Transperineal repair of persistent rectourethral fistulas using a
advertisement

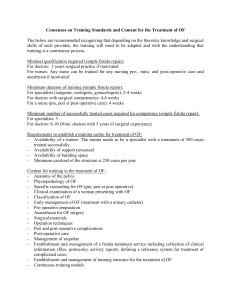
Transperineal repair of persistent rectourethral fistulas using a porcine dermal patch as interposition tissue: preliminary experience Aims of the study: We aimed to describe, for the first time, the technique and results of persistent rectourethral fistula (RUF) repair through a perineal approach using a porcine dermal patch as interposition tissue. Material & Methods: With the patient placed in the lithotomy position, a cystoscopy is performed and the ureters are stented. The fistulous tract is stented to facilitate recognition. The lithotomy position is exaggerated. An inverted U-shaped perineal incision is made outside the anus and inside the ischial tuberosities. The subcutaneous tissue is divided and the central tendon of the perineum transected, thus opening the ischiorectal fossae and exposing the ventral rectal wall. The scarring between the urethra, the bladder and the anterior rectal wall is dissected sharply and the fistulous tract, with the stent passing through it, is identified. The fistula is excised at the level of the rectal wall with the surrounding scarred tissue to create vital margins. The anterior rectal wall is closed in two layers, using continuous 5-0 monofilament sutures. The bladder defect is repaired with interrupted 3/0 suture. A porcine dermal patch is positioned to cover the defect and sutured to the rectal wall ( Figure 1). Results: Two patients with history of recurrent RUF after RP were treated with the technique described at our institution. Mean patients’ age was 68.7 years. Patients had history of previous transurethral resection of the prostate. All patients had undergone a first attempt of trans-abdominal repair of the RUF and had a colonstomy. Operative time was 105.6 minutes (range: 90-120). Mean intra-operative blood loss was 98.7mL (range: 80-110). No intra-operative complications occurred. A cystogram performed on postoperative day 15 excluded pathologic urinary leakages in all cases. The ureteral catheters were removed 4 weeks after surgery and the bladder catheter was removed 2 weeks later. No early- and late post-operative complications occurred. Re-establishment of intestinal continuity was achieved after a mean of 6.5 months. No fistula recurrence occurred at a mean follow-up of 1.1 years. Discussion: RUF is a rare major complication after radical prostatectomy (RP). Management of persistent RUF that have failed previous attempts at repair is technically challenging. The perineal approach provides good exposure of the surgical field. The use of interposition flaps has been reported to enhance fistula healing and prevent fistula recurrence. However, the use of autologous patchs is technically challenging and time consuming. Previous studies have demonstrated favorable results, technical simplicity, safety and efficacy of using a porcine dermal collagen patch as interposition tissue for vesicovaginal fistula repair. Conclusions: According to our initial experience, transperineal repair of persistent RUF with porcine dermal patch interposition is a simple, efficacious and safe procedure. Figure1: Pre-operative, intraoperative and post-operative details