Title: Detection of antibiograms, calss I integron and antibiotic
advertisement

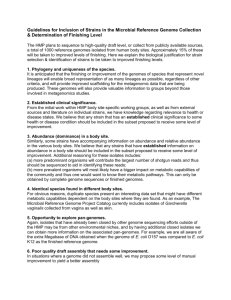
Title: Detection of antibiograms, calss I integron and antibiotic resistance genes for Salmonella Choleraesuis strains isolated from swine in southern Taiwan JEN-CHIEH PANG1, TSAI-HSIN CHIU1, WEN-ZHE HWANG1, MING-HUEI LIAO2, GAN-NAN CHANG2 AND HAU-YANG TSEN1*. 1 2 * Department of Food Science, National Chung-Hsing University, Taichung, Taiwan, R.O.C. Department of Veterinary Medicine, National Ping-tung University, Ping-tung, Taiwan, R.O.C. Corresponding author: Hau-Yang Tsen, Professor Department of Food Science, National Chung-Hsing University, Taichung, Taiwan, R.O.C. Abstract Antibiotic susceptibilities for 95 Salmonella Choleraesuis strains collected from the swine field in Southern Taiwan were analyzed. A total of 17 antibiotics were tested. Results showed that 43 antibiograms were obtained. All these 95 strains were multidrug resistant strains. PCR was used to screen the genes encode for the resistance to ampicillin (PSE group), streptomycin-spectinomycin (aadA), kanamycin (aphA), sulfadiazine (sulI), trimethoprim (dfrA12), chloramphenicol (cat, cmlA) and the presence of class I integron. Results showed that 32.6% of the 95 strains of Salmonella Choleraesuis have the class I integron. The antibiotic resistance genes in integron cassette were further analyzed by PCR mapping. Five types of patterns including dfrA12-aadA2, oxa1-aadA, dfrA12-aad2-su1l, pse and dfrA12 were found. Our data demonstrated that the problem of antibiotic resistance for Salmonella Choleraesuis need to be paid with attention, since this Salmonella species has recently emerged as the major species for swine infection in Taiwan. . Key words: Salmonella Choleraesuis, integron, antibiogram. INTRODUCTION Antibiotics have been used in the therapeutic, subtherapeuitic and growth promotion for domestic animals, such as swine, in many countries (Aarestrup, et al., 2001). Many antibiotics used for human are also used as feed additives in Taiwan, for example, avoparcin, virginiamycin, kanamycin and enrofloxacin, that analog to vancomycin, kanamycin, gentamicin ciprofloxacin, ofloxacin, quinupristin, and dalfopristin. Certain antibiotics are critical for human use because there is no other drug available for the treatment of human infected by multi-drug resistant pathogens, or because alternative therapies are less effective or are associated with increased side effects. There are now an increasing number of reports suggesting that critical forms of antibiotic resistance arise in human pathogens as a result of using certain antibiotics in food-producing animals, and that such resistance can be transmitted to humans via the food chain (Molbak, et al., 1999; Smith, et al., 1999; Stobberingh, et al., 1999; Soltani, et al., 2000; McDonald, et al., 2001). In 2000, the Council of Agriculture in Taiwan prohibited the use of several antimicrobial agents, such as avoparcin, kanamycin, kitasamycin, lasalocid, spiramycin, salinomycin, and streptomycin, which had been widely used as growth promoters or prophylactic agents in animal husbandry in Taiwan during the past 2 to 3 decades (Hsueh, et al., 2002). In Taiwan, recent reports have shown the widespread emergence of reduced-susceptibility and full-resistance to fluoroquinolones among human isolates of Salmonella spp (Ho, et al., 1999; Chiu, et al., 2002). In recent years, S. Choleraesuis has become the most frequent isolated Salmonella serotype from swine. The hosts of this Salmonella spp. could be swine and humans (Bäumler, et al., 1998). Thus, regular surveillance of S. Choleraesuis in domestic animals could be helpful for human health. An efficient route of acquisition and vertical and horizontal dissemination of resistance determination is through mobile elements including plasmids, transposons, and gene cassettes in integrons (Stokes, et al., 1989; Recchia, et al., 1995). Recent advances in molecular characterization of antibiotic resistance mechanisms highlighted the existence of integrons (Hall, et al., 1995), those integrons contain many different antibiotics gene cassettes (Mazel, et al., 1998; Fluit, et al., 1999). A class 1 integron has the following formal arrangement (Bennett, et al., 1999): IntI attI (r59b)n qacEΔ1 sul1 orf5 ofr6. Where r59b represents a resistance gene cassette and n indicates the number of gene cassettes integrated at the locus. The set of gene cassettes are currently known to accommodate genes that confer the resistance of many antibiotics. To elucidate the relationship of antibiotics resistance between the phenotypes and the genotypes, in this study, we assayed the antibiotics resistance susceptibility for S. Choleraesuis isolates from swine fields in Southern Taiwan and used the PCR to detect their the resistance genes. MATERIAL AND METHODS Strains Salmonella Choleraesuis strains were obtained from swine fields in southern Taiwan. They were isolated during the period of 2000 to 2002. 67 of these 95 strains were isolated from diarrhea swine and 28 isolated strains from systemic infection swine by the Department of Veterinary Medicine, National Pingtung University, Pingtung, Taiwan. Reference strains that have been identified to have integrons map were obtained from the National Laboratory of Food and Drug, Department of Health, Taipei. Those strains were S. Typhimurium U302 from chicken, S. Typhimurium DT008 from egg yolk, S. Typhimurium from beef, S. Schwarzengrund from chicken. All the isolated strains were grown on Tryptic Soy broth (TSB) and were stored frozen at -80℃ for future transfer. Antibiotic susceptibility testing The 95 of S. Choleraesuis isolates were subcultured onto Mueller-Hinton agar (BD) for disk diffusion. Antibiotic susceptibilities of these isolates were determined according to the guidelines of National Committee for Clinical Laboratory Standards (NCCLS). 17 of antimicrobial agents were used. The antibiotic and its conc. per disc were contained ampicillin (10μg), amoxicillin-clavulanic acid (20 and 10μg), gentamicin (10μg), cephalothin (30 μ g), chloramphenicol (30 μ g), erythromycin (15 μ g), tetracycline (30 μ g), sulfamethoxaeole-trimethopmin (1.25 and 23.75μg), norfloxacin (10μg), ciprofloxacin (5μg), ofloxacin (5μ g), nalidixic acid (30μg), sulfonamides (300μg), strepmycin (10μg), carbencillin (100μg), kanamycin (30μ g), and stretionmycin (10μg). Determination of the susceptibility were according to the NCCLS standard breakpoint for gram-negative enteric organisms. Escherichia coli ATCC 25922, the control strain, was routinely used. PCR amplification and sequence Bacteria cells were grown on TSB overnight at 37℃, then transfered 100l culture to 3ml TSB, and incubated for 8h. The cells were collected and lysed by heating at 100℃ for 10 min. 10l of cell dilution (approximately 105 CFU/10l) was mixed with PCR buffer (10mM Tris-HCl, pH 8.8; 1.5mM MgCl2; 50mM KCl; and 0.1% Triton X-100), 200 pmol each of dATP, dGTP, dCTP, dTTP (Boeheringer Mannheim, Germany), 50 pmol each of the PCR primer, and 0.2 U ProTaq. The PCR conditions were denaturation at 94℃ for 5 min followed by 35 cycles of 94℃, 30s; 60℃, 30s; 72℃, 30s, and a single final extension of 10 min at 72℃. PCR amplification specific for pse group (AmpicillinR), dfrA12 (Sulfamethoxaeole- trimethopmin or TrimethoprimR), oxa1 (AmpicillinR), aadA1a (streptomycinR and spectinomycinR), aphA (kanamycinR), cmlA (chloramphenicol R ), sul, QS (SulfonamideR), aadB (Gentamycin R), cat (Chloramphenicol R) (Table 1) genes were carried out. The amplified products were analyzed by electrophoresis on 2% agarose gel. Integron analysis The integrons in Salmonella strains were detected using primers 5’CS-3’CS, and intI1F-intI1R (Table 1). These primers were specific for integron conserved segments and class I integronase gene. For the primers 5’CS-3’CS, DNA from target bacteria was amplified during 35 cycles of 94℃, 30 s; 55℃, 30 s; 72℃, 2 min. PCR conditions for primers intI1F-intI1R was the same as those for the analysis of antibiotic resistance genes. The amplified product was examined by electrophoresis on 2% agarose gel. RESULTS Antibiotic susceptibility test Results from the antimicrobial susceptibility test are shown in Table 2. The total strains could be grouped into 43 antibiotic resistant patterns. All the 95 strains were multi-drug resistant strains. They were resistant to two to fifteen antimicrobial agents. For example, strains in pattern No. 38 were resistant to 15 kinds of antimicrobial agents. All of the isolates were resistant to nalidixic acid and sulfonamides (100%), which have been grouped to quinolones and folate pathway inhibitors. More than 80% of the strains were resistant to ampicillin (89.5%), erythromycin (80.0%), tetracycline (93.7%), kanamycin (80.0%), and carbenicillin (87.4%). All of the 95 isolates were susceptible to amoxicillin-clavulanic acid, which was -lactam and -lactamase inhibtor combination. About 21.1 % to 24.2% isolates were fluoroquinolone- resistance (norfloxacin 21.1%, ciprofloxacin 21.1%, and 24.2%) (Table 3). The result also presented that S. Choleraesuis isolates from systemic infection were more antibiotics resistant than the diarrhea isolates. For example, the fluoroquinolone- resistant strains were only found in systemic infection. PCR amplification of the antibiotic resistance gene Nine PCR primer pairs specific for antibiotic resistant genes were used for screening of the 95 S. Choleraesuis isolates. The results showed that 30 of 95 isolates (31.6%) have dfrA12 gene, 1 of 95 isolates (1.1%) have pse gene, 29 of isolates (30.5%) have aadA1a gene, 82 of 95 isolates (86.3%) have aphA gene, 1 of 95 isolates (1.1%) have oxa1 gene, 29 of 95 isolates (30.5%) have cmlA gene, 26 of 95 isolates (27.4%) have qs gene, were PCR positive while aadB and cat genes were not found. The sizes of all the PCR products were as expected (Table 1). Integron analysis Results from the determination of the class 1 integron in these 95 S. Choleraesuis isolates showed that 31 strains (32.6%) were with the class 1 integron. Most of the strains from systemic infection swine harbored the integrons. As 5’CS and 3’CS primers were used to amplify the integrons of 31 strains. PCR products obtained showed that the sizes of integrons were in between 650 to 2100 bp. Integronase gene also have been detected with int1F and int1R primer pair. All of the 31 strains with class I integron generated positive reactions. They all generated a 280 bp product. Further PCR analysis for antibiotic resistant genes was then performed for these 31 strains which harbored integrons. Five patterns, including dfrA12-aadA1a, oxa1-aadA1a, dfr12-aadA1a-sul, pse and dfrA12 patterns were found (Table 4). These integrons preferentially harbored one or two of dfrA12, aadA2, and pse gene cassettes. The 1500 bp integron size was found to encode for the streptomycin-spectinomycin and -lactams resistance, i.e., with the oxa1- aadA1a gene cassettes. Other four types of gene cassettes belong to an integron of 2100 bp size, which encode for the resistance to trimethoprim- sulfonamides and -lactams. DISCUSSION Antibiotics are often used in domestic animals for therapy and prophylaxis of bacterial infections and for promotion of their growth. The use of antibiotics for domestic animals may cause problems in the therapy of infections due to the antibiotic resistance of bacterial pathogens which infected animals or humans (Aarestrup, et al., 1999). In this study, we incestigated the antibiotic resistant patterns for S. Choleraesuis isolates from swine. The antibiotics surveyed were those commonly used for clinical therapy and animal treatment. High percentage of these strains were found to be antimicrobial resistant and multi-drug resistant. Because of the emergence of multiple resistant bacteria which may cause infection in humans, some antimicrobial agents have now become last line-drugs in treatment of the bacteria infection. Chiu, et al. (2002) reported that approximately 90% of S. Choleraesuis isolates from humans was found to be resistant to at least one of the following antibiotics, ie, ampicillin, chloramphenicol, and trimethoprim-sulfamethoxazle. Also, the rate of floroquinolone resistant strains was 60 percent. In this study, we found that for S. Choleraesuis isolates from swine, the rate of ampicillin resistant strains was about 90%, chloramphenicol resistant strains was 76%, trimethoprim-sulfamethoxazle resistant strains was 33% and floroquinolone resistant strains was about 21%. The lower rates of resistant strains for isolated from swine might be due to the samples from different sources. For example, human isolates were generally obtained from patients with blood and other organs infection, and swine isolates were obtained from swine withdiarrhea (about 70%) and systemic infection (30%). However, almost all the isolates from systemic infection were resistant to those three antimicrobials. Ampicillin, chloramphenicol, and sulfa drugs have been recognized as standard first-line drug for the therapy of Salmonella infection. If human infections were caused by Salmonella with multidrug-resistance, all of these antibiotics will be ineffective, and treatment of Salminella infection will be difficult. In Taiwan, those antimicrobial agents are no longer the drugs of choice for treatment of serious nontyphoidal Salmonella infection. Cephalosporins and floroquinolone are now the preferred drugs for treatment of invasive Salmonella infection (Yang, et al., 1998). However, emergence of floroquinolone resistance would change the policy for treatment of S. Choleraesuis infection on humans or swine in Taiwan (Chiu, et al., 2002; Aarestrup, et al., 2003). As for the detection of antibiotic resistance genes by PCR, positive PCR results did not coincide exactly with the phenotype. This could be due to the following reasons. First, the phenotype of antimicrobial resistance was due to the expression of several different resistance genes. For example, resistance to ampicillin may be due to oxa1, oxa2, and pse genes or others. Second, that resistant gene was unexpressed, such genes may be pseudo-genes, which may have not complete regulator region including promoter. By using PCR mapping with primers specific for integrons, the major finding of this study was that class 1 integron carrying the dfr12- aadA1a was widely distributed in S. Choleraesuis isolates from swine in Taiwan. If S. Choleraesuis strains were resistant to streptomycin, spectinomycin, and sulfamethoxaeole-trimethopmin, the class 1 integron carrying the gene cassettes of this type could be found. Surveillance and monitoring of antimicrobial-drug resistance of S. Choleraesuis from animals, including the work of screening for class 1 integrons, are necessary steps in study of epidemiology and gene evolution of antimicrobial resistance. ACKNOWLEDGMENTS This project is supported by the Nation Science Council, Taipei, Taiwan. The project No. is NSC 91-2313-B-005-074. REFERENCE Aarestrup, F. M. 1999. Association between the consumption of antimicrobial agents in animal husbandry and the occurrence of resistance bacterica among food animals. Int. J. Antimicrob. Agent 12:279-285. Aarestrup, F. M., A. M. Seyfarth, H.-D. Emborg, K. Pedersen, R. S. Hendriksen, and F. Bager. 2001. Effect of abolishment of the use of antimicrobial agents for growth promotion on occurrence of antimicrobial resistance in fecal Enterococci from food animals in Denmark. Antimicrob. Agents Chemoth. 45:2054-2059. Aarestrup, F. M., C. Wiuff, K. Mølbak, and E. J. Threlfall. 2003. It is time to change fluoroquinolone breakpoints for Salmonella spp.? Antimicrob. Agents Chemoth. 47:827-829. Alessandra, C., I. Luzzi, L. Villa, and E. Filetici. 2001. Serotype distribution, antimicrobial resistance and detection of class 1 integrons among Salmonella enterica isolated in Italy. Second Interational Virtual Conference on Pork Quality, December, 06, 2001. Bäumler, A. J., R. M. Tsolis, T. A. Ficht, and L. G. Adams. 1998. Evolution of host adaptation in Salmonella enterica. Infect. Immuno. 66:4579-4587. Bennett, P. M. 1999. Integrons and genecassettes: a genetic construction kit for bacteria. J. Antimicrob. Chemoth. 43:1-4. Bert, F., C., Branger, and N., Lambert-Zechovsky. 2002. Identification of PSE and OXA beta-lactamase genes in Pseudomonas aeruginosa using PCR-restriction fragment length polymorphism. J. Antimicrob. Chemother. 50:11-8. Boyd, D., A. Cloeckaert, E. Chaslus-Dancla, and M. R. Mulvey. 2002. Characterization of variant Salmonella genomic island 1 multidrug resistance regions from serovars Typhimurium DT104 and Agona. Antimicrob. Agents Chemoth. 46:1714-1722. Hsueh, P.-R., C.-Y. Liu, and K.-T. Luh. 2002. Current status of antimicrobial resistance in Taiwan. Emeng. Infect. Dis. 8:132-137. Chiu, C. -H., T.-L. Wu, L.–H. Su, C. Chu, J.-H. Chia, A.-J. Kuo, M.-S. Chien, and T.-Y. Lin. 2002. The emergence in Taiwan of fluoroquinolone resistance in Salmonella enterica serotype Choleraesuis. 346:413-419. Fluit, A. C., and F. J. Schmitz. 1999. Class 1 integrons, gene cassettes, mobility, and Epidemiology. Eur. J. Clin. Microbiol. Infect. Dis. 18:761-770. Frana, T. S., S. A., Carlson, and R. W., Griffith. 2001. Relative distribution and conservation of genes encoding aminoglycoside-modifying enzymes in Salmonella enterica serotype typhimurium phage type DT104. Appl. Environ. Microbiol. 67:445-448. Guerra, B., S. M. Soto, J. M. Arguelles, and M. C., Mendoza. 2001. Multidrug resistance is mediated by large plasmids carrying a class 1 integron in the emergent Salmonella enterica serotype [4,5,12:i:-]. Antimicrob. Agents Chemother. 45:1305-8. Hall, R. M., and C. M. Collis. 1995. Mobile gene cassettes and integrons: capture and spread of gene by site-specific recombination. Mol. Microbiol. 15:593-600. Ho, M., L. C. McDonald, and T. Lauderdale. 1999. Surveillance of antibiotic resistance in Taiwan, 1998. J. Microbiol. Immunol. Infect. 32:239-249. Lévesque, C., L., Piché, C., Larose, and P. H., Roy. 1995. PCR mapping of integrons reveals several novel combinations of resistance genes. Antimicrob Agents Chemother. 39:185-191. Mazel, D., and J. Davies. 1998. Antibiotic resistance. The big picture. Adv. Exp. Med. Biol. 456:1-6. McDonald, L. C., M.-T. Chen, T. L. Lauderdale, and M. Ho. The use of antibiotics critical to human medicine in food-producing animals in Taiwan. 2001. J. Microbiol. Immunol. Infect. 34:97-102. Molbak, K., D. L. Baggesen, F. M. Aarestrup, J. M. Ebbesen, J. Engberg, K. Frydendahl, P. Gerner-Smidt, A. M. Peterant, and H. C. Wegener. 1999. An outbreak of multidrug-resistant, quinolone-resistant Salmonella enterica serotype typhimurium DT104. N. Engl. J. Med. 341:1420-1425. National Committee for Clinical Laboratory Standards. 2000. Preformance standards of three categories of susceptibility testss; approved standard, 7th ed., M2-A7. National Committee for Clinical Laboratory Standards, Wayne, Pa. Ng, L. K., M. R., Mulvey, I., Martin, G. A., Peters, and W., Johnson. 1999. Genetic characterization of antimicrobial resistance in Canadian isolates of Salmonella serovar Typhimurium DT104. Antimicrob. Agents Chemother. 43:3018-3021. Orman, B. E., S. Piñeiro, S. Arduino, M. Galas, R. Melano, M. I. Caffer, D. O. Sordelli, and D. Centrón. 2002. Evolution of multiresistance in nontyphoid Salmonella serovars from 1984 to 1998 in Argentina. Antimicrob. Agents Chemoth. 46:3963-3970. Recchia, G. D., and R. M., Hall. 1995. Gene cassettes: a new class of mobile element. Microbiol. 141:3015-3027. Rodrigue., D. C, D. N. Cameron, N. D. Puhr, F. W. Brenner, M. E. ST. Louis, I. K. Wachsmuth, and R. V. Tauxe. 1992. Comparison of Plasmid Profiles, Phage Types, and Antimicrobial Resistance Pattern of Salmonella enteritidis Isolates in the United States. J. Clin. Microbiol. 30: 854-857. Rowe-Magnus, D. A., and D., Mazel. 1999. Resistance gene capture. Curr Opin Microbiol. 2:483-488. Sandvang, D., F. M. Aarestrup, and L. B., Jensen. 1998. Characterisation of integrons and antibiotic resistance genes in Danish multiresistant Salmonella enterica Typhimurium DT104. FEMS Microbiol. Lett. 160:37-41. Smith, K. E., J. M. Besser, C. W. Hedberg, F. T. Leano, B. J. Bender, J. H. Wicklund, B. P. Johson, K. A. Moore, and M. T. Osterholm. 1999. Quinolone-resistant Campylobacter jejuni infection in Minnesota, 1992-1998. N. Engl. J. Med. 340:1525-1532. Soltani, M., D. Beighton, J. Philpott-Howard, and N. Woodford. 2000. Mechanisms of resistance to quinupristin-dalfopristin among isolates of Enterococcus faecium from animals, raw meat, and hospital patients in Western Europe. Antimicrob. Agents Chemother. 44:433-436. Stobberingh, E. van den B. A., N. London, C. Driessen, J. Top, and R. Willems. 1999. Enterococci with glycopeptide resistance in turkeys, turkey farmers, turkey slaughterers, and (sub)urban residents in the south of The Netherlands: evidence for transmission of vancomycin resistance from animals to humans? Antimicrob. Agents Chemother. 43:2215-2221. Stokes, H. W., and R. M. Hall. 1989. A novel family of potentially mobile DNA elements encoding site-specific gene integration functions: integrons. Mol. Microbiol. 3:1669-1683. Vatopoulos, A. C., E. Mainas, E. Balis, E. J. Threlfall, M. Kanelopoulou, V. Kalapothaki, H. Malamou-Lada, and N. J. Legakis. 1994. Molecular Epidemiology of Ampicillin- Resistant Clinical Isolates of Salmonella enteritidis. J. Clin. Microbiol. 32:1322-1325. Yang, Y.-J., C.-C. Liu, S.-M. Wang, J.-J. Wu, A.-H. Huang, and C.-P. Cheng. 1998. High rates of antimicrobial resistance among clinical isolates of nontyphoidal Salmonella in Taiwan. Eur. J. Microbiol. Infect. Dis. 17:880-883. TABLE 1. PCR primers used in the identification of integrons and antibiotic resistant gene. primers sequence target 5’CS 3’CS intI1F GGC ATC CAA GCA GCA AGC intI1R PSE G1 TCC ACG CAT CGT CAG GC ACC GTA TTG AGC CTG ATT TA PSE group (PSE-1, PSE G2 ATT GAA GCC TGT GTT TGA GC PSE-4,CARB-3 , ) dfr12-F dfr12-B oxa1-F oxa1-R ACT CGG AAT CAG TAC GCA dfrA12 ant-3’-1aF ant-3’-1aB aphA-1L aphA-1R cat-F cat-B aadB-F GTG GAT GGC GGC CTG AAG CC aadB-B cmlA-F cmlA-B sul1-F sul1-R QS-1 QS-2 CTG TTA CAA CGG ACT GGC CGC specific antibiotic resistant accession no. M73819 Levesque, et al., 1995. integrase I - M73819 Orman, et al., 2002 oxa1 aadA1a ATT GCC CAG TCG GCA GCG aphA 321 trimethoprim AF175203 ampicillin AJ009819 streptomycin, spectinomycin kanamycin M10241 U63147 Guerra, et al., 2001. 462 Sandvang, et al., 1998. 708 Sandvang, et al., 1998. 527 Ng, et al.,1999 489 GAG AAA ACT CAC CGA GGC AG CCT GCC ACT CAT CGC AGT cat chloramphenicol U46780 CCA CCG TTG ATA TAT CCC GAG CGA AAT CTG CCG CTC TGG TGTCATTTACGGCATACTCG aadB cmlA gentamycin chloramphenicol ATCAGGCATCCC ATT CCC AT CCT CGA TGA GAG CCG GCG GC sul GCA AGG CGG AAA CCC GCG CC ATG AAA GGC TGG CTT TTT CTTG TGA GTG CAT AAC CAC CAG CC 280 Bert, et al., 2002. ampicillin ATT CGA CCC CAA GTT TCC TTA TGC CTC TTC CGA CCA TC - - GTG TAC GGA ATT ACA GCT AGC AGC GCC AGT GCA TCA product size (bp) integron AAG CAG ACT TGA CCT GAT CCC TCC CGC ACG ATG ATC reference qac/sul1 sulfonamide AF078527 M64556 Guerra, et al., 2001. 632 Frana et. al., 2001 310 Guerra et al., 2001. 435 Sandvang et al., 1998. 437 Boyd et al., 2002 850 TABLE 2. Antiograms of Salmonella Choleraesuis isolates from swine in southern Taiwan. Type Antibiogarm No. of strain Strain 1 AmpGmCfCETSxtNaSuSpSCbK 1 SCV02 2 AmpGmCfCETSxtNaSuSpSCb 1 SCV03 3 AmpGmETNaSuCbK 1 SCV04 4 AmpCETNaSuCbK 7 SCV05, SCV06, SCV08, SCV15, SCV19, SCV46, SCV47 5 AmpGmCETNaSuCbK 11 SCV07, SCV09, SCV28, SCV38, SCV39, SCV40, SCV44, SCV50, SCV52, SCV58, SCV59 6 AmpGmCETSxtNaSuSCbK 1 SCV10 7 AmpGmCETSxtNaSuCbK 3 SCV11, SCV32, SCV71 8 ENaSu 3 SCV12, SCV18, SCV66 9 AmpCTNaSuCbK 1 SCV13 10 AmpETNaSuSpCbK 1 SCV14 11 GmETNaSu 1 SCV16 12 AmpGmCfETNaSuCbK 2 SCV17, SCV65 13 AmpGmCETNaSuSCbK 8 SCV20, SCV24, SCV30, SCV31, SCV36, SCV49, SCV57, SCV64 14 AmpCTNaSuCb 1 SCV22 15 AmpGmCfCETNaSuCbK 2 SCV23, SCV69 16 AmpGmCfCETSxtNaSuSpS 1 SCV25 17 ETNaSu 2 SCV26, SCV27 18 AmpTNaSuCbK 1 SCV29 19 AmpCETNaSu 1 SCV33 20 GmCNaSuS 1 SCV34 21 AmpTNaSuSCbK 1 SCV35 22 AmpGmCfCETNaSuSCbK 2 SCV37, SCV42 23 AmpCETNaSuCb 1 SCV41 24 ETNaSuS 2 SCV43, SCV53 Type Antibiogarm No. of strain Strain 25 AmpETNaSuCbK 3 SCV45, SCV55, SCV70 26 AmpGmENaSu 1 SCV54 27 AmpGmETNaSuSCbK 1 SCV60 28 CTNaSuS 1 SCV61 29 AmpGmCETNaSu 1 SCV62 30 AmpGmCETNaSuCbK 1 SCV63 31 AmpGmCTNaSuS 1 SCV67 32 GmCETNaSuCbK 1 SCV68 33 AmpCfETSxtNaSu 1 SCV72 34 AmpGmCETSxtNaSuSCb 2 SCV1a, SCV 17a 35 AmpGmCTSxtNorCipOflNaSuSpSCbK 7 SCV 2a, SCV 3a, SCV 4a, SCV 6a, SCV 8a, SCV 11a, SCV 14a 36 TSxtNorCipOflNaSu 1 SCV 5a 37 AmpGmCETSxtNorCipOflNaSuSpSCbK 11 SCV 9a, SCV 10a, SCV 12a, SCV 13a, SCV 15a, SCV 18a SCV 22a, SCV 23a, SCV 24a, SCV 26a, SCV 27a 38 AmpGmCfCETSxtNorCipOflNaSuSpSCb 1 SCV 16a 39 AmpCETSxtNaSuSpSCbK 2 SCV 19a, SC 40 AmpGmCETSxtOflNaSuSpSCb 1 SCV 20a 41 AmpGmCETSxtNaSuSpSCbK 1 SCV 21a 42 AmpGmCETSxtNaSuSpSCb 1 SCV 25a 43 AmpCTSxtNaSuSpSCbK 1 E55 Amp:ampicillin AMC: amoxicillin-clavulanic acid Gm:gentamicin Cf:cephalothion C:chloramphenicol E:erythromycin T:tetracycline Sxt:sulfamethoxaeole-trimethopmin Nor:norfloxacin Cip:ciprofloxacin Ofl:ofloxacin Na:nalidixic acid Su:sulfonamides Sp:strepmycin S:stretionmycin Cb:carbencillin K:kanamycin TABLE 3 . Phenotypes of antimicrobial resistance for S. Choleraesuis isolates Clsaa and/or antimicrobial % Resistance strains (n=95) Penicillins Ampicillin 89.5% Amoxicillin-clavulanic acid 0% Carbenicillin 87.4% Aminoglycosides Gentamicin 67.4% Streptomycin 70.6% Kanamycin 80% Cephalosporin I Cephalothin 7.4% Phenicols Chloramphenicol 75.8% Tetracycline 93.7% Sulfonamides and potentiated sulfonamides Trimethoprim-sulfamethoxazole 32.6% Sulfonamides 100% Quinolones and fluoroquinolones Nalidixic acid 100% Ciprofloxacin 21.1% Norfloxacin 21.1% Ofloxacin 24.2% Macrolides Erythromycin 80% Aminocyclitols spectinomycin 31.6% TABLE 4. Genotypic and phenotypic characteristics for antibiotic resistance of Salmonella Choleraesuis isolates. AMP Strain SCV02, SCV03, SCV24a SCV62 SCV1a TMP STR KAN CHL GEN SUL qacE/ oxa1 blaPSE dfrA12 aadA1a aphA cat cmlA aadB sul1 sul - - + + + - + - - - + - + + + - - - - - - + + + + - + - + + integron pattern integron size dfrA12-aadA2 ~2100 bp oxa1-aadA2 ~1500 bp dfrA12-aadA2-sul1 -2100 bp pse SC, E55 SCV2a, SCV3a, SCV4a, SCV5a, - - + - + - + - + + dfrA12 -2100 bp - + + + - + - + + dfrA12-aadA2-sul1 -2100 bp - - + + - - + - - - dfrA12-aadA2 -2100 bp - - + + - - + - + + dfrA12-aadA2-sul1 -2100 bp - SCV6a, SCV9a, SCV10a, SCV11a , SCV12a, SCV13a, SCV14a, SCV15a, SCV18a, SCV19a , SCV21a, SCV22a, SCV23a, SCV26a, SCV27a SCV8a ,SCV16a, SCV17a , SCV20a, SCV25a a. Amp: ampicillin 10μg per disk, Neo: Neomycin 30μg per disk, Chl: Chloramphenicol 30μg per disk, Kan: Kanamycin 30μg per disk, Str: Streptomycin 10μg per disk, Sul: Sulfonamide 250μg per disk, Cef: Cefoperazone 75μg per disk, Sxt: Trimrthoprim-sulfamethoxazole, Nor: Norfloxacin 10μg per disk, Tet: Tetracyclin 30μg per disk. 1 2 3 4 5 6 7 8 9 10 11 M a b c d e f g h i jM k l m n o p q 12 13 14 15 16 17 18 19 20 Fig. 1 PCR amplification of the integrons and gene cassettes for S. Choleraesuis 21 22 23 24 25 26 isolates. Lane M: 100 bp ladder marker; lane a-d: products of 5’CS/3’CS primer pair of SCV2, SCV62, SCV1a, and SCV2a; lane e-g: gene cassettes of dfrA12, aadA1, and dfrA12-aadA1 of SCV2; lane h-j: gene cassettes of oxa-1, aadA1, and oxa-1-aadA1 of SCV62; lane k-m: gene cassettes of dfrA12, aadA1,and sul1 of SCV1a; lane n-p: gene cassettes of dfrA12, aadA1,and sul1 of SCV2a; lane q: gene cassettes of dfrA12 of E55.