physics and clinical measurement for the primary frca
advertisement

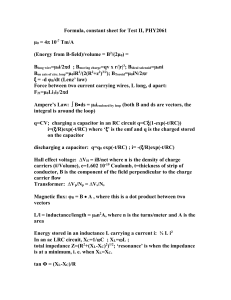
PHYSICS AND CLINICAL MEASUREMENT FOR THE PRIMARY FRCA Ian Wrench - 2002 Electricity Source material: 1.Basic physics and measurement in anaesthesia - Davis, Parbrook and Kenny, fourth edition, Butterworth and Heineman. 2. Electrical safety – JA Langton, Royal College of Anaesthetists Newsletter January 2000 – Issue 50 page 290 – 292. 3. Key Topics in Anaesthesia – TM Craft and PM Upton, second edition, Bios Scientific Publishers. 4. Anaesthesia for patients with pacemakers and similar devices. P Diprose and JM Pierce, BJA CEPD reviews – volume 1, no 6 pages 166 – 170. 5. Electrical safety in the operating theatre. S Boumphrey, JA Langton, BJA CEPD reviews – 2003, volume 3, no1 pages 10-14. 1 CLINICAL MEASUREMENT FOR THE PRIMARY FRCA For the primary fellowship it is necessary to understand some of the principles on which clinical measurement is based. This part of the handout serves as an introduction to this subject area. ELECTRICITY, MAGNETISM AND MONITORING Monitors are designed with a view to producing the best recording possible of a physiological process. For this reason many of the principles of monitoring are concerned with the production of an amplified signal which is as free as possible of interference. Whilst the following account is relevant to all theatre monitoring, the ECG is used as a specific example. First, however it is necessary to understand some basic principles of electricity and magnetism:1) Capacitance - the ability of an object to hold electrical charge (e.g. a capacitor figure 1). Capacitance is measured in farads. A capacitor consists of two plates which are separated by an insulator. When a direct current (DC) is applied, one of the plates becomes positive and the other negative and thus charge is stored (e.g. a defibrillator). A capacitor will not allow the passage of DC across it, however alternating current (AC) may flow. In an operating theatre a capacitor may be formed from an electrical device acting as one plate, the patient as the other and with the air inbetween as the insulator. AC may flow across such a capacitor and act as a source of interference to monitors. 2) Inductance - Electrical current is induced in a wire by movement of the wire relative to a magnetic field (Fleming’s right hand rule). For example an electric generator uses this principle to generate electricity. In theatre many components of electrical apparatus have strong magnetic fields around them and the passage of electrical current through a conductor also causes a magnetic field. As these fields change or as wiring is moved through them so current is induced which may cause electrical interference. 3) Impedance - Whenever the resistance to current flowing varies with frequency it is known as impedance and is measured, as with other forms of electrical resistance, in ohms. When AC flows across a capacitor the impedance diminishes as the frequency of the AC increases. In contrast for an inductor the impedance becomes greater as the frequency increases. Working principle of the ECG 1) The ECG electrode - The ECG signal is picked up by an electrode. Interference may arise at this site in a number of ways. Firstly the signal may produce a chemical change in the electrode which causes it to become polarised altering its impedance and generating a potential which may interfere with the signal. Another possible source of interference is the formation of a battery between the metal electrode and skin moisture. Both of these problems are minimised by the use of the 2 BATTERY CAPACITOR ++++++++++ INSULATOR ---------- Figure 1 – A capacitor. The capacitor plates are charged positively and negatively by the potential difference produced by the battery. The quantity of charge stored is measured in coulombs in the SI system and the capacitance is measured in farads. LAYER OF SILVER CHLORIDE SILVER ELECTRODE GEL WITH CHLORIDE IONS SKIN Figure 2 – The ECG electrode 3 silver/ silver chloride electrode in which a silver electrode is in contact with a silver chloride solution which is in turn in contact with a chloride solution in a gel which is next to the skin (figure 2). The junction between the silver and the silver chloride gives a stable DC potential which does not cause interference. The impedance of the electrode may also be greatly increased by poor contact with the skin which may attenuate the signal. To avoid this problem the electrodes are securely fixed with a sticky pad. 2) The ECG leads - The leads conduct the signal to the ECG machine. Both capacitance and inductance effects may give rise to electrical currents in the leads which may overlie the signal. This interference can be reduced by covering the leads with a metallic mesh which is earthed, a system known as screening. In this way the currents occur in the mesh rather than the ECG leads and are conducted to earth and not to the machine (figure 3). 3) The Amplifier - The biological signal is small and must be increased in size by means of an amplifier. The degree of amplification is known as the gain (figure 4), for example an amplifier which delivers an output power 1000 times greater than the input power is said to have a gain of 1000. For an amplifier as the power of the input increases the power of the output should be similarly raised, this is known as a linear response (see figure 5). The monitoring device contains many different components but provided they all display linearity it is possible to predict the response of the system to a complex signal by breaking the signal down, seeing what effect each part of the signal produces and then adding them up. This simple relationship may however become distorted in the amplifier so that it is not linear over the whole range. It may also happen that the response to an increasing power is different to that of a decreasing one, an effect known as hysteresis (figure 6). In order that the correct response is recorded it is important that allowance for these variations is made in the design of the ECG machine. Amplifiers usually measure the difference in potential between two sources looking at the signal from two different directions (differential amplifiers). In this case the biological signal will be different from each source whereas any interference will be the same. By disregarding the common signal, only the biological one is amplified, this is known as common mode rejection ratio. For the ECG the biological signal lies within a range of frequencies which is 0.5 to 100 Hz. In order to produce the best image, the amplifier should have a bandwidth which responds to this range of frequencies. The bandwidth of the amplifier is the range of frequencies over which the amplification is relatively constant. Sometimes the bandwidth of the amplifier is restricted so that frequencies where interference is likely to occur are not included. For example, high frequency interference from muscle movement for the EEG is minimised by excluding these frequencies from the amplifier bandwidth. It is important to have an amplifier with a high input impedance relative to the signal source. If the input impedance of the amplifier is low then this results in attenuation of the input signal. The skin impedance is reduced by using electrode gel 4 Screening Mesh ECG Monitor ECG Electrode Earth Figure 3 – A mesh surrounds the ECG electrode and conducts away interference to earth (screening). Amplifier Figure 4 - The degree of amplification is the gain and the range of frequencies to which the amplifier responds is the bandwidth. The power of the output increase with the power of the input although the relationship is not always simple (see figures 5 & 6). The amplifier must have a high input impedance relative to the signal source or the signal may be attenuated. The amplifier converts the physiological analogue signal to digital information via an analogue to digital converter so that the signal may be processed. Sufficient data is stored in the random access memory to fill the ECG screen. 5 Power of input Power of output Figure 5 – An amplifier for which there is a proportionate increase in output for an increase in input. This is an example of a linear response. Power of input Power of output Figure 6 – An amplifier which displays hysteresis. The response to an increasing power is different to a decreasing power. 6 and ensuring that there is good contact with the skin. Additionally most modern amplifiers have a very high input impedance to get around this problem. Amplifiers contain semiconductors that are used in components such as transistors and diodes. The conductivity of semiconductors varies with temperature leading to inaccuracy, for example if equipment becomes heated. This phenomenon is known as drift. Using an amplifier that is designed for AC rather than a DC potential considerably reduces this problem. 4) The display - Most modern monitors make use of microprocessor technology which uses digital information. The physiological signal is analogue (a continuous scale) and must be converted digital (a discontinuous scale – “yes” or “no” data) by means of an analogue to digital converter. Sufficient ECG data is then stored in the random access memory to fill the screen. As the latest information is stored so the oldest is lost to produce a rolling display. If the display is via a cathode ray tube then the data must be converted back to analogue using a digital to analogue converter. However, this is not necessary for a liquid crystal display that can use digital information. In more sophisticated monitors further analysis of the trace may be performed such as ST segment or arrhythmia analysis. Algorithms may be programmed in so that the machine alarms if certain parameters are exceeded. Despite the measures to reduce interference, this may still occur and is referred to as noise and the amount of noise the noise to signal ratio. The noise to signal ratio can be improved by averaging a repetitive waveform. The interference is random and is averaged to zero leaving the signal alone. Diathermy is a particularly troublesome source of noise the effects of which may be reduced by the use of a high frequency electronic filter. 7 ELECTRICAL SAFETY FOR THE PRIMARY FRCA How electricity is supplied: Substation Wall socket and plug Live Wall Neutral Earth Apparatus Earth Figure 7 – Electricity emerges from the substation and flows to apparatus via the wall socket/ plug. The neutral wire completes the circuit back to the substation. Electricity may flow back to the substation via an alternative route if a connection is made from the live wire back to earth. This will only happen if there is a fault with the apparatus or the apparatus is not used correctly. If this route to earth is via a person then they are electrocuted. Electrocution When faulty apparatus allows electricity to flow through the anaesthetist to earth, the greater the impedance the smaller the current (current = potential/ impedance). The impedance is mostly due to foot wear and the floor. With the standard 240 volt supply, if the impedance is 240 kilo ohms or more then the current is 1 mA - i.e. relatively small and harmless. If the impedance is only 10 kilo ohms or less then the current is 24 mA which is enough to stop the anaesthetist letting go and may cause ventricular fibrillation (VF). The impedance of footwear is recommended to be between 75 kilo ohms and 10 mega ohms to reduce the risk of electrocution whilst allowing the dissipation of static electricity. The set limits for electrical resistance for anaesthetic flooring (defined as the resistance between 2 electrodes 60 cm apart) are 20 kilo ohms to 5 mega ohms. Skin impedance is very low and made lower by moisture and a large surface area of contact with the electrical source. These factors become important if for some reason the impedance of the footwear is low. With regard to a patient in theatre, if their skin is in contact with earthed equipment this provides a route from faulty live apparatus to earth. The impedance is likely to be low so that a dangerously high current may flow in the patient. The risk of VF with an electric shock is increased by - timing with the T wave of the ECG, a relatively low frequency (e.g. mains - 50 Hz) and CVS disease. 8 Classification of electrical equipment (British Standard 5724). Class I - Any accessible conducting parts are connected to earth. If the live supply connects to these parts an abnormally high current flows from live to earth resulting in melting of the fuses in the live wire. Class II - The equipment is double insulated so that it is impossible to touch the live wire. There is no earth wire. Class III - The equipment is internally powered (e.g. batteries). Any electric shock would not be as harmful as from the mains. Any of the above class of apparatus may contain floating circuits that are not earthed and are electrically isolated from the rest of the equipment by transformers. Even so the alternating current of mains electricity can produce small electrical currents through inductive and capacitative effects. These small currents are known as leakage currents - they will usually be small but may lead to microshock. Leakage currents may lead to microshock to the heart if conducted down a wire in close contact with it. This may lead to VF or damage to the heart. This may occur with cardiac pacemakers, cardiac catheters or a temperature probe in the lower third of the oesophagus. Damage is caused by these small shocks (around 100 μA) because the current density in the myocardium is equal to that of a generalised 24 mA shock. The current may arise from faulty equipment and find a route to earth through the endocardial wire. Classification of equipment for leakage currents All equipment is tested for leakage currents in the event of a fault. For equipment that contacts the heart the classification is CF (F is for floating circuit) and the leakage current should be less than 10 μA. For other medical monitoring equipment the classification is B or BF if it contains a floating circuit. For B or BF the maximum permitted leakage current if 100 μA Equipotentiality Different pieces of equipment may operate at different potentials, electricity may therefore flow from the higher to the lower potential via a user causing an electrical shock. To avoid this, the terminals of each piece of equipment in a stack are connected so they are all at the same potential. Pacemakers There are 2 types of pacemaker - temporary with an external wire and permanent that are contained within the patient and are battery powered. Usually pacemakers have a demand mode. Theoretically interference from an external source of electromagnetic radiation may be misinterpreted as a QRS complex causing the pacemaker not to produce a stimulus. As a general rule with pacemakers no diathermy is best followed by bipolar which is in turn theoretically safer than unipolar although the risks are small. Many pacemakers switch to a fixed mode if there is excessive interference as a safety measure. However, most modern pacemakers will function normally during surgery provided the diathermy plate is kept well away from them so that the diathermy current does not flow towards them. Important exceptions are those pacemakers that cardiovert or defibrillate. These pacemakers may interpret diathermy 9 as ventricular fibrillation or a tachyarhythmia and shock the heart unnecessarily. Such pacemakers should have this facility discontinued prior to surgery. Formerly it was the case that an external magnet could be applied to a pacemaker to convert it to a fixed mode of 70 beats per minute. However, the application of an external magnet may be harmful to a modern pacemaker and should no longer be used. Radiotherapy may also damage pacemaker circuits if directed at them and the use of flecainide may elevate the threshold required to trigger depolarisation so that the pacemaker no longer works. Other factors which may rarely be sources of interference include lithotripsy, factors which may cause lead displacement (IPPV, shivering, patient position), factors which may confuse the rate modulator (shivering and fasciculation) peripheral nerve stimulators, and TENS. Should a patient with a pacemaker in situ require defibrillation then it is important that the pads are positioned appropriately: Pacemaker Defibrillator pads Figure 8: Correct positioning of defibrillator pads with the pacemaker sited below the left clavicle (taken from manufacturers recommendations). The pads should be reversed if the pacemaker is on the other side. However, some texts suggest that defibrillation should be at 90 degrees to the pacing wire (paddles front and back). Mobile phones All medical electronic equipment may behave as a radio receiver at a number of frequencies. These frequencies are difficult to predict. Mobile phones, even in standby mode, send signals to the base station. If the frequencies that the mobile phone is using match those of medical equipment in the vicinity then interference may occur. To prevent this it is recommended that mobile phones should not be switched on within 10 metres of medical equipment. 10 DIATHERMY Diathermy involves the passage of a high frequency current (usually 1 megaHz) through the patient in order to cause cutting/ coagulation. A sine wave is used for cutting diathermy and a modulated waveform for coagulation diathermy. The frequency must be high as low frequency current may cause muscle contraction and VF. In unipolar diathermy the cutting probe in contact with the patient has a small tip and thus the current density is high and so is the degree of tissue damage. Also attached to the patient is a patient plate that completes the circuit back to the diathermy machine. The area of the patient plate is large so that the current density is small and there is no tissue damage. The patient plate is attached within the diathermy machine to an isolating capacitor. The diathermy current which is of high frequency flows easily across the capacitor (impedance decreases with increasing frequency of current) whilst the lower mains frequency is subject to a much higher impedance. In this way the patient plate is prevented from becoming a route to earth through which a current from faulty equipment may be conducted. Diathermy Machine Isolating capacitor Patient Earth Patient plate If the patient plate is not properly attached then the current may flow to any point where the patient is in contact with a conducting surface. In this circumstance the current may also flow by capacitance effects in the absence of direct contact. In an alternative arrangement there is no isolating capacitor and the diathermy is not earthed at all. This is called a floating or isolated circuit. There is still a risk of burns with stray capacitance linkages however. Modern ECG’s also contain floating or isolated circuits to avoid providing a route to earth for any stray currents. The amplified signal then passes into the rest of the equipment through isolating transformers which ensure electrical isolation. In older models the reference or neutral lead was earthed through the casing and electrocution could occur. In bipolar diathermy there is no patient plate as the current is conducted between the two prongs of the diathermy forceps. Bipolar diathermy is relatively low power and is therefore used for delicate work only. 11 ELECTRICAL SYMBOLS Capacitor Battery Inductor Resistor Diode (rectifier) – converts AC to DC e.g. used in a defibrillator to allow AC mains current to charge the capacitor. Amplifier Earth Transformer Class 2 equipment (double insulation) Floating circuit Switch On/ Off switch High Voltage equipment Hazard – read instructions before use Equipment which is safe to be connected to patient during defibrillation 12