1.4.2.d.4 Viral Hepatitis Prevention & Control
advertisement

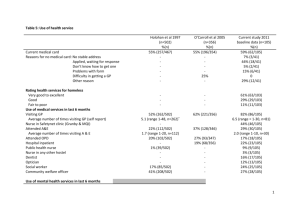
1 HEALTH SERVICES DELIVERY 1.4 DISEASE CONTROL PROGRAMME 1.4.2.d.4 Communicable Diseases Control: Immunizable Diseases Control: Viral Hepatitis Prevention & Control (as of March 2008) A B Focal Point Implementing Agencies C Target Areas & Beneficiaries Epidemiology Unit Epidemiology Unit Provincial Director of Health Services Regional Director of Health Services Medical Officer of Health Curative Care Institutions (All hospitals) Target Areas: MOH Areas, Curative Care Institutions Beneficiaries: Community in respective MOH areas, Health workers of curative care institutions Project Summary: Viral hepatitis (VH) comprises of at least five disease entities, which are indistinguishable clinically, yet totally different aetiologically and pathologically. Hepatitis A accounts for the majority of cases in the country. In addition, serious consequences of hepatitis B have been identified as emerging public health issues. Therefore it is important to have a national programme on control and prevention of VH with following activities: 1. Assess burden of VH in the country Establish a National Task force on control and prevention of VH in Sri Lanka Strengthen surveillance (particularly laboratory surveillance) of VH Improve excreta disposal system at local settings Ensure safe drinking water Introduce of Hepatitis A vaccine for high risk groups Strengthen law enforcement in order to ensure environmental sanitation Ensure universal infant immunization against hepatitis B Justification: Viral Hepatitis (VH) is one of the notifiable diseases in Sri Lanka. Hepatitis A is the commonest type of viral hepatitis in the country. It is endemic in almost all parts of Sri Lanka, and occurs throughout the year. The average annual admission rate to government hospitals in Sri Lanka for VH is 22.5 per 100,000 populations in 2001. However, the actual incidence of VH is likely to be more than that of reported numbers. The hospital mortality rate is 0.4%. Data on other types of VH in Sri Lanka are limited. Prevalence of hepatitis B and C ranges from 0.27% to 2.5% and 0.56% to 0.97% respectively. These data are based on epidemiological and serological surveys done in defined geographical areas in the country. Health authorities have not given sufficient priority for prevention and control of VH. Laboratory surveillance of VH is limited due to many constraints. Direct and indirect impact of socioeconomic and political /administrative re-organization on public health issues, such as unsafe water, unauthorized constructions on increase of VH in the country are significant. There is a timely need to have a functioning national programme on control & prevention of VH in Sri Lanka. This programme has to cover all possible aspects, where active intervention could be implemented. 2. Important Assumptions/ Risks/ Conditions: Assumptions: Government commitment and policy to prevent and control VH Commitment by the Department of Health with the other sectors, such as local government to control and prevent VH, as a priority in public health Public need to have a active programme on control and prevention of VH and their support and active participation into the programme Risk / Conditions: 3. Cost: Screening for types of VH, injection safety practices and immunization are important strategies in implementing a successful preventive and control programme. However, this will require an additional financial commitment by the Ministry and inability to provide such facilities would affect the expected outcome. Project Objective: Objective Indicators Prevention and Morbidity and mortality Control of Viral Hepatitis of VH in Sri Lanka 4. Means of Verification Survey: review of Medical statistician and Institution records / community survey Project Output/Product: Outputs VH morbidity and mortality reduced Indicators Hospital admission rate MOH notifications Case Fatality Rate of VH All infants immunized % immunized against Hep B and the high risk groups immunized against Hep B and Hep A Universal precautions % of immunizations strengthened with regard to performed with Auto all invasive procedures Disable(AD) syringes at all medical institutions / clinics VH surveillance Notification rate of VH strengthened Timeliness notification Means of Verification Review data at Epidemiology Unit and Medical Statistician records Record and returns Hospital records Epidemiology Unit Review at Epidemiology data Unit Timeliness and completeness of special investigations Notification of VH from private sector surveillance Number of functioning Provincial / district laboratories with facility to carry out VH investigations % of laboratory confirmed cases Laboratory strengthened 5. Hospital and laboratory based survey Related Projects: Project No. 6. and Medical Statistician records Project Title Hepatitis B Immunization Programme for infants and selected high risk groups: (ongoing) Hepatitis A Immunization Programme for high risk groups Injection safety programme – Provision of Auto-disable syringes (ongoing) Provision of Safe Drinking Water Provision of hygienic latrine facility Provision of laboratory facility at the Provincial / district level for VH laboratory investigations Relevant Agencies to be Coordinated: Ministry of Local Government and Public Administration, Ministry of Education, Ministry of Water Supply and Drainage, All Provincial councils and other related Ministries 7. Monitoring & Evaluation: 1. Who? Director General of Health Services and Epidemiology Unit 2. When? Quarterly 3. What actions to be taken based on results of monitoring & evaluation? Continues reviews with Provincial / District / Divisional Health Authorities Periodical reviews with other relevant agencies to be coordinated 8. Activities: Activities 1 Establish a National Task Force Control and Prevention of VH Expected Results for Policy formulation / Implementation level coordination M & E major activities at Process Indicators Regular quarterly meeting 2 3 Conduct VH Burden study (Part of this study will be based on secondary data) Establish Hepatitis B Immunization Programme 4 Establish Hepatitis A Immunization Programme for high risk groups 5 Establish Injection safety programme – Provision of Auto-disable syringes (ongoing) 6 Strengthen VH Surveillance 7 Provide of laboratory facility at the Provincial/ District level for VH laboratory investigations 8 Establish and maintain a surveillance system to maintain water quality national level To estimate morbidity, mortality and disabilities caused by each type of VH in the country Cost analysis for patient management at the government medical institutions Immunization of all infants against Hepatitis B Immunization of all high risk groups/adolescents against Hepatitis B Immunization of all high risk groups against Hepatitis A Use AD syringes for all immunizations Improved notification of VH (both State & Private sector) Investigation of all VH outbreaks Early prediction of out breaks Strengthened laboratory Surveillance Surveillance on water quality established Final report to be made available before end of year 2005 95% coverage by 2005; 100% in 2007 & 2010 50% coverage by 2006; 60% in 2008; 70% in 2010 50% coverage by 2006; 60% in 2008 70% in 2010 100% EPI vaccines by 2005 100% Non EPI Vaccine by 2007 % Notification ra Timeliness & completeness % of outbreaks investigated % of outbreaks predicted Functioning laboratory by province by 2010 > 50% reported cases are confirmed by laboratory tests by 2010 100% Timeliness and completeness of laboratory reports by 2010 % of districts which have the surveillance on water quality established