History of Early Dengue Researcg before 1950—Narrative
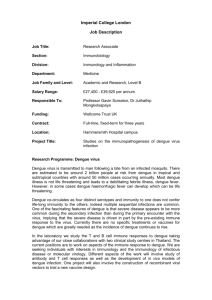
advertisement
1 History of Early Dengue Research before 1950—Narrative (Prepared by G. Kuno, September 16, 2009) Information about the slides: For many of you, presentation of historic events in seminar may be refreshingly different, since today we are too often accustomed to attending seminars or lectures where only recent, original research data are presented. This presentation is definitely not designed to burden the audience to digest new data or difficult concepts. This set of slides was prepared in a story-telling (show-and-tell) style. All slides are simple, self-explanatory or self-evident. You can relax and just watch slides. Obviously, the major casualty of such a style of presentation is any subject that requires presentation of highly complicated data, which, by necessity, requires a far lengthy explanation. Often, these subjects are more scientifically important. Unfortunately, they are unsuitable for the types of simple presentation this set of slides was designed for and, therefore, excluded as much as possible because of limited time allotted. Despite the exclusion, this set of slides was prepared to cover practically all subjects of major importance in the early history of dengue research. This set of slides may be presented in multiple lectures or seminars, by selecting specific topics per presentation. If presented without any modification, the set has a sufficient information for as many as 4 presentations, assuming one hour-meeting consisting of 45 minutes talk followed by 15 minutes of discussion. For some slides, this narrative is too long, because a lot of background information is provided. For these slides, speakers can cut short and talk briefly only the essentials, reserving the rest of the background information for discussion. PowerPoint slides provide speakers a tremendous flexibility. Speakers can modify according to their taste or emphasis by reorganizing, revising and/or by inserting another slides of choice, as they wish. Time constraint is another factor for consideration for modifications of narrative or selection of topics. The source references or materials used in this set are all in public domain; and one does not need to be concerned about copyright issues. However, regardless of how speakers modify the slides, please make sure that the correct sources are shown clearly on the slides, if the materials were originally produced by someone other than the speakers. Nearly all sources identified in the narrative only by author and year are found in the following publications: (1) Kuno, G. A bibliographic database on dengue. U.S. Dept. Health and Human Services, San Juan, Puerto Rico; 1993; (2) Kuno, G. Clin. Microbiol. Rev. 22:186; 2009. For others, full texts of most dengue references cited in the slides are obtained from the online library at http://www.afpmb.org. [1] Title. 2 Currently, dengue is unquestionably the number one vector-borne arbovirus in terms of the morbidity and mortality, magnitude of global public health problem, amount of funding for research, number of publication per annum or of the researchers, the complexity of unraveling the pathogenesis of severe syndromes, and of the unique difficulty of developing effective vaccines. Despite the enormous importance of dengue today, however, compared with the early history of yellow fever research, which is widely known not only by the contemporary researchers but in general public because of abundantly available books and other easily available documents, the early history of dengue research is poorly understood even among active dengue researchers today. [2] Early dengue investigation in the shadow of yellow fever research. As most virologists know well, historically, yellow fever research preceded dengue investigation. Although both YF and dengue are transmitted in urban areas by the same vector, Aedes aegypti, there are interesting contrasts that explain why dengue research evolved in the shadow of yellow fever research. The history of yellow fever outbreaks in Europe and North America has been well documented for more than a few centuries ever since the contact with tropical countries by the people in the temperate climate began. Because YF has captured the interest of people with its devastating socio-medical-economic impacts, the enormously fascinating and dramatic events including tragic deaths during YF investigations in Cuba and West Africa, and major scientific accomplishments not only during the Walter Reed Commission investigation in Cuba at the turn of the 20th century but also thereafter leading up to the development of an effective YF vaccine in 1937 by Max Theiler, so many books have been published, and the whole history of YF has been immortalized in medical history ever since. Even those not in microbiological professions publish books about something related to the history even today. Because of its popularity, some of the legendary figures in YF history were featured in commemorative stamps issued in several countries; and Hollywood made a movie, Yellow Jack, which was followed by a Broadway adaptation and TV dramatization. But, for dengue history similarly rich in fascinating events and important discoveries made in the tropics, no single book has ever been published, as far as I remember. No commemorative stamp has ever been issued, and of course, no Hollywood movie has been released. Do those dengue researchers deserve such a neglect? [3] Reminder. In this presentation, except for a small number of laboratory-confirmed outbreaks, “dengue” refers to either true dengue or “dengue-like illness”, because in the early history, 3 no reliable laboratory confirmation technique by today’s standard was available. As I mention later, diagnosis based on clinical manifestation has been a topic of controversy. The period covered in this presentation primarily (but not exclusively) falls between 1890 and 1950. [4] Important events: 1897-98. Now, I must turn the clock back to the 1890s. This last decade of the 19th century turned out to be extremely important for us, arbovirologists, for several reasons. Important scientific discoveries were reported in this decade, in particular between 1897 and 1898. First, it was discovered by Loeffler and Frosch in 1898 that foot and mouth disease was caused by a new infectious disease entity, or “filterable agent [=virus].” Remember, 1890s was still in the golden age of bacteriology, and non-bacterial infectious agents as causes of animal diseases was an anomalous, new concept that was not readily accepted by most microbiologists then. Second, Ronald Ross discovered malaria transmission by mosquitoes. That followed the early discovery of filarial transmission by mosquitoes by Patrick Manson in the 1870s in Asia. These discoveries firmly established that some of human diseases could be carried by arthropods. Third, the fortuitous discovery of extrinsic incubation period by Henry Rose Carter in 1898 during his keen observation of YF outbreak in Mississippi provided a crucial information which Carlos Finlay in Cuba did not have to complete his otherwise near complete theory on mosquito-borne transmission of YF. Fourth, Sanarelli’s controversial bacterial etiology of YF disturbed medical communities and stimulated physicians and microbiologists to pay a more serious attention to the etiology of YF. Fifth, the huge dengue outbreaks in Galveston and Houston in 1897 reminded medical communities in the US that there were a lot more infectious disease problems to be concerned besides YF. Then, on top of these events, an important political event took place—Spanish-American War of 1898. With this war, United States had to confront for the first time with a host of unfamiliar tropical diseases (with the only exception of YF) prevalent in the former Spanish territories . It should be clearly understood that, at that time, US was far behind the European colonial powers in terms of medical research on tropical diseases, because US, unlike several major European countries with a long history of colonization and hence medical experience to deal with tropical diseases, did not have a colonized territory in the tropics until that time. [5] George Miller Sternberg. 4 As a result of this war, US acquired former Spanish territories in the tropics. This necessitated the country to deal with unfamiliar tropical diseases. The responsibility fell on the shoulder of then surgeon general, George Sternberg. He was an accomplished bacteriologist and has been called the father of American bacteriology. [6] U.S. military’s two sites of tropical disease investigation. The US military established two investigative boards (or commissions) of tropical disease investigation, one in Havana to deal exclusively with yellow fever and the other in Manila of the Philippines to deal with a variety of diseases, in particular malaria, plague, and dengue. Both sites are shown in orange dots on the map. [7] Walter Reed. The man chosen to lead the investigation of YF in Havana was none other than Walter Reed. Because he is such a legendary figure, I guess many in the audience know quite well who he is and what he did. Usually, in a gathering of 20-50 microbiologists, always there are a few individuals deeply knowledgeable about his YF investigation. So, I do not need to elaborate at all. Here, it suffices to introduce just two individuals during the Walter Reed Commission era (1900-1901) to make a connection between YF and dengue research histories. [8] Clara Maass. Clara Maass was the head nurse at the German Hospital in Newark, New Jersey. When the Spanish-American War broke out, military was ill prepared to deal with wounded or sick soldiers. So, it recruited volunteer nurses and physicians. She was one of many contract nurses hired. She first served in a few military camps in the US and was then shipped to Santiago, Cuba. Because YF was very prevalent at that time, she must have attended soldiers sick of YF there. However, the duration of the War was unexpectedly brief, and she was discharged. Then, she volunteered in the military service again. This time, the US military shipped her to Manila. There, she cared for malaria and dengue patients, among others. But, after several months, she contracted dengue herself. Worried about her health, military quickly sent her home. Undaunted, she volunteered again. This time, she received a telegram from William Gorgas, then chief sanitation officer in Havana during the Walter Reed Commission investigation, to report to duty immediately. So, she set sail to Havana and began to care for the YF patients at that historically famous Las Animas Hospital. By mid-1901, much of the Commission studies were completed and many members of the Commission returned home. However, some, including James Carroll and others, stayed to carry on supplemental human experiments. She was one of the volunteers in one of those human experiments so-called Gorgas-Guiteras experiment for devising an immunization protocol based on attenuation. She was exposed to blood-engorged mosquitoes several times but did not develop illness. So, the physicians thought she was somehow immune to YF. 5 They were dead-wrong. In her last exposure to mosquito bite in August, 1901, she developed a full-blown YF and died 10 days later. She was only 25. The uproar that followed in the aftermath of her tragic death put an end to all human experiments for the YF investigation by the US military. Anybody who lived in northern New Jersey may still remember Clara Maass Medical Center established in honor of her dedication. [9] Charles Franklin Craig. Everybody who attended annual meeting of the American Society of Tropical Medicine and Hygiene probably heard Charles Franklin Craig lectures given by distinguished speakers chosen. Craig was one of the pillars of American tropical medicine, specializing in parasitic diseases. However, I guess, that few people know the fact that he had a brief career in YF and dengue research. He was hired as a contract surgeon by the military during the Walter Reed Commission period. He, like Clara Maass, served in a few military bases in the US before he was sent to Havana and assigned to the Columbia Barrack where Walter Reed began his historic investigation. Although I never found any documents about Craig’s activities there during this period, he must have been assigned to do something about care of YF patients, because that was the only business there and because his biography clearly records his presence in that Barrack at that time. A few years later, he enlisted formally in the military and was sent to Manila. There, in 1906-07, teamed up with Percy Ashburn, he determined for the first time that the etiologic agent of dengue was also virus. [10] Vector-borne transmission of human diseases. The biological transmission, the very basis of all human experiments in dengue investigation in early history was made possible because of earlier contributions by Manson, Ross, Finlay, Carter, and Reed. Without the knowledge accumulated by those pioneers, dengue experiments could not have been possible. Some of those who made great contributions are shown in the following slides more or less chronologically. [11] Patrick Manson. He is regarded the father of tropical medicine. His discovery of filarial transmission by mosquitoes was a historic discovery. When he was in Xiamen, China, in 1872, a dengue outbreak occurred. His clinical definition of dengue was based on his observation in that outbreak. [12] Ronald Ross. I already mentioned the importance of his discovery of malaria transmission by mosquitoes. Although he received Nobel Prize, one of the crucial observations he made was based on an invaluable suggestion by Patrick Manson. [13] Carlos Juan Finlay. Not much introduction is necessary, since his contribution in YF investigation is legendary. His theory was almost complete, except that he lacked one piece of crucial 6 information, extrinsic incubation period. Because of the lack of this knowledge, all his attempts to transmit YF with mosquitoes failed. [14] Henry Rose Carter. During an YF outbreak in Mississippi in 1898, he assigned an assistant to meticulously record occurrence of YF cases in households in the context of family relation and of location. The record convinced Henry Carter to deduce that a period ranging from several days to as long as 3 weeks elapsed between the first cluster of cases and the next cluster of cases. This is what is known now as “extrinsic incubation period required for virus to replicate sufficiently in mosquitoes, optimizing them to be infective upon bite on susceptible humans. Adoptation of his fortuitous discovery to complete the hypothesis of Carlos Finlay was crucial to the success of the Walter Reed Commission studies in Havana. [15] Etiologic investigation regarding transmission mechanism of dengue. At the turn of the 20th century, the guiding principle in etiologic investigation was Koch’s postulates. For that reason, dengue investigators tried to isolate a putative dengue agent from patients, propagate it in suitable animal hosts or in humans, re-inoculate the samples from these inoculated animals or humans back to normal humans, to reproduce the dengue syndrome. Because use of humans was always dangerous, researchers looked for alternative animals for model, but in vain. The need to strictly adhere to the Koch’s postulates probably was one of a few reasons why they did not look for dengue virus in mosquitoes during outbreaks as a source of dengue agent and relied only on humans for the source of virus as well as for transmission experiment. This is also due to the fact that the role of mosquitoes in dengue transmission was poorly understood in the early history of dengue research. Thus, one had to wait until 1958 when dengue viruses were isolated from wild mosquitoes during a hemorrhagic dengue outbreak in Manila by William Hammon. [16] Experimental design for dengue transmission studies. In the early period of dengue transmission studies, like in yellow fever investigation, initially human experiment was the basic approach; but with a growing knowledge of the role of mosquito vectors, the importance of mosquito in transmission experiments rose. Then, to conduct human experiments in dengue endemic locations, first, investigators needed to decide which kind of infectious samples they could (or would like to) use. The first kind was blood sample of acutely-ill patient. Hopefully, the patient at the time of blood sampling was viremic. However, at that time, investigators did not know well about the correct timing of viremia period, because it was unknown and had to be determined in human experiments. Selecting a proper location for human experiment was also an inseparable issue. By selecting fresh blood, researchers had to set up a laboratory right in the endemic area in the tropics. But, that compromised the validity of the experiment, because there was no guarantee that the volunteers of human experiments were free of dengue or not exposed to infective mosquitoes prior to human experiments, given abundance of vector mosquitoes everywhere. For this reason, investigators chose to build a laboratory made 7 mosquito-proof. Besides, they had to design isolation rooms in the laboratory to observe volunteers in isolation for a period, to ensure total absence of dengue-exposure of the volunteers prior to experimentation. All this cost a lot of money. This is why very few groups, such as US Army in Manila, could conduct such experiments in the endemic locations. All other groups of investigators chose the second kind of infectious materials: bloodengorged mosquitoes. To prepare them, first they needed to have a colony of mosquitoes. Then, when they found new dengue patients, they visited clinics or houses carrying cages of mosquitoes. If patients consented, they let mosquitoes feed on patients until mosquitoes were fully-engorged. Hopefully, those mosquitoes acquired virus; and the virus would be kept infectious in mosquitoes until human experiments. The major advantage of this approach is that researchers gained mobility. They could carry cages of engorged mosquitoes to dengue-free locations far away and safely conduct human experiments there. Thus, Graham of Beirut took cages to high altitude in the nearby mountain (where mosquitoes were few and dengue was not known to exist) to conduct experiments. Cleland of Australia prepared caged mosquitoes during outbreaks in Queensland, boarded a train and moved south to dengue-free Sydney, where he could safely conduct human experiments. One of the most unusual attempts was done by Snijders, a Dutch physician in Indonesia. He shipped from Sumatra to Amsterdam many cages of not only blood-engorged mosquitoes but normal mosquitoes on board ships sailing to Amsterdam. During the long journey lasting nearly 3 weeks, on-board physicians nourished mosquitoes with cotton swabs soaked in sugar solution. Remarkably, most mosquitoes arrived healthy at the destination, and human experiments were conducted successfully in Amsterdam. [17] Special considerations in human experiment. Now, let me spend a few minutes talking about the essentials of human experiments in early part of the 20th century for both YF and dengue investigations. Here, we find sharp contrasts. During the Havana experiments, after the tragic death of Jesse Lazear, Walter Reed was pressured to draft an Informed Consent form. It is emphasized that this was the first time in the history of experimental medicine anywhere in the world informed consent form was prepared for volunteers. Furthermore, in the YF investigation in Havana, each volunteer was offered a reward of $100; and if a volunteer developed YF as a result, he was offered additional $100 for compensation. In contrast, in Manila, for dengue investigation no consent form was prepared and the reward was far smaller (only 25 local pesos/volunteer). This contrast clearly reflected the prevalent perception of YF as deadly illness versus as non-fatal nuisance for dengue. In terms of the number of volunteers, the cumulative total in dengue investigations by nearly 2 dozen groups in several countries is far greater than the total for YF investigations in Cuba, West Africa, Central America, and South America combined. Still, in early days, recruiting volunteers for dengue experiment was not easy due to strong fear in general public. Sabin ran out of volunteers in Cincinnati and moved his 8 experiment to New Jersey because of more available (and willing) volunteers at the State Penitentiary. Both Ashburn/Craig in Manila and Cleland in Sydney could not complete all planned experiments due to shortage of volunteers despite monetary incentive. Similarly, in Japanese experiments, physicians, nurses, and interns were the volunteers in hospitals; while professors, medical students, friends, and family members were volunteers in medical schools. Thus, when Hotta isolated dengue virus for the first time in history during the WWII, because of acute shortage of laboratory mice necessary for virus passage, his mother volunteered to keep the virus infectious. [18] Early investigators of dengue transmission mechanism. Several investigators deserve mention for their valuable contributions to unravel the mechanism when much was poorly known about vector-borne transmission. Although I emphasize only biological transmission experiments, actually, many investigators at that time conducted experiments for direct transmission. Clearly, their interest reflected similar experiments focusing on fomites during YF investigations earlier in Havana. Some of dengue investigators reported successful intranasal or corneal transmission by physical contact with infectious material and even recorded very brief discharge of infectious agent in urine. Skin scarification was another method utilized to induce dengue infection. The major objective of those direct transmission studies was to determine if they were the principal mechanisms by which dengue was transmitted. A small number of physicians were, however, interested in evaluating direct methods of transmission for non-invasive vaccination. [19] Harris Graham. He was a physician in Beirut. He conducted biological transmission experiment using volunteers and mosquitoes in 1902 in the mountain in Lebanon. Although his experiment is historically important for its first attempt for dengue using mosquitoes, his use of Culex mosquitoes and his conclusion of Plasmodium-like organism found in blood as etiologic agent of dengue were both equivocal. Clearly, he was too much influenced by Ronald Ross’ discovery of malarial parasite (Plasmodium) only a few years earlier. [20] Aristides Agramonte and Juan Guiteras. These scientists of Cuban descent played important roles as members of the Walter Reed Commission. After the YF studies were terminated in Havana, these two scientists shifted their attention to dengue which caused occasional outbreaks there. Apparently, they were influenced by the 1903 report of Graham. They used the wrong mosquitoes, Culex fatigans and obtained puzzling results. Naturally, they had trouble drawing a meaningful conclusion. [21] Thomas L. Bancroft. He was a physician in Queensland, Australia. In 1906, he determined that the true vector of dengue was Ae. aegypti (which was not the name used at that time). Unfortunately, Tom is not known as well as his father. Anybody who took a parasitology course may still remember the well-known filarial worm, Wuchereria bancrofti, which was named after his famous father, Joseph Bancroft. 9 [22] Percy M. Ashburn. He and Craig determined in Manila in 1907 that the agent of dengue was also filterable (=virus). Unfortunately, there were problems in their experiments. Their use of Culex mosquitoes was inappropriate; and the extrinsic incubation period they observed was too short. They also had an additional problem of recruiting volunteers, which made repeat testing impossible. [23] Makoto Koizumi. He was a physician in Taipei, Taiwan. By the time he conducted experiments in 1917, he had read the publication of Tom Bancroft which reported Ae. aegypti as vector of dengue. However, in his environment in northern Taiwan there was no Ae. aegypti. Accordingly, he used several local species of mosquitoes for experiments and proved that Ae. albopictus was a good vector of dengue agent. He also studied the direct transmission, intrinsic incubation period, and minimum dose for infection. [24] Burton Cleland. He was a physician in Sydney, Australia. As I mentioned earlier, around 1916-19, he obtained blood-engorged mosquitoes during repeated dengue outbreaks in Queensland, boarded train carrying mosquito cages, moved south, and conducted human experiments in Sydney. His numerous experiments were described in a 120-page long journal article. He also tried to attenuate dengue agent for vaccine preparation, although he was unsuccessful. [25] Joseph Siler. He was assigned by the US military to the Manila laboratory in 1924. [This photograph was actually taken in France during his previous assignment for typhoid fever.] Basically, he conducted very comprehensive and very sound studies in 1924-25 and repeated nearly everything other groups had conducted earlier. His group’s meticulous journal publication is amazingly more than 480-page long. No such a long manuscript is accepted today in regular journals. [26] James Simmons. He succeeded Siler at the US laboratory in Manila in 1929. During the following 2 years, he conducted more or less the same types of experiments as Siler’s. He confirmed that Ae. albopictus was a good vector of dengue. He was also involved in vaccine development. Like Siler, Simmons’ publication is more than 450-page long. [27] Emilius Paulus Snijders. He was the Dutch physician in Indonesia who I mentioned earlier regarding the story of mosquito cage shipment to Amsterdam. [28] Human experiment in Amsterdam. This is an oil painting commemorating the successful conclusion of the dengue human experiments in Amsterdam. Snijders is shown to the extreme right. Looking at this slide, you may also realize that the value of dengue scientists is better appreciated in some 10 countries, such as the Netherlands, because you rarely find oil painting of dengue scientists hanging in local museums even in dengue-endemic countries. [29] Virus isolation. Virus isolation took place during the World War II on both sides of the military conflict in Asia and the Pacific. On each side, isolation was attempted not only in the battle field but at home. [30] Susumu Hotta. On the Japanese side, when soldiers came down with dengue in large numbers as in the Philippines, New Guinea, Singapore, Malaysia, Indonesia, and Burma, Japanese military physicians tried to isolate virus. In Burma, physicians inoculated blood samples of the sick soldiers with dengue syndrome into chick embryos and shipped the eggs to their laboratories in Japan via military aircraft. At that time, almost nobody knew if dengue agent would grow in chick embryos. However, short time earlier, it was reported by a British physician in India that dengue agent could grow in chick embryos. Japanese military groups claimed that they could isolate more than a dozen of strains of dengue agents; but, retrospectively, it is most likely that they did not isolate the authentic dengue viruses, because dengue viruses do not readily replicate in chick embryos, unless they were first adapted to other more susceptible vertebrate cell cultures. The true dengue virus isolation took place in 1943 in Nagasaki, during a summer outbreak caused by imported cases. There, Susumu Hotta isolated DENV-1 in suckling mice, using the blood sample from a woman patient named Mochizuki. This was the first dengue virus isolated in the world. Other Japanese institutions, mostly medical schools, also claimed to have isolated strains of dengue pathogen in a few cities, including Nagasaki. The total number of so-called “dengue isolates” exceeded more than 30, as far as published records reveal. This is a picture of Hotta. He did not live in Nagasaki when he isolated dengue virus. He traveled 400 miles every summer from Kyoto to spend much of summer in Nagasaki to investigate the exotic disease. [31] Mrs. Mochizuki. This is a photograph of Mrs. Mochizuki from whose blood Hotta isolated the virus for the first time. The virus strain has been known as “Mochizuki strain” of DENV-1. Although medical ethics today prohibits, in the early part of history, using the patient’s name for strain designation was a very common practice in microbiology. [This photograph was published by Hotta with the full consent of the son of late Mrs. Mochizuki] Sometimes, in medical history, medical “first” or “last” has some historic significance. For example, you may remember the face of Mr. Asibi, the source of Asibi strain of YFV, the first isolated yellow fever virus. Or, you may remember the last victim of smallpox at the end of the WHO’s successful eradication campaign. Perhaps, Mrs. Mochizuki’s photograph may have a similar value. 11 [32] Albert B. Sabin. On the side of Allied Forces, the man in charge of virus isolation was Albert Sabin. First, he isolated DENV-1 strain in Hawaii during the 1944 outbreak. He further isolated more strains from the blood samples sent from New Guinea. Because the background story of New Guinea isolates is interesting, let me spend a few minutes to tell you the episode. During the heavy fighting in the jungle of New Guinea, many Allied Forces soldiers came down with dengue. Physicians drew blood samples and put them in an improvised jug stuffed with wet ice and shipped the jug by a military aircraft. The jug was shipped across the Pacific with numerous stops, often changing plane. At each stop, the jug was replenished with fresh wet ice, until the jug was safely in American soil. Thereafter, the specimens were packed with dry ice and shipped to Sabin in Cincinnati. The whole journey took 7.5 days, and virus isolation was attempted more than 40 days later. Fortunately, 4 strains were successfully isolated. Anybody who worked with dengue virus never forgets New Guinea “C” strain, the prototype of DENV-2. This is a picture of Sabin at his youth. During the WWII, Hotta did not know that someone in the US side was competing with him for dengue virus isolation. On the other hand, Sabin did know something about Japanese dengue research, because the US military intelligence units, through interrogation of Japanese POWs, most likely including military physicians, learned about dengue research in Japan and routinely passed the information to Sabin. [33] Hotta-Sabin reunion. So, within 2 months after the end of the WWII, Sabin flew into Japan to gather information, collect blood samples, and arrange shipment of isolated dengue strains to his laboratory. This is not the picture taken in 1945, because no picture of that occasion is available. I substituted instead with one of the pictures taken on his later visits for a reunion with Hotta that took place in 1961. You see that Sabin, center, did age, since he now sports silvery hair. Hotta is shown to the right. [34] Cornelius Becker Philip. The fellow who coordinated this trans-Pacific shipment of blood samples from New Guinea was Cornelius Philip. He happened to be in New Guinea for scrub typhus control for the U.S. military during the WWII. Before his heroic achievement for dengue, he had done another valuable contribution in YF investigation in west Africa. When Rockefeller group isolated Asibi strain for the first time in 1927, Philip was already there as member of the team. Within 2 years, using the Asibi strain, he established firmly that, besides Ae. aegypti, Ae. africanus and Ae. simpsoni were the vectors of YF in Africa. [35] Laboratory-identified dengue serotypes. The serotypes of dengue virus strains identified in this period are shown in this slide. [36] Serologically-identified serotypes. Archival blood specimens were retrospectively tested serologically when neutralization test was developed later. As shown in this slide, DENV-4 was identified earliest. 12 Although DENV-3 was not isolated or serologically identified, there was a strong possibility of the existence of all 4 serotypes in this period. This speculation was based on a small number of carefully-studied reports of individuals who experienced multiple dengue infections. Interestingly, in those cases, the maximum number of multiple infections per person in endemic locations, such as Philippines and Indonesia, was 4. [37] Clinical definition of “dengue.” The early history of dengue is rich in controversies over the clinical definition of “dengue.” Some of the sources of variation of clinical manifestation are shown in the slide. Some physicians strongly speculated that “dengue” was actually a collection of multiple etiologies all sharing the same set of symptoms and signs. While many definitions were based on observations during natural outbreaks, others were the observations reported in human experiments. Because all volunteers in human experiments were adults, the symptoms more prevalent in children could have been missed in those definitions. It should be also stressed that in those human experiments, the performers of the experiments knew nothing about infectious dose used, serotype, immunological status of the volunteers, and others. Naturally, variation in clinical manifestation among experiments could be partly attributed to those unknown factors. Also, it should be noted that as early as in 1928, Blanc, et al. clearly recognized asymptomatic infection in dengue. [38] Atypical symptoms. In old textbooks of medicine, dengue was invariably characterized as non-fatal, febrile illness which was considered a mere nuisance. As a result, when patients died during dengue outbreak, very often, the causes of death were attributed to something other than dengue. After 1950s and even today, it is not uncommon to find a “standard” statement that serious syndromes (dengue hemorrhagic fever [DHF] and dengue shock syndrome [DSS]) began to emerge only after 1950 in southeast Asia. Are they both true? Hemorrhagic manifestations, such as epistaxis, petechiae, and menorrhagia were very common in the early history, but even then they are considered less serious. However, in these patients experiencing extensive hematemesis or other gastrointestinal bleeding (as manifested in extensive melena) sometimes bradycardia developed, leading to a state of “collapse”, “somnolence” or “coma.” These developments ultimately resulted in death. In critically-ill children, seizure often developed. Although the word “shock” was not used in this period, depending on the conditions in terminal phase, such a word as “typhoidlike syndrome” was used, among some physicians. Although it is unclear what that meant, it is possible that it actually meant a condition similar to septic shock in bacterial infection. [39] F.E. Hare. Dr. Hare, then in Queensland, Australia, is credited to be the first physician to document in 1897 many cases of severe dengue syndrome most compatible with DHF, as we know 13 today. In this photograph, he is seated at extreme left in the front row. After his invaluable contributions in Queensland, he could not secure funding for his work and unfortunately had to return to UK, where he operated a sanatorium. [40] Investigation of vascular permeability changes in early days. As hemorrhagic cases increased in frequency, some physicians applied tourniquet test, then known as Rumpell-Leede test. Alternatively, Borbely’s test was performed by applying negative pressure on the skin. Some physicians established a correlation between increase in vascular permeability, thrombocytopenia, and development of hemorrhagic manifestation by monitoring the volunteers inoculated with “dengue agent” (blood of acutely-ill dengue patient). [41] Histologic studies and atomic bomb. When fatal cases occurred, sometimes autopsy was conducted. Abnormalities in cardiovascular system were reported. Also, histologic slides were prepared, as it occurred in Nagasaki, Japan during the WWII. Then, atomic bomb dropped over Nagasaki. Three professors of the School of Medicine of Nagasaki University investigating fatal dengue cases died instantly, and the slides perished. Had the slides survived the blast, they could have provided interesting materials for a comparative study with the samples obtained during DHF outbreaks in the Philippines and Thailand in the 1950s. Hotta was supposed to be in Nagasaki in the summer of 1945. But, because of heavy bombing raids that destroyed railway tracks severely, all train services were suspended indefinitely. So, Hotta reluctantly stayed home. That saved his life. [42] Selected records of fatal cases. This table lists only the selected records of dengue-associated fatality. As you can see, mortalities in Australia were very high between 1895 and 1926. High mortality was also reported in 1931 in Japan and in Taiwan. [43] Geographic mapping of three clusters of dengue outbreak with fatality. Historical study of dengue outbreaks reveals an interesting trend that outbreaks in multiple locations tended to occur clustered in a relatively short period (mostly within 5 year period), disappeared, and re-appeared later in another short period, as shown in this slide. The slide shows that locations where fatal cases occurred were not the same among three cluster periods, suggesting that severe dengue had not become a fixed clinical feature in most urban areas in that period. This is contrasted to post-1950 period, because in the latter period, DHF became a perpetuated clinical feature in many large urban centers in the tropics. [44] Other “unusual symptoms.” Atypical clinical features observed in the early period include CNS syndrome (including stiff neck, encephalitis syndrome, meningitis, epilepsy, facial paralysis, paraparesis, and paraplegia). Pulmonary dysfunctions were invariably reported as “pneumonia-like syndrome”, which was more often observed in eldery patients. 14 [45] Ophthalmologic problems. Vision problems ranged from more frequent conjunctivitis and hemorrhage to more serious retinal hemorrhage, central scotoma, and/or total blindness. One of the studies illustrating such an impaired vision is shown in this slide. [46] Medical care. Salicylates were frequently used. It is noted that even before 1950, some physicians, concerned with increasing number of dengue patients with hemorrhagic manifestations, advised against the use of Aspirin. Antiserums obtained from individuals who recovered from dengue were sometimes used to ameliorate the disease condition, but absolutely no benefit was found in the treatment. Blood transfusion was occasionally attempted by some physicians in desperate attempts to save lives. [47] Pandemic pattern of dengue spread and human movement. It was recognized that ships carrying sick passengers spread dengue over a long distance to other locations free of dengue but infested with dengue vectors. Over years, people noticed that outbreak of dengue coincided with the arrival of passenger ships or naval ships transporting soldiers, after a length of lag period. This should be clearly distinguished from the frequent occurrence of dengue outbreak in a large number of healthy individuals (including soldiers) upon arrival at dengue-endemic locations and subsequent exposure to infective mosquitoes, which suggests dengue endemicity in fixed locations in the tropics rather than dengue spread from one place to the other. Even in the urban centers in temperate climate, arrival of a large number of passengers by ships from the tropics sometimes signaled the beginning of an outbreak, if the port areas were infested with competent dengue vectors. As an example, several port cities of Japan suffered from outbreak every summer during the WWII because of the return of a large number of dengue-infected soldiers and seamen from the war zones in the tropics. In contrast, after the end of the War, this summer outbreak completely ceased to exist, obviously because very few people arrived from the tropics. [48] Unraveling the mechanism of dengue spread by the physicians on board ships. In the covered period, when no jet was used for passenger travel or commerce yet, much of the long-distance travel of people was primarily via ship. Depending on the route and itinerary, it took steamers from several days to as long as a few weeks to reach destination directly without intermediate stops. In many parts of the tropics, many sailing schedules included multiple stopovers before arriving at the final destination. At each stopover for a few days of rest and restocking of supplies, some passengers disembarked because it was their destination, while other passengers disembarked for business, tourism, or personal rest for a day or two but embarked on the same ship again to continue their travel. Also, at each stop, new passengers boarded. 15 Because of long journey, each ship had at least one physician on board to attend the medical needs of the passengers and crew. Records show that dengue outbreaks among passengers erupted occasionally in front of the eyes of on-board physicians. Thus, they had a unique advantage of analyzing the transmission mechanism. Some of those physicians kept a meticulous record of the occurrence of dengue among passengers on board, by paying a special attention to where they boarded, where they disembarked, in which location (port of departure, stopover, or destination) dengue was endemic at the time of travel, when and where new epidemic was reported shortly after the ship’s journey, etc. Each observation recorded only a fragment of information, but when many observations by multiple physicians were retrospectively pieced together later, a more complete picture of the mechanism of dengue spread over long distance by the ship passengers gradually emerged. Today, much of long-distance travel is by much faster jet planes which do not carry onboard physicians. Here, we find an irony when today’s epidemiologists need to study how an exotic disease is imported by passengers of jet planes. Because of the fast travel, practically there is no opportunity to observe the stages in progress before emergence of an outbreak. By the time epidemiologists learn emergence of an outbreak of a new disease brought in by the passengers, often more than several days have passed since their disembarkation at the airports. Locating the passengers for medical interview based on passenger list provided by airline companies is time-consuming and difficult because of mobility of humans and complicated and busy modern life style. These further delay unraveling how an exotic disease is introduced by jet travel. In other words, in the old days, because of much slower travel by ships, physicians on board ships, with keen eyes on the health of passengers, played a role of medical detective or investigative epidemiologist. Today, except for certain types of ships carrying a large number of passengers and crews over a long distance for more than a few days, such as cruise ships, military ships, and some cargo ships, the roles played by the physicians and the strategies used for unraveling the transmission mechanism of emerging, introduced new diseases are somewhat different today. The important roles of the physicians attending passengers and crews in the early history should not be forgotten. One should remember that Patrick Manson could make many valuable contributions to tropical medicine because he was employed at the Seamen’s Hospital in London. There, he had rare opportunities and fortuitous access to a large number of patients presenting a variety of tropical diseases for his studies. In the US, because of the dominant importance of ships in transoceanic travel and commerce and hence of the health care of passengers, crews, and seamen, Marine Hospital Corp [later Marine Hospital Service] was established. This was the forerunner of the present-day U.S. Public Health Service. [49] Dengue pandemic of 1870-73. Occurrence of dengue outbreak in 1870. 16 Now, I would like to show one of the examples of dengue pandemic in Asia and Pacific that occurred between 1870 and 73. This slide shows that in 1870 dengue outbreak recorded only in India. The position of red spot in the center of India is arbitrary, because the exact western port city (or cities) where the outbreak occurred was ambiguous in the old records. [50] Occurrence of dengue outbreak in 1871. This slide shows spread to more locations. [51] Occurrence of dengue outbreak in 1872. This slide shows further spread in southeast Asia and semitropical areas. Actually, in the following year (1873), outbreak was reported even in New South Wales of Australia but disappeared thereafter. [52] Patterns of dengue spread in urban areas. For studying how dengue spread in urban area, locations of the houses of dengue cases were sometimes mapped in chronologic order. This was an early application of the concept of GIS. [53] Examples of the case mapping study. In Australia, it was revealed that dengue spread linearly along houses on street. However, as in other studies, the pattern of spread was more complicated. This slide shows the pattern of spread in the 1931 outbreak in Okinawa where more than 500 died. [54] Recognition of dengue as an urban disease. That dengue was essentially an urban disease was clearly recognized in India. In this map, the solid areas with frequent dengue occurrence correspond very well with urban areas; while the areas with infrequent occurrence correspond with the shaded areas. The huge blank areas without any dengue correspond to rural areas. It was also recognized in such places as Baguio of the Philippines, Lebanon, and La Reunion Island in the Indian Ocean that dengue occurred only in low altitude in the tropics, because the communities located at much higher altitude were basically denguefree even if they were very close to dengue-endemic communities at low altitude. [55] Investigating the mechanism of transmission in living quarter. In many households and a variety of facilities housing a considerable number of humans (such as prisons, police station, military barracks, etc.), dengue spread quickly. Direct transmission was one of the early possibilities speculated. In the following two slides, interesting observations that intrigued the early investigators are shown. [56] Transmission in a military barrack. The slide shows the blueprint of a military garrison where an extensive outbreak of dengue occurred among soldiers. In this diagram, each rectangle represents a barrack for sleeping quarter in which beds are laid out in two or three rows and 10-11 columns of 17 beds per row. Each dot represents the location of bed whose occupant contracted dengue; while the open space represents beds whose occupants were not infected. From this diagram, it is evident that the majority of the soldiers got sick. Because soldiers in contiguous rows or columns of beds were infected, the initial impression signaled a strong possibility of direct transmission. [57] Difference in attack rate between indoor and outdoor sleeping. In a similar study of another military barrack, the difference in attack rate between the soldiers who slept indoor and those who slept outdoor was compared, as shown in this slide. The upper structure is the blueprint of the first floor of the sleeping quarter. The long rectangle laid out horizontally in the middle is the soldiers’ sleeping quarter. This quarter is sandwiched on the north and on the south sides with outdoor veranda which run parallel. In the right part of the blueprint is a perpendicularly laid rectangle, which represents a sleeping quarter for the officers. Like soldiers’ quarter, it is also surrounded with veranda to the east and to the south. Because it was so hot and humid in this part of India that many soldiers opted to sleep outdoor in veranda at night, while others slept indoor. The blueprint below is the bird eye view of the second floor, which is much smaller in the size of floor space. Like in the first floor, some slept outdoor, while others slept indoor. In this diagram, each tiny rectangle vertically drawn represents a bed whose occupant contracted dengue. The blank space represents the beds whose occupants did not get sick. This diagram is very difficult to view for the audience, because it is cluttered with handwritten annotations (name of the soldier occupying the bed and the date of onset of illness) next to the bed on the diagram. So, please focus only on the density of the number of beds (tiny rectangles) indoor and outdoor sleeping areas and ignore all illegible annotations next to them. From this figure, it was interpreted by the investigators that, although soldiers who slept indoor and those who slept outdoor were both exposed to bite of mosquitoes, the frequency of dengue in the soldiers who slept indoor was significantly higher. From these data, a speculation emerged that the vectors of dengue are probably indoor species rather than outdoor species. Why the proportion of the infected soldiers sleeping outdoors was higher in the second floor than in the first floor was not explained, however. [58] Epidemiologic reporting. In the early period, epidemiologic surveillance and reporting systems were not developed in nearly all countries endemic with dengue. Exceptionally, in Western Australia, because of repeated imported outbreaks, dengue was designated a reportable disease in 1912. That 18 marked the first time any government in the world classified dengue as a reportable disease. In the aftermath of the tragic dengue outbreak in Greece in 1928, League of Nations drafted an international sanitary convention that was ratified in 1934. By this convention, participating nations were obligated to report occurrence of dengue and to quarantine at the port of entry all passengers and crew of ships who were suspected to be infected with dengue. However, this treaty was a total failure, because, surprisingly, most of the countries that ratified the convention were European counties where dengue was not endemic, while nearly all currently dengue-endemic countries in the tropics were not invited to ratify. Also, other countries with a strong interest in tropical medicine, such as USA, was not a member of the League. [59] Cyclic pattern of epidemic in dengue-endemic area (or seasonality). Seasonality of dengue outbreak was well recognized in endemic areas. [60] Seasonality of dengue in endemic location. As shown in this figure, cyclical pattern of dengue in endemic location, such as Manila of the Philippines, is very clear. [61] Multiple dengue infection. Many physicians reported patients who suffered from dengue multiple times in life. In some of those reports, each patient was examined by the same physician at every episode of “dengue”; and the physicians had absolutely no doubt about the accuracy of dengue etiology in each episode. Gradually, a small number of physicians conceived a concept of multiple “immunotypes” as causes of dengue. Interestingly, the maximum number of dengue episodes per patient was 4. In a more convincing report made by the US Army laboratory in Manila, it was estimated statistically that a small faction (much less than 1%) of the US soldiers serving in the Philippines would suffer from dengue as many as 4 times during 2-year tour of duty. From these accumulated data, retrospectively, it is reasonable to speculate that all 4 dengue serotypes most likely existed in highly dengue-endemic tropical locations in this early period. It should be noted that this speculation was later confirmed when Wm. Hammon isolated 4 serotypes of dengue virus between late 1950s and early 1960s in southeast Asia. In other locations, however, physicians observed that the residents who suffered dengue once rarely suffered dengue again when epidemic returned later. For them, longevity of immunity against dengue appeared to be very long. This sharp contrast in observations regarding multiple infections was a source of major controversy over the duration of immunity conferred by dengue infection. For those physicians who observed multiple episodes of dengue per person, development of dengue vaccine was an exercise in futility. It should be noted that at that time little was known 19 that dengue agents consisted of 4 serotypes none of which confers life-time crossimmunity among serotypes. [62] Antibody responses to dengue infection. With the advent of neutralization test in vivo using laboratory mice, neutralizing antibody titer could be measured to depict more clearly the dynamic profile of antibody response. [63] Antibody response profiles-primary vs re-infection. Based on NT, Hotta and Kimura was able to differentiate the antibody response to primary from secondary infection, as shown in this slide. [64] Development of serologic tests. In this period, complement fixation test (CF) and neutralization test (NT) were developed and applied for dengue. Historically, CF was developed for YF earlier in 1929. But, its application to dengue was performed only in 1948 by Sabin. Neutralization test was developed for YF in 1929. Saywer and Lloyd applied it in the 1930s for the survey of neutralization antibody to YF in tropical locations in the world. Their result conclusively ruled out the past existence of YF in Asia and the Pacific. After the isolation of dengue virus in the 1940s, specific NT for dengue was developed and became the primary confirmatory serologic technique of dengue outbreak. [65] Animal model. Many animals, including cold-blooded vertebrates, were tested to determine if they could serve as useful animal models. None of them were found suitable. Subhuman primates (Macaca fasciatus and M. philippinensis) were tested. Although virus replicated, the absence of dengue syndrome was a major problem. Fortuitously, a unique breed of Swiss albino mice, “dba” (for “dilute brown non-agouti”) from Bar Harbor Laboratory (in the USA) was discovered by Sabin to be very susceptible to dengue virus for animal experiments. Even with this breed of mice, clinical syndrome of dengue in humans could not be exactly reproduced. [66] Vector identification and biology. Ae. albopictus is often depicted to be an inferior vector compared with Ae. aegypti. That is generally true in much of the tropics. However, one has to be extra-careful elsewhere. During the WWII, every summer, in several port cities in Japan, dengue epidemics originating from a large number of sick soldiers and seamen returning from the battle grounds in the tropics occurred. The total number of cases over 4 summers in several cities was as many as 2 million. The only vector found was Ae. albopictus, and absolutely Ae. aegypti was not involved. Ae. scutellaris was identified as vector in New Guinea during the WWII. 20 Breeding technique for Ae. aegypti was optimized by Siler, et al., in Manila. [67] Geographic distribution of vectors. Entomologic studies were carried out very actively during this period. The compilation of the geographic distribution of YF and dengue vectors in the world by H. Kumm (1931) was a fruit of the arduous field research by many groups. A survey of infestation by Ae. aegypti in southeast Asia was prompted by the potential threat of YF invasion to Asia as a result of the completion of the Panama Canal. Thus, Stanton visited several locations (such as Bangkok, Vietnam, Indonesia) for the entomologic survey. As for the mosquitoes in the Philippines, Clara Ludlow reported in 1902 a new species of mosquito, Ae. scutellaris samarensis. This mosquito discovered by Ludlow was later found to be synonymous with Ae. albopictus. Although she never did an experiment to prove its vector competence for dengue, she had a strong suspicion that it was involved in dengue transmission in the Philippines; and in fact, in her dissertation are found annotations with the word dengue for the collections of this mosquito from the military posts where soldiers became sick of dengue. [68] Clara S. Ludlow. I would like to spend a few minutes to introduce this extraordinary entomologist. She graduated from the prestigious New England Conservatory of Music, majoring in piano. We do not know much records about her professional life. Remember, in the maledominant world of the 19th century, for women to pursue a professional career was very difficult. At least we do know that she taught music at religious organizations such as seminaries. At the age of 45, she suddenly became interested in mosquitoes. Then, she broke the gender barrier and enrolled in male-only Mississippi A & M (now Mississippi State University). After obtaining bachelor degree, she advanced to master’s program. Upon completion of her Master’s degree, she traveled to Manila to visit her brother serving in the military. Over there, somehow she convinced the military brass about the importance of mosquito studies in the context of malaria and dengue. It must be emphasized that when she was there, in 1901-02, it was before Graham conducted the first vector-borne transmission of dengue in Beirut, and still nobody knew if dengue was transmitted by mosquitoes. I surmise that she got the idea after reading the Walter Reed Commission Report of YF submitted to the Congress only a short time earlier. Also, she had a correspondence with William Gorgas. Apparently, she got an appointment in the military during her brief visit to Manila, because when she left the Philippines, she headed directly to Presidio in San Francisco, the military base. From the base, she requested then Surgeon General, George Sternberg, 21 his support for her mosquito study in the Philippines. Sternberg then ordered all US military posts (nearly several hundred) throughout the archipelago of the Philippines to regularly collect mosquitoes and ship them to Clara in San Francisco. She was, thus, very busy shipping mosquito collection kits to the military posts for replenishment. Naturally, in a relatively short time, she amassed a huge collection of mosquitoes of the Philippines, which she used to write her doctoral dissertation. Thus, in her dissertation submitted to George Washington University, Sternberg is listed as her advisor. She was later admitted to be the first female member of the American Society of Tropical Medicine and Hygiene. At the age of 55, she still tried to enroll in medical school. [69] Venereal and vertical transmissions in mosquitoes. The two forms of transmission in mosquitoes were studied earlier for YF, influencing the minds of early dengue researchers. Simmons, et al. (1931) were unsuccessful in proving venereal transmission in mosquitoes. However, they concluded that it was still possible under natural conditions. A strong influence of the YF study in 1901-05 in Brazil by French scientists from the Pasteur Institute, such as Simond and Marchoux, was also felt for dengue researchers, although Bauer, Philip, and others failed to prove for YF in west Africa. The first conclusive proof for YF was reported only in 1997. For dengue, Legendre (1911) speculated the possibility of vertical transmission but did not prove it. Siler, et al. (1925) failed to demonstrate it using Ae. aegypti. Like in YF studies, the conclusive evidence of vertical transmission of dengue virus was obtained more than several decades later. [70] Jean-Paul Simond. This is a picture of Simond. [71] Emile Marchoux. This is a picture of Marchoux. [72] Vector competence. The influence of YF research was also felt strongly in this subject. For YF, Bauer in 1928 demonstrated in West Africa that a few mosquito species other than Ae. aegypti could transmit YF. For dengue, a Dutch group (Snijders, et al.) in Sumatra demonstrated in late 1920s that Ae. albopictus could transmit YF. Koizumi tested in 1917 many species of mosquitoes indigenous to northern Taiwan and concluded that Ae. albopictus was a good vector. Sabin similarly tested several species of mosquitoes in the US but found none of them to be competent. [73] Vector control: biological control. 22 Biological control using predatory mosquitoes, Toxorhynchites spp., was proposed in Australia as early as in 1911. When Stanton was visiting Bangkok for the survey of Ae. aegypti infestation, he observed Toxorhynchites mosquitoes eating the larvae of dengue vector and quickly proposed a biological control strategy utilizing the predatory mosquitoes. Others emphasized the utility of fishes. [74] Toxorhynchites larva. This is a larva of the predatory mosquito. [75] Kill fish (Oryzias latipes). This fish is small, easy to breed, and has been known in Japan by its common name, “medaka.” In the 1940s, a strategy was conceived in Japan to mass breed the fish, transport them via railway and apply for larval control in urban areas. Although a smallscale experiment was encouraging, it was never tested in large scale. Elsewhere, minnows (Gambusia, spp.) were used for mosquito control. [76] Vector control: applications of insecticides including indoor residual spray of DDT. Traditional insecticides for mosquito control were used. The efficacy of DDT for the control of blood-sucking insects was proven when it was tested in 1943 against sandflies in Italy during the WWII. Accordingly, it was quickly applied in 1944 for malaria and dengue control for the protection of Allied soldiers in the Pacific. Among several formulations tested, residual spray was good against dengue. [77] Vector control: source reduction, community participation, public education and organized campaign. Source reduction, community participation, and public education were conducted vigorously in some locations, such as Taiwan and Hawaii. Berraud (1928) also emphasized cleaning up gutters to eliminate Ae. aegypti. In Manila, depressions in urban areas were filled to prevent mosquito breeding. Use of mosquito net was also stressed. A more comprehensive campaign encompassing several methods was adopted in Taiwan in early 1930s. There, the governor proclaimed a dengue control campaign with frequent radio messages. Traditional insecticides were used to control mosquitoes. People were advised to empty regularly water receptacles in and around house. Citizens were mobilized to remove unnecessary water receptacles in residential area. Free copies of brochure with photographs of vectors and common mosquito-breeding water containers as well as instruction for source reduction were distributed to residents. Furthermore, educational slides were shown in movie theaters at intermission. In Queensland, brigades of sanitation inspectors regularly visited houses to check mosquito control practice, provide advice, and to determine change in larval density since last visit for evaluating the efficacy of public educational campaign. [78] Dengue prevention by other means. 23 Preventing or restricting human movement has always been legally difficult or nearly impossible in most countries. Nonetheless, when faced with a threat of invasion of a dangerous disease, people may resort to unusual measures for self-defense. During a major dengue outbreak in Okinawa archipelago of Japan in the 1930s, outbreak first occurred in the largest island of Okinawa. After the news of the outbreak spread to the smaller islands nearby, when ships carrying passengers from that disease-devastated island arrived, residents of those smaller islands blocked disembarkation of the passengers at ports. This is reminiscent of a similar incident that happened in the southern regions of the US when serious YF outbreaks occurred in Louisiana and Mississippi in the 19th century. When trains carrying a large number of citizens of the cities fleeing in panic moved north, suddenly a group of armed men appeared on the railway track, halted trains, and ordered conductors to turn back at gun point. After the devastating outbreak in Greece in 1828, an international sanitary convention was drafted in 1934 by the League of Nations to obligate participating countries to notify (imported) dengue cases and to quarantine all passengers and ship crew suspected of being infected at the ports of entry. However, the convention was a total failure, as explained earlier. Legislation to make elimination of mosquito breeding in domestic environment obligatory was considered in a few countries. But, implementation of such laws was difficult to say the least, and proposals for legislation most often died during debate among politicians. [79] Vaccine development- attenuation or inactivation methods. Attempts to develop vaccine started very early in the history of dengue research. As mentioned earlier, the controversy over the duration of immunity against dengue discouraged some physicians from engaging in vaccine development. This slide shows that both inactivation and attenuation were applied to prepare candidates. Human clinical trial with formalin-inactivated mouse-adapted DENV-1 vaccine candidate was conducted by Hotta and Kimura in 1944. Sabin and Schlesinger prepared a huge amount of attenuated vaccine candidate to protect more than 50,000 Allied soldiers in the Pacific, but the plan for vaccination was cancelled because the War ended much earlier than they expected. During the vaccine development for an attenuated vaccine, Sabin conceived an idea of simultaneous vaccination with a mixed vaccine by incorporating YF (17D). Based on his evaluation of the efficacy, he concluded that he could not recommend such a mixed (multivalent) vaccine because of interference. It is of interest to recall what happened to the international effort to develop a tetravalent attenuated dengue vaccine which was initiated in early 1980s by the World Health Organization. Interference was one of the major causes of failure; and after nearly 30 years since then, still no vaccine is available today, although applications of modern technologies are expected to overcome this problem. 24 [80] Economic cost. Many economic impact studies on dengue have been published lately. However, unknown to many authors of those recent publications, economic impact was indeed studied in the early period, because economic loss by the devastating dengue outbreak was a major concern even at that time. [81] Economic impact study in Queensland, Australia. The slide shows one of such studies conducted in Queensland, Australia. In this study, the author classified occupations into 9 categories and determined the proportion of people in each category in the affected city. Then, based on the average wage and the percentage of work force sick of dengue in each category, he could calculate the economic impact for the affected community. [82] Completing the full circle of the interaction between YF and dengue research histories. I started this presentation with the interesting influence and crossing of the early histories of research between the two important vector-borne viral diseases. In closing this presentation, once again I touch on the relationship. Albert Sabin was close to Max Theiler, the man of yellow fever vaccine fame. In fact, they spent life together briefly at the Rockefeller Institute of Medical Research in New Jersey between 1935 and 39. Thus, it is not surprising that Sabin made the second of three nominations of Max Theiler for Nobel Prize. Although Sabin’s failed, the third nomination by a little-known Spanish woman, Antonia Navarro, succeeded in 1951. So, Sabin’s role in dengue research history was to bridge between YF and dengue research. Very fittingly, Sabin is buried very close to the gravesite of Walter Reed at the Arlington National Cemetery in Virginia. [83] Acknowledgments. The following individuals in the slide provided a variety of valuable assistances during the preparation of the slides and are deeply appreciated.