NORMAL LIVER FUNCTIONS
advertisement

NORMAL LIVER FUNCTIONS
1. Hepatocytes
Albumin formation
Clotting factors (Vitamin K dependant)
Immunoglobulin
Bile juices
Metabolism of CHO, Proteins, Lipids
Detoxify the Drugs & Bio-transformation
Storage of Iron, B12, Glycogen etc…
2. Reticulo endothelial Cells
Sinusoid (immunity)
3. Ito Cells (in space of disse)
Vitamin “A” storage
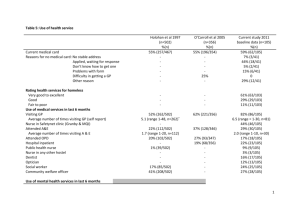
TEST
LIVER FUNCTION TEST
(LFT)
NORMAL VALUE
Bilirubin
Direct (Conjugated)
Indirect (Un conjugated)
< 1.2
2.
AST (SGOT)
5 – 40 units/L
3.
ALT (SGPT)
5 – 35 units/L
4.
Alkaline Phosphate
30 – 115 units/L
5.
Serum Albumin
3.5 – 5.5 g/dL
1.
0.1 – 0.3 mg/dl
0.1 – 0.7 mg/dl
CLOTTING FACTORS
I
---------Fibrinogen
II
---------Prothrombin
III
---------Tissue Thromboplastin
IV
---------Ca++ Factor
V
---------Proaccelerin
VI
---------Labile Factor
VII ---------Stable Factor
VIII ---------Anti Hemophilic Factor A
IX
---------Christmas Factor (Anti Hemophilic Factor B)
X
---------Stuart Prower Factor
XI
---------Anti Hemophilic Factor C
XII ---------Hageman Factor
XIII ---------Fibrin Stabilizing Factor
1
COAGULATION PATHWAY
EXTRINSIC PATHWAY
INTRINSIC PATHWAY
Factor III
XII----------------------XIIa
VII ------------------------ VIIa
XI -----------------------XIa
VII Complex
(VIIa, III, Ca++, Phospholipid)
IX -----------------------IXa
VIII Complex
(VIII, IXa, Ca++, Phospholipid)
COMMON PATHWAY
X-------------------------Xa
V Complex
(V, Xa, Ca++, Phospholipid)
Prothrombin-----------------Thrombin
Fibrinogen --------------------------Fibrin
XIII
Fibrin Polymer
2
JAUNDICE
Def: - It is the yellowish discoloration of Sclera & Skin because of Hyperbilirubinemia
> 3 mg/dL.
Types
Pre-Hepatic
(Hemolytic)
Hepatocellular
Post Hepatic
(cholestatic)
Bilirubin Metabolism
Breakdown of Red blood Cells
Heme + Globulin
Heme
Fe++ removed
Enters in liver
Attached with albumin
Unconjugated Bilirubin
Albumin is dissociated
Bilirubin taken by Hepatocytes
Biliverdin
conjugated with Glucuronic acid
Excreted in bile
HYPERBILIRUBINEMIA
Predominant
Indirect Hyperbilirubinemia
Predominant
Direct Hyperbilirubinemia
Congenital Causes
Criggler- Nijjar Syndrome
Gilbert’s Syndrome
Physiologic Jaundice of new born
Congenital Causes
Dubin Johnson Syndrome
Rotor Syndrome
Acquired
Infective Erythropoiesis
Hemoglobin Breakdown
Hematoma
Acquired
Hepatitis
3
Criggler- Nijjar Syndrome
It is of two types
In type I Syndrome there is Absolute deficiency of Glucuronyl Transferase.
In type II Syndrome there is Partial deficiency of Glucuronyl Transferase.
Gilbert’s Syndrome
It is the most common congenital Hyperbilirubinemia
In this case there is Partial deficiency of Glucuronyl Transferase & also there is some
defect in entry of Bilirubin in Hepatocytes.
Dubin Johnson Syndrome
In this syndrome defect is in excretion of conjugated Bilirubin from
caniliculi because there is catamine like substance which is attached to Bilirubin.
Rotor Syndrome
In this syndrome there is defective Bilirubin uptake & reduced intrahepatic
binding. Its inheritance is Autosomal dominant.
How to evaluate a Case of Jaundice from Hepatitis?
History
H/o Occupation
Sewerage Worker ------------------------------- Leptospirosis (Weil’s Disease)
Address
Low socioeconomic status ------------------------ Hepatitis A
H/o Exertional Dysponea
H/o Pallor
H/o Pruritus (Obstructive Jaundice / Cholestesis)
Colour of stool (Clay colour {Obstructive})
Colour of urine
Dark
(Conjugated)
Acholuria
(Unconjugated)
H/o Blood Transfusion (Glass Syringes)
H/o Sexual Contacts
H/o Alcohol intake
H/o Rash
H/o Pigmentation
H/o Drugs (Phenylbutazone, Isoniazid, Rifampicin, Anti Psychotic, Anti
depressants, Sulfonamides, Methotrexate, MAO Inhibitors etc…)
Examination
General Physical
Anemia
Jaundice
Duprytron’s Contracture
Palmer Erythema
4
Spider Nevi
Edema
Lymph Nodes
Bruises & Petechiae
Abdominal Examination
Liver size
Tenderness
Liver span
Spleen
Ascities
Murphy’s Sign
Courvoisor’s Law
(Hepatomegaly)
TREATMENT
PRE-HEPATIC
Treat the cause
HEPATIC JAUNDICE
General Management
Bed Rest
Plenty of Fluids
High Calories Intake
Syp: Hepamerz
Specific Management
Treat the cause
POST HEPATIC JAUNDICE
General Management
Bed Rest
Plenty of Fluids
High Calories Intake
Syp: Hepamerz
Treatment of Pruritus
Cholestyramine
(Questran 4 mg)
Specific Management
Treat the cause
5
HEPATITIS
Def: - It is the inflammation of Liver Parenchyma.
Types of Hepatitis
1. Viral Hepatitis
2. Drug Induce Hepatitis
3. Alcoholic Hepatitis
4. Parasitic Hepatitis
5. NASH (Non-Alcoholic Steato Hepatitis)
6. NAFLD
Viral Hepatitis
It is of two types
Non- Hepatotrophic Virus(Cytomegalo Virus, Herpes, Adeno, Coxseckie, EBV)
Hepatotrophic Virus
o Hepatitis B
------------------------
DNA Virus
o Hepatitis A
o Hepatitis C
o Hepatitis D
--------------
RNA Virus
o Hepatitis E
o Hepatitis G
6
HEPATITIS “A”
It is belongs to picornavirus group of enterovirus
It is RNA virus
Its size is 27 nm
Route of transfusion is Orofaecal
Caused by Poor Hygiene, over crowding, poor sanitation etc …
Incubation Period is 30 days (CMDT) & 2 – 4 weeks (Davidson)
Within 2 – 3 weeks of incubation Virus appears in Faeces
PHASES
1.
Prodomal phase
Lethargic, Anorexia, Malaise, Nausea, Vomiting
2.
Icteric Phase (10-15 days)
Jaundice
3.
Convalescent Phase
Sign & symptom are start to resolve
4.
Recovery Phase
DIAGNOSIS
Ig M for Hepatitis “A”
TREATMENT
Symptomatic Treatment
PREVENTION
“HAV” Vaccine
COMPLICATIONS
Hepatitis “A” does not leads to Chronic Hepatitis
The only & very Rare complication is Acute Fulminant Liver.
7
HEPATITIS “B”
It is belongs to Hepadna Virus
It is only DNA virus causing Hepatitis
Its size is 42 nm
Route of transfusion is Parenternal (Blood Transfusion, glass syringe, razors,
ear gun, tattooing, surgical instruments, unprotected sexual intercourse, etc…)
Incubation Period is 2 – 24 weeks
PHASES
1 Prodomal phase
Lethargic, Anorexia, Malaise, Nausea, Vomiting
2
Icteric Phase (10-15 days)
Jaundice
3
Convalescent Phase
Sign & symptom are start to resolve
Some Important Terminologies
1.
HBsAg
Surface Antigen (+ve means infection)
2.
Anti HBs
Antibody against HBsAg
3.
HBeAg
Envelop Antigen (showing active replication)
4.
HBc
Core Antigen
DIAGNOSTIC SCENARIOS
1
HBsAg
Anti HBs
Anti HBc
+ve
-ve
+ve Ig M
Case of Acute Hepatitis
2.
HBsAg
Anti HBs
Anti HBc
+ve
-ve
+ve Ig G
Case of Chronic Hepatitis with Active Replication
3.
HBsAg
-ve
4.
HBsAg
-ve
Anti HBs
Anti HBc
+ve
+ve Ig G
Patient is in Recovery Phase
5.
HBsAg
-ve
Anti HBs
-ve
Window period
Anti HBs
+ve
Vaccinated Person
HBeAg
+ve
HBeAg
+ve
Anti HBc
-ve
Anti HBc
+ve
8
TREATMENT
Acute Hepatitis “B”
Symptomatic treatment during Acute infection & Regular monitoring of Anti HBs
titer. (every two months)
OR
Start with interferon 2 alpha
Chronic Hepatitis “B” with Active replication
1. Start with interferon therapy 2 alpha
Dose: 6 million units for 5 days in a week subcutaneouly
OR
5 million units daily for 4 months
Side effects of interferon
Leukopenia
Thrombocytopenia
Hypersensitivity reaction (flu syndrome)
Increased Suicidal Tendency
Allopesia
Hypothyroidism
Contra indicated in Pregnancy & Elderly
2. Start with Lamivudine (Tab: Zefix 100 mg 1x OD)
3. Adefovir Dipivoxil (10 mg 1x OD)
COMPLICATIONS OF HEPATITIS “B”
1.
2.
3.
4.
Hepatic Complications
Extra Hepatic Complications
Chronic hepatitis
Liver Cirrhosis
Fulminant Hepatitis
Hepatocellular carcinoma
Glomerulonephritis
Cryoglobulinemia
Poly Arteritis Nodosa
Porphyria Cutanea Tarda
PREVENTION
Prevented by Vaccine
9
HEPATITIS “C”
It is belongs to FlaviVirus
It is RNA virus
Its size is 30 – 38 nm
Route of transfusion is Parenternal (Blood Transfusion, glass syringe, razors,
ear gun, tattooing, surgical instruments, etc…)
Incubation Period is 2 – 26 weeks
Acute phase is sub clinical so these patients usually present as chronic Hepatitis.
PHASES
1. Prodomal phase
Lethargic, Anorexia, Malaise, Nausea, Vomiting
2. Icteric Phase (10-15 days)
Jaundice
3. Convalescent Phase
Sign & symptom are start to resolve
INVESTIGATIONS
Anti HCV (if +ve it shows infectivity)
Then go for
HCV – RNA
Quantitative
Qualitative (this is more beneficial)
ELISA (this require at least 500 – 1000 RNA to be picked)
RIBA {(Radio Immuno Blot Assay) This picked even 50100 HCV virus RNA}
10
If HCV RNA +ve then go for Genotyping
There are 6 genotypes of HCV but 2,3 are common in Asia & 3 is common in Pakistan.
TREATMENT
Start INTERFERON (3 million units three times in a week for 6 months
S/c)
FOLLOW UP RESPONSE
After completion of six months of Interferon therapy then do HCV – RNA if it is –ve
then after another 6 months again do HCV – RNA.
STANDARD REGIMEN OF HEPATITIS “C”
INTERFERON + RIBAVERIN (400 mg) for 6 months.
TYPES OF INTERFERON
1.
CONSENSUS INTERFERON
9 mg three times a week for 6 months
2.
PEGILATED INTERFERON
It is slow release
It is long acting
Given once in a week (180 mg for 48 weeks)
It is more effective then others
HEPATITIS “D”
It is a defective RNA Virus
Its size is 35 nm
Route of transfusion is Parenternal (Blood Transfusion, glass syringe, razors,
ear gun, tattooing, surgical instruments, unprotected sexual intercourse, etc…)
Incubation Period is 6 – 9 weeks
11
It does not cause infection directly only infect on already infected by Hepatitis
B virus
It can cause “Co – infection” that Hepatitis B & D virus infest the Hepatocytes
Simultaneously
It increases the chances of Hepatocellular carcinoma.
It can diagnosed by Anti HDV test
There is no any management for hepatitis D but it can be prevented by
prevention of Hepatitis.
HEPATITIS “E”
It is belongs to CaliciVirus
It is RNA type of Virus
Its size is 27 nm
Route of transmission is Orofaecal
Incubation Period is 3 – 8 weeks
It is notorious for Fulminant Hepatitis
Females are more affected then males Specially during Pregnancy
Mortality is 20 %
Diagnosed by Anti HEV
MANAGEMENT
Bed Rest
Properly Hydrated
Give high ATP diet
10% of Dextrose water
Hepamerz.
12