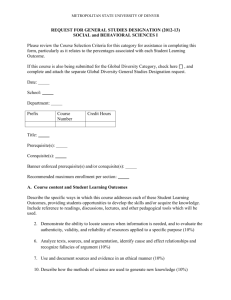
Metropolitan Health Service Annual Report 2010*11
advertisement

Significant Issues Significant Issues impacting the agency Delivering a Healthy WA 1 Metropolitan Health Service Annual Report 2010-11 2010 - 11 Highlights and Significant Issues Four Hour Rule Significant Issues Child and Adolescent Health Service April 2011 marked the second year of the Four Hour Rule Program (FHR) for Princess Margaret Hospital (PMH). Over the past two years PMH staff have made significant changes to the management of unplanned patients by focusing on a whole of hospital approach, from triage to discharge. On 30 April, the hospital celebrated reaching and sustaining the 98% target of admitting, discharging or transferring emergency patients within a four hour time period from the patient presenting at triage. Figures show the number of Emergency Department (ED) attendances admitted, discharged or transferred within four hours increased from 89.9% to 95.7% over March 2010 to March 2011. Timely patient discharge remained a focus of the program and this was reflected in an increase of 11% in the number of patients discharged before 10.00am. During 2010-11, safety and quality measures were the key indicators of the program that were closely monitored. PMH reported no increase in representation rates of discharged patients relating to the FHR. The hospital continues to actively monitor all safety and quality measures via a fortnightly PMH specific dashboard to ensure all arising issues are promptly addressed. Feedback collected from parents indicated increased visitor awareness about discharge times and processes. Parents expressed feeling more in control of their hospital journey and were satisfied with the way reasons for ED waiting times were communicated. South Metropolitan Area Health Service Royal Peth Hospital (RPH) has led the way for tertiary hospitals in WA and Australia by exceeding the FHR program target well ahead of the April 30 deadline. With a 90% average throughout April, RPH exceeded the target of admitting, discharging or transferring 85% of patients presenting to the ED within four hours. In addition, access block had dropped from 50% in mid 2008 to less than 10 per cent in 2011. RPH has implemented changes and programs across the hospital to help achieve the four hour rule target and to ensure safe quality patient care, including utilisation of “Lean Thinking” principles and tools, enhancement of ward leadership, introduction of an Acute Admitting Unit, Patient Journey Boards visible to the whole team and the optimal use of Hospital in the Home and Rehabilitation in the Home. In October 2010, the Armadale Kelmscott Memorial Hospital (AKMH) commenced implementation of the FHR program and implemented the control phase, allowing for solutions to be applied. The introduction of a second triage nurse in the ED facilitates the flow of patients through the ED and allows for faster admittance to the ED after a patient presents to triage. 46 Delivering a Healthy WA Rockingham General Hospital (RGH) is on track to meet the October 2011, 85% FHR program target. During the April – June 2011 quarter RGH ED treated 11,455 patients with 83.3% being treated in four hours. Solutions across the hospital have been introduced to fast track patients who are ambulant to self present to medical imaging, implement reductions for a patient’s emergency length of stay by 20 minutes, and implement daily bed management meetings and the introduction of a new LEAN ‘booking a bed’ process, with results so far showing a 63% improvement. Fremantle Hospital and Health Service (FHHS) has had significant success with initiatives to support the FHR program, reducing access block by 15 per cent and decreasing ambulance ramping. Extended staffing and operation hours in the Gage Roads Transit Lounge assisted with early discharges and resulted in a 51.4% increase in throughput in 2010 (compared to 2009) and saw a 20.6% increase in throughput from January – May 2011 (compared to the same time last year). A FHHS home ward model was introduced to enhance multidisciplinary care and discharge planning processes for medical patients. An inter-hospital transfer discharge coordinator has been introduced to coordinate all inter-hospital transfers to increase bed availability and assist with patient flow. 24/7 ED Navigators managing the patient journey from ED admission to the ward have streamlined ED admission processes. Improvements to accelerate pathology and pharmacy requests have also contributed to improvements. During 2010-11 FHHS saw an 11 per cent increase in ED presentations with a noticeable winter flu season spike. North Metropolitan Area Health Service During 2010-11 Swan District Hospital (SDH) made good progress in implementing the FHR falling just 3% short of the planned activity target, which will be achieved prior to October 2011. SDH emergency department has been reconfigured to increase capacity. King Edward Memorial Hospital (KEMH), a Stage 3 FHR site, is progressing improvements for the patient experience and enhanced staff satisfaction for both admission and discharge pathways, and is improving efficiency and productivity with coordinated bed management to reduce poor patient experiences whilst awaiting clinical care. The program addresses unplanned presentations to the Emergency Centre (EC) and the Maternal Fetal Assessment Unit (MFAU). KEMH has appointed facility and clinical leads to support the FHR, and the ‘define’ and ‘measure’ phases are completed. Preliminary results show that Women’s and Newborns Health Service is performing well against the FHR targets. Delivering a Healthy WA 47 Significant Issues Metropolitan Health Service Annual Report 2010-11 Metropolitan Health Service Annual Report 2010-11 Elective Surgery Child and Adolescent Health Service PMH completed another very busy year for elective surgery with around 11,000 cases completed. Over boundary reportable cases were reduced from 100 to 12 cases in the last financial year, with ear nose and throat (ENT) eliminating all 70 reportable over boundary cases. Significant Issues A gastroenterology blitz list for Saturday mornings was introduced towards the end of financial year and the initiative will continue on weekends over the next year to assist with the high demand for gastroenterology services. South Metropolitan Area Health Service SMAHS performs well in developing and providing quality elective surgery services and exceeding many elective surgery targets. AKMH, Bentley Hospital (BH) and FHHS exceeded the elective surgery targets set for 2010-11. The RGH elective cases increased by 38% compared to 2009-10. FH completed an additional 800 elective surgery cases above the target. The hospital’s clinic and waitlist times were some of the shortest in the State. In addition, urology services were improved with the appointment of a urology nurse practitioner, a new Nurse Practitioner Wound Management Service commenced delivering evidence-based wound care to patients resulting in improved chronic and vascular wound care. A new rostering arrangement for surgical consultants, and the designation of a specific Acute Surgical Unit (ASU) improved access to senior surgical expertise and streamlined the surgical admission process. North Metropolitan Area Health Service Additional capacity will be provided by two new operating theatres funded by the Commonwealth at the Osborne Park Hospital (OPH) Surgicentre, scheduled for completion in 2014, and the hospital has commenced an outpatient clinic service for general surgery to ensure the correct hospital referral at the first point of contact. Sir Charles Gairdner Hospital (SCGH) has implemented strategies to ensure bariatric patients receive dietetic education in a timely manner, facilitating minimal disruption to the elective surgery waitlist. During 2010-11 endocrine surgical services commenced at SDH for non-tertiary cases. The NMAHS commenced a trial for a Clinical Nurse Plastics Co- Coordinator role to provide one point of contact, and promote a reduction in long wait over-boundary cases and improved theatre utilisation at both OPH and SCGH. The Area Health Service has also implemented process reviews for plastic surgery services (patient journey mapping with key stakeholders), and for in-patient booking services using ‘Lean’ methodology leading to improvements in departmental practises, and generally achieved a decrease in over boundary cases through active audit, outpatient clinic review and consultation with medical staff. 48 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 Service development The OPH Stroke Services Program commenced in October 2010, supported by COAG funding. Inpatient stroke beds increased to 10 and an Early Supported Discharge (ESD) program for stroke patients over 65 years of age commenced. This is first ESD Program for stroke in WA. During 2010-11 a trial of a Clinical Nurse Specialist (CNS) commenced in the Women’s and Newborn Health Service (WNHS). The KEMH staff development educator has implemented a time saving ‘bed to bed’ clinical handover process, for which she won the Extreme Lean Award as part of the Emerging Leaders Program. SKHS has increased in-patient and outpatient activity in all disciplines, including general and sub-speciality medicine, paediatrics, antenatal, obstetric and neonatal care, and introduced additional gynaecology, geriatric, aged care and rehabilitation and stroke services. SKHS has also increased capacity in training infrastructure, progressed the development of telehealth, and, in May, re-opened the endoscopy theatre at Kalamunda Hospital. During 2010-11 the SCGH progressed a number of initiatives for rehabilitation services including appointing a rehabilitation physician, seeking Australian Rehabilitation Outcome Centre accreditation for the Gairdner Rehabilitation Unit (GRU), introducing Rehabilitation In The Home (RITH) for the Joonadalup Health Campus catchment area and developed a Throbolectomy service in stroke care. SCGH has commenced: An integrated mitral valve disease service. Increased speech pathology and diet therapy support for patients with swallowing and communications problems secondary to head and neck cancer. Allocated additional resources to cancer and palliative care occupational therapy. Provided a centralised NMAHS service resulting in a reduction in length of stay (LOS) for patients awaiting permanent care options. Commenced cystic fibrosis, respiratory and vascular outpatient clinics. Introduced hospital total parenteral nutrition inpatient and outpatient services. Introduced ’Assistant in Nursing’ (AIN) students. With COAG funding, a Parkinsons Clinical Nurse Specialist has been appointed for the NMAHS. The WNHS Mother and Baby Unit (MBU) reviewed the follow up care arrangements for discharged patients, seeking opportunities for improvement. The review has resulted in an increase in community visits and the introduction of joint visits with Community Child Delivering a Healthy WA 49 Significant Issues North Metropolitan Area Health Service KEMH has maintained clinical services during significant infrastructure projects such as the Maternal Fetal Assessment Unit and the new Neonatal Critical Care Unit. The hospital has recruited a Nurse Practitioner in Urology to support the increasing demand in this area. Metropolitan Health Service Annual Report 2010-11 Health Nurses with regular meetings with nursing staff to review current practice and share information across the metropolitan area. Significant Issues South Metropolitan Area Health Service RGH continues to transition to full general hospital status, providing for most of the health needs of our population and providing care closer to home. Inpatient specialties include expanded surgical services, chemotherapy, intensive care, neonatal, major orthopaedic, maxillary facial, neurology and urology. The hospital currently has 155 general hospital and 20 mental health beds. New clinics or services commenced in 2010-11 include lactation consultation, speech pathology and newborn hearing screening. In addition, the hospital now has 24/7 Medical Registrars. The hospital hosted an Open Day, forging closer local community links. Members of the public were able to met with staff, joined tours to see how the hospital operates, learnt about new facilities/services and career opportunities, as well as enjoying ‘health and wellbeing’ entertainment. During 2010-11 a 10 bed Intensive Care Unit (ICU) at the AKMH, the first non-tertiary ICU in SMAHS commenced. The new unit is staffed by specialised medical and nursing personnel, and increases the hospital’s capability to treat patients with potentially lifethreatening conditions relieving pressure on tertiary hospitals. A level 2A neonatal nursery has been established, the upgraded nursery allowing staff to provide high dependency neonatal care to newborns, with fewer babies requiring transfer to the state’s tertiary newborn facility. A new peripherally inserted central catheter (PICC) line service commenced in the latter half of 2010. Patients can now have PICC lines inserted at AKMH, and are no longer required to travel to other hospitals. PICC lines are inserted as alternatives to cannulae for patients requiring long term treatment, resulting in less stress and discomfort for patients, and a reduced chance of infection. During 2010-11 the BHS relocated and expanded its antenatal service, offering easier access and on-site antenatal medical support and offering an Antenatal Doctor Clinic. Catheter-based renal denervation is now offered at the RPH Cardiology Department. This is a new non-invasive treatment option for patients with blood pressure in excess of 160 who cannot reach target blood pressure levels even with the use of three or more medications. The procedure works by disabling the nerves leading in and out of the kidney using radio frequency energy. FHHS became the first public hospital in Western Australia to implant a Magnetic Resonance Imaging compatible pacemaker into a public patient. The Patient Blood Management (PBM) program was officially launched in April 2011. It helps reduce the need for blood transfusions, improves results for patients, and reduces the pressure on blood supply capacity. Following the success of the pilot program at FHHS, the PBM is currently being rolled out to other major hospitals across WA. An Australian-first stent graft procedure to remove an 11cm aneurysm from the aortic arch was successfully completed at Fremantle Hospital in February 2011. During 2010 50 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 Activities to enhance FHHS emergency services to the community included more than 500 referrals to the GP Consultation Liaison Clinic in 2010, and new CoNeCT service which coordinates care for ED patients with complex problems. The FHHS Ladies’ Auxiliary continues to raise funds for the hospital and in 2010-11 donated $186,000 to purchase patient care equipment and amenities. The extended Moss Street Parkinson’s Disease Service began accepting patients in January 2011. Four regional sites have been set-up to care for patients nearer to their homes. The number of patients using the service is now more than 500 and growing steadily. In February 2010, a nearby fire in Roleystone resulted in an increased number of ED patients presenting to the AKMH for fire-related injuries. The hospital activated their emergency response unit, and a temporary second emergency department was set up to help manage the increase in service demand. Child and Adolescent Health Service During 2010-11, the Child and Adolescent Community Health Service (CACH) continued to deliver a range of services in partnership with key stakeholders including the Department of Education (DE), the Department for Communities (DC) and nongovernment organisations. CAHS community and child health nurses and allied health professionals were: Located at the Challis Early Childhood Education Centre. Co-located with Department of Child Protection (DCP) staff at Brookman House. Located to the Parents Place in Mandurah encompassing services delivered by CACH, DC, the City of Mandurah, and non-government organisations such as Child Australia. Located at school sites including Roseworth and Hudson Park primary schools. A number of services were expanded during 2010-11 including lactation consultants and the Best Beginnings Program, which is an evidence-based intensive two year home visiting program for identified ‘at risk’ families. Community health nurses responded to the adult pertussis campaign through provision of immunisation clinics in community sites across the metropolitan area. Health assessments for children in the care of the Chief Executive Officer DCP were provided and will be conducted annually for all new and existing children in care. Community health nursing was recognised through one of its staff members - Jackie Roberts who was awarded ‘Community Nurse of the Year’ (Consumer Award) at the 2010 Western Australian Nursing and Midwifery Excellence Awards. The separate Child and Adolescent Mental Health Service (CAMHS) managed by NMAHS and SMAHS, transitioned to CAHS in February 2011. This transfer involved approximately 335 FTE. All CAMHS staff were engaged in consolidating services and Delivering a Healthy WA 51 Significant Issues the Kaleeya Hospital Maternity Unit achieved their highest number of births with 1,249 deliveries. Metropolitan Health Service Annual Report 2010-11 developing an organisational structure which has resulted in CAMHS now being a dedicated stream under CAHS, similar to Child and Community Health (CACH). The transition of CAMHS progressed smoothly with the team focusing on governance, financial and resource management, workforce and service development priorities. The engagement with and feedback from CAMHS staff regarding the transition was very positive. Significant Issues The main priorities for consolidating CAMHS were to: Create a child-focused, rather than disease-focused culture, by embedding child mental health services in general health services for children. Ensure equitable access to services. Develop consistent and clear clinical models and pathways of care. Integrate governance and reduce duplication. Maximise funding and resources for CAMHS. Improve inter-sectoral relationships with other child and family related services (e.g. NGOs, Departments of Education, Disability Services, Child Protection, Community, and Justice). Increase research, teaching and training. Services consolidated include: CAHS Psychological Medicine Unit (PMH Ward 4H, Paediatric Consultation Liaison, Psychiatric Liaison, Assertive Outreach Team, Eating Disorders and Family Pathways). SMAHS CAMHS (Bentley Adolescent Unit, Transition Unit, Families at Work, community clinics in Armadale, Bentley, Fremantle, Peel and Rockingham, YouthReach South, Multi-systemic Therapy, Complex Attention Hyperactivity Disorder Service Murdoch). NMAHS CAMHS (community clinics in Clarkson, Hillarys, Warwick, Swan and Shenton, YouthLink, Complex Attention Hyperactivity Disorder Service Joondalup). CAHS (manages) statewide operational policy development and negotiations with the Mental Health Commission regarding metropolitan and regional CAMHS. During 2010-11 CAMHS was also successful in the development of business cases to upgrade the Bentley Adolescent Unit, where significant issues in its therapeutic milieu and general environment have been identified. A $4.5 million investment from the Commonwealth will see significant improvements over the next 18 months and Mental Health Commission and Commonwealth funding support will enhance emergency and assertive community services for children and adolescents. Metropolitan Child Development Service In 2010-11, the State Government committed $49.7 million state-wide over four years to improve access to child development services across WA. During the year, the Metropolitan Child Development Service (CDS) created an additional 45 positions including speech pathologists, occupational therapists, physiotherapists, clinical psychologists and social workers. As at May 2011, 44.5 new positions had been filled. A key objective of the budget increase was to reduce waiting times by 50% for the key disciplines of speech pathology, physiotherapy and occupational therapy. As at May 2011, physiotherapy and occupational therapy had achieved the target and speech 52 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 pathology had achieved a 48% reduction. It is anticipated that speech pathology will achieve the 50% target by the end of the financial year. The CDS introduced a range of innovative models including the expansion of community nurse led clinical intake and triage teams as well as the therapy assistant model. During 2010-11, the CDS partnered with five non-government organisations to deliver speech pathology services in the south metropolitan area. Also during the year, Infant Child Adolescent and Youth Mental Health Service (ICAYMHS) transitioned to CAHS, appointed a second con-joint paediatric neurosurgeon at SCGH for the isolated service and the SKHS implemented a back referral process for paediatric services ex PMH, developed linkages with community paediatric services in Lockridge and commenced a registrar rotation with the rural paediatric service in Merredin. Cancer services South Metropolitan Area Health Service Cancer patients in Esperance now benefit from a fortnightly visiting RPH oncologist, removing the need for patients to travel to Kalgoorlie or Perth to see an oncologist. This also enhances the chemotherapy service, available in Esperance, since March 2008 provided by nurses supervised by GPs with phone advice provided by the RPH oncologist. Cancer Clinic Services, the collaboration between RPH, WA Cancer and Palliative Care Network and WACHS are held in Albany (monthly), Geraldton (every three weeks), Kalgoorlie (fortnightly) and Northam (monthly). Accreditation South Metropolitan Area Health Service In 2010-11 AKHS, FHHS and RPH received accreditation. The Australian Council on Health Care Standards (ACHS) indicated RPH is leading the way in providing quality patient care, awarding three Outstanding Achievements in the areas of Research, Learning and Development, and Policies. In addition, RPH also received 13 Extensive Achievement (EA) ratings. Only five recommendations for mandatory change prior to the next accreditation period were received. The FHHS was awarded Outstanding Achievement in Medication Management. RGH is one of two WA hospitals participating in the World Health Organisation (WHO) High 5s Assuring Medication Accuracy at Transitions in Care quality improvement project. The program commenced in 2010. North Metropolitan Area Health Service Successful ACHS accreditation assessment for OPH in October 2010 increased the current ratings in several areas with five EA ratings in credentialing, infection control, evaluation of care, policy and OSH. The WNHS completed a highly successful Organisation Wide Survey for accreditation resulting in 11 identified areas of excellence and ongoing accreditation until March 2015. Delivering a Healthy WA 53 Significant Issues The number of children waiting for services between May 2010 and May 2011 was reduced by 30% from 6,284 to 4,331. This was achieved in an environment where demand for services continues to grow. Metropolitan Health Service Annual Report 2010-11 WoundsWest WoundsWest, Silver Chain and Curtin University were recipients of a federal innovative Clinical Teaching and Training Grant to develop a virtual Wound Clinical Education Centre at Curtin University to enhance education and competency development in wound management for all health professionals. Significant Issues WoundsWest, in partnership with Curtin University, DoHA, OATSIH and remote WA and NT Health Services is also undertaking in a 12 month research project to develop sustainable practices in wound management knowledge and competency amongst Aboriginal Health Workers and health professionals in remote Indigenous communities in the Pilbara region of Western Australia. A further three online wound education modules have been published: the Aboriginal Health Worker, Leg Ulcer and RACGP modules. WoundsWest was nominated for the 2011 Excellence in Teaching Awards, University of Western Australia (UWA) Faculty of Medicine and Dentistry and Health Sciences. North Metropolitan Area Health Service The OPH participated in the WoundsWest Wound Prevalence Survey in May 2011. Occupational therapy staff at OPH and SCGH, are working collaboratively with nursing staff on pressure ulcer reduction strategies including hospital-wide audits. Podiatry staff at SCGH are involved in development and ongoing review/update of a Foot Ulcer Module for WoundsWest. Sub-acute and rehabilitation North Metropolitan Area Health Service During 2010-11 the SKHS undertook a reorganisation of its sub-acute care and rehabilitation services to align with the area-wide framework, and improved service liaison with local Kalamunda GP’s regarding rehabilitation and palliative care services. SCGH progressed the appointment of a rehabilitation consultant and the credentialing of the Rehabilitation Unit expanded Rehabilitation in the Home (RITH) to the Joondalup area and introduced Functional Independence Measure (FIM) training by a master trainer (Occupational Therapy) to SCGH rehabilitation staff. South Metropolitan Area Health Service The RGH received Commonwealth funding for 24 sub-acute beds (14 Aged Care Rehabilitation Unit, 10 Mental Health Inpatient Unit). The South Metropolitan Area Palliative Consultancy is now operational providing specialist palliative care support to general hospitals and residential aged care facilities. The Sub-Acute Spinal Injuries Program (SASIP) is a partnership between Royal Perth Hospital Spinal Unit and the Quadriplegic Centre for the inpatient management of subacute and non-acute spinal cord injured patients. The aim of the SASIP is to reduce length of stay at the Spinal Unit by utilising the services of the Quadriplegic Centre. This enables greater access by reducing delay to the services provided by the Spinal Unit. 54 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 This has become necessary as advances in medicine and surgery means that more people are surviving spinal cord injuries. During 2010-11, the Aboriginal Health Team (AHT) was successful in securing additional funding through COAG Element 3 Indigenous Early Childhood Development, to increase access to parent/child health services. The funding enabled the AHT to increase human resources to deliver services in the Armadale/Gosnells and Wanneroo/Joondalup local government areas. The AHT was also successful in receiving funding to develop culturally appropriate resources to promote ear health in the 0-4 year old age group for Aboriginal children in the metropolitan region. The ear health resource kit will be available for staff in July-August 2011. In April 2011, the AHT manager position was established as a Section 50D position, to provide leadership and strategic direction to the team and to ensure cultural security be maintained in the development and delivery of services. The Aboriginal Health Worker Wound Education Program (AHW WEP) was awarded the MIMS Best Presentation Award for the best overall presentation for this program at the Primary Health Care Research Evaluation and Development Annual Research Conference in Perth on 12th November 2010. In order to ensure services are appropriate and accessible, alternative service models have been implemented including speech and language playgroups to support the children with speech and language concerns (Moorditj Yarning Kulungas). The playgroups are led by Aboriginal health workers, with support from CDS staff who have been re-allocated to AHT. North Metropolitan Area Health Service During 2010-11 the NMAHS Reconciliation Action Plan (RAP) was developed, to be finalised in August 2011. The Area Health Service undertook project planning; development, establishment and implementation to address the COAG initiatives under the National Partnership Agreement (NPA) and Closing the Gap (CTG). Priority areas are tackling smoking; healthy transition to adulthood; making Indigenous health everyone’s business; primary health care services that can deliver; fixing the gaps and improving the patient journey as well as Elements two and three of the Indigenous Early Childhood Development (IECD) NPA, increasing access to antenatal care, prepregnancy and teenage sexual and reproductive health and increased access to, and use of, maternal and child health services by Indigenous families. The newly established Aboriginal Maternity Services Support Unit (AMSSU) at the WNHS is a COAG funded initiative. The AMSSU has supported Area Health Services during the planning and early implementation phase of Aboriginal Maternity Group Practice services across their regions. This has involved consultation with the Regional Planning Forums that determined the successful programs. The Unit will recruit and form a community reference group as one of its first priorities and will also be working with the Aboriginal Health Council of WA and Health Consumers’ Council. Delivering a Healthy WA 55 Significant Issues Aboriginal health Metropolitan Health Service Annual Report 2010-11 This Unit has coordinated specific NMAHS proposals, including a chronic disease self management (LIFE) proposal, support for Aboriginal liaison strategies, introducing a tailored smoking cessation and a street doctor, and for a number of metropolitan-wide projects including a podiatry and nutrition outreach program, an Aboriginal men’s health program, and a ‘Strong Spirits Strong Mind’ Program. Significant Issues Challenger TAFE and Rockingham students were engaged in the design, completion and erection of an Aboriginal mural placed in the foyer of KEMH to acknowledge and welcome indigenous people to the health service. SCGH podiatry staff were involved in the development of Moorditj Djena program to provide services for Aboriginal patients as part of the ‘Close the Gap’ initiative South Metropolitan Area Health Service More than $25 million of COAG and WA Health funding has been proposed for SMAHS Aboriginal health projects. All projects commenced in 2010-11 and will be developed and evaluated over the next three to four years. Projects include: The Aboriginal Health Liaison Officer project - the appointment of eight Aboriginal Health Liaison Officers in SMAHS hospitals. These officers provide Aboriginal patients with culturally secure liaison services and provide cultural advice to health care teams. An Aboriginal men’s health project officer has been appointed and is working with men’s health providers and the community to improve access to health services for Aboriginal men. A mobile podiatry service has been established and is servicing Aboriginal people with, or at risk of, diabetes and foot problems in their local community; and Aboriginal community forums and local District Aboriginal Health Action Groups have been held on a regular basis across the SMAHS. These groups are providing Aboriginal cultural and community advice on all projects. Workforce achievements and initiatives North Metropolitan Area Health Service The NMAHS mental health team implemented training and operational planning workshops to support positive work environments, promoting staff retention and supporting leadership development training and positive attitudes to workplace training utilising the ‘FISH!’ philosophy. During 2010-11 NMAHS staff were recognised for a number of achievements: A WA Nurse Excellence Award for Ailish Owens at OPH (‘Graduate of the Year). OPH allied health staff members Deanne Jones and Cathy Viandante - the Stroke Society of Australasia Service Awards. OPH’s Alex Zivanovic awarded the Karrinyup Rotary Nurse of the Year. Shane Douglas (OPH Patient Services Officer) won the ‘Pride in Workmanship City of Stirling award. OPH Clinical Nurse Manager in Rehabilitation and Aged Care presented at the ‘Innovations In Nursing’ Conference Perth May 2011. 56 Delivering a Healthy WA OPH medical resident Dr Emma Allanson awarded the WA Confederation of Postgraduate Medical Education Council’s Doctor of the Year 2010. Dr Paul Mc Gurgan, Clinical Head of Service Women’s and Newborn Health Service, was made a fellow of the Australian Association for Quality in Health Care due to innovations and improvements in OPH relating to the introduction of Universal cord PH in 2010. Dr Mc Gurgan also was nominated by UWA for a national tertiary education Early Career award. (The Australian Learning and Teaching Council Awards 2011). Midwife Cassandra Simcock and Dr Mike Allen awarded the OPH Medical Student Outstanding Teacher Awards; and. Kaye Browne Occupational Therapist received funding from Curtin University and DoHA to complete a guide on: ‘Dementia: OPH Guide for OTs in Clinical Practice.’ WA Nurse Midwife of the year was awarded to KEMH’s midwife Sadie Geraghty. Two Churchill Scholarships were awarded to SCGH allied health staff, Claire Langdon for the use of speech pathology stimulation devices to improve function in people with eating and drinking impairments, and Jamie Wood for physiotherapy techniques for people with cystic fibrosis and bronchiectasis. Another Churchill Scholarship was awarded to State Head Injury Unit’s Louisa Cato for community support for those living with communication impairments following acquired brain injury. SCGH has also introduced inaugural Allied Health Week Awards and Celebrations with awards for Rookie of the Year, Clinical Excellence and for Outstanding Contribution. The SCGH Pharmacist awarded the Eric Kirk Memorial Award to Michael Cain for contributions to oncology services. HITH nurse, Lesley Homer presented a paper describing how sleep studies are now provided in the child’s own home at the 3rd Annual HITH National Conference in Melbourne (2010). South Metropolitan Area Health Service SMAHS is continuing to provide an increased number of initiatives to retain staff, and maintain a happy and healthy workforce. During 2010-11 SMAHS staff were recognised for a number of achievements: The Nursing and Midwifery Executive Council hosted the first FHHS Nursing and Midwifery Excellence Awards recognising the skills and attributes of our many nurses and midwives. The awards were held on International Nurses Day -12th May and were supported by the WA Hospital Nurses and Midwives Support Fund. This year’s winners were: Joanne Hardy- Research and Evaluation, Sherrill McMahon- Training and Development, Judy Dowling- Clinical Leadership and Jennie Opie- Core Practice. Drs Wendy Davis and Anita Chew received a New Independent Researcher Infrastructure Support Award in August to carry on their important medical and health research work in WA. FHHS’ Dr James Anderson was awarded the inaugural AMA WA Young Doctor of the Year Award. FHHS Pain Medicine Unit received a 2010 WA Health Award – Hospitals Award in recognition of its innovative Self-training Educative Pain Sessions (STEPS) program. Delivering a Healthy WA 57 Significant Issues Metropolitan Health Service Annual Report 2010-11 Metropolitan Health Service Annual Report 2010-11 Charlotte Collins, A/Clinical Nurse Manager Mental Health was named 2010 Nurse of the Year. Significant Issues Endoscopy Nurse at Kaleeya Hospital, Ms Jo Robinson headed her class in a Gastroenterology Nurses exam in Brisbane and holds the title of 2010 Credentialed Nurse of the Year in Gastroenterology. Ms Sue Thurston, Clinical Nurse Manager of the FHHS Hyperbaric Unit, received the Hyperbaric Technicians and Nurses Association (HTNA) Annual Award for Excellence in Hyperbaric Oxygen Treatment (HBOT). The award recognises innovation or exceptional efforts to advance clinical, technical or safe practice in HBOT by an HTNA member. Acting Clinical Nurse Manager ICU Claudia Howe was awarded the Critical Care Nursing Excellence Award 2011 by the Australian College of Critical Care Nurses at the 12th Annual Institute of Continuing Education meeting held in Perth in May. FH Clinical Director of Critical Care and Emergency Department Physician Dr Tom Hitchcock was appointed to the role of Emeritus Consultant for Patient Safety for the WA Department of Health. Debbie Nelson – Mental Health Nurse of the Year (Australian College Mental Health Nursing). Kathy Bruton – Primary Health Care Nurse of the Year (Office of the Chief Nurse, WA). Ambulatory Care Service Clinical Nurse Manager Julie Vine’s leadership was recognised with a nomination in the ‘Emerging Leader’ category in the 2011 Western Australian Nursing and Midwifery Excellence Awards. Clinical Nurse Consultants, Toni Ilich and Lara Jackson co-authored an article published in the Journal of Voice March 2011 – ‘Drilling Speaking Valves to Promote Tolerance and Facilitate Phonation in Tracheotomised Infants and Children with Upper Airway Obstruction.’ Workforce initiatives and achievements in 2010-11 include: the introduction of employee support officers, providing staff with confidential support for workplace issues; EMERGO Emergency Response training for key staff. Ten AKMH nursing educators completed Certificate IV in Training and Assessment, the current industry benchmark for staff development and ensuring a consistent approach to staff training across the hospital Federal funding for two RGH positions on the doctors’ specialist training program (geriatric medicine and general surgery). Additional Nurse Practitioner (NP) Post at FHHS designated to the Wound Management Service to a total of five NP’s at the hospital. Appointment of SMAHS Clinical Cluster Leads, their role being to engage staff and confirm future service delivery and workforce models for the AHS. A Graduate Diploma in Perioperative Nursing course was offered to FHHS nurses to develop skills and knowledge. Six new anaesthesia technicians graduated after completing a hospital-based training program and off-site tertiary studies and placements through FHHS. 58 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 Capital and infrastructure KEMH received $18.3 million for capital works to upgrade facilities. Wards 3, 4, 5 and 6 underwent refurbishment, resulting in improved storage facilities and additional work space for staff. Work also involved midwife stations and offices and neonatal assessment areas. The first stages of the KEMH Neonatal and Intensive Care Unit Expansion (NICU) and the KEMH Maternal Fetal Assessment Unit (MFAU) were completed in June 2011. The project aims to expand the Neonatal and Intensive Care Unit, enabling sufficient accommodation to meet current and immediate needs for the intensive care requirements of neonates. This will increase optimal safe operating capacity and improve operational workflows within MFAU thereby reducing demand pressures and waiting times and provide adequate space within the MFAU to ensure best practice quality of care and minimise patient safety risks. South Metropolitan Area Health Service Stage 2 of the Fiona Stanley Hospital (FSH) contract was signed with the Managing Contractor in August 2010, establishing a maximum sum for construction. The private sector preferred bidder for facilities management services was announced in October 2010. The project continues to be on time and on budget. Ward 1 at RPH Shenton Park Campus provides care to patients who are recovering from a brain injury. A $4.08 million upgrade has allowed the ward to be extended and refurbished. It now consists of 29 beds in four single bed rooms with no ensuites, four single bed rooms with ensuites, and one two-bed room, one three-bed room and four four-bed rooms. All exit doors are secured locked with new swipe card access. Stage 1 of the FHHS $5.7 million ICU/CCU project was completed on 6 October 2010. The refurbished $3.6 million Coronary Care Unit (CCU) has enabled the consolidation of all hospital heart services including cardiac catheter theatres, heart patients’ cardiac testing unit, and the hospital’s main operating theatres. Stage 2 of the hospital’s $5.7million ICU/CCU project was completed in June 2011 including an expansion of the Intensive Care Unit with an additional seven beds. Other FHHS work included replacing carpeted areas with vinyl throughout Fremantle and Kaleeya hospitals to minimise infection control issues, the redevelopment of the Emergency Department Triage/Waiting Area to include a designated consultation room for patients and expanded workspace for nursing and clerical staff and two new operating tables to accommodate bariatric patients were installed in FHHS theatres where the tables are electric, easier to move, and suitable for people weighing up to 450kg. Delivering a Healthy WA 59 Significant Issues North Metropolitan Area Health Service SKHS has completed the Stage 1 redesign of ED, the Community Midwifery Program (CMP) base at the hospital and the staff tutorial room as well as the refurbishment of the theatres and the morgue. Metropolitan Health Service Annual Report 2010-11 The RGH $115m redevelopment has been completed. FHHS Pathology Laboratory was refurbished to create a more efficient workspace and allow large, specialised equipment to be installed in the laboratory. Works began in February 2010 and were completed November 2010. Significant Issues The Rottnest Island Nursing Post received a new roof and a roof-mounted emergency communications link. A duress alarm system and new examination lights were installed. Equipment Acquisition and replacement North Metropolitan Area Health Service During 2010-11 Automated Cardiac Defibrillators were installed in the NMAHS mental health facilities, and policy/procedure and training for all non-inpatient areas to facilitate efficient response of medical emergency was carried out. SCGH purchased video stroboscopic equipment and commenced a voice clinic. The NMAHS purchased a ‘Panda’ Resuscitation Cot for the Nursery and two new camera stacks for theatres at OPH. SCGH purchased a constellation vitrectomy machine and a digital videostroboscopy unit for Ear Nose and Throat (ENT) clinical work and speech pathology to allow comprehensive assessment of voice and swallowing functions. The Medical Technology Management Unit (MTMU) at the WNHS implemented the Emergency Care Research Institute (ECRI) Asset Information Management System database across the health service improving tracking of medical systems and electronic record keeping, including service contracts and made significant investment in upgrading Neonatal equipment across KEMH and PMH. South Metropolitan Area Health Service During 2010-11 SMAHS undertook equipment acquisition and replacement including: For the AKMH new urology equipment, a Trans Rectal Ultrasound Scan and Biopsy Unit for prostate ultrasounds and biopsies, a service previously unavailable at the hospital, and advanced healthcare technology for the new Intensive Care Unit. A 64 slice CT scanner for RGH Medical Imaging Department. For Fremantle and Kaleeya hospitals ultrasound equipment for anaesthesia, an ICU hyperbaric unit, endoscopy, laparoscopic and vascular laboratory equipment, an ENT laser for Kaleeya Hospital theatre, an ophthalmic laser, patient monitors and anaesthesia induction units for theatres, two cardiothoracic heater/cooler systems, a liver ultrasound and a transportable foetal monitor for Kaleeya Hospital’s Maternity Unit. The FHHS Radiology Department is able to produce x-ray images in seconds and reduce a patient’s exposure to radiation by approximately 40% thanks to the purchase of cutting edge wireless, digital technology. 60 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 The purchase of Optical Coherence Tomography (OCT) allows FHHS Cardiologists to see 3D-images of cholesterol and clot damage directly inside a beating heart’s arteries. The three-dimensional imagery detects in real-time (while the heart is beating) the presence of cholesterol plaque or blood clot blockages within an artery. It also allows doctors to accurately view the placement of a stent. A new state-of-the-art mobile imaging and navigation system, part-funded and donated by the Fremantle Heart Patients Support Group, is correcting cardiac arrhythmia. The Carto 3 Navigation System has advanced imaging technology to treat patients with cardiac arrhythmias at FH. New technology has enabled a more comprehensive screening of newborns in the Kaleeya Maternity Unit (KMU). The testing, carried out by Kaleeya specialist newborn hearing screeners, ensures any hearing problems are picked up in their first month of life. The program screens newborns for permanent congenital hearing loss (PCHL) which occurs in one to two infants per 1,000 births. Telehealth and video conferencing Video conference services are used for emergency trauma management, remote patient diagnostics and follow-up consultation, patient observation and monitoring, distance education and staff training, broadcast of conference programs, administrative and collaborative project meetings, simulation observation and on occasion legal and court requirements. There are now 19 Telehealth locations and it is possible to access any Department of Health video conference from a desktop computer using a webcam. These options have dramatically increased service demand over 100% in 2011 from the previous year. It is anticipated by the end of 2011; over 1,000 occasions of service will have been provided. Delivering a Healthy WA 61 Significant Issues Hip and knee revision surgery at FHHS received a boost and donation to purchase a $90,000 piece of equipment to reduce trauma and improve surgical outcomes for patients. The Orthosonics System for Cemented Arthroplasty Revision allows surgeons to melt the cement surrounding an existing hip or knee replacement joint. Metropolitan Health Service Annual Report 2010-11 North Metropolitan Area Health Service SCGH provides regular involvement in speech pathology with the Dysphagia Interest Group via video conferencing and coordinates the National Renal Interest Group teleconferences for Dieticians’ Association of Australia. NMAHS has purchased two mobile units and facilitated the development of infrastructure to support telehealth at the SKHS. Significant Issues The WNHS has continued to develop Telehealth options across WA to provide patients with alternative methods to receive clinical services in rural and remote locations and has achieved increased occasions of service, provision of a dedicated Telehealth room and new equipment and implemented a Scopia Desktop to link into WA Health telehealth network events via a desktop computer. Telehealth is the focal point for video conferencing activity at CAHS coordinating administrative assistance, equipment and technical support to both internal and external clients. CAHS is committed to supporting and promoting telemedicine and Telehealth programs to all hospital sites and to our community partners. South Metropolitan Area Health Service SMAHS continued to utilise Telehealth throughout 2010-11 including: Use during cross-site Executive meetings and a combined governance committee across Health Services. Linking hospitals, remote medical sites and operating theatres anywhere in the world using video and audio technology. Clinical teachers and students benefit greatly because some surgery and medical procedures can be completed with supervision at tertiary and secondary sites. Ear Nose and Throat Surgeon, Professor Gunesh Rajan presented a paper on the merits of Telehealth to an ENT conference in Russia. He is currently using the technology to allow remote patients access for follow-up appointments post-surgery. Public health and ambulatory care The introduction of joint weekly multidisciplinary meetings between the Ambulatory Care Coordination Program (ACC), nurses and the Department of Paediatrics and Adolescent Medicine medical staff has improved communication, with subsequent increased utilisation of ACC and other Ambulatory Care Programs for children and their families. Nurse, Tess Zappia delivered a presentation of the ACC Program at the 6th National Australian Disease Management Association Conference. An article was also submitted for publication in a peer-reviewed paediatric nursing journal. The Ambulatory Daystay Facility accommodated 3,879 (total inpatients and outpatients) children over the financial year, representing a 15% increase compared to the previous year. A number of children involved in clinical research within the immunology and endocrinology specialties have received care in Daystay this year, to ensure a safer environment and closer monitoring. 62 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 The Botox Clinics are held in the Daystay area and have recently increased the number of patients from four to five at each clinic session, enabling increased numbers of children receiving this intervention. North Metropolitan Area Health Service RITH commenced at SCGH and the development of podiatry diabetes services at Joondalup continued. The WNHS Patient Flow Coordinator position within the Outpatient Department was reviewed and significant changes to the branding and role of the position were introduced. This position is now known as the Clinical Nurse / Nurse Manager Referral Coordinator, the role is designed to liaise with patients and triage the outpatient referrals. The patient focus of this service has been retained, ensuring that General Practitioners (GPs) are aware of the requirements for referral to individual clinics, and patients attend their first appointment with sufficient information to commence treatment/care options, with no delay caused by a need for further testing. After triage, a continuity process ensures appointments are attended and prioritised. During 2010-11 the planning and implementation of the metropolitan COAG NPA Preventative Health project – ‘Tomorrow People’ focusing on Aboriginal communities continued. This project supports the Commonwealth Measure Up- Social Marketing Project to prevent chronic disease focusing on nutrition and physical activity. Under the same NPA NMAHS Public Health Advisory Committee (PHAC) supported the City of Wanneroo in the implementation of the Healthy Communities Initiative within the local government area. The NMAHS also implemented a partnership with the City of Wanneroo to implement the Health and Wellbeing Project, completing a community report on specific issues to influence local government planning and prevention of chronic disease. NMAHS PHAC continued to develop local government population profiles across the Area Health Service (AHS) to support local government in chronic disease prevention. It supported City of Stirling and Town of Vincent in their submissions for COAG NPAHealth Communities Funding, and the Shire of Kalamunda in drafting their local public health plan. NMAHS PHAC continued the development and implementation of the Crossroads and Joondanna Community Gardens Project and implemented a small grants project across the AHS, with 16 funded and implemented Physical Activity and Healthy Eating projects. Implemented the Mirrabooka Social Inclusion Project incorporating the Health and Wellbeing, Aboriginal Leadership, and Cultural Awareness programs. In partnership with the Injury Control Council of Western Australia, NMAHS developed and implemented the Community Violence Project, developing a Community Violence Prevention Strategy for the NMAHS. Delivering a Healthy WA 63 Significant Issues The immunology wait list was targeted for the 2010-11 reporting period and successfully achieved a reduction from over 600 days to just over 300 days. Metropolitan Health Service Annual Report 2010-11 Developed a Culturally and Liguistically Diverse (CALD) Baseline Data Report to identify risk factors for CALD groups across the NMAHS to address chronic disease prevention. The SKHS provided active input into public health and community care activity integrating their service delivery via an ambulatory care service committee and liaising with the Perth Primary Care Network. Significant Issues As part of KEMH’s demand management initiative, the WNHS’s Public Relations Department developed ‘Having a Baby in Perth’ a new website providing women with more information about their pregnancy and birth choices in the metropolitan public health system. PMH Ambulatory Care continues to work closely with the paediatric units within the general hospitals located in the metropolitan area. Last year policies were established to enable direct referrals of children from both Armadale Hospital and Swan Kalamunda District Hospital directly to the PMH HITH Program. South Metropolitan Area Health Service The SMAHS ambulatory care program continues to expand across various programs to improve access to services so that patients can receive care closer to home and spend less time in hospital. Specific achievements include opening of a new outpatient unit at RGH with increased capacity of clinics and specialties now available to the local community as well as continuing the Moss Street Clinic which now provides ambulatory geriatric services including a falls clinic, memory clinic and continence clinic. The residential care outreach service has proved a useful liaison between residential care facilities and general practice to try and reduce hospital admissions. During 2010-11 the South Metropolitan Public Health Unit continued to implement the Health Promotion Strategic Framework 2007 – 2011 across the Area Health Service, delivering four health promotion projects targeting the risk factors for lifestyle related disease (tobacco, alcohol, physical activity and nutrition). Nutrition In 2011 the Maddington-Kenwick Fruit and Vegetable Project in five primary schools resulted in the development of the Planting and Cooking Guide for local schools, the establishment of a community kitchen at Maddington Primary School and over 450 parents and students participating in healthy nutrition learning at school events. The Planting and Cooking Guide teaches students how to grow fruit and vegetables in a school kitchen garden and cook healthy meals. The Unit worked in partnership with other stakeholders to establish the Armadale Farmers’ Market, which operated five times throughout 2010-2011 on the Kelmscott Senior High School grounds. The project incorporated the promotion and education of healthy eating and was used as a platform to involve the community, including local produce providers. Healthy eating messages were promoted at the market and ‘Go for 2&5’ health education resources were distributed. Cooking demonstrations, healthy cookbooks, tastings, food preparation sessions and public participation activities also took place. 64 Delivering a Healthy WA Alcohol Harm Minimisation Armadale Youth Binge Drinking Project – South Metropolitan Public Health Unit (SMPHU) worked in partnership with Armadale Youth Resources, City of Armadale, Police and Citizens’ Youth Club (PCYC) and WA Police and Drug Arm. The partnership resulted in Armadale Youth Resources successfully receiving a $250,000 Commonwealth Grant to address the issue of alcohol-related harm among Armadale youth. The funding has been used to deliver health education and participation activities for youth. Activities to date have included a Battle of the Bands competition (500 youth participating), Midnight Basketball program (70 youth per session), Youth Week BBQ (70 participants) and the creation of a PCYC Climbing Wall (1,460 youth involved over 12 weeks). Tobacco Cessation Indigenous Tobacco Cessation Program – An Aboriginal Health Worker was appointed to support Aboriginal people in Rockingham/Kwinana to stop smoking or reduce the likelihood of taking up the habit in the first place. Recommendations from this initial work are currently being developed, but include the development of a culturally secure education resource and Aboriginal artwork to deliver key messages. Physical Activity and Local Government Partnerships The Unit continued to progress the Be Active Belmont Project with the City of Belmont as part of a Physical Activity and Eating Plan 2010-2014. SMPHU has supported a number of events including Bike Week, Walk Week, Autumn River Festival, TravelSmart initiatives and the Healthy Living Seminar series for community members. The ongoing partnership has resulted in an increasing number of participants at each event in 201011. SMPHU worked closely with 16 other agencies in the Peel region to promote Bike Week. More than 468 participants ensured a National Cycling Promotion Foundation award being presented. RPH – Party program The PARTY (Prevention of Alcohol Related Trauma in Youth) Program has been operating at RPH for five years. Over 5000 high school students from the metropolitan area have attended the program during this time. In 2011, the program was extended to Bunbury Regional Hospital, providing an opportunity for students from regional areas to get an insight into injuries caused by risky behaviour. Communicable Disease Control A staff healthcare worker influenza vaccination program was implemented across SMAHS over a six-week period throughout March – May 2011. The staff take-up rate moderately increased from the 2010 program. The Unit will continue to implement strategies to maintain and improve influenza vaccination rates amongst heath care workers in SMAHS. Palliative Care for non-oncology Funding was secured in 2011 from the WA Cancer and Palliative Care Health Network to undertake a comprehensive service review and to develop a strategic plan for the way forward in relation to optimal models of care and staffing structure and resources. A project officer was employed to undertake a review of paediatric palliative care education and training, with the aim to develop state-wide resources through electronic learning and other mechanisms. Delivering a Healthy WA 65 Significant Issues Metropolitan Health Service Annual Report 2010-11 Metropolitan Health Service Annual Report 2010-11 Community Health Significant Issues South Metropolitan Area Health Service Initiatives were taken to implement the chronic disease models of care across the SMAHS (for example pulmonary rehabilitation classes were expanded including new classes at RGH). Considerable work has been done to build and develop relationships with community services and local GP networks. North Metropolitan Area Health Service The SKHS has developed linkages with the Epilepsy Association and implemented improvements in after hours GP clinic services. The Coaching On Achieving Cardiovascular Health (COACH) service was embedded into tertiary hospitals for a further three years. The Community Physiotherapy Service has received funding under the National Partnership Agreement (NPA) on Hospital and Health Workforce Reform- Schedule C: Subacute Care to expand the volume of service delivery. BreastScreen WA Under the BreastScreen Australia national mammography screening program, BreastScreen WA (BSWA) aims to reduce mortality and morbidity from breast cancer by actively recruiting and screening women aged 50 to 69 years for early detection of the disease. BSWA provides all services from the initial mammogram to any follow up diagnostic procedures required. Free, Statewide, accredited mammography screening is available for women aged 40 years and over, from eight metropolitan clinics, one rural clinic in Bunbury and four mobile van units. Breast assessment of screen detected abnormalities is provided at clinics located at RPH and SCGH. Thirteen x-ray units across all metropolitan clinics were upgraded to Full Field Digital Mammography (FFDM) which improves the ability to detect breast abnormalities in women with dense breast tissue and peri-menopausal women. An additional 3 FFDM machines were installed to increase the screening capacity. A fixed digital Breast Screening Van in the Bunbury Health Campus commenced in March 2011 replacing the two-yearly mobile Unit. This facility will provide all year round services to Bunbury and neighbouring towns. During 2010-11 the BreastScreen WA (BSWA) Services Plan was implemented addressing demand gaps for mammography services Statewide taking into account equipment upgrades, potential changes in national policy for screening target age group and other issues. A Call Centre Process Redesign is underway to address a large number of incoming calls from potential clients which were being lost. This process is looking at software upgrades, staffing needs and business workflow. A new strategy to attract Aboriginal lapsed attendees involving personal phone calls by the Indigenous Program Officer resulted in 15% of contacted women making a re-screen appointment. 66 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 BSWA aims to provide information in 30 languages and is able to provide interpreter services at appointments if required. The BSWA State Coordination Unit (SCU) is located in Perth and handles promotion and recruitment initiatives, appointments, film reading, client files, data collection and entry, the data registry, the mailing of screen invitations, reminders and result letters and the coordination of screening services. The Unit monitors and reports on program performance to both State and Commonwealth authorities, manages the financial aspects of the program and produces and disseminates promotional materials. Community mental health North Metropolitan Area Health Service During 2010-11 the NMAMHS undertook a review of Mental Health Emergency Services, implemented a standardised suite of services, developed definitions of Clinical Rehabilitation Pathways within the Recovery paradigm, and shared documentation for Consumer/NGO/Private/Public- Crisis Plans. The Women and Newborn Drug and Alcohol Service (WANDAS) introduced a satellite clinic at Bandyup women’s maximum security prison providing shared-care for pregnant incarcerated women, who have previously misused drugs and alcohol. In collaboration with the Parent Education Department, the WANDAS team has piloted a parent education session at the satellite clinic catering for the diverse prison community of approximately 180-240 women, 45% of whom are Aboriginal. South Metropolitan Area Health Service At the beginning of the 2010-2011, the Bentley Mental Health Service signed a Memorandum of Understanding (MOU) with Holyoake and Mission Australia. The MOU recognises the three parties agreement to work together to provide an extensive range of services to patients who require mental health care and rehabilitation for drug and alcohol addiction. The collaborative approach means patients will have easy access to additional services, resources and advice which was previously unavailable. The Acute Response Mental Health Course was developed in collaboration with the University of Notre Dame. First course participants completed in December 2010 and course evaluation is being undertaken. Approval has been received from the Human Research Ethics Committee for the Evaluation of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in a mental health setting (a joint research project with the Drug and Alcohol Office). SMAHS Mental Health is involved in a multicentre international trial of Schema Focussed Therapy as an alternative management for people with Borderline Personality Disorder. Delivering a Healthy WA 67 Significant Issues BSWA achieved the highest number of screens completed in one month since the program commenced with a total of 9,367 in May 2011. The total number of screens for the 12 month period June 2010 to May 2011 was 95,123. Total number of screens for the program up to end of May 2011 was 1,316,408. This total included total number of first screens: 318,064 and total number of later screens: 998,344. Metropolitan Health Service Annual Report 2010-11 Rural Care Coordination Significant Issues A Rural/Remote Tertiary Paediatric Partnership Program research study was completed during 2010-11. A nurse was employed to provide care co-ordination for children residing in the Kimberley and Goldfields who require care at PMH. This involved working in collaboration with medical and multi-disciplinary teams both within the rural and remote regions, as well as a PMH. The results from the study showed a 54% reduction in families who were required to make trips to PMH. A 26% reduction in bed days for the initial 60 participants in the research group was also achieved. The program accomplished significant cost benefits for the AHS through savings in the Patient Assisted Travel Scheme. It was highly regarded by both parents and health care professionals, with a number of health care outcomes improved through follow up treatment of patients who did not attend their set appointment, and by combining scheduled theatre procedures. The program was recognised by being named a finalist and ‘runner up’ at the WA Department of Health Awards 2010 Healthy Hospital Category. Technology Dependency Care The clinical nurse consultants (CNC) for technology dependent children focussed their efforts on developing new guidelines, updating protocols and working with community agencies - Perth Home Care and Lady Lawley Cottage High Needs Unit, to review all the education and training packages for children with technology dependency. The funding plans for children on the CATCH Program were also updated. Admitted mental health The Bentley Health Service Families at Work unit received refurbishments in the past financial year. The Unit was re-opened following a $100,000 upgrade. Renovations were made to the outdoor area, the unit was repainted and refurnished, and the program was redeveloped, making the unit friendlier for patients. This is a State-wide service providing mental health treatment for young people aged 8-13 with social, emotional and behavioural problems. The upgrade also allows for the service to be offered for day care services in addition to the previously available residential care services. A $460,000 facilities upgrade to the Bentley Mental Health Service was commenced in May 2011 to mitigate Occupational Safety and Health risks, improve the environment for the consumers of the service and in response to concerns raised by the Council of Official Visitors. RGH opened of dedicated mental health inpatient unit. FHHS staff were among the first to graduate from an Emergency Mental Healthcare Worker’s Course designed for staff who work in front-line areas of emergency mental healthcare. Participants included allied health and nursing staff. 68 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 The Reduction in Seclusion and Restraint project has led to a significant decrease in the use of seclusion and restraint in authorised units. Consumer and carer input into this project has been invaluable in making this a partnership in care. New dental therapy centres have been constructed at Deanmore, Girrawheen, Greenwood, Wattle Grove and Karratha. The redevelopment of Merredin and Yakamia Primary Schools has commenced and includes replacement of the dental therapy centres. Dental Health Services (DHS) has undertaken extensive community consultation in regard to fluoridation of public water supplies in Carnarvon, Dongara, Jurien Bay, Kununurra, Moora and Yanchep. DHS has implemented arrangements to ensure no reduction in service delivery at Aboriginal Medical Services in Geraldton, Kalgoorlie, Roebourne, Warburton and Wiluna. This service was previously provided by The University of Western Australia’s Centre for Rural and Remote Oral Health (CRROH). However, this service ceased with the WA Country Health Service at the end of 2010. To increase the uptake of oral health care and promotion for 0-4 year olds, DHS has introduced the following initiatives; ‘Children in Care’ programme - in partnership with the Department for Child Protection (DCP) the initiative ensures that all new children entering into the care of DCP from 2010 will receive a health and dental assessment. ‘Lift the Lip Program’ - provides training to metropolitan and rural/remote Child Health Nurses on dental disease and referral pathways for children accessing child health checks at 8, 18 and 36 months of age. Eligible children aged 0-4 years of age (dependants of Health Care Card or Pensioner Concession Card holders) can access subsidised oral health care and promotion through DHS dental clinics. DHS actively participates with a range of community organisations including educational authorities to provide oral health input into health lifestyle promotions, for example, obesity reduction programs. There is a national and international shortage of dentists, and it is estimated that by 2020 in Australia there will be an under supply of 800 dental clinicians. Over the past 10 years the DHS has experienced substantial difficulty in attracting and retaining sufficient numbers of dentists, dental therapists and dental clinic assistants. The Rural Dental Scheme has been the main recruitment vehicle for rural areas for the past three years and WA has been fortunate in implementing this program without competition from other States, although this is changing with the Eastern States jurisdictions commencing to recruit South African trained dentists. In September 2009 the Minister of Health and the Director General of Health commissioned Public Dental Health Services in Western Australia – A Functionality Delivering a Healthy WA 69 Significant Issues Dental Health Services Metropolitan Health Service Annual Report 2010-11 Significant Issues Assessment. The assessment was to examine how publicly funded dental services matched population needs and identify key issues for consideration for future service planning and delivery. Despite the gains realised in the oral health of the WA population, this Assessment has identified large disparities, inequities and unmet needs in nearly all areas of current service delivery but in particular: Children aged under five years Aboriginal and Torres Strait Islanders Western Australian adults aged 65+ years. prisoner population people with special needs The National Dental Foundation and DHS jointly participated in the Perth City Council’s Homeless Connect Day in November 2010. Both organisations provided clinical staff and DHS supplied two mobile dental vans for the day. This initiative enabled 59 eligible patients to receive dental care. DHS also provided a mobile dental van to the Town of Victoria Park Community Connect Day held in August 2010. PathWest The tender for a new laboratory information system has been released. Building work continues on the new laboratory facilities at QEII Medical Centre. PathWest continues to consult on the laboratory design for the Fiona Stanley Hospital complex. PathWest, in partnership with the University of Western Australia, continues to develop the curriculum for the Masters of Laboratory Medicine to be offered by the School of Pathology and Laboratory Medicine. The first student enrolments were offered in the discipline of Biochemistry. 70 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 Priorities 2011-12 Child and Adolescent Community Health Significant Issues In 2011-12 CACH will continue to develop partnerships with other stakeholders including providing services on school sites. The Child Development Information System (CDIS), a client and clinical information system currently used across metropolitan Child Development Service (CDS) sites, will be expanded to enable collection of data on the seven universal child health checks. This will enable CACH to collect reliable and accurate data for key community health services for the first time. CACH will also continue to work with staff at Princess Margaret Hospital (PMH) to improve discharge planning and ensure continuity of care for children and families. Child and Adolescent Mental Health During 2011-12 the Child and Adolescent Mental Health Service (CAMHS) will develop a CAMHS Model of Care to identify priority areas for investment and ensure improved access to services. CAMHS will implement a consolidated organisational structure promoting a culture of excellence, innovation and customer focus, develop the emergency and assertive community service, and enhance the CAMHS workforce by improved training and development opportunities and by increasing the range of multidisciplinary staff (such as Aboriginal mental health workers). Four Hour Rule Child and Adolescent Health Service During 2011-12 the Child and Adolescent Health Service will examine its processes to better manage the seasonal increase in patient presentations and the PMH FHR Team will continue to support the fourteen ‘Lean Teams’ who are undertaking challenges to identify waste and improve workflow within various departments to achieve the FHR target. The team will continue to provide support and advice to the outpatient reform team regarding the use of Clinical Services Redesign Methodology to inform this reform process. South Metropolitan Area Health Service While RPH continues to routinely meet the 85 per cent target for the FHR, sustaining this performance in 2011-12 will be a priority. To ensure this, the hospital will focus on initiatives that will reduce ambulance ramping and decrease the overall length of a patient’s stay. As the Bentley Hospital and Health Service will fall under the governance of RPH in 2011-2012, there will also be opportunities to develop closer relationships and initiatives between the two hospitals to ensure the continued management of patients. In 2011-12, the AKMH is expected to achieve its first target of 85 per cent with many noteworthy changes including: Opening of a Transit Lounge replacing the current Discharge Lounge accommodating patients awaiting discharge and those waiting for a ward bed. The new lounge will assist with patient flow through the hospital. Delivering a Healthy WA 71 Metropolitan Health Service Annual Report 2010-11 Placing display screens in prominent areas providing FHR information to patients, visitors and staff. Developing an Acute Admission Unit to assist in the management of both acute medical and surgical patients; and Significant Issues Further develop the management of acute medical patients in the clinical areas with an improved senior medical staff structure, clinically appropriate patient average length of stays, and ensure the completion of discharge summaries to enable more timely coding of patient records. At the RGH in 2011-12 improvements to patient flow will continue with a rapid assessment team and team-based care in the emergency department and improved pharmacy processes to facilitate the provision of discharge medication with the introduction of “Script Tracker” allowing ward staff to track the progress of a patient prescription without phoning Pharmacy. At FHHS strategies to maintain the FHR achievements so far will include the purchase of a stretcher and electric passenger-carrying vehicles, the development of an Integrated Paediatric Service, introduction of electronic journey boards and improving patient and junior medical officer discharge education. North Metropolitan Area Health Service The WNHS will continue to progress the FHR including: The introduction of the Script Tracker program to address demands on pharmacy to dispense discharge medications. The refurbishment of the Agnes Walsh Lodge to accommodate rural and remote women and their babies experiencing delays whilst awaiting PATS services. The development of a training program for shift co-ordinators. The development of visual aids displaying expected length of stay for hospital-wide use, streamlining process for Breast Pump Hire and improved access to a central location. The development of educational DVD for Breast feeding women with babies in Neonatal Critical Care Unit (NCCU) to address demand for this service. Streamlining clerical work and the development of Clinical Pathways for the top five Diagnosis Related Groups to assist with postnatal discharge paperwork. The development of 22 guidelines for care of the ward neonate to facilitate neonatal discharge. The development of Triage Midwife and shift co-ordinator role for the Maternal Fetal Assessment Unit (MFAU). The installation of electronic tracking system for MFAU patients to capture activity. The disposition of each presentation and the development of management outcome plans for clinic patients transferred to MFAU. 72 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 Child and Adolescent Health Service To further increase the percentage of patients who have their procedure completed within their respective clinical timeframe a new electronic booking system (EBS) will be implemented in late 2011. The waitlisting of patients will then be completed electronically by medical staff, rather than on hardcopy forms. The appropriate consent will be electronically tagged to the waitlist form. It is anticipated the outcome of this will see a dramatic reduction in the time spent locating waitlist and consent forms. South Metropolitan Area Health Service RPH will continue to focus on developing strategies that will help reduce elective surgery waitlists. In 2011-12, RPH will prepare a business case to upgrade two Wellington Street Campus theatres to manage high risk orthopaedic cases in an effort to reduce those waiting for surgery at the Shenton Park Campus, review theatre capacity at sites and identify more readily those cases appropriate for surgery at Shenton Park, undertake a review of the scheduling and allocation processes of theatre sessions across emergency and non-emergency surgery, and tighten pre-operative procedures to reduce surgery cancellation including better communication with the patient and early discharge planning prior to operation. North Metropolitan Area Health Service At SCGH the elective access redesign program will commence Aboriginal Health Under the Aboriginal Health Worker Wound Education Program (AHWWEP), the MHS ill support the expansion of the AHW Wound Education Program into Aboriginal Medical Services in the Great Southern, Kimberley and Pilbarra regions, continue collaborations with Marr Mooditj Training Centre to implement a new wound management curriculum for Enrolled Nurses, and promote the AHW WEP as the agreed national standard for wound education for AHW’s. Child and Adolescent Health Service The CAHS Aboriginal Health Team will continue to develop career pathways for Aboriginal staff including the reclassification of aboriginal health workers, the development of enrolled nurse positions and pathways for graduate nurses, progress the implementation of the Enhanced Aboriginal Child Health Schedule, and the Moorditj Yarning Kulungas program will be evaluated and refined as appropriate prior to implementation across the metropolitan area. South Metropolitan Area Health Service The SMAHS will continue to progress proposals under the South Metropolitan Aboriginal Health Plan and the aboriginal health projects funded by COAG and WA Health for the next 3-4 years. Delivering a Healthy WA 73 Significant Issues Elective Surgery Metropolitan Health Service Annual Report 2010-11 North Metropolitan Area Health Service Planning and increasing the Aboriginal and Torres Strait Islander workforce including the implementation of NMAHS Aboriginal Employment Strategy 2011 – 2015 featuring attraction and retention strategies, workforce skill development, promoting appropriate workforce culture and environment and facilitating workforce design. Significant Issues WNHS will progress scoping the role of Aboriginal Health Workers within KEMH and include the Statewide Coordinator on the NMAPCC to provide advice and input to policy, that encompasses the Reconciliation Action Plan (RAP) and establish a family meeting ground on KEMH site. Telehealth Child and Adolescent Health Service CAHS has submitted a business case to employ a Telehealth Support Officer to further enhance the level of clinical video conferencing occasions of service, promote the use of Telehealth Services (on-site and Statewide), ensure Telehealth capacity in design plans for new/refurbished areas and improve the evaluation processes of Telehealth services. North Metropolitan Area Health Service The AHS proposes to resource more videoconferencing equipment for OPH, and at the WNHS support increased staff to meet demand, increase the level of video conferencing occasions of service, ensure the ability to facilitate Telehealth in design plans for new areas and improve service evaluation. Metropolitan Child Development Service Further partnerships will be developed in 2011-12 for the provision of social work and psychological services, services to Aboriginal families, paediatric services and early intervention play-based programs. Public health and ambulatory care North Metropolitan Area Health Service During 2011-12 NMAHS PHAC will progress the implementation of its Reconciliation Action Plan (RAP) across all sites, inviting increased input into policy development; contribution and participation in NMAHS RAP, and promoting Aboriginal and Torres Strait Islander cultural leadership in strategic development especially in Regional and State forums. The AHS will continue facilitating the COAG initiatives for ‘Closing the Gap’ and in population health including expanding accommodation for these programs and utilising the COAG funded Aboriginal Liaison Services initiated by NMAHS and Derbarl Yerrigan. The NMAHS PHAC will also: Increase the volume of clients in service and implement diversification of services. Continue with volume expansion of the Community Physiotherapy Service. Minimise the spread of communicable diseases through correct follow up of notifications, case investigations, management and contact tracing of notifiable diseases. Complete, implement and maintain the Pandemic Plan for the NMAHS. Promote immunisations to Health Care Workers (HCW), Primary Care HCW and staff within Residential Care Facilities and Child Care Centres as opportunities arise. 74 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 Support the rollout of the ‘Healthy Councils: Healthy Communities Resource’ for the Local Government Areas within NMAHS. Child and Adolescent Health Service CAHS with promote a collaborative approach with specialist departments to increase access to HITH as an alternative to hospital inpatient stay: Developing with the Department of Respiratory Medicine policies and pathways to facilitate continuous positive airway pressure in non-invasive ventilation and to undertake oxygen saturation monitoring studies in the home. Submitting an endocrinology and ambulatory care research proposal to various funding bodies to trial an Ambulatory Care Diabetes Pathway for newly diagnosed Type I diabetes. A research study to compare cost, patient health related quality of life and clinical outcomes for patients on subcutaneous immunoglobulin (SCIg) replacement via pump or push, versus hospital based intravenous immunoglobulin (IVIg) replacement. The Rural/Remote Partnership Program will continue for children residing in the Kimberley region with proposals submitted to expand to other rural areas, especially the development of a paediatric Telehealth service to avoid unnecessary visits to PMH for children residing in rural and remote areas across WA. Working to secure dedicated medical sessions for the ambulatory care service to improve medical governance and leadership, including antibiotic therapy stewardship. A statewide paediatric palliative care education package will be completed and made available to healthcare workers across WA. A collaboration with Joondalup Health Campus to develop a policy whereby children from the Children’s Unit at Joondalup can refer directly to the PMH HITH program. South Metropolitan Area Health Service New initiatives for 2011-12 include enhancement of Cardiac Rehabilitation and General Rehabilitation services in the community. SMAHS will develop and implement actions to further enhance ambulatory care services based on the WA Health Primary Health Care Strategy. During 2011-12 the SMAHS Public Health Unity Unit will continue to implement the Health Promotion Strategic Framework 2007 – 2011 (and subsequent plans), delivering health promotion projects targeting risk factors for lifestyle related disease (tobacco, alcohol, physical activity and nutrition). The Unit will continue its work with the local Aboriginal community and service providers to develop local, culturally secure strategies for the Aboriginal population. South Metropolitan Public Health Unit will continue to deliver communicable disease control services in SMAHS. In 2011-12, the SMPHU will again coordinate and implement the staff healthcare worker influenza vaccination program in SMAHS hospitals. The Unit will report on influenza vaccination coverage for this group. Delivering a Healthy WA 75 Significant Issues Continue to support, develop, implement and evaluate the following projects: ‘ Tomorrow People’, ‘NESB Program’, ‘Healthy Communities’ ‘Healthy Workers’ ‘Community Gardens Project’ and the ‘Community Violence Project’. Metropolitan Health Service Annual Report 2010-11 WoundsWest The WoundsWest Advisory Service (WWAS) is to be piloted in outlying metropolitan hospitals and one or more Aboriginal Medical Services, and implemented across all WACHS sites. Significant Issues Under the Online Wound Education Program two or more online wound education modules will be developed. Conduct a “Train the Trainer” program on the modules with staff development nurses in major tertiary teaching hospitals. It will also investigate translation of modules into other languages. Under Wound Education - Translation into practice, the MHS will investigate the otential for common undergraduate wound education for health professionals and will liaise with the Divisions of General Practice to incorporate wound management into professional development programs. Service Development South Metropolitan Area Health Service AKMH expects to see an increase in the number of more complex hip replacement cases referred from tertiary hospitals and the retention of more complex general surgical patients. Progress RGH to its full capacity of 209 beds including general and mental health and expand the graduate program to include graduate midwifery. Radiotherapy equipment at RPH will be replaced with Genesis Care providing state-ofthe-art radiotherapy services for the hospital. Staff shortages across several medical and non-medical disciplines, is a particular concern and will be the focus of recruitment strategies in 2011-2012. This will include developing alternative workforce models to address the shortage of midwives, theatre nurses and ward nurses. Develop a medical workforce plan that will clearly outlines the transition from a fee for service medical workforce to a mixed salaried and fee for service model. A dedicated stroke unit is scheduled to open at BH in September 2011. The dedicated 10-bed unit will be located within the existing rehabilitation ward, with the beds reallocated to provide stroke patients with more specialised rehabilitative care. Commonwealth funding of $1.3 million will be used for an additional 12 FTE positions for medical, nursing and allied health staff. 76 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 A midwife practitioner in diabetes. A midwifery group practice planned for the Family Birth Centre. Implementing an additional afterhours nursing staff in Occupational Therapy. Expansion of a ‘Pelvic Pain Clinic’. Providing additional urology sessions to address demand issues and significant funding for an additional Fellow and Senior Nurse. At SCGH; Developing Clinical Nurse roles for Plastics and Orthopaedics. Follow up issues identified in thepatient journey mapping session held with the Department of Plastic Surgery (identifying patients suitable for a secondary facility). Implement a one system booking process for surgery, initially in plastic surgery, with the view that other specialties would follow. at SKHS: Salaried surgeons will be recruited. Emergency theatre use will be introduced. Facilitate service growth for Rehabilitation In The Home (RITH), Hospital In The Home (HITH) and Hospital At The Home (HATH). A Geriatric Evaluation Medicine (GEM) Unit is to be established at SCGH. SCGH will also participate in developing updated Nutritional Specifications for Hospital Food Services at WA tertiary and secondary sites and specifically update the hospital’s menus to be consistent with outcomes of the Nutritional Specifications. SCGH will move to place current Assistants In Nursing (AIN) students in permanent positions and provide a learning environment for future AIN students. An amputee outreach service is to be provided at SCGH. In addition: Medical salaried consultant model and the junior doctor rotation education program will be completed at the SKHS. Family friendly employment strategies will be enhanced,. Integrate and improve service delivery with NMAHS and the Wheatbelt as part of the Southern Inland Health Initiative. Develop an appropriate rotational paediatric service model for Northam. Implement a Parkinson service and improve out-patient neurology. Facilitate the development of a stroke unit. Implement a planned COPD area-wide service via a QUIP proposal in conjunction with SCGH and JHC. Delivering a Healthy WA 77 Significant Issues North Metropolitan Area Health Service Across the NMAHS a number of workforce and service development initiatives will be progressed including at WNHS: Metropolitan Health Service Annual Report 2010-11 Capital and infrastructure development projects Significant Issues South Metropolitan Area Health Service During 2011-12 the SMAHS will continue to oversee the construction and commissioning of the Fiona Stanley Hospital, especially in relation to the provision of facilities management services and progressing the furniture, fittings and equipment requirements of the hospital, and will continue to ensure that the project remains on time and on budget During 2011-12 planning for building works will commence to expand hospital services at the RGH. This is Stage 2 of a two stage upgrade required to reach general hospital status and develop an improved model of governance for women’s and children’s health by combining them in one clinical area. The Bentley Health Service will commence the design and development of a $4.2 million Commonwealth funded refurbishment to Ward 5 to accommodate 18 extra aged care rehabilitation beds scheduled for completion in 2012-13. The FHHS Acute Endoscopy Unit will undergo a complete refurbishment to address safety and quality issues. Royal Perth Hospital will prepare business cases to upgrade the following facilities: Plastics Department and Clinic. Medical Oncology Day Treatment area. Catheter Laboratory. Theatres at Wellington Street Campus. Ambulatory Surgicentre. North Metropolitan Area Health Service During 2011-12 capital works to enhance full theatre capacity at SCGH will be undertaken and work will commence on an intra-operative MRI suite. Commonwealth funds totalling $22.5 million have been allocated to DPH infrastructure to build two new theatres, additional procedure room and consultation rooms, scheduled for completion in April 2014. WA Health has agreed to apportion a parcel of land to Telethon to construct a Juvenile Diabetics Centre at the OPH site. At the SKHS the re-design of Stages 2, 3 and 4 for the Swan emergency department is in progress and the pharmacy upgrade at Kalamunda will continue. In conjunction with the WNHS implement the redevelopment of therapies and ambulatory service areas at Kalamunda Hospital. The WNHS has facilitated the purchase of the nearby Subiaco Police Station to expand ambulatory care services with a new Ambulatory Care Centre at the site. The final stages of the Neonatal Intensive Care Unit and Maternal Fetal Assessment Unit are scheduled for completion in early December 2011. 78 Delivering a Healthy WA Metropolitan Health Service Annual Report 2010-11 For the NMAHS Mental Health Service, the design, tender and building commencement of the new Mental Health Inpatient Unit at SCGH will occur in 2011-12 as well as the planning, approval and design of a new Mental Health Inpatient Unit at the OPH. Equipment Acquisition and Replacement South Metropolitan Area Health Service Demand for MRI outpatients has increased substantially in recent years and to meet this demand, RPH will commission in August 2011 a second MRI scanner at a cost of $2 million plus building works. This new scanner will treat up to 20 outpatients each day, allowing the current scanner to be utilised for inpatients. The two scanners together will help reduce length of stay for inpatients and outpatient waiting lists. North Metropolitan Area Health Service At a number of sites across the AHS budgeted equipment acquisition and replacement programs will be continued, particularly for bed replacement at the SKHS and the purchase of simulation manikins for education and training of medical staff, a new ultrasound machine, the purchase of additional Level 2 monitors for Special Care Nursery and a cremator for peri-natal pathology at the WNHS. Admitted Mental Health Following formal approval and gazetting of the RGH mental health unit by the Chief Psychiatrist, secure beds in the unit will be opened, bringing the unit to its full capacity at 30 beds. Community Mental Health At the NMAHS Mental Health Service the implementation and evaluation of Team Service Delivery policy and structures will continue as well as the implementation of a 360 degree feedback and performance development review process. BreastScreen WA During 2011-12 BSWA will undergo national re-accreditation with BreastScreen Australia in February 2012 and host the BreastScreen Australia Digital User Group conference in March 2012. The service proposes to replace the four existing Mobile Breast Screening Units with new Mobile Units equipped with Full-Field Digital Mammography technology by December 2012 and is working with the HIN to develop a Picture Archiving Computer System (PACS) and softcopy reading of Digital Mammograms in 2012. BSWA will trial a secure electronic messaging of results letters to General Practitioners, with a view to implement an electronic ‘Result Letter’ system to provide up to thirty per cent of GP practices with electronic notifications and result letters. The new Bunbury Breast Assessment Centre is schedule to open in October 2012 in collaboration with the St John of God Health Bunbury Regional Cancer Centre to provide Delivering a Healthy WA 79 Significant Issues The relocation of the Department of Nursing and Midwifery Education and Research (DNAMER) will commence during 2011-12. Significant works will be undertaken in the Hospital Sterile Supplies Department (HSSD) to comply with Australian Standards for the sterilisation of equipment. Metropolitan Health Service Annual Report 2010-11 local breast assessment services to the women in the South West. Additionally the service aims to open a new BreastScreen WA Rose Clinic in Perth in the Murray Street David Jones Store, as part of the national partnership between David Jones and BreastScreen Australia. Significant Issues BSWA plans to develop a five year TV media campaign, sponsored by Atlas Iron, with the aim to promote awareness and uptake of mammography screening Statewide and facilitate health promotion for rural and remote areas. The Service aims to implement an online appointment booking facilities to existing clients. The Service plans to implement an SMS reminder system to encourage women to attend who are overdue for a screening mammogram. Dental Health Services A functional assessment of public dental services in Western Australia has been submitted to the State Health Executive Forum. This assessment will identify the current state of service provision and provide an evidence based framework for determining where current services can be redirected or where additional services are required. In addition the DHS will commence the implementation of computerisation for school dental service records to replace the current manual administrative and clinical systems. Dental Health Services will be part of a Department of Health review of the classification structures for all dental occupational groups. The objective will be to establish a sustainable classification regime which is recognised as essential for sustaining public dental services in WA. PathWest PathWest will undertake the selection of a replacement laboratory information system and commencement of commissioning the solution. The transition to the new laboratory building at the QEII Medical Centre will be progressed as well as the plan for the relocation of services from RPH and FHHS laboratories to the new Fiona Stanley Hospital. 80 Delivering a Healthy WA