadenopathy. Early morning gastric aspirate smear for AFB on consecutive three days and tuberculin test were negative. Miniexploratory laparotomy was done because of his worsening clinical status on 7th day of admission. Liver and retroperitoneal lymph nodes biopsy showed multiple epitheloid cell granulomas with occasional Langhans’ giant cells and central necrosis in few of them. Antituberculous treatment was started on 8th day of admission. The family screening for tuberculosis was negative. Endometrial biopsy in the asymptomatic mother confirmed the source of infection and the perinatal onset of illness. ID/24(P) CALVARIAL TUBERCULOSIS Neeraj Awasthy 123, Anandkunj, Vikaspuri, New Delhi, 110018 Calvarial tuberculosis is a very rare entity scantily described in literature. It forms 0.2-1.3% of the bone tuberculosis. This entity is rare even in the endemic areas for tuberculosis thus necessitating the awareness of the lesion so as to enable diagnosis. Primary Calvarial tuberculosis with no evidence of tuberculosis is still rarer of these cases. We describe six cases of Calvarial tuberculosis. The relevant clinicoradiological features and management are discussed. A high index of suspicion and awareness of this condition may lead to more cases being diagnosed early. ID/25(P) PEDIATRIC MDRTB – FOUR CASE REPORTS FROM BELUR ESI TB HOSPITAL Sumit Kumar, Amit Kumar Poddar, Kunal Dutta, Pradip Bhattacharya Belur ESI TB Hospital, Sapuipara, Bally, Howrah, West Bengal – 711227 Introduction: MDRTB is a ticking time bomb which is not being treated by RNTCP. Out of 200 beds in our hospital we have 16 in 3 wards reserved for MDRTB. These beds are always occupied. Materials and Methods: After sputum is persistently AFB positive for 5 months, sample is sent for culture in LJ Media and MDR Regimen is started. Drugs available are: Kanamycin, PAS, Cycloserine, Ethionamide, Sparfloxacin/Levofloxacin/Ciprofloxacin. Case Reports: Four Children below 18 years were treated successfully between 1999-2005. Sahazad (14 years) admitted for 5 years was initially treated by Streptomycin PZA, Ciprofloxacin and Ethionamide for 2yrs 4mths. Then due to fall and rise of Sputum positivity, he was treated with Kanamycin, Sparfloxacin, Cycloserine, Dapsone and Clofozimine for 2yrs 2mths and cured. Nityananda (10 yrs) admitted for 2yrs 4mths, Robin (17yrs) admitted for 2yrs 6mths, Pavan (16yrs) still admitted, were treated with Kanamycin, PAS, Ethionamide, Cycloserine, Sparfloxacin/Levofloxacin/Ciprofloxacin. All the cases were HIV and HBsAg negative. ADR encountered were hypothyroidism, psychosis and gastritis. Conclusion: MDRTB should be treated institutionally and under supervision to prevent an epidemic if not a global pandemic. ID/26(P) MILIARY TB – AN UNUSUAL PRESENTATION Lalitha Kailas, B. Vijayakumar, Kiron S. Professor & HOD, Dept. of Pediatrics, SAT Hospital, Medical College, Trivandrum Miliary TB usually presents in infants and yound children with fever and respiratory symptoms and signs. We present a 6 ½ year old child who presented with PUO but no respiratory complains. The fundus examination showed choroid tubercles and the repeat Xray showed miliary mottling. ID/27(P) EFFICACY OF HIGHLY ACTIVE ANTIRETROVIRAL TREATMENT (HAART) IN VERTICAL HIV INFECTED CHILDREN. Sanjiv Nanda, Ashish kumar Ho No 11/8 F M, Medical Enclave, PGIMS, Rohtak drsanjivnanda@gmail.com Objective: To evaluate the efficacy of highly active antiretroviral treatment (HAART) in vertical HIV infected children. Material and methods: This study was conducted on thirty vertically transmitted HIV infected children aged 20 months to 156 months, at ART centre of a tertiary hospital. Every patient at enrolment was categorized into WHO clinical staging and revised immunosuppression staging. Fixed dose combination of HAART was given based on patient's weight. Baseline investigations were repeated after six month of HAART. Observations: Presenting features were weight loss (90%), generalized weakness (80%), fever (76.7%), diarrhoea (73.3%), cough (36.7%), hepatomegaly (50%), generalized lymphadenopathy (53.3%), splenomegaly (40%), molluscum contagiosum (3.3%), herpes zoster (3.3%) and tuberculosis (3.3%) . The mean hemoglobin at enrolment was 9.41.3 which increased to 11.050.93 after six month of HAART (p<0.05). The mean absolute lymphocyte count , mean CD4 count and mean CD4 cell percentage 27201314, 226.11, 95.7 respectively, increased to 2774959, 584335 and 2213 after 6 month of therapy. The change in absolute lymphocytes count was not significant (p>0.05), however the increase in CD4 count and mean CD4 cell percentage was significant (p<0.05). Adherence to HAART was found more than 95% in all patients. Use of FDC resulted in better tolerance, simplification of treatment, reduction in number of pills and thus better adherence. Adverse effects in form of skin rashes was observed only in one patient, which resolved by itself and HAART was not stopped. Conclusion: HAART is safe and significantly improves the clinical as well as immunological outcomes in perinatally infected HIV positive children. ID/28(P) SPINA VENTOSA: AS A PART OF DISSEMINATED TUBERCULOSIS Payal Shah, Manish K. Arya, A D Rathod, Pallavi Saple, Ravi Bharadwaj Dept. Of Paediatrics, Grant Medical College And Sir J.J. Group Of Hospitals, Mumbai 8. manjioo7@yahoo.co.in Introduction: The name of “spina ventosa” being given to TB dactylitis of the short bones of the hand because of the radiographic features of cystic expansion of the short tubular bones. Case Report: A 11 year old boy presented with history of fever and difficulty in walking due to pain in left lower leg since 15 days. He also gives history of loss of appetite and loss of weight since 2 to 3 months. On examination child was having low grade fever with stable vitals. He was undernourished. There was tenderness over shin of left tibia. On investigation CBC showed anaemia with raised ESR. MT was significant. A chest radiograph showed right upper hilar adenopathy consistent with pulmonary tuberculosis. CT thorax and abdomen showed necrotising lymph nodes. CT of left tibia showed features of TB osteomyelitis. Patient was started on 4 drug AKT. But over a period of 6 months patient develops a painless mass overlying the fourth finger of the left hand and dorsum of right hand. A radiograph of the left hand showed a cystic, expansile lesion of the distal portion of the middle phalanx of the right ring finger and similar swelling over 3rd metacarpal bone of right hand. A large soft tissue mass surrounded the bone lesion. This was diagnosed as tuberculous dactylitis based on the imaging findings and the coexisting diagnosis of pulmonary TB. ID/29(O) CLINICAL PROFILE OF DENGUE FEVER IN IGICH Ameet Kumar S M; Sanjeeva; Basavaraj G V; Shivananda Dept of pediatrics, IGICH, Bangalore ameet_managuli@yahoo.co.in Introduction: Dengue fever is arthropod borne viral fever caused by 4 antigenic types of dengue viruses with varied spectrum ranging from simple dengue fever to fatal dengue hemorrhagic fever & dengue shock syndrome. The incidence has increased drastically in the recent past creating fear among people. Aims & Objective: To study the varied clinical presentations & response to treatment & outcome in children admitted in tertiary referral centre IGICH . Material & Method: All cases of suspected dengue fever according to WHO criteria admitted in IGICH over a period of 4 months i.e from may 2010 to august 2010 were studied prospectively with respect to varied clinical presentation, response to treatment & outcome. Results: Out of 362 cases (55.8% Male , 44.2% Female ) admitted over a period of 4 months from May 2010 to August 2010, spectrum of disease include Dengue fever ( 41.7% ), Dengue shock syndrome ( 32.8% ) & Dengue Hemorrhagic Fever ( 3.3% ), maximum cases were seen in age group of >5 yrs ( 69.8% ) with most common manifestation being Fever ( 100% ) with mean duration of 3-5 days ( 41.4% ), followed by pain abdomen ( 53.8% ), Puffiness of face ( 42.8% ), rash in only 4.9% cases, Mucosal bleeding ( 3.6% ) and Altered sensorium (2.7% ), with most common clinical observation being tender Hepatomegaly ( 57.4% ), Flushing (52% ), Puffines of face ( 42.8% ), Ascitis ( 49.6% ), Pleural effusion ( 45% ), hypotension ( 32.8% ), edema ( 25.6% ). All cases were treated according to recent WHO protocol 2009. Out of 362 cases 38.6% cases were treated with Plan A i.e only oral fluids ( ORS ), 56.9% with Plan B i.e required I V fluids ( 5-10ml/kg/hr ), 4.5 % with Plan C i.e I V Fluids 10->20 ml/kg/hr. 6% treated with Lasix infusion for respiratory distress with acute lung injury to prevent ARDS, 1.6% with Whole blood, 1.1% with FFP, 0% with Platelet transfusion, 2.2% needed ventilator support. During follow up, fever lasted for < 3days in 57.7%, hypotension resolved in with only fluid therapy either oral or intravenous within 2 days, itching over palms & soles were observed in 23% during recovery phase, Mean duration of stay being 3-5 days in 57.4% . complications like ARDS ( 4.6% ), encephalitis ( 0.8% ) were observed and Death in 1.1% cases. Conclusion: Though Dengue fever is a life threatening disease , It can be managed effectively avoiding complications with early clinical detection & proper fluid management. ID/30(P) HAND- FOOT- AND- MOUTH DISEASE Ajit Chhetri, Niru Chhetri, Arup Sengupta c/o B.Bhattacharjee, Sargam Apartment, Behind Soudamini Apartment, Nivedita Road, Pradhan Nagar, Siliguri. 734003. drjeetsingh@yahoo.co.in Hand, foot and mouth disease (HFMD) is a distinctive rash syndrome caused by Coxsackie virus, a member of non polio enterovirus. It is an illness which is perhaps common but highly under diagnosed in Indian children and to our knowledge only few cases have been reported. In an epidemic in 2003 that occurred in Calicut, Kerala, the disease exclusively affected children of age seven months to eight years, during October and continued till February of the following year. (1) We are reporting here 28 cases of HFMD. Case report: From 3 rd week of August 2010 till the end of September 2010 (coinciding with heavy rainfall in this region, including North Bengal), many children were brought by parents with history of irritability, excessive crying , refusal to feed and, rashes on hands and feet. The age group ranged from 7 month to 3.5 years, averaging approx 2 yrs. There were 15 male and 13 female children . The spectrum of clinical presentation is as following, figure in bracket being percent of children : Irritability (100), excessive crying (64), increased salivation (86), refusal to eat (93), rashes on hands & feet (100), rashes on buttocks & groin (21),vesicles on pharynx & palate (71),vesicles on tongue and buccal mucosa (29), fever more than 1010 F (29), fever less than 1010 F(64) and vomiting(29). Please see figures 1 to 5 below. Investigations done on 3 children with fever, vomitings and excessive crying revealed normal blood counts and normal liver function tests. Final diagnosis of HFMD was made by the history & physical examination demonstrating the characteristic vesicles on the hands, feet & oral cavity. With re-assurance to parents about the mild nature of the disease, calamine lotion and analgesics (paracetamol and / or ibuprofen), all recovered by 6 – 9 days, average 7.5 days, with no complications. Figures. (1) Figure (2) Figure (3) Figures 1 to 5 depicting rashes over hand, foot , buttock and oro-pharynx. Discussion: HFMD is most frequently caused by coxsackie virus A 16 and can also be caused by enterovirus 71 , coxsackie A viruses 5, 7, 9 and 10; and coxsackie B viruses 2 and 5. It is usually a mild illness. (2,3,4)It spreads from person to person through throat and nasal discharges, saliva, fluid from blisters, or the stools of an infected person. Incubation period ranges from 3 to 7 days. The most important risk factor is age. The infection occurs most often in children under age 10 but can be seen in adolescents and occasionally adults. The outbreaks occur most often in summer and early autumn. (3,4) The oropharynx is inflammed and contains scattered vesicles on the tongue, buccal mucosa, posterior pharynx, palate, gingiva and / or lips. These may ulcerate, leaving 4 – 8 mm shallow lesions with surrounding erythema. Maculopopular, vesicular and / or pustular lesions may also occur on the hands and fingers, feet, and buttocks and groin; hands are more commonly involved than the feet. Lesions on the hand and feet are usually tender vesicles varying in size from 3 to 7 mm and more common on dorsal surfaces but frequently also occur on palms & poles.(2) HFMD caused by enterovirus 71 is frequently more severe than due to coxsackie A16 with high rates of neurologic diseases, fulminant pulmonary edema and high mortality especially in young children.(2,5) There have been reports of fingernail and toenail loss occurring mostly in children within 4 weeks of their having HFMD, with nail growth resuming without medical treatment.(6) There is no specific treatment for HFMD. Good hygiene practices especially hand washing and avoiding close contact (kissing, hugging) with persons with HFMD can lower the risk of infection. ID/31(P) INCIDENCE AND CLINICAL PROFILE OF DIABETES MELLITUS IN HIV POSITIVE CHILDREN Harmeet Singh Arora, Kirandeep Sodhi, M Ganguly, M K Behera Dept of Pediatrics, Military Hospital, Roorkee, Uttarakhand – 247667 hsarora18@gmail.com Introduction : Diabetes mellitus is a very rare presentation of HIV infection, especially in children. It is usually attributable to highly active antiretroviral therapy (mainly protease inhibitors), which through complex mechanism increase the insulin resistance. HIV per se is also known to cause Diabetes mellitus. Very limited data exists on incidence of Diabetes in children with HIV infection. We report the incidence of this endocrinal abnormality in pediatric HIV infection. Aim: To study the incidence and clinical profile of Diabetes mellitus in HIV positive children. Materials & Methods: Sixty two confirmed HIV positive children, who presented to a tertiary care hospital, over a period of 24 months were extensively studied for their clinical and laboratory profile, including blood sugar. Complete blood sugar profile was performed in children who were found to have hyperglycemia on initial evaluation at the time of presentation. Diabetes mellitus was defined as per standard definition by WHO. Results: Five (8.3%) children were found to have diabetes mellitus. Two out these had symptoms (which were noted retrospectively) suggestive of Diabetes including polyuria and polyphagia. No past record of blood sugar levels was available. Three were girls and two boys. None of them had family history of Diabetes mellitus upto last three generations of the family tree. Both parents who were also HIV positive, had normal blood sugar. Mean age of presentation was 9.8 years (Range 8-12 years). One child was on protease inhibitor as a component of HAART. Rest four were not on HAART or being treated for Pnemocystis carinii pneumonia. None of them was obese. All had normal serum cholesterol (lipid profile could not be done) and other biochemical parameters. Mean CD4 count was 210/ cumm (156-311cumm) in these diabetic children, which was lower as compared to other non diabetic subjects in the study (p<0.05). All of them had high viral load, with a mean of 7.6 lac copies/ml (5.4-9.1 lac copies/ml). The disease severity as per CDC classification was stage B in two and C in three cases. Two children were in stage 3, and three in stage 4 of revised WHO classification. Conclusion : Incidence of Diabetes mellitus in HIV positive children is very low. Although it is usually drug (HAART) induced, HIV per se can cause diabetes, through a complex interaction, even in the absence of usual risk factors. It is more likely to occur in advanced disease, with low CD4 count, and high viral load. ID/32(P) THE INFLUENCE OF NUTRITIONAL STATUS ON THE RESPONSE TO HAART IN HIV-INFECTED CHILDREN AT REGIONAL ART CENTRE IN NEW DELHI Aaradhana, Divya Jain, Tripti Pensi Department of Pediatrics, Dr Ram Manohar Lohia Hospital, New Delhi draaradhna@gmail.com Introduction: While the impact of HAART on growth in children is well established, the influence of prior nutritional status on the response to HAART is not well known. Methods: A retrospective study was conducted on 88 children attending the ART centre of Dr Ram Manohar Lohia Hospital in New Delhi. Patients were divided into 3 groups (normal, moderately underweight, and severely underweight) based on weight-for-age z-scores. Age, weight, CD4 cell percentage were recorded at the initiation of HAART and after 24 months of therapy. Data were analyzed using t-tests, chi-square tests, and one-way ANOVA Results: At baseline, 24% of children were normal weight, 23% moderately underweight and 50% severely underweight. All three groups had almost similar average CD4 counts. After 24 months of HAART, mean CD4 cell percentages increased significantly in all 3 groups. Conclusions: Underlying malnutrition does not adversely affect immunologic response to HAART in HIV-infected children. Underweight children exhibit an equally good response to treatment as their well-nourished peers. ID/33(P) CONGENITAL PLASMODIUM VIVAX MALARIA MIMICING SHOCK- A CASE REPORT M.Simhachalam Babu,D.Satish,Abani Kanta Sahu, Ratan ku Dash,P.Sudarsini Alluri Sitarma Raju Academy of Medical Sciences, Eluru, Andhra Pradesh. dr_abani@rediffmail.com SEPITIC Introduction: Diagnosis of congenital malaria in few reported cases is delayed because of atypical presentation and more importantly its least suspicion as a differential diagnosis. A delay in diagnosis often leads to its severe complications. Case Report: A 21 days old male baby ,born at term by LSCS to a primi mother ,birth weight 2.5 kg and doing well upto 14days of life was admitted with complain of intermittent high grade fever since then and refusal of feed with lethargy of 24 hrs duration being treated with out proper treatment documentation .On examination was lethargic,pale,icteric and in hypotensive shock.AF was normal with a normal Liver span & Gr II firm splenomegally,also had a normal lungs air entry with a GrII flow murmur. A working diagnosis of LONS in septic shock was made and resuscitated with fluid bolus+dopamine drip+temporary oxygen. Samples for sepsis work up including blood and urine culture were sent and empiric IV antibiotics started. At this point laboratory reports showed B positive blood group, Hb-10.4g%,TLC-5,700,N38L59M2Band1%,TPC 45,000 ,retic count 1.5%.and a microcytic hypichromia with mild anisopoikilocytosis blood picture with RBCs containg trophozoites of plasmodium vivax was reported by the Pathologist.CRP 6 micog/dl .TSB 13.0,direct 11mg/dl.Blood urea 47mg/dl,creatinine 0.6mg/dl,sodium 135,potassium 4.8meq/dl. Next day CSF analysis-normal .The Osmotic fragility was normal.High fever persisted over next 48 hrs while awaiting antibiotic response .On D3 of admission a repeat hemogram to monitor blood counts suggested Hb 7.8g%,TLC 5,400,TPC 26,000 with reporting of occasional RBC containing Trophozoite of plasmodium vivax ,subsequently confirmed by a positive trophozoite of vivax in a smear for Malaria parasite.A directed history for maternal malaria suggested an febrile episode with chills & rigor of 2-3 days in her at 4th month of gestation without recollection of any antimalarial use. She was tested negative for malaria parsite in smear with a negative malarial antigen test. This alerted us to revise our diagnosis to complicated congenital plasmodium vivax malaria.He was transfused with 20ml/kg packed cells in two settins,and started on chloroquin in standard regimen. By 36 hrs of this baby became afebrile and put on direct breast feed and discharged on D6 of admission after getting the negative culture reports. Conclusion: Antimalarial antibodies in the pair was not done due to feasibility which would have confirmed the diagnosis of congenital malaria. Still this case reemphasizes importance of keeping congenital malaria as a differential diagnosis particularly while evaluating neonates with suspected sepsis ,more so in presence of anemia, jaundice and splenomegaly to prevent its severe complications. ID/34(P) CEREBRAL MALARIA- CLINICAL FEATURES AND OUTCOME N.L. Phuljhele, Gajanan Shriram, Hemant Kumar. Kanchanganga phase-II, Danganiya, PO. R.S.University Raipur (C.G.) 492010 drnsph@gmail.com Introduction: Cerebral malaria collectively involves the clinical manifestations of Plasmodium falciparum malaria that induces changes in mental status and coma. It is an acute, widespread disease of the brain which is accompanied by fever. The mortality ratio is between 25-50%. If a person is not treated, it is fatal in 24-72 hours. Aim: To study the clinical features and outcome in the cases of cerebral malaria Methods: Total 25 cases of cerebral malaria included in this retroprospective study. The clinical features of the patient were observed and final outcome was documented Results: male-16,female-9) The clinical presentation included; fever-96%,pallor60%,hepatomegaly-48%,splenomegaly-40%,headache-36%, general body pain-32%, anorexia16%, shivering-36%, sweating-28%, abdominal-8%, malaise-4%, nausea-4%, refusal of food4%, diarrhoea-20% and vomiting-20%. Out of 25 cases 13 cases were malaria antigen test and/or peripheral smear positive where Pl.vivax was seen in 3, Pl. Falciparum in 9 cases and mixed type in 1 patient. Rest of the patients were diagnosed on the basis of strong clinical suspicion after ruling out the other causes of unconsciousness. Treatment given included anti malrial medicines like quinine in 11, artimisinin derivative in16, clindamycin in 9, doxycycline in 2 cases. Patients also required ancillary treatment in form of Red blood Cell transfusion in 5, whole blood transfusion in 5, Fresh Frozen Plasma in 1case. Eleven out of 25 patients did not survive while 14 were discharged. Conclusion: Cerebral malaria is a fatal disease having a very high mortality ratio compared to other complicated forms of malaria. ID/35(P) RICKETTSIOSES: TIP OF THE ICEBERG Merriyet.M.B,Lalitha.M,Rajshekar Murthy,Basavaraj.G.V,Shivananda Department Of Pediatrics, Indira Gandhi Institute Of Child Health , Karnataka merriyetmb@yahoo.co.in Introduction: Child with fever and rash , too often is labeled as a case of viral exanthematous illness by the treating doctor .This diagnosis may hold good in most cases and no active therapy is indicated. There are however several non viral illnesses,that present with rash and fever , which are amenable to treatment and untreated are associated with significant morbidity and mortality -Rickettsioses is one such entity. Aims & Objectives: To evaluate the clinical spectrum, laboratory profile,response to treatment,complications & outcome of rickettsial infection. Methodology & Materials: This is a 1 year prospective study,conducted in Indira Gandhi Institute of Child Health ,Bangalore from July 2009 to August 2010 in children admitted with fever, suspected of rickettsioses. Results: Total of 95 patients were enrolled.Epidemiology –Chikkaballapur & Bangalore-20% each. Seasonal incidence -July to January (peak incidence- September to October),male:female- 1.7 : 1,age 5-10yr-45.7%, ,duration of stay(4-7 days)- 65.9% .Of the spotted group, fever <=1wk (21%), fever->1wk (79%) , rashes (52%) ,edema-6.6%, CNS manifestations (33.3%),myocarditis(6.6%),stroke like syndrome (3.3%) and death(6.6%).Of the scrub typhus group,fever>1 week(95% ), rashes(15.3%) edema(83%), hepatosplenomegaly(70.7%),CNS manifestations (30.7%) and death(6.1%).56.5% had onset of rash by D3 of fever,clinical triad(fever,headache & rash- 52.6%).LAB-TC >11,000-87%,neutrophilia(>50%)86.1%,thrombocytopenia-60%,CRP positive-94%,Hyponatremia-56.8%,elevated transaminases-72.6%,hypoalbuminemia-91.3%, triad(leucocytosis,positive CRP&hyponatremia)-53.6%, CSF- 31.5% had 10-50 & 100- 500 cells each,max-160 cell,100% - lymphocytes>50%,89.45%- normal glucose, protein 50-100mg/dL42.1% . weil felix test -65 cases were scrub typhus (OX K) and 30 cases were spotted group (OX2&OX19).Response to doxycycline- 24-48hrs- 90%, >48hrs- 10% Conclusion: A child with fever, with or without rash,edema,hepatosplenomegaly, thrombocytopenia,hypoalbuminemia & hyponatremia must prompt us to think beyond the usual suspect of viral exanthematous fevers.It poses diagnostic difficulty and delay in treatment,which causes life threatening complications.Dramatic response to doxycycline is seen if instituted early,hence empirical treatment is justified in endemic areas. ID/36(P) PLASMA OXIDANT STATUS IN CHILDREN WITH SEVERE MALARIA Nidhi Narsaria, SP Mishra, RS Upadhya, B.K.Das C/o. Prof and Head Department of Pediatrics, IMS,B.H.U , Varanasi - 221005. profbkdas@yahoo.co.in Objectives: The present study was done to evaluate oxidants (malondialdehyde, protein carbonyl, nitrite) & antioxidant levels (superoxide dismutase, glutathione peroxidase, ceruloplasmin, copper & zinc) in plasma in children with severe malaria. Design & setting: Prospective observational study in Department of pediatrics, biochemistry and faculty of science, Banaras Hindu University. Methods: The study included 50 children with newly diagnosed cases of severe malaria (positive thin and thick smear and HRP2 antigen) admitted to Pediatric ward. Age and sex matched 50 subjects with minor ailments such as abdominal pain and short stature were taken as controls. Informed consent was taken from the parents or attendants in all cases. A detailed clinical history & examination and investigations were done in all cases. Under all aseptic precaution plasma was collected in deionized polyethylene vials and stored at -200C and were analyzed for malondialdehyde, protein carbonyl, nitrite, superoxide dismutase, glutathione peroxidase, ascorbic acid, ceruloplasmin in the department of biochemistry of the Institute of Medical Sciences. The concentrations of copper and zinc in plasma were measured by the atomic absorption spectrophotometer. Results: The most common presenting age group was 0-5 years with a mean of 6.2±3.6 years . Out of 50 cases, 36 were males and 14 were females with a male:female ratio of 2.57:1. Out of the 50 cases , 33 (66%) were caused by P.falciparum and 17 (34%) were caused by non P.falciparum species. Severe anemia was the most common manifestation of severe malaria in all the age groups (54.3%) which was followed by hyperpyrexia (30%) , cerebral malaria and jaundice (24%) each. The mean hemoglobin ,total leucocyte count, platelet count, blood urea and serum creatinine in the cases were 6.2±2.2 g/dl ; 10.4 ± 6.3 103 /mm3 ; 1.1 ±0.72 105 / mm3 ; 81.8 ± 59.9 mg/dl and 1.9 ±2.2 mg/dl respectively. Thrombocytopenia followed by severe anemia was the most frequent hematological manifestation in cases with severe malaria. The plasma malondialdehyde, protein carbonyl, nitrite, ascorbic acid and copper levels were significantly raised in the cases with severe malaria. The plasma superoxide dismutase, glutathione peroxidase and ceruloplasmin were significantly decreased in the cases with severe malaria. Conclusion: The present analysis showed concurrent reduction in the anti-oxidants with momentous increase in the oxidative stress in untreated severe malaria cases. It can be concluded that oxidative stress has functional duality involved in both tissue damage as well as parasite destruction. ID/37(P) HINDURAO HOSPITAL DELHI Payal Mittal, D.K. Bhagwani, K.sharada,Pranav Gupta S K Jain, Veena Devgan mittal.payal@gmail.com Introduction: Infections result in significant morbidity and may also be responsible for a poor response to steroid therapy or induce relapse in a child who has already attained remission. Aims and objective: To study the clinical profile of infections, correlation of serum albumin and serum cholesterol level with episode of infection and the predictive value of C-reactive protein in cases of suspected infection in children with steroid responsive nephrotic syndrome nephrotic syndrome Material and Methods: This is a prospective cohort study included 65 children with steroid responsive nephrotic syndrome. These children were divided in 2 groups (1). Short term steroid (1st episode & Infrequent relapser) - < 3 month steroid/ annum (2). Long term steroid – (Frequent relapser & Steroid dependent ) > 3month steroid/annum Group 2 divided in 2 subgroups (a). On steroid only (b) On IV cyclophosphamide and steroid both Results: Total of 386 infections were found of which 182 underwent relapse. Most common infection is URI (63.7%), AGE (23.38), UTI (3.38%), followed by viral fever, CSOM, TB, Peritonitis. Albumin was significantly low and cholesterol was higher during infection than noninfection state. CRP was positive only in 4 patients. Conclusion: Nephrotic children are in immunocompromised state hence more prone to infection. Infections were more common in steroid dependent and frequent relapser. CRP is not a reliable indicator of infection in children with nephrotic syndrome. Albumin is low and cholesterol is very high during infection. ID/38(P) CLINICAL PROFILE OF NON-PERINATAL TRANSMISSION OF HIV IN CHILDREN Bharath Reddy, Sanjeeva G N, Govindraj M, Shivananda C/o. Dr. Sanjeeva GN, Senior Medical officer, Regional Pediatric ART Center, Indira Gandhi institute of Child health, Bangalore sanju_gn@rediffmail.com Objective. Perinatal transmission accounts for the majority of HIV infection in children, there have been scarce reports of HIV transmission through nonperinatal routes. We characterized children <15 years of age who may have acquired HIV infection through non-perinatal route. Methods. All children with HIV infection (n=755) registered at regional pediatric ART center, IndiraGandhi institute of child health through April 2007 were reviewed for mode of transmission. Children whose biological parents & siblings with confirmed HIV rapid test negative reports (n=17) were included, to characterize their clinico-immununological profile. Results. Of 755 children reported with HIV infection, parents of 17 children were not infected with HIV infection; mean age of these children at diagnosis of HIV infection was 8.9 years (range, 3.9 to 14.7 years). There were 11 males and 5 females; of these, 12 had unknown risks for HIV infection and 5 had history of receiving transfusion of blood & blood products; of these 12 children with unknown risk factors, 1 children had chronic illness requiring frequent hospitalization, 2 children had undergone surgeries previously, 1 child had a family member with HIV infection & remaining 8 children had no risk factors. Among these children 4 were diagnosed during presurgery screening of HIV & 13 were tested due to symptoms suggestive of HIV. Most common clinical manifestation was PersistentGenralizedLymphadenopathy (58%), Hepato-Splenomegaly (52%), Broncheictasis (41%), Candidiasis (41%), TB (35%) & 24% were asymptomatic. 23% of the children were severely malnourished at the time of diagnosis. 76% of the children had symptomatic HIV infection at the time of diagnosis. Average CD4 count at the time of diagnosis was 378(14%), which increased to 930(26%) at 1yr of follow up. At the end of 1yr, 2(11%) children died & 1 child was lost to follow up. Conclusions. These 17 cases highlight the nonperinatal mode of transmission of HIV. Majority of these children has no risk factors for HIV transmission. The probable mode of transmission would be either unsafe injections which are still prevalent in many parts of India or sexual abuse which even parents may be unaware. Although the number of reported cases of non perinatal transmission of HIV infection among children is small, it is a minimum estimate and is an important and likely underrecognized public health problem. Among the children who have received blood transfusions, majority were for presurgery correction of anemia. Clinical manifestation is similar to any child with perinatally transmitted HIV with is increased incidence of bronchiectasis (41%). 1yr survival rate of 76%. ID/39(O) CLINICAL & MICROBIOLOGICAL PROFILE OF EARLY AND LATE ONSET SEPSIS IN VLBW NEONATES. Shivani Deswal, Harish Chellani Dept. Of Pediatrics ,Safdarjung hospital & V.M.M.C, New Delhi shivanipaeds@gmail.com Introduction-Neonatal Septicemia continues to be a major cause of neonatal mortality and morbidity all over the globe.Due to paucity of data on sepsis in VLBW neonates who are at increased risk of sepsis ,this prospective study was conducted in a large tertiary care centre of Northern India providing NICU facility . Aims & Objective-To study and compare the incidence, risk factors, clinical spectrum, microbiological profile and outcome of early and late onset sepsis in VLBW Neonates. Material & Methods- Study site:- NICU of Safdarjang Hospital, New Delhi a tertiary care hospital with delivery rate of 15-18000/ year with almost 20% deliveries requiring nursery admission. A sample size of 450 VLBW neonates was studied in one year.VLBWs with Maternal risk factors and /or clinical symptomatology of sepsis in less than 72 hours were screened for EOS and those presenting with clinical features of sepsis after 72 hours were screened for LOS by sepsis screen and manual and Bact-alert blood cultures. Results- Incidence of Blood culture Proven sepsis-6.78/1000 live births(Incidence of Proven EOS-1.9/1000 live birth,Incidence of Proven LOS-4.88/1000 live births) .On univariate analysis risk factors significantly associated with EOS were premature rupture of membranes, multiple per vaginal examinations, maternal fever and chorioamniotis while on multivariate analysis,PROM and chorioamniotis were statistically significant associations. Significant risk factor for LOS was intravenous catheter use (P<.001). Most frequent clinical presentation in EOS were tachypnea,temperature instability,apnea and prolonged capillary refill time while in LOS, most common were temperature instability, apnea, poor feeding and significant gastric aspirate. In EOS Staphyloccocus aureus was the single most common pathogen isolated(10.4%) followed by Klebsiella(7.8%).In LOS,CONS and Staphylococcus aureus being the predominant pathogens. .Bact/Alert showed a culture positivity rate of 28.7% and 21.8% in EOS and LOS respectively while manual had positivity rate of 22.6% and 9.4% in EOS and LOS respectively. Mortality in EOS was 60.6% compared to 38.5% in LOS.(p-value<.005). ESBL positivity rate in EOS was 62.5% in E.Coli,44.4% in klebsella while in LOS ,E.coli showed 75% and klebsella 60%,Acinetobacter 100% and Pseudomonas 50% ESBL positivity. Mortality was higher in ESBL POSITIVE cases in both EOS and LOS. It was highest with ESBL positive E.Coli (EOS) and ESBL positive Acinetobacter and E.coli.(LOS). Mortality among gram positive pathogens was highest with MRSA(28.6%) followed by Staphylococus aureus(26.5%). Conclusion- By depicting aggressive nature of sepsis in VLBW neonates and emergence of multidrug resistant pathogens, this study helped in formulation of stringent preventive guidelines of strict hand washing, judicious use of antibiotics and good surveillance system and change of existing first line antibiotic protocols for the Nursery. ID/40(P) COMPARATIVE ANALYSIS OF CLINICAL CHARACTERISTICS, LAB PROFILE AND OUTCOME OF CULTURE POSITIVE ENTERIC FEVER IN CHILDREN LESS THAN 2 YRS AND MORE THAN 2 YRS S.Karthika, R. Monica, Vijayalakshmi, S.Thangavelu. Department of pediatrics. Dr.Mehta Hospital,Chetpet, Chennai karthika.selveswaran@gmail.com Introduction: Enteric fever constitutes a significant health burden in our community even in young children. Aims And Objectives: To compare and analyse the clinical characteristics of children less than 2yrs and more than 2yrs with culture positive enteric fever. Study Period: Retrospective analysis of case records of children with enteric fever from May 2008 to May 2010 Study Place: Dr. Mehta’s Hospital, Chetpet, Chennai Materials And Methods: Case records of 93 children who were diagnosed to have culture positive enteric fever were obtained and the difference between the clinical features, peak temperature, defervescence period, lab profile, widal positivity, antibiotic therapy and resistance patterns of age group less than 2yrs and more than 2yrs were analysed. Results: Out of 93 children, 24 (25.8%) were less than 2yrs. In addition to fever, vomiting and diarrhea were more in younger and myalgia and headache in older. Critical illness (Altered sensorium, shock and respiratory distress) were more common in young (20%) which was statistically significant(p=0.013) and 4.3% in older. Defervescence period was less than 48 hours in younger age group (47%) compared to older (22%) which was statistically significant. Hepatitis was more common in older children (78% vs 52%) which was proved by statistical significance. One grew S.ParatyphiA. Sensitivity to naldixic acid seen in 72.4%. Most responded to ceftriaxone and cefixime. All 93 of them recovered. Conclusions: Children less than 2yrs with enteric fever constitute 25.8% and they behave differently with more critical illness and early defervescence if not critically ill. ID/41(O) APPLICATION OF WHO-2009 GUIDELINES IN MANAGEMENT OF DENGUE AND ITS OUTCOME Mahantesh Matti, Sayeed, Sanjeeva, Basavaraja G V, Shivananda Indira Gandhi Institute of Child Health, Bengaluru mahantesh.mbbs@gmail.com Introduction: The numbers of dengue cases are increasing in recent days. Most of clinicians are unaware or not sensitized about WHO-2009 guidelines in classification and management of dengue cases. In our hospital we managed the dengue cases according to guidelines of WHO2009 and found it to be effective. Aims And Objectives: To study and evaluate the outcome of dengue cases which were treated based on WHO-2009 guidelines. Method: 143 Suspected dengue cases were selected based on presumptive diagnostic criteria and were classified as group A, B and C, and all the patients were treated according to WHO guidelines. 108 cases with positive dengue IgM/IgG were chosen for analysis and rest of the cases were excluded from the study. The ELISA for IgM & IgG was sent on 5th-6th day of fever. Setting: Indira Gandhi Institute of Child Health, Bengaluru. Period Of Study: August 1–31, 2010 RESULTS: 108 dengue IgM/IgG positive cases were selected for the study. They were grouped as Group A (20), Gr B (60), Gr C (28) according to guidelines. Most common associated symptoms were vomiting (60%), pain abdomen(61%),and puffiness of face(58%).Rashes were present in small number of patients(7.4%) and bleeding in 2.7% children. Most of the patients belong to age >5 yrs, 60% in Gr A, 78% in Gr B, and 64% in Gr C. Male to female ratio was 1.3:1 35% patients had fever for 3-5 days, 48.1% had 6-8 days, 11% had >8days. In Gr -A 60% had plt count of 50000100000,10% had 20000-50000 and 5% less than 20000. In Gr-B 45% had plt count of 2000050000 , 43% had 50000-100000, and 6.6% had less than 20000. In Gr-C 39% had 20000-50000 and 50000-100000,17.8% had<20000. 70% of Gr-A , 75% of Gr-B and 85.7% of Gr-C had PCV of >35, with max of 53.2. Hypoalbuminemia was significant finding in all groups (Gr A95%, Gr b-95%, Gr C-85.7%) Management The iv fluid was given to those patients who had hypotension and for those who were not tolerating oral fluids.The iv fluid used was Ringer lactate. All the Gr-A patients were treated with ORS and oral fluids with strict urine output monitoring. 76.6% of Gr B patients were treated in similar way and only 23% were given iv fluids, of them 71% given for 2 days & 29% for 3 days. Gr C patients were given iv fluids,46% for 2 days,37% for 3 days,17% for 4 days.3% needed 20ml/kg bolus initially (decompansated shock)and needed iv fluids for 3 days because of persistent hypotension. Average duration of stay was <3 days in 13.8 % children, 3-5 days in 69% and only 3.7% patients needed >7 days. With WHO guidelines 2 patients in Gr B &4 in Gr C received Blood product(FFP), and 1 in GrB and 2 patients in Gr-C had complication like ARDS and encephalitis. 1 patient changed from Gr A to Gr B in course of treatment and 3 patients changed from Gr B to Gr C. Conclusion: In our hospital we managed all the dengue suspect cases as per guidelines of WHO. The treatment is cost effective and has very good outcome with less complications. The mortality, morbidity and duration of hospital stay was reduced. The need for iv fluids, blood and blood products brought down significantly. Hence we can conclude that application of WHO 2009 guidelines in management of dengue has good outcome. ID/42(P) FREQUENCY OF INFECTIONS CAUSED BY EXTENDED- SPECTRUM BETA- LACTAMASE- PRODUCING ORGANISMS IN NEONATES– A PROSPECTIVE STUDY Nandini V, Dheeraj Bahl, Nirmaljit Kaur, N.K.Dubey, Arti Maria Department of Pediatrics, Dr.Ram Manohar Lohia Hospital, New Delhi nandini_mmc@yahoo.co.in Background : Resistant bacteria are emerging world wide as a threat to the favorable outcome of common infections in community & hospital settings..Widespread use of third generation cephalosporins and aztreonam has led to the emergence of the ESBL enzymes that are capable of hydrolyzing and inactivating a wide variety of Beta-lactams, including third generation cephalosporins, penicillins and aztreonam. Limited information is available on these infection in children especially neonates. Hence the need for this study. Objectives : To determine the frequency of infections caused by ESBL-producing organisms in neonates and to identify the various bacteria producing ESBL Materials & Methods :- Setting:-Tertiary level referral/ inborn neonatal unit. Study design :-Prospective cohort Study Clinical samples were obtained from the suspected cases of neonatal sepsis admitted to the referral / inborn neonatal units of Dr. Ram Manohar Lohia Hospital during the period ( December 2009- September 2010) as directed by their clinical condition. The samples were subjected to standard microbiological methods to isolate the organisms and to detect the ESBL producing organisms. Results : Cultures were positive in 30 out of the 123 enrolled cases( 24.39%). The frequency of ESBL producing organisms was found to be 4.06% (5/123) among total enrolled cases and 16.67%(5/30) among the culture positive cases. Blood cultures were positive in 13.0%(16/123) , pus cultures in 17.8% (22/123) urine in 2.4% (3/123) and CSF in 1.6% (2/123) cases. ESBL producing organisms were found in 2/16 (12.5%) positive blood cultures, 3/22 ( 13.6%) positive pus cultures( including ET tip, long line tip, UV tip etc.,) and were not found in urine/CSF cultures.Out of the 5 ESBL isolates , 1 was Escherichia coli( blood), 3 were Klebsiella(1 blood , 2 pus) and 1 was Acinetobacter (pus). Conclusion: Thus ESBL-producing organisms are an important cause of nosocomial infections in neonatal intensive care units. A knowledge of resistant pattern of bacteria strains in each geographical area is necessary to guide the appropriate & judicious antibiotics use, thereby, decreasing the morbidity ID/43(P) CASE REPORT: YOUNGEST SURVIVOR OF NAEGLERIA MENINGITIS Dinesh Yadav, Satinder Aneja, *Renu Dutta, Anu Maheshwari, Anju Seth Lady Hardinge Medical College and Associated kalawati Saran Children's Hospital, New Delhi-110001 dineshmamc@gmail.com Primary amoebic meningoencephalitis is a rare condition, usually caused by free living motile amebae Naegleria, Acanthamoeba and Balamuthia. These are universally fatal infections with very few survivors reported till now. Most of the earlier case reports of Naegleria survivors are from adult patients and the youngest survivor was 8 month old. We hereby report a 35 day old youngest survivor of Naegleria meningitis with neurological sequelae. Our patient was admitted with a diagnosis of partially treated meningitis. Due to inadequate response to treatment, repeat CSF wet mount examination was done to look for atypical causes which revealed free living motile amoebae resembling Naegleria, which was further confirmed by culture on E.coli enriched nutrient agar. He was treated with amphoterecin B, rifampicin and chloramphenicol. Repeat CSF examination after 2 weeks of therapy was free of Naegleria. However, the child developed obstructive hydrocephalous. Ventriculoperitoneal shunt was inserted and he was discharged after 4 weeks of therapy. At 3 month follow up, child has survived, though hydrocephalous and generalized hypertonia persists. Amoebic meningoencephalitis can present in two different forms. An acute form, which is almost universally fatal, is known as primary amoebic meningoencephalitis and is caused by Naegleria. The other form is a more chronic form, known as chronic granulomatous amebic meningoencephalitis, caused by Acanthameba and Balamuthia. Several medications such as rifampin, chloramphenicol, miconazole, ketokonazole, amphotericin B and sulfisoxazole have been used for the treatment of Naegleria meningitis and optimum treatment is not known. ID/44(P) SAFETY AND REACTOGENICITY OF A LIVE-ATTENUATED HUMAN ROTAVIRUS VACCINE ROTARIX™: AN INDIAN POST-MARKETING SURVEILLANCE STUDY Vijay Yewele, Amarjeet Chitkara, Sundaram Balasubramanian, Indu Khosla, Jaydeep Choudhury, Kishore Kumar, Pallab Chatterjee, Pankaj Garg, P.V. Suryakiran, Htay Htay Han. Dr Yewale’s Multispecialty Hospital for Children, Plot No. 6-B, Sector-9, Vashi, Navi Mumbai400 703 vnyewale@gmail.com Introduction: Rotarix™ has been licensed in over 100 countries worldwide, including India. As per the requirement of Drugs Controller General of India, post-marketing surveillance (PMS) was conducted to ascertain the safety in Indian population. Aims and objectives: An open, single-group, PMS study in India evaluated the safety and reactogenicity of Rotarix™, when administered to healthy infants following the prescribing information. Materials and methods: Infants aged 6 weeks at Dose 1 received two doses of Rotarix™ (interval of at least 4 weeks between doses; Dose 2 to be administered before 24 weeks of age) prescribed as part of routine clinical practice. Routine vaccines were co-administered. Occurrence of solicited and unsolicited symptoms was recorded during the 8-day and 31-day post-vaccination follow-up period, respectively. Serious adverse events (SAEs) were recorded throughout the study period. Results: 332 infants (265 received Doses 1 and 2 [mean age at Dose 1:10.54.29 weeks]; 67 received Dose 2 only as they had received Dose 1 before joining the study [mean age at Dose 1:10.14.20 weeks]) were enrolled. At least one Grade 2 or 3 symptom (fever, vomiting or diarrhea) was recorded in 42 infants (12.7% [95% CI:9.3;16.7]). Solicited symptoms reported post-Dose 2 were lesser than post-Dose 1 (Table). At least one unsolicited symptom was reported in 23 infants (6.9% [95% CI:4.4;10.2]). No SAEs or intussusception were reported. Conclusion: The symptoms reported are similar to that observed in earlier clinical trials. Rotarix™ was welltolerated by healthy Indian infants when administered following prescribing information as part of routine clinical practice in India. Solicited symptoms Dose 1 Dose 2 N=265 N=272 n % (95% CI) n % (95% CI) Cough 33 12.5 (8.7;17.0) 20 7.4 (4.5;11.1) Diarrhea 12 4.5 (2.4;7.8) 4 1.5 (0.4;3.7) Irritability 61 23.0 (18.1;28.6) 36 13.2 (9.4;17.8) Loss of appetite 31 11.7 (8.1;16.2) 23 8.5 (5.4;12.4) Fever 13 4.9 (2.6;8.2) 13 4.8 (2.6;8.0) Vomiting 56 21.1 (16.4;26.5) 27 9.9 (6.6;14.1) N= number of infants with at least one administered dose n/%= number/percentage of infants reporting at least once the symptom ID/45(P) TO STUDY THE OUTCOME MALARIA AND IT’S CMPLICATIONS N.L.Phuljhele, Kawtikwar Gajanan Shriram, Hemant Kumar , Mrs.K.Ramnani Deptt of Pediatrics, Pt.J.N.M.Medical college Raipur (C.G.)- 492001, mail4riyaz@yahoo.com Introduction- Malaria is responsible for 1000 deaths annually in India. Chhattisgarh is highly endemic state with an A.P.I.>5. Aims and objective-To study the outcome of malaria and it’s complications Material & method- Type of study: a retrospective and prospective observation based study Inclusion criteria- all children who were suffering from malaria and clinical malaria admitted in the medical college of Raipur and Bilaspur (C.G.) from July 2009 to 2010.Exclusion criteria –fever other than malaria excluded by suggestive investigations Methodology: Data was collected as per preformed proforma and compiled as per the outcome and complications observed. Result & discussion-Total 74 cases [male-48 ,female-26 ] were studied. Various clinical presentations were fever-95.94%, pallor-51.35%, shivering-35.13%, hepatomegaly- 35.13%, headache-32.43%, splenomegaly-31.01% etc. Among 74 cases 54 were malaria antigen test and/or peripheral smear positive in which Pl.vivax-7.4%,Pl.falciparum72.22% and mixed type-18.51%.Treatment given were chloroquine3, quinine-27, artemisnin derivatives-44, RCC-15, Whole blood-7 cases. Total children died-21 and mortality rate with various complications were in cerebral malaria-14.86%, A.R.F.-1.35%, pulmonary oedema1.35%, algid malaria-9.45%,,0% black water fever,thrombocytopenia-4.05%, hypoglycaemia4.05%. Most common complication was cerebral malaria followed by algid malaria, thrombocytopenia and hypoglycaemia. Conclusion-Cerebral malaria and algid malaria were major culprit for mortality as compare to thrombocytopenia, hypoglycaemia, A.R.F., pulmonary oedema, black water fever. ID/46(P) A STUDY OF THE CLINICAL PROFILE OF DENGUE FEVER IN CHILDREN CATEGORY INFECTIOUS DISEASE Agarwal Vishnu, Verma C.R., Gupta Ashok, Sharma R.B. Department of Paediatrics, SPMCHI, Jaipur vishnu.agarawal@yahoo.in Introduction - Dengue fever is an acute febrile illness, caused by viruses belonging to the flaviviridae family and is characterized by biphasic fever, myalgia, arthralgia and rash. Aim & Objective : The present study was undertaken to evaluate the clinical profile of serologically confirmed dengue cases, admitted at Sir Padampat Mother and Child Health Institute, Jaipur. Material & Method : In this retrospective, hospital based, descriptive case study, serologically confirmed cases of Dengue fever / Dengue hemorrhagic fever from Sept. 2008 to May 2010 were included and followed up prospectively with regard to clinical features, various haematological parameters and other investigations like liver function test, and abdominal sonography. Results : Out of total 36 cases, 22 were diagnosed as Dengue fever, 8 were as DHF and 6 were as D.S.S. Main clinical symptoms present were - fever 100% (36/36); vomiting 61.11% (22/36); pain abdomen 27.77% (10.36), and bleeding manifestation 38.88% (14/36). Main clinical signs present were - flushing of palm and sole 77.77% (28/36); haemorrhagic manifestation 38.88% (14/36); hepatomegaly 83.33% (28/36); peri gall bladder edema 77.77% (28/36); ascites 55.55% (20/36); epistaxis 8.33% (3/36); pulmonary edema 8.33% (3/36), low platelet count 38.88% (14/36); and deranged liver function test 55.55% (20/36). Conclusion : High index of suspicion to diagnose and rapid appropriate management is necessary to save patients of dengue haemorrhagic and dengue shock syndrome. ID/47(P) ACUTE VIRAL HEPATITIS - ETIOLOGY, CLINICAL PROFILE AND OUTCOME IN CHILDREN INFECTIOUS DISEASE Agarwal Vishnu, Verma C.R., Gupta Ashok, Sharma R.B. Department of Paediatrics, SPMCHI, Jaipur vishnu.agarawal@yahoo.in Introduction : Acute viral hepatitis is a common clinical, medical problem in developing countries, where poor sanitary conditions are still prevailing like lack of access to safe water supply and unhygienic excreta disposal. Aim & Objective : To evaluate etiology, clinical profile and outcome of acute viral hepatitis in children. Setting & Study Design : Retrospective, hospital based, descriptive case study. Material and Method : In this study, total 40 children diagnosed as acute viral hepatitis, on the basis of clinical history, examination, relevant routine and specific laboratory investigations like viral marker were included. Results : Main symptoms present were jaundice 100% (40/40); nausea and vomiting 90% (36/40); abdominal pain 80% (32/40); anorexia 75% (32/40); myalgia 25% (10/40); fever 37.5% (15/40); altered sensorium 20% (8/40); and bleeding manifestations 20% (8/40). Major clinical signs present were hepatomegaly 80% (32/40); splenomegaly 70% (28/40); ascites 30% (12/40); and anaemia 30% (12/40). Liver function tests like total & direct bilirubin and SGPT were deranged in all patients with bilirubin level more than 10 mg/dl and SGPT level > 2000 IU/L in 8 patients. PT was deranged in 37.5% (15/40) patients. Viral marker like Anti HAV (IgM) was positive in 26/40 patients and HBs antigen was positive in 8/40 patients. 6 patients were negative for these two viral markers . Out of total 40 patients, 34 patients improved symptomatically, hence were discharged from hospital, while 3 patients died and 3 patients left against advice. ID/48(P) CLINICAL CHARACTERISTICS AND OUTCOME OF PEDIATRIC H1N1 CASES PRESENTING TO A MEDICAL COLLEGE HOSPITAL IN JAIPUR, RAJASTHAN Agarwal Vishnu, Gupta Ashok, Verma C.R., Sharma R.B. Department of Paediatrics, SPMCHI, Jaipur vishnu.agarawal@yahoo.in Introduction: Swine flu is a highly contagious, acute respiratory infection. Setting and Design : Hospital based retrospective study Aim and Objective : To determine clinical characteristics and outcome of pediatric H1N1 cases after their treatment with oseltamavir. Material and Method: This hospital based, retrospective, case study was undertaken to study the clinical characteristics and out comes of pediatric H1N1 cases. In this study, we reviewed the case history of total 193 confirmed cases of pediatric swine flu, which were positive for novel H1N1 influenza by RTPCR. Observation : Out of 193, 186 patients were treated on outdoor patient basis, while 7 patients required hospitalization. Mortality among study group was nil. 182 patients were asymptomatic / clinically well, while 11 patients had persistence of symptoms at completion of five days of therapy in forms of fever (6/11), cough (11/11) and running nose (2/11), which also recovered with a additional symptomatic therapy of 2-4 days. Only 3.62% (7) patients out of 193 required admission. Mortality among all patients was nil. Conclusion : In our study, clinical features were mild in 96.37% (186/193) and non specific in majority of patients, suggesting the low virulence of the present virus (H1N1). ID/49(P) A COMPARATIVE STUDY AMONG EARLY VERSUS LATE STARTERS OF OSELTAMAVIR AMONG PAEDIATRIC H1N1 PATIENTS PRESENTING TO A MEDICAL COLLEGE HOSPITAL IN JAIPUR, RAJASTHAN Agarwal Vishnu, Gupta Ashok, Verma C.R., Sharma R.B. Department of Paediatrics, SPMCHI, Jaipur vishnu.agarawal@yahoo.in Introduction: Swine flu is a highly contagious, acute respiratory infection. Setting and Design : Hospital based retrospective study Aim and Objective : To evaluate differences if any among early and late starters of oseltamavir regarding persistence of symptoms like fever, cough, running nose and need for hospitalization Material and Method : In this study, we reviewed the case history of total 193 confirmed cases of pediatric swine flu, which were positive for novel H1N1 influenza by RT-PCR. This study was undertaken to evaluate differences if any among early and late starters of oseltamavir regarding persistence of symptoms like fever, cough, running nose and need for hospitalization. Observation : There was no significant difference statistically regarding outcome, persistence of fever and other symptoms, need for hospitalization among early and late starters of oseltamavir, hence signifying that late therapy is as effective as early therapy for treatment of paediatric swine flu cases. Our study clearly revealed that even late starters (115/193) responded well to treatment (105/115), got afebrile within 48 hours (110/115) and were asymptomatic (105/115) at the end of 5 days therapy. Conclusion : Late therapy is as effective as early therapy with oseltamavir for treatment of paediatric H1N1 patients. ID/50(P) A STUDY OF THE SEVERE MANIFESTATIONS ASSOCIATED WITH P. VIVAX MALARIA IN CHILDREN : A CHANGING CLINICAL SCENARIO OF P. VIVAX MALARIA Agarwal Vishnu, Verma C.R., Gupta Ashok, Sharma R.B. Department of Paediatrics, SPMCHI, Jaipur vishnu.agarawal@yahoo.in Severe malaria is classically associated with P. falciparum malaria. Information though little, is available on the contribution of P. vivax to severe disease. Setting & Design : Hospital based, prospective, descriptive case study Aim & objective : The present study was undertaken to study the severe manifestations associated with P. vivax malaria. Material & Method : This study was conducted in Department of Paediatric Medicine, SPMCHI, Jaipur from 1st April 2010 to 15th September 2010. In this study, all the patients confirmed for malaria either peripheral blood film examination or rapid diagnostic test for malaria were included. Results: Out of total 21 patients of P. vivax malaria, seven (33.33%) were severely anaemic, rest 14 (66.66%) were also anaemic, though their Hb was more than 5 gm/dl. Other reported severe manifestations were thrombocytopenia (with platelet count less than 1 lac) - 71.42% (15/21); repeated convulsion 19.04% (4/21); altered sensorium 23.80% (5/21); deranged renal function 19.40% (4/21); deranged liver function 4.76% (1/21); minimal ascites 9.52% (2/21); Headache 14.28% (3/21); Hypoglycaemia 14.28% (3/21); Epistaxis 9.52% (2/21); respiratory distress 4.76 (1/21), hemetamesis 4.76% (1/21); and loose motion / vomiting 19.04% (4/21). Conclusion : P.vivax malaria should not be underestimated looking into above changing clinical scenario. ID/51(O) ANTIMICROBIAL SENSITIVITY & RESISTANCE PATTERNS FOLLOWING CHANGE IN ANTIBIOTIC POLICY COMPRISING WITHDRAWAL OF 3RD GENERATION CEPHALOSPORIN IN NICU. Jyoti Bagla Asst. professor pediatrics,GMC Kota & S. Ramji (Prof& Head), Deptt. Of Neonatology , MAMC ,New Delhi . jyotibagla@yahoo.co.in Background: With the rise in antimicrobial resistance have come a variety of strategies designed to prevent this problem. We assessed the effect of an antibiotic restriction protocol on the antibiotic susceptibility in our NICU. Objective: To evaluate antimicrobial sensitivity and resistance pattern in culture isolates from NICU and to guide rational antibiotic policy based on isolated organism profile and antimicrobial sensitivity pattern. Design: Retrospective comparative analysis. Setting : Intramural tertiary level neonatal unit.Methods: We analyzed 1140 blood culture taken during period-1 ( from May 2005 to Dec. 2006) and period-2(Jan. 2007 to Dec. 2008) for Isolated organisms and the sensitivity and resistance results of various antibiotics compared following a change in antibiotic protocol . There were significant difference in antibiotics usage policies during period 1 & Period 2 based on microbial surveillance but the indications to use antibiotics remained unchanged. Antibiotic policy during period 2 comprising of starting of only amikacin in 1) early onset sepsis, 2) newborns weighing <1500 gm born to mothers having either leaking for >72 hours or leaking for >24 hours and evidence of chorioamnionitis, maternal fever, foul smelling liquor, or gastric aspirates showing >5 polymorphs/ hpf. Antibiotics empirically used for late onset sepsis and in surgical babies were ceftriaxone and amikacin. Meropenem and vancomycin were the alternative second line antibiotics. The important features of our policy were overall restricted use of antibiotics, use of amikacin monotherapy and withdrawal of 3rd generation cephalosporin (cefotaxim) as first line antibiotics in early onset sepsis, use of ceftriaxone instead of cefotaxim for late onset sepsis, no prophylactic use of antibiotics except in surgical babies and reduction of duration of antibiotics. Results: The leading causes of neonatal sepsis have been Klebsiella species, S. aureus and E. coli. Amikacin and netilmicin emerged as an antibiotic showing good sensitivity to commonly isolated bugs both gram positive and negative including most of staph. aureus and CONS and its resistance decreased significantly (p<0.0001) in period 2. Withdrawal of cefotaxim and restricted use of of ceftriaxone led to significant increase in sensitivity and reduction in resistance to this drug. (p<0.001). Vancomicin and meropenam maintained good sensitivity during both the periods as second line drugs. Ampicilline is no longer sensitive now and piperacillin and amoxyclave did not show any significant change. On the other hand ciprofloxacin showed significant increase in resistance even though we did not use it. kliebsella maintained good sensitivity to amikacin, netilmycin and meropenam. Inspite of use during both the periods sensitivity of amikacin significantly (p<0.02) increased in period 2. For staph. aureus and CONS aminoglycosides (amikacin, netilmycin and gentamicin) and vancomycin turned out to be best drugs with sensitivity varying between 80-100% during both the periods. Conclusions: Continuous change of antibiotic policy and restricted use of drugs based on microbial surveillance ensure increasing sensitivity and decreasing resistance to antibiotics. ID/52(P) NEW CHALLENGE IN NICU – ESBL SEPSIS MANAGEMENT!! TO STUDY THE RISK FACTORS, CLINICAL COURSE AND OUTCOME OF ESBL SEPSIS IN NEONATES ” Jawa Gaurav, Arya Sugandha, Chelani H.K , Gaind Rajni Dept. of Pediatrics, Lok Nayak Hospital and MAMC, New Delhi drgauravjawa@yahoo.com Background : Gram-negative bacillary sepsis is becoming a common nosocomial problem in neonatal units with emergence of resistant pathogens such as the ‘Extended spectrum-βlactamase producing enterobacteriacae (ESBL’s) compounding this issue. Methods : A Prospective hospital based study from April 2006 to March 2007 was conducted at neonatal intensive care unit of Safdarjung Hospital. All newborns with signs of sepsis or risk factors predisposing to it and a positive blood/CSF culture for gram negative bacteria were taken as study subjects. Gestational age, birth weight, sex, maternal and environmental risk factors, clinical presentation, antibiotic therapy and outcome were recorded for each case. The sensitivity to antibiotics and a screening, confirmatory test for ESBL detection was carried out for each isolated organism. This data was then compared between the ESBL and the non-ESBL producers and analyzed using the Chi-square and student –t test. Results : During the study period a total of 16820 deliveries took place, including normal and caesarean, of which 5116 newborns were admitted to NICU. Sepsis was suspected and blood cultures were sent in 1890 newborns. Of the total gram negative isolates, 102 were taken for study of which 50 were ESBL producing strains. The most common organism isolated was Klebsiella(54 cases) of which 37(68%) were ESBL producers. Other isolates were Acinetobacter(2/4),E.coli(12/35) and Pseudomonas(0/5). An almost equal number of ESBL producers & the total gram negative isolates were seen in the Early ( /46) and Late onset sepsis( /56) groups. Amongst risk factors; Prolonged rupture of membranes (p=0.039) and previous treatment with antibiotics(p=0.010) predisposed the neonate to harbor an ESBL producing strain. Newborns with ESBL infection were more likely to manifest lethargy (p=0.04), seizures (p=0.024) and shock(p=0.012), as compared with non-ESBL group. The ESBL producers showed more resistance to antibiotics with no susceptibility to Augmentin and only partial to Ciprofloxacin (58% ESBL vs. 78% non-ESBL). Highest susceptibility rates of 100% were seen in both the groups to the Carbepenem. Morbidity in terms of mean duration of stay (19 vs 17.9 days) was not significantly different but mortality was found to be much higher (13 vs 4 cases) in the ESBL group, which was statistically confirmed (p=0.07). Conclusion: ESBL production was found to be significantly associated with prolonged rupture of membranes in the mother prior to delivery and prior usage of antibiotics in the baby. A high incidence of positive isolates (49%) in gram negative sepsis that was equally distributed in EOS(22/46) and LOS(28/56), indicated percolation of this phenomenon in community. Their isolation in a neonate requires specific microbiological tests and complete antibiogram for treatment. A more fulminant outcome is associated with such sepsis and higher end, expensive antibiotics required to treat them. ID/53(P) QUALITY OF LIFE IN HIV-INFECTED ADOLESCENTS IN NORTH INDIA Tripti Pensi, Pyarelal Asso Prof, Department of Paediatrics, Dr. Ram Manohar Lohia Hospital, New Delhi drpensi@gmail.com Issues: HIV illness and its consequences can affect the lives of children. However, Children’s experience of ill-health, medical intervention, and the effects of these upon development and adjustment are not well understood. In order to understand these effects and improve paediatric healthcare it is important that we are able to assess children’s quality of life effectively. Description; The study was conducted from January 2008 to December 2008 at Dr. Ram Manohar Lohia Hospital, New Delhi, India, at the ART center. During the study period, 100 HIV-infected and 200 uninfected children between 12-18 years of age accompanied by their caregivers were enrolled. Some of uninfected children, who recruited to assess their HRQoL, were siblings of the infected children, and others were from institution based care homes. Among our study group, there were some infected children who were living in the same care homes as the uninfected children. All the children considered for the study had similar socio-demographic characteristics. As per the National Guidelines, written informed consent for history and examination was obtained from the primary caregivers of 300 children. The PedsQLTM 4.0 Generic Core Scales is a pediatric HRQoL instrument for ages 2–18 years which distinguishes between healthy children and pediatric patients with acute or chronic health conditions. The Peds- QLTM 4.0 includes child self-reports (ages range 8–12 years) and parent proxy-reports., The PedsQLTM 4.0 encompasses the following subscales: Physical Functioning (8 items), Emotional Functioning (5 items), Social Functioning (5 items), and School Functioning (5 items). The Physical Health Summary Score and The Psychosocial Health Summary Score are calculated. Further the Total Scale Scores for child self report and parent proxy-report were also calculated and compared. Overall, HIV infection was associated with a negative impact on QoL among children, with lower scores for physical, school, emotional functioning subscales, and health symptoms for children 12-18 years of age. The uninfected children had lower social functioning scores which is attributed to the fact that infected children have better access to support and social services from health care providers in HIV clinics. On comparing QoL with the antiretroviral regimen we found that children who were not receiving any antiretroviral therapy reported worse QoL. Interestingly, our results identified infected children living at home to be at a higher distress of psychosocial functioning and health symptoms when compared with children living in care homes Lessons learnt: PedsQLTM 4.0 had adequate reliability and validity, and could be used as an outcome measure of generic HRQoL in HIV-infected children. Children living in care homes were better in terms of psychosocial functioning and health symptoms Next Steps: Efforts should continue to focus on identifying opportunities to support good quality care either in homes or by supporting the care givers of infected and affected children in order to improve their quality of life ID/54(P) CLINICAL SPECTRUM AND ORGAN SPECIFIC MANIFESTATIONS IN PEDIATRIC HIV Maj Sachendra Badal, Veena Singh, Col Rakesh Gupta, Brig Mukti Sharma Dept of Pediatrics AFMC, Pune 41104 badalsachendra@yahoo.com Introduction: HAART has dramatically changed the natural history of HIV infection and recognized HIV as a chronic, rather than terminal illness with varied clinical manifestations. Aims & Objectives: To study the clinical spectrum and organ specific manifestations in pediatric HIV and effect of HAART Materials & methods: A prospective study from Jan 2007 to July 2010 at Pediatric HIV clinic of a tertiary care hospital. All the enrolled HIV+ children were followed for clinical and immunological status as per WHO guidelines. HAART was started as per NACO guidelines. Data were compiled and analyzed. Results: 225 HIV positive children were enrolled in the study. Majority of children were between 1-5 years 99(44%) and male 128 (57%). 115 children (51%) lost their parents and reared by NGOs. The mode of transmission was vertical in 218 (96.8%) children and mean age of detection was 2.1 yrs. Clinical category at the time of enrollment were cat I, II, III and IV in 82, 70, 58,and 15 cases and immunological category 72,32,53 and 68 cases respectively. Organ specific manifestations were protein energy malnutrition (87%), lymphadenopathy (53%), Skin manifestations (47%), GI involvement (45%), Hematological (34%), Tuberculosis (27%), respiratory (23%), dental caries (19%), cardiac involvement (13%), otorrhoea (12%), neurological involvement (5%), recurrent parotitis (6%) and renal involvement (3%). 121 (54%) children were on HAART. There were 6 deaths over last 3 years. HAART side effects were rare except one patient who had fatal lactic acidosis. The incidence of OIs seen in children on HAART is much less as compared to HAART naïve children and growth rate was significantly higher in children on HAART. Conclusions: Pediatric HIV cases were seen more commonly in males, 1-5 years of age in our study. Children have rapid immunological deterioration as compared to clinical. Multi system involvement was seen and common manifestations were PEM, lymphadenopathy, skin manifestations, GI involvement and respiratory disorders. Children tolerate HAART well and incidence of OIs seen was much less in children on HAART and their growth rate was significantly higher than children not on HAART. ID/55(P) CARDIOVASCULAR MANIFESTATION OF HIV IN CHILDREN: A PROSPECTIVE STUDY Radha Binod Pal, Subhasish Bhattacharyya, Malay Kumar Sinha, Sukanta Chatterjee Department of Pediatrics, Medical College & Hospital, Kolkata. rbinod100@gmail.com Introduction: Cardiac manifestation of human immunodeficiency virus (HIV) infection in children is protean and common. They include asymptomatic and symptomatic cardiac dysfunction, hemodynamic abnormalities, dysrhythmias, cardiac arrest and cardiac death. The incidence of cardiovascular disease reported amongst HIV infected children ranges from 72% to over 90%. Subclinical cardiac abnormalities in HIV infected children are common, persistent and often progressive. Clinical examination, chest radiographs, electrocardiography and echocardiography may pick up both the clinical as well as subclinical cardiac diseases at the earliest. Aims & Objectives: 1. to determine the cardiovascular status of HIV infected Indian children. 2. To find out the difference of cardiovascular diseases if any between the HIV infected children who are on HAART (stavudine based FDC >1yr) (Group-2) vs. without HAART (Group-2). Materials & Methods: Design: Prospective observational study. Settings: Regional Pediatric ART centre, Department of Pediatrics, Medical College & Hospital, Kolkata. Duration: June, 2009 to August, 2010. Subjects: All HIV infected children between 2-12yrs of age. Congenital heart diseases, pre existing heart diseases and multi transfused thalassemia patients are excluded. Methods: History taking, clinical examinations were done with special emphasis on cardiovascular system. Necessary investigations like ELISA test for HIV, CD4 count, lipid profile, chest X ray, ECG & echocardiography were done. The studied parameters were age 5 to <10 yrs, WHO clinical stage 3, symptomatic related to CVS, hypertension, dyslipidemia, cardiomegaly in chest X ray, abnormal ECG,abnormal left ventricular shortening in echocardiography and presence of cardiomyopathy. The data are analyzed statistically using SPSS software. Results: Out of total 90(n) HIV infected children 50% were from each group, 54% were male and 46% were female. The mean age was 7.32yrs and 95% CI for mean 6.8-7.8. Most of the children, 48.9 %( n=44) were in WHO clinical Stage-3 of HIV disease. Among 45 patients of HIV infected children not on HAART 57.8% (n=26) had cardiovascular disease and only 15.3% (n=4) of them were symptomatic. On the other hand among 45 patients of HIV infected on HAART >1yr, 62.2% (n=28) had cardiovascular disease and only 17.9% (n=5) of them were symptomatic. The maximum number of patients found to be suffering from HIV associated cardiovascular disease were in WHO Clinical Stage-3 (n=28). Most common echocardiography abnormalities in HIV infected children were LV enlargement (45.5%), abnormal LV fractional shortening (23.3%), pericardial effusion (12.2%) and pulmonary hypertension (11.1%). The most common cardiac manifestations were cardiomyopathy (70.4%) followed by systemic hypertension (50%), myocarditis (48.1%) and pericardial diseases (29.6%). There was no statistically significant difference in cardiac diseases between the two groups. Conclusion: Cardiomyopathy and hypertension are the most common cardiac manifestation of HIV and there is no significant difference between the two groups. ID/56(P) CORNEAL CLOUDING IN A CASE OF CONGENITAL CMV INFECTION -A RARE MANIFESTATION Vinay Mishra, Charusheela Warke, Jitendra Mandvade, Rahul Gosavi, Sushma Malik. Pediatric Resident, Department of Pediatrics, 1st Floor, College Building, TNMC & BYL Nair Hospital, Mumbai Central, Mumbai-400008 breakfree_777@rediffmail.com Introduction: Bilateral extensive corneal clouding results from a variety of genetic, metabolic, developmental and idiopathic causes. Here we present a newborn with corneal clouding as a rare manifestation of CMV infection. Case History: A 25yrs G2P2L1D1 mother, with third degree consanguineous marriage delivered a full-term severe IUGR (730 gms). First issue was also severe IUGR (650 gms) with no obvious dysmorphism. In this pregnancy her CMV IgG was positive, APLA/ACL/Anti dsDNA- negative and thyroid profile normal. Examination of the baby revealed dysmorphic facies with microcephaly, redundant scalp, sloping forehead, hypertelorism, bilateral corneal opacities, small oral fissure, natal teeth, left rockerbottom foot and overlapping of toes. On auscultation systolic murmur was noted. No hepatosplenomegaly or rashes were found. At birth, serum CMV IgG of the baby was four-fold as compared to the maternal titres. Karyotype, USG Skull/Abdomen, IOP/Corneal diameter were normal. 2D-ECHO revealed small PDA . Xray Skull showed no intracranial calcifications. B-scan-ruled out vitreous or retinal abnormalities. Our clinical impression was congenital CMV infection and patient succumbed on day 7 due to fulminant sepsis. Discussion: Corneal clouding whether idiopathic or linked to genetic syndromes is extremely uncommon in newborns. Buphthalmos is one of the most common etiology of neonatal corneal clouding. The other rarer causes being Peters anomaly, sclerocornea, TORCH infections, birth trauma, dermoid, metabolic diseases, maternal alcohol abuse and idiopathic. TORCH infections are usually associated with cataract and chorioretinitis; however, cloudy cornea are a rare manifestation of rubella and CMV infection, and the latter was seen in our case. Conclusion: Bilateral corneal clouding is an important cause of blindness in neonates besides bilateral cataracts and glaucoma. Although extremely rare, cloudy cornea can be associated with CMV infections acquired in utero. ID/57(P) HEMATOLOGICAL PROFILE OF DENGUE INFECTION IN CHILDREN AT IGICH Merriyet.M.B, Shivananda, Sanjeeva, Shruthi.B Department Of Pediatrics, Indira Gandhi Institute Of Child Health, Karnataka merriyetmb@yahoo.co.in Introduction: Dengue infection is an unpredictive viral illness that can cause significant morbidity and mortality if not managed properly. Blood and blood product transfusions are rarely indicated. Aims & objectives :To study the haematological profile in children admitted at a tertiary care hospital with dengue infection till recovery. Materials & Methods:362 children hailing from in and around Bangalore,admitted from April 2010 to August 2010 suspected of dengue infection were included.The following haematological parametershaemoglobin,hematocrit and platelets were done on a daily basis till recovery.Other parameters like total count,C-reactive protein,liver enzymes and serum albumin were done routinely. Results: At admission-75.9% patients had Hb of 10-15 gm%,average Hb-12.53 gm%,65.4% had PCV >35,average PCV-36.9,42.2% had platelet count ranging from 50,000- 1 lac, minimum platelet count- 3800,average platelet count-73,954, TLC- (4000-15,000)-77.4% & leucocytosis in 9.3%. On follow up-Hemoglobin-On D2-71.8% had Hb of 10-15gm%,which increased to 81.3% on D5 & 5.8% had Hb >15 gm% on D1 which dropped to 0.85% on D4 & D5 of recovery. Drop of Hb(in %)-maximum drop of >20% was seen on D2 of admission in 48.8 % patients & decreased to 22.5 % on D5. PCV-steady decline was observed during the stay.On D2-62.8% had PCV >35 which dropped to 32% on D5.By D3 to D5 36.1% to 43.9% had reached a PCV plateau of 30-35%. Drop of PCV(in %)- on D2 maximum drop was seen in the range 0-5% in 36% patients,but >20% drop was maximum on D3 in 11.4% which decreased to 8.6% and 8.7% on D4 & D5 respectively. Platelet count- patients with platelet count in the range 1-1.5 lac gradually increased during the stay,from 16% on D2 to 58.8% on D6,whereas patients in the range 50,0001lac platelet count remained relatively stable around 42% till D5 & dropped to 35.2% on D6,whereas patients in the group with platelet count less than 50,000 gradually decreased in number during the stay indicating steady recovery. CRP was positive in 10.45%(29) of patients,among them 62%(SGOT) & 51.7%(SGPT) were elevated with hypoalbuminemia in37.9% of patients.Of which 5(17.2%) had ARDS and 1 had encephalitis. Liver enzymes were elevated in 58.3%(SGOT) & 46%(SGPT) of patients.Around 80% had 2-10 times elevation.Of which 39% had grade 3 & 4% had grade 4 DHF/DSS. Hypoalbuminemia seen in 33.3% patients,of which SGOT elevated in 80% and SGPT elevated in 65.8%.2 had ARDS. Conclusion: In dengue infection,response to treatment & recovery can be monitored effectively with daily monitoring of Hb,PCV & platelet till recovery.Other parameters like elevated liver enzymes & low albumin can predict liver cell injury. ID/58(P) EVALUATION OF TOURNIQUET TEST AS AN EARLY MARKER OF DENGUE SHOCK SYNDROME Smitha H.V, Prahalad Kumar, Govindaraj, Shivananda, Vishwanath, Hemalatha, Pradeep Dept of Pediatrics, IGICH, Bangalore ameet_managuli@yahoo.co.in Introduction: engue, a vector borne disease has an unpredictable course ranging from an asymptomatic presentation to florid complications. It is characterized by increased capillary fragility & thrombocytopenia in the DHF variant. Tourniquet test is a sensitive bed side test that can be used as an early marker of DSS. It is therefore indeed a handy & life saving screening procedure to detect those with risk of developing DSS. Objectives: To evaluate the role of tourniquet test as an early marker of DSS. To correlate tourniquet test with clinical parameters & platelet count Design:Prospective study, study period from july 2010 t0 september 2010 (3 months) Setting: Indira Gandhi Institute Of Child Health, Bangalore Materials & Methods: Sixty children admitted to IGICH, fulfilling the WHO criteria of dengue fever formed the study group. These children after detailed history & thorough clinical examination were subjected for tourniquet test as per standard test. The result of the test was correlated with the clinical features & platelet count. Results: Out of 60 children, 32 children had f/o DSS, 18 children with DHF & 10 children with DF. In all these children Serum IgG & IgM was positive. Out of 32 children with DSS, tourniquet test was positive in 25 children.(78%) Out of 18 children with DHF, 15 children had positive tourniquet test.(83%) Out of 10 children with DF, only 2 children had shown positive tourniquet test.(20%) Out of 10 child with DF, only 2 children had shown positive tourniquet test. The above observation also correlated positively with platelet count. Out of 60 children,all children had platelet count of <1,00,000. 40 children had platelet count of <50,000 & 20 children had platelet count of <20,000. Out of 40 children with platelet count of <50,000, 30 children were positive for tourniquet test and out of 20 children with platelet count of <20,000, tourniquet test was positive in 16 children. Conclusion: DHF & DSS is still a preventable vector borne disease. Early recognition & treatment will reduce both mortality & morbidity. We conclude from our observations that tourniquet test is a dependable bed side screening procedure which can effectively detect those high risk patients who are at risk of developing DSS, especially in the peripheries, where want of lab results should not handicap for making diagnosis of DHF/DSS & also the test also correlates well with the levels of thrombocytopenia. ID/59(P) CLINICAL PROFILE OF TUBERCULOSIS IN CHILDREN. Anupam Bahe, Amol Joshi, L.S. Deshmukh Department of Pediatrics, GMC, Aurangabad. dramolkj@yahoo.com Introduction: Childhood Tuberculosis is different than that of adults. This study was conducted to study the clinical profile of childhood tuberculosis Aims and Objectives: To study the clinical profile of Tuberculosis in children including HIV& the difficulties in categorization of Pediatric patients as per RNTCP. Material and Methods: Observational study conducted in Pediatric Department, GMCH, Aurangabad included 150 patients admitted in wards and attending Pediatric OPD from January 2007 to November 2008. Patients were evaluated in details regarding history, physical examination and diagnostic tests. Results: Most common age group of presentation was 1-5 years, 74% belonged to Lower socioeconomic class, having Severe Malnutrition. History of Tuberculosis contact was seen in 52.66% patients. History of BCG vaccination was given by 71.33% of all patients. Most common symptom was Fever 90.67% followed by cough 49.33%. Lymphadenopathy and pallor were most common signs on presentation. 68% patients were Mantoux Reactive. X-Ray chest was normal in 52% patients. In Neurotuberculosis only 15.78% patients were effectively vaccinated with BCG, Mantoux was Non Reactive in 81.5% patients. Of those HIV seropositive, 94.12% were mantoux NonReactive. Only 3,3%patients had all 3 criteria of AFB demonstration ,XRay changes and Mantoux Positivity as per RNTCP. Conclusion: NeuroTuberculosis was most commom Extrapulmonary Tuberculosis. BCG vaccination has Neuroprotective Role. Pulmonary Tuberculosis was most common presentation with HIV patients. RNTCP Criteria are inadequate for diagnosis of Tuberculosis in children. ID/60(O) CLINICAL PROFILE AND LABORATORY FEATURES OF TUBERCULAR LYMPHADENITIS IN CHILDREN Rashmi Ranjan Das, Rakesh Lodha, Sushil Kabra Department of Pediatrics, AIIMS, New Delhi dr_rashmipgi@yahoo.com Aims and objectives: To analyze the clinical presentations, laboratory investigation results, and histopathology evaluation of tubercular lymphadenitis in children. Materials and methods: Retrospective study of 717 children in the Department of Pediatrics between year 1996 and 2010. Results: The age range was from 6 months to 14 years with M:F ratio = 1.1:1. Common constitutional symptoms were: fever (49%), cough (36.7%), weight loss (49.6%), and reduced appetite (50%). Only 35% had chest radiographs suggestive of pulmonary tuberculosis. Fineneedle aspirates from 73% patients showed caseating granulomas. However, acid-fast bacilli were seen in only 23% aspirate smears. Thirty six patients (5%) required a lymph node biopsy to confirm the diagnosis. History of contact was positive in 35.8% children, and 47.7% had received BCG. Mantoux test was positive in 442 (62.4%) children. Cervical, axillary and inguinal nodes were found in 77%, 26.7%, and 16% children respectively. The consistency of nodes was firm in 512 (71.4%), fluctuation was present in 205 (28.6%). In 465 (65%) lymph nodes were matted. Hepatomegaly of more than 2 cm was present in 26 (3.6%) and spleen was enlarged (> 2 cm) in 4 (0.5%) only. Conclusion: Findings suggest that tubercular adenitis occurs in all age groups and can occur in vaccinated children also. It may be a sole manifestation of tubercular infection. The cervical nodes are predominantly involved. There is no typical location of nodes in individual groups but multiplicity and matting of nodes are characteristic features of tubercular adenitis in children. ID/61(P) APPLICABILITY OF RNTCP PEDIATRIC ALGORITHM IN CLINICAL PRACTICE Ashima Goyal, Nilofer Mujawar, Meenakshi Girish, Maitreye Bhusari dr.ashimagoyal@gmail.com Introduction: Tuberculosis remains a major public health problem in India. On the recommendations of an expert committee, a revised strategy of control tuberculosis was pilot tested in 1993 in a population of 23.5 lakh and thereafter increased in phased manner. A full fledged programme was started in 1997 and rapidly expanded with excellent results. This revised national tuberculosis control programme ( RNTCP ) uses the DOTS strategy, which is based on results of tuberculosis research done in India. RNTCP states tuberculosis should be suspected among children presenting with fever and/ or cough for more than 3 weeks, with or without weight loss or no weight gain; and history of contact with a suspected or diagnosed cases of active tuberculosis within last 2 years. Aim: Applicability of RNTCP Pediatric Algorithm in clinical practice Objectives: 1. How often AKT is started in Pediatrics as per RNTCP Algorithm for pediatric patient 2. To Study role of sputum examination in paediatric patients Study Design: Retrospective study of cases registered in RNTCP in LMH. Study Method: All case sheets of children registered with RNTCP unit of LMH bet August 2006 to July 2010 were analyzed. Various parameters as to why they were started on AKT were studied. Result: To be computed. ID/62(P) A STUDY OF AWARENESS AMONGST THE CLIENTELE POPULATION ABOUT OPTIONAL VACCINES IN THE IMMUNIZATION PROGRAMME Aman Tyagi, Amit Devgan Undergraduate Medical Student, Dept. of Pediatrics, Armed Forces Medical College, Pune. Dr.aman.tyagi@gmail.com Background: The current trend is to combine immunizing agents into small packages and thus reduce the number of doses an individual must receive. A well thought out immunization schedule must be epidemiologically relevant, immunologically effective, operationally feasible and socially acceptable. It is keeping in mind the last point of successful immunization that the present study was carried out to assess the awareness amongst the clientele population about the new optional vaccines and to assess their acceptability in the population. Methods: Study was a cross sectional study carried out in paediatrics immunization clinic of a tertiary care service hospital .A total of 100 parents bringing their children (below 5yr) to immunisation clinic were interviewed as per questionnaire to ascertain their awareness about the vaccines being provided at the clinic. Results: Out of studied population awareness regarding optional vaccines was found to be present in 39% of studied individuals. On associating awareness level with factors affecting it following observations were made. 58% educated individuals were aware whereas none of the illiterates were aware of optional vaccines, they lacked the knowledge of basic purpose of vaccination i.e. prevention from a disease. Joint family structure had a positive effect on awareness of an individual. In relation to occupational status those belonging to working class were more aware (56%) than housewives whose awareness level was 33%. Very few (4%) were unaware of the side effects. Out of studied population 33% made conscious effort to gain further knowledge. Misconceptions regarding vaccination were present only in 3%. Conclusions: Awareness can be raised by improving health education among the general population. Measures can be taken to spread awareness through media as well. Posters and banners showing importance and need of vaccination can be displayed at places like railway station, places of people gathering. Information regarding Optional vaccines should be made available at primary health care level. During pulse polio immunisation programme people can be educated in masses about other important vaccines. ID/63(P) DOTS STRATEGY FOR TREATMENT OF PEDIATRIC ABDOMINAL TUBERCULOSIS IN A TERTIARY HOSPITAL OF SOUTH DELHI, INDIA. Sangeeta Sharma Specialty and Head Department of Pediatrics, L.R.S. TB Institute, New Delhi sangeetasharma2000@gmail.com Setting: Pediatrics Department. TB Institute, Delhi. Objective: To study the efficacy of DOTS strategy for pediatric abdominal tuberculosis patients. Design: Retrospective analysis of 60 children with abdominal tuberculosis. Results: Out of total 60 pediatrics patients of abdominal TB 58 (96.6%) had ascites while 2 (3.3%) had intestinal TB. Mean age was 9.8 years with more female (71.7%) than males (28.3%). A total of 40 children ( 66.6%) were in the age group of 1114 years while 17 (28.3%) were in 6-10 years age group with only 3 ( 5.0%) children were less than 5 years old. Diagnosis was made by ultrasound , CT Scan while aspiration cytology was performed in 26( 43.3%) cases. Cat I, II and III was started 56(%) 4 (%) and 0 respectively Treatment completion rate was seen in 94.6% cases in Cat I as compare to 50% in Cat II. Two patients (3.3%) died with one each in Cat I and II. There were 2 (3.6%) failure in Cat I, and 1 (25%) failure in Cat II. Conclusion: The study confirms the efficacy of DOTS strategy for pediatric abdominal TB in endemic area. ID/64(P) IMMUNOGENICITY AND SAFETY PROFILE OF A 3-DOSE PRIMARY VACCINATION WITH 10-VALENT PNEUMOCOCCAL NON-TYPEABLE HAEMOPHILUS INFLUENZAE PROTEIN-D CONJUGATE VACCINE (PHID-CV) IN INDIAN INFANTS S. Lalwani, S. Chatterjee, J. Chhatwal, V.P. Verghese, F. Shafi, D. Borys , M. Moreira,L. Schuerman. Dept of Pediatrics, Bharati Vidyapeeth University, Medical College, Pune sanjaylalwani2007@rediffmail.com Introduction: Pneumococcal non-typeable Haemophilus influenzae protein-D conjugate vaccine (PHiD-CV; GlaxoSmithKline Biologicals) demonstrated good immunogenicity when coadministered with DTPw-HBV/Hib (GlaxoSmithKline Biologicals) according to the Expanded Program on Immunization (EPI) in the Philippines and Mali. Aims and objectives: This singleblinded, controlled, randomised (2:1), multi-centre study (111188/NCT00814710) assessed the immunogenicity and safety of PHiD-CV following 3-dose primary vaccination co-administered with DTPw-HBV/Hib in Indian infants. Materials and Methods: 360 infants received either PHiD-CV + DTPw-HBV/Hib (PHiD-CV group; N=240) or Hib + DTPw-HBV (control group; N=120) at 6, 10 and 14 weeks of age. Immune responses to pneumococcal serotypes, protein-D and DTPw-HBV/Hib vaccine antigens were measured 1 month post-dose 3. Solicited and unsolicited (local/general) symptoms and SAEs were recorded. Results: For each vaccine pneumococcal serotype, ≥98.3% of PHiD-CV vaccinees reached 22F-ELISA antibody concentrations ≥0.2 g/mL, except for 23F (89.5%) and 6B (77.7%), and ≥95.7% had OPA titres ≥8, except for serotypes 1 (90.5%) and 6B (84.5%). All PHiD-CV vaccinees except one developed measurable antibody levels against protein-D. All infants were seroprotected/seropositive for diphtheria, tetanus, pertussis and hepatitis B, and all except one (control group) against Hib (anti-PRP ≥0.15 g/mL). Incidences of solicited and unsolicited symptoms were comparable between groups, although fever (rectal temperature >38°C) occurred more frequently in the PHiD-CV group. Six infants reported SAEs (five from PHiD-CV group, one from control group), which were not causally related to vaccination. Conclusions: PHiD-CV was immunogenic and well tolerated when administered with DTPw-HBV/Hib to Indian infants in the EPI schedule in-line with previous Malian and Philippinean studies. ID/65(P) DENGUE SHOCK SYNDROME WITH MULTIORGAN FAILURE IN AN INFANT: A SUCCESSFUL OUTCOME Sreenivasan VK, Aparna Gulvadi, S Ramraj Department of Paediatrics, Amala Institute of Medical Sciences, Trichur babuappu@yahoo.com Introduction: Dengue Shock Syndrome (DSS) carries a very high risk of morbidity & mortality especially in infancy. High index of suspicision with appropriate timely intervention especially fluid management is the crux for successful outcome. Case report: A four month old infant presented with history of fever, lethargy, multiple episodes of convulsions, altered sensorium & purpuric rash of two days duration. Father gave a history of viral fever three weeks prior, which was clinically diagnosed as Dengue fever. Mother also had fever on presentation which was eventually proven to be Dengue fever. Infant required ventilator support on admission. Based on evidence of circulatory failure (Weak rapid pulse, narrow pulse pressure, low BP), diagnosis of DSS were considered. Her Hb 13 gm%, Hct 38.5% and Platelet count 55,000 with serum albumin of 2 gm%. X- ray chest confirmed bilateral pleural effusion and ultrasound abdomen ascites. Dengue Ig M was positive. Child was put on volume replacement as per protocol for DSS Grade III, IV. Subsequently there was drop in Hct with improvement in urine output. Patient developed signs of disseminated intravascular coagulation and hepatic failure and was appropriately managed with FFP transfusion, packed cell transfusion, platelet transfusion and anti hepatic failure measures. Over a period of ten days baby improved and was discharged home. Baby is doing well on follow up Conclusion: Management of Dengue is mainly symptomatic. Early identification of the leakage phase, prompt fluid replacement with close monitoring of serial Hb & Hct and urine output remains the cornerstone in successful treatment. Mortality in DSS is very high with liver failure and encephalopathy. Hence DSS is a medical emergency requiring high index of suspicion in endemic areas. ID/66(P) OUTCOME OF ANTIRETROVIRAL TREATMENT IN HIV-POSITIVE ORPHANS VS. NON-ORPHANS AT AN ART CENTRE IN NORTH INDIA Malobika Bhattacharya, AP Dubey, Prasenjit Haldar Department of Pediatrics, Maulana Azad Medical College, New Delhi drmalvikab@gmail.com Study design: Retrospective cohort Method: Children started on ART between September 2005August 2008 were included. Orphan status at ART initiation and baseline demographic, disease and treatment-related variables were recorded. Three monthly absolute CD4 counts, weight-forheight z-scores (WHZ) and height-for-age z-scores (HAZ) of the orphans and non-orphans were retrieved. Children orphaned within the study period were excluded from final analysis. Results: The cohort included 87 children aged 11 months-13 years, a male:female ratio of 1.5:1 and 31 (46.2%) orphans. Majority of the surviving parents (92%) were HIV-positive themselves. Median follow-up was 34 months. After ART initiation, both orphans and non-orphans showed sustained increase in absolute CD4 counts (p<0.0001) with an average gain of 86% after 3 months. After 1year of therapy, <10% in both the groups were still severely immunosuppressed. The baseline WHZ and HAZ scores of the two groups were similar (p=0.21 and 0.62 respectively) and below the standard norms (-1 to +1). The orphans showed a steady increase in both median WHZ and HAZ after ART initiation and both reached +1 at 39 and 42 months of ART respectively. The non-orphans showed identical initial rise in WHZ and HAZ but reduction after 21 weeks of therapy. Conclusions: It is possible to get good response to ART in a resource poor setting. The better outcome in the orphan group implies that the extended family is taking adequate care of these children. Moreover, parental illness may affect care and hence, outcome of the non-orphans, a factor no longer applicable in orphan group. ID/67(O) STUDY OF IMMUNIZATION STATUS OF RURAL CHILDREN (12-23 MO AGE) OF RAJASTHAN AND FACTORS INFLUENCING IT : A HOSPITAL BASED STUDY R Masand, AM Dixit, RK Gupta Department Of Pediatrics, NIMS Medical College, Jaipur-303121 masand.rupesh@gmail.com; masand_rupesh28@yahoo.co.in Introduction: According to the National Family Health survey (NFHS-3, 2005-06), only 44.3% of 12-23 months old children were fully immunized in urban Rajasthan . This rate drops to 22.1 % in rural areas of this state . Aims and Objectives: This study was designed to outline a) The immunization status of children (12-23 months age group) appearing in Pediatric OPD of a Medical College hospital situated in District Jaipur (Rural),Rajasthan b).The factors influencing the immunization status of the study subjects. Material and Methods: Parents of 300 children (who had appeared in the Pediatric OPD of this hospital for various ailments) were interviewed using a preformed questionnaire. Children who had received BCG and three doses of DPT/oral polio vaccine (OPV) and measles vaccine as scheduled in the first year of life were classified as ‘completely immunized’. Those who had missed any dose of the above vaccines were labelled as ‘partially immunized’, and those who had not received any vaccine, except OPV in pulse polio immunization, up to 12 months of age, were defined as ‘non-immunized’. Reasons responsible for partial or non-immunization were recorded. Appropriate statistical tests were performed. Results: Out of the 300 children (176 males, 124 females),100 (33.3%) children were ‘completely’ immunized, 56(18.7%) were ‘non immunized’ and the remaining 144(48%) were ‘partially’ immunized. Out of the 244 completely or partially-immunized children, 231 (77%) had received BCG, 222(74%) received DPT1/OPV1, 197 (65.7%) received DPT2/OPV2, 155 (51.6%) received DPT3/OPV3, and 126 (42%) received measles vaccine. Drop-out rate from BCG- measles was 35% & from DPT1/OPV1- DPT3 / OPV3 was 23.7%. The immunization status varied significantly (p<0.00001) with education of parents, per-capita income, caste, social class of the family, place of delivery & birth order. Distance of the home from the vaccination centre & presence of immunization cards were also significantly associated (p<0.00001). Sex of the child, type of the family and religion had no impact over immunization status (p>0.05).The most common reasons for non-immunization (n=56) were: lack of knowledge regarding vaccines and dose schedule(n=43, 76.7%); Fear of ‘injection’(n=19, 33.9%) ; Busy by profession(n=18 ,32.1%); Health facility was far away from residence(n=14, 25%).The most common reasons for partial immunization (n=144) were: Parents ‘forgot’ the advised schedule (n=58, 40.2%); Adverse effects observed after the previous vaccine(n= 48, 33.3%); Not recalled by the health worker for vaccination (n= 39, 27%); Fear of Injection (n=38, 26.3%). Conclusions: Immunization status of children in rural areas is far below the national health goal of 85% coverage. A herculean effort is required to bridge this gap. ID/68(P) CLINICOPATHOLOGICAL PROFILE OF DENGUE FEVER IN A TERTIARY CARE CENTRE Meetu Rawat Gupta, Aaradhana, Tribhuvan Pal Yadav Department of Pediatrics, Dr. Ram Manohar Lohia Hospital, New Delhi. meetur2007@yahoo.com Introduction: Dengue fever is one of the most important arthropod-borne epidemic fevers. Wide variety of presentation and associated high fatality rate prompted us to present data from our centre. Aim and Objectives: To study clinicopathological profile of dengue fever in children. Material and Methods: Data accumulated between July-November 2009. Results: A total of 168 children mean age 12.74±4.22years and male:female ratio 113:55 were admitted with dengue illness. Average duration of hospital stay was 4.56±2.70days. Clinical manifestations seen were fever(90.48%) of average duration 5.74±3.42days, vomiting(61.90%), abdominal pain(38.09%), edema(4.76%), itching(3.57%) and altered sensorium(1.19%). Bleeding manifestations were present in 56.55% including petechiae(23.21%), melena(20.24%), hemetemesis(10.71%), epistaxis(14.29%), hematuria(1.19%) and gum bleed(5.95%). Clinical examination revealed hypotension(25.59%), decreased pulse pressure(6.55%), erythema(8.93%), rashes(20.24%), hepatomegaly(35.12%) and splenomegaly(12.5%) Investigations showed 15.48% cases with leucocyte count <4000/mm³ and hematocrit >40 in 54.76%. Platelet counts were graded as ≥1lac(10.12%), 50,000-1lac(28.57%), 50,000-20,000(55.95%) and <20,000(5.36%). Liver function test, done in 81 cases showed raised SGOT(96.29%), SGPT(89.41%) and ALP(61.73%). Out of 139 patients in which serum electrolytes were indicated, 105 had dyselectrolytemia presenting as hyponatremia(76.19%), hypernatremia(42.86%), hypokalemia(2.86%) and hyperkalemia(5.71%). Renal profile done in 128 patients were deranged in 25%. Out of total cases, 32.74% were diagnosed as dengue fever, 41.67% dengue haemorrhagic fever and 25.59% dengue shock syndrome. Complications were pleural effusion(19.05%), ascites(17.62%) and gall bladder wall edema(10.71%). 20.24% required blood products and 2.98% required vasopressors. 97.02% recovered and were discharged and 2.98% patients succumbed predominantly secondary to pulmonary complications. Conclusion: Fever and thrombocytopenia were consistent features, giving first hint of the disease. Pulmonary complications are the leading cause of death in these patients. ID/69(P) HOSPITAL INFECTION CONTROL PROCESSES ASSESSMENT FOR STANDARDISATION, ERNAKULAM, INDIA M.A.Mathew, S.Kamath, K.Beena, S.Singh, B.Sonwal Associate Professor, Department of, Pediatrics, MOSC Medical College, Kolenchery, Erankulam 682311 drmathew_11@yahoo.com Aim: IAP and BD have been associated since 2003, primarily on issues that impact human health and injection safety. The journey towards 'Safe-I', started in 2008 when it was decided to upscale from the 'Safe- Injections' workshops that were conducted across 15 medical colleges in Kerala. It was perceived that this program could be expanded under 'infection control processes' with special focus on safe infusion, 'healthcare workers safety and safe biomedical waste management' over and above the safe injection practices. 'Safe –I’ is a certification program for hospitals on infection prevention.Methodology: To assess and suggest hospital infection control, following steps incorporated: &nb sp;1.Application & self- assessment form of hospital sent to Safe-I board 2. Scrutinizing the details by the board. 3. Final assessment dates informed to the hospital, after completion of the requirements. Results: 20 hospitals certified as Safe-I Hospital, 5650 nurses trained on Safe-I 1466 doctors trained on Safe-I , 5650 nurses ensured vaccination Criteria improvement made:Fully functional infection control committee - 90% Hep-B vaccination status - 93% Safety product usage - 60 % Free treatment in case of NSI 100% Awareness to HCW in infection prevention - 90% Protocols for all 5 important criteria 94% Conclusions: The pre-assessment clearly shown that > 90% of hospitals did not have the required criteria in infection control. This project of assessment and certification helped 20 hospitals to improve their infection control practices to meet prescribed standards. This certification is for 2 years. ID/70(P) PILOT STUDY OF AUTOMATED SURVEILLANCE TO MEASURE THE BURDEN OF ROTA VIRUS' IN KUNNATHUNADU, ERNAKULAM, SOUTH INDIA M.A. Mathew, P.Kilgore , S.Chithralekha, A.Paulose Associate Professor, Department of, Pediatrics, MOSC Medical College, Kolenchery, Erankulam 682311 drmathew_11@yahoo.com Aims: Rota virus is an important cause of severe diarrhoeal disease in children. Rotavirus infects children within the first 2 years of life. In India, diarrhoeal disease represents major leading causes of morbidity and mortality. We initiated a hospital -based surveillance to know the incidence and type of Rotavirus prevalence in Kunnathunadu, Kerala,India. Methods: Fecal specimens were collected from all diarrhoeal admissions from children less than 5 years of age and Rotavirus testing was performed. Rotavirus positive specimens were analysed by RT-PCR genotyping assays to determine the distribution of Rotavirus G and P types. Relevant data were collected from parents. Results: During February 2009- August 2010, a total of 1542 stool samples were tested, the overall detection rate of Rotavirus infection was 38% with a seasonal variation of 62% - 8%. highest in February -March 62% and lowest in October - November 8%. Rotavirus occurrence was highest among children aged 6-11 months (48%), followed by children aged 12-33months (38%). 82% of children with Rotavirus were infected by 2 years of age. Combination of intravenous fluids and ORS was the common treatment compared with children having diarrhoea due to other causes. Genotyping results showed that G1 (P8)(54%) followed G9 (P8)(23%). Conclusions: A significant proportion of diarrhoeal admissions were due to Rotavirus and occurred in children below 2 years. This data, despite their limited generalisability, will help policy decisions to introduce Rotavirus vaccines in India. ID/71(P) THE SIGNIFICANCE OF WHITE BLOOD CELL COUNT IN CASES OF ACUTE OTITIS MEDIA (AOM) IN CHILDREN BETWEEN 2 TO 17 YEARS OF AGE. Kumara V. Nibhanipudi, Getaw Hassan JR. Akshat Jain New York Medical College, Metropolitan Hospital Center, New York, NY. 10029 Kumara.nibhanipudi@nychhc.org Objective: To determine whether white blood cell count (WBC Count) may help/aid making treatment decisions in children with uncomplicated acute Otitis media (AOM). Methodology: Children with a clinical diagnosis of AOM between the ages of 2 to 17 years of age were included in the study. All partially treated kids with antibiotics and AOM with ear discharge were excluded. All patients were subjected to a veni-puncture and a complete blood cell count (CBC) with differential was performed, after informed consent from the parents for the study was taken. Pain was assessed using the Pain analog Scale as developed by the NYC HHC (New York City hospital and Health Corporation). Patients with a WBC count >15,000 were given Amoxicillin. Pts with WBC count <15,000 were not given any antibiotic but were given analgesic ear drops. Patients in both groups were given either acetaminophen or ibuprofen for pain relief/or fever reduction in the appropriate dosages. The patients were scheduled for a follow up appointment on the 3rd day and were evaluated clinically. The standard pain analog scale was used for evaluation. Children who did not receive antibiotics initially and still had otalgia, were prescribed antibiotics and those already receiving antibiotics initially, were considered for change of the antibiotic regimen. Pain relief was used as the primary parameter of the study. Results: A total of 100 patients were enrolled in the study. Seven patients with WBC count >15,000 were given Amoxicillin. Out of 7 pts, 6 pts pain resolved completely with (0) pain score on day 3. One out of 7 patients (14%) initially treated with amoxicillin had a pain score of 8 on day 1 and the pain remained at 4 on day 3. This patient’s treatment was changed to Augmentin. 93 out of 100 patients had WBC count <15,000 and were not given antibiotics initially. 90 out of 93 patients had significant improvement in pain severity which came to (0) on day 3. Three out of 93 pts did not have significant pain relief on day 3. All these pts were given amoxicillin. A comparison of the proportions between the groups was analyzed using Fisher Exact Test. Conclusions: The outcome of our study with an objective parameter (WBC Count) could help guide physicians to treat AOM appropriately, by avoiding the unnecessary use of antibiotics without causing significant complication from the disease. This could also reduce the adverse effects of antibiotics as well as the increasing bacterial resistance to common antibiotics. ID/72(P) FROM MICE TO MEN: TRYPANOSOMIA LEWISI INFECTION IN A 37 DAY OLD Archana, Samiksha, Nirmal, Archna, Lab Tec, JP Dept of Pediatrics and Hematology, St. Stephen's Hospital, Delhi dr.archanaverma@gmail.com Trypanosomes were observed in peripheral blood smear from a 37 day old Indian infant displaying fever, anorexia and convulsion during fever episode. Human trypanosomiasis is not endemic in India. Parasite identification was undertaken at Institute of Tropical Medicine, Belgium. Molecular analysis of the blood spot on filter paper and morphology of the trypanosomes on thin slide suggested that the blood was infected with T. lewisi. Trypanosoma (Herpetosoma) lewisi is a trypanosome of the sub-genus Herpetosoma (Stercoraria section), parasite of rats (Rattus rattus and Rattus norvegicus) transmitted by fleas. Rats are infected principally by oral route, through contamination by flea faeces or ingestion of fleas. Our child was treated with Amphotericin B initially. Patient became asymptomatic within 3 days. The parasites in the smear reduced progressively. Injection Pentamidin was started on day 5. The drug had to be imported for the child through the Drug Controller. Based on molecular results, it was concluded that the infant was infected with a T. Lewisi species.