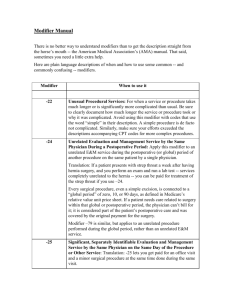
understanding & coding with modifiers
advertisement

UNDERSTANDING & CODING WITH MODIFIERS
-21
Prolonged Evaluation and Management
When the service provided is prolonged or otherwise greater than that usually required for the highest level of service in a
given category.
An office visit that usually requires 45 minutes to 70 minutes to complete. (This modifier may only be used with the
highest levels of service for E&M codes.)
Correct coding:
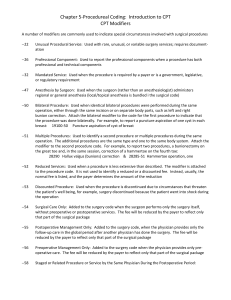
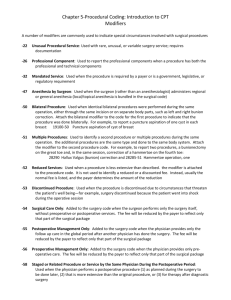
-22
99215-21
(Established patient office visit)
Unusual Procedural Services
When the service provided is greater than the time or service usually required for the procedure.
A surgical procedure that usually takes 1 hour took 3 hours. A report or summary should accompany the claim to explain
the reason for the increase in charges.
Correct coding:
-23
58180-22
(Supracervical abdominal hysterectomy)
Usual Anesthesia
Occasionally, a procedure that usually requires either no anesthesia or local anesthesia must be done under general
anesthesia because of unusual circumstances. This situation is reported by adding modifier -23 to the procedure codes of the
basic service.
During a sigmoidoscopy, the patient required general anesthesia.
Correct coding:
-24
45330
45330-23
Sigmoidoscopy, flexible
General anesthesia applied
Unrelated Evaluation and Management Service by the Same Physician during a Postoperative Period
Use this modifier when the physician needs to indicate that an E&M service was performed during a post-operative period
for a reason unrelated to the original procedure.
A patient had gall bladder surgery but came to the office because of a cold 3 weeks following that procedure (same
physician). By using this modifier, the coder alerts the carrier that the office visit was not related to the surgical procedure.
The physician will then be paid for the visit pertaining to the cold.
Correct coding:
-25
________________
_____________________________
Significant, Separately Identifiable E&M Service by the Same Physician on the Day of a Procedure
This modifier indicates that on the day a procedure or other service was performed, the patient's condition required a
significant, separately identifiable E&M service in addition to the usual preoperative and postoperative care associated with
the procedure.
1
Patient was seen for a sore throat and removal of a wart. Both services (the office visit and the procedure) could be coded
because the office visit (sore throat) was unrelated to the reason for the surgery.
Correct coding:
-26
________________
________________
_____________________________
_____________________________
Professional Component
Certain procedures are a combination of a physician component and a technical component. To report only the physician
component, add this modifier to the CPT code number.
The patient has had a chest x-ray. and the physician is only interpreting the film.
Correct coding:
-32
________________
________________
_____________________________
_____________________________
Mandated Services
This modifier applies to mandated consultation and services related to mandated consultations.
Correct coding:
-47
________________
_____________________________
Anesthesia by Surgeon
Use this modifier to code regional or general anesthesia provided by the surgeon. Do not use it to code for local
anesthesia.
The surgeon who drains this patient's cyst also administered the regional anesthesia.
Correct coding:
-50
________________
_____________________________
Bilateral Procedure
When the same procedure is performed on both sides of the body use this modifier to indicate that service. The
modifier is appended to the second procedure.
This patient has two hernias. one in the right groin and one in the left
Correct coding:
-51
________________
________________
_____________________________
_____________________________
Multiple Procedures
When multiple procedures other than E&M services are performed on the same day or at the same session by the
same provider, the primary procedure or service may be reported as listed and the additional procedure reported
2
with the multiple procedures modifier.
The surgeon removed the patient's uterus and also cut an opening into the bladder and drained it.
Correct coding:
-52
________________
________________
_____________________________
_____________________________
Reduced Services
Under certain circumstances, a service or procedure is partially completed. This modifier alerts the carrier that a
reason exists for a lower-than-usual charge. The reduced services modifier will protect the charge data for the
practice.
Noninvasive physiologic studies of upper or lower extremity arteries, multiple levels or with provocative
functional maneuvers, complete bilateral study (e.g., segmental blood). The study was performed on a patient
who has a history of amputation of the extremity.
Correct coding:
-53
________________
________________
_____________________________
_____________________________
Discontinued Procedure
The physician may need to terminate a procedure due to extenuating circumstances or terminate those that
threaten the well-being of the patient. Note: This modifier is not used to report the elective cancellation of a
procedure before patient's anesthesia induction and/or surgical preparation in the operating suite.
Physician began a colonoscopy but had to discontinue the procedure because the patient had not been properly
prepped
Correct coding:
-54
________________
_____________________________
Surgical Care Only
This modifier indicates that one physician performed a surgical procedure and another physician provided
preoperative and/or postoperative management.
The physician performed only the laminectomy.
Correct coding:
-55
________________
_____________________________
Postoperative Management Only
This modifier indicates that a physician other than the surgeon provided the postoperative care.
The physician provided the postoperative management for a laminectomy performed by another physician
Correct coding:
________________
_____________________________
3
-56
Preoperative Management Only
This modifier indicates that a physician other than the surgeon provided the preoperative evaluation of the patient.
The physician provided the preoperative evaluation for a laminectomy performed by another physician.
Correct coding:
-57
________________
_____________________________
Decision for Surgery
Use this modifier for an evaluation and management service that resulted in the initial decision to perform
surgery. It applies only to major procedures (those with a 90 day global period) when surgery is performed
within 24 hours of the decision for the surgery.
The patient saw the surgeon, and the decision was made for surgery the next day.
Correct coding:
-58
________________
_____________________________
Staged or Related Procedure or Service by the Same Physician during the Postoperative Period
This modifier is used when the physician needs to indicate that a procedure or service performed during the
postoperative period was planned prospectively at the time of the original procedure (staged), was more extensive
than the original procedure, or was performed for therapy following a diagnostic surgical procedure.
Patient had breast biopsy. Results indicated a need for a partial mastectomy. The service was scheduled within
the 10-day global period of the biopsy.
Correct coding:
-59
________________
_____________________________
Distinct Procedural Service
This modifier indicates that a procedure or service was distinct or independent from other services performed on
the same day. It is used to identify procedures or services that are not normally reported together but are
appropriate under the circumstances. It may represent a different patient encounter, different site or organ system,
separate lesion, or separate injury not ordinarily encountered or performed on the same day by the same physician.
Removal of a lesion from the arm and another lesion from the back.
Correct coding:
-62
________________
________________
_____________________________
_____________________________
Two Surgeons
Under certain circumstances two surgeons (usually with different skills) may be required to manage a surgical
procedure.
Laminectomy performed by a neurosurgeon and an orthopedic surgeon. Each bills the same CPT code with
4
modifier –62.
Correct coding:
-63
________________
_____________________________
Procedure Performed on an Infant Weighing Less than 4 kg
In some cases, the small size of an infant significantly increases the complexity and physician work
components required for a procedure. This modifier is only used for procedures on patients in this
circumstance.
The patient is a 3-kg infant who requires an enterectomy, resection of small intestine.
Correct coding:
-66
________________
_____________________________
Surgical Team
Used when highly complex procedures (requiring the concomitant services of several physicians, often of
different specialties, plus other highly skilled, specially trained personnel, various types of complex equipment)
are carried out under the .”surgical team” concept
A heart transplant involves the skills of a highly trained cardiovascular team
Correct coding:
-76
________________
_____________________________
Repeat Procedure by Same Physician
Use this modifier when a physician needs to indicate that a procedure or service was repeated subsequent to the
original service on the same day.
Patient had an EKG in the morning with a repeat EKG in the afternoon.
Correct coding:
-77
________________
_____________________________
Repeat Procedure by Another Physician
This modifier indicates that a procedure had been performed by another physician on the same day and was
repeated by a different physician.
Patient had an EKG at the primary care physician's office and was sent to a cardiologist that same day who
repeated the EKG on the same day.
Correct coding:
-78
________________
_____________________________
Return to the Operating Room for a Related Procedure
This modifier indicates that another procedure, related to the first procedure, was performed during the initial
procedure's postoperative period and required a return to the operating room.
5
The patient had abdominal surgery. Three days after surgery an infection occurs in the wound site, requiring the
patient to be returned to the operating room for debridement of the wound site.
Correct coding:
-79
________________
_____________________________
Unrelated Procedure or Service in a Postoperative Period
When a patient is seen by the same physician for an unrelated problem or condition in a postoperative period, use
this modifier.
A patient has a Maze procedure for treatment of atrial fibrillation. The patient goes home; the wound site is
healing well. Two weeks later, the patient is seen by the same physician for pericardiotomy for removal of
foreign body. Since the second procedure is within the global period for the original surgery, attach modifier -79
to the second procedure.
Correct coding:
-80
________________
_____________________________
Surgical Assistant
This modifier identifies the services of another physician, who acts as a second pair of hands during a surgical
procedure.
A patient is treated for an intestinal fistula closure, which required the assistance of another physician to complete
the procedure. The primary surgeon reports the service. To report the services of the assistant you would add
modifier -80 to the code.
Correct coding:
-81
________________
_____________________________
Minimum Assistant Surgeon
Use this modifier for a procedure that does not normally require a surgical assistant but because of extenuating
circumstances, requires the services of another physician for a short time.
Note: Many commercial insurance companies allow this modifier to be used when assistance is provided by
personnel other than an MD or DO. For Medicare carriers, you must use modifier -AS to report services provided
by an assistant who is not an MD or DO.
A patient is treated for gingivitis requiring Gingivectomy, excision gingiva, each quadrant. The assistance of
another physician was required for a short period of time to complete the procedure. Using the same example, if the
physician had used a nurse practitioner or physician assistant for help with this service you could apply modifier -81 with
some commercial carriers.
Correct coding:
________________
_____________________________
6
-82
Assistant Surgeon
Use this modifier when a qualified resident surgeon is not available. This modifier is typically reserved for
teaching hospitals and teaching physician services
A teaching physician required assistance for the closure of an intestinal fistula. At the time of the procedure, a
resident was not available to provide assistance. Another teaching physician was called to provide surgical
assisting.
Correct coding:
-90
________________
_____________________________
Reference (Outside) Laboratory
This modifier is used when laboratory procedures are performed by a party other than the treating or reporting
physician. Only use this modifier with the 80000 code series.
A patient with Conn's disease is scheduled for aldosterone studies in the morning and in the afternoon to compare
results of electrolyte excretion by the kidneys.
Correct coding:
-91
________________
_____________________________
Repeat Clinical Diagnostic Laboratory Test
Used to indicate a repeat of the same laboratory test on the same day to obtain subsequent (multiple) test results.
Note: This modifier may not be used when tests are rerun to confirm initial results; when testing problems with
specimens or equipment occur; or for any other reason when a normal, one-time, reportable is all that is required.
This modifier may not be used when other code{s) describe a series of test results (e.g., glucose tolerance tests,
evocative/suppression testing)
Patient's test results for aldosterone are inconclusive, so the lab runs the test again.
Correct coding:
________________
________________
_____________________________
_____________________________
7