movement_disorders_LECT16
advertisement
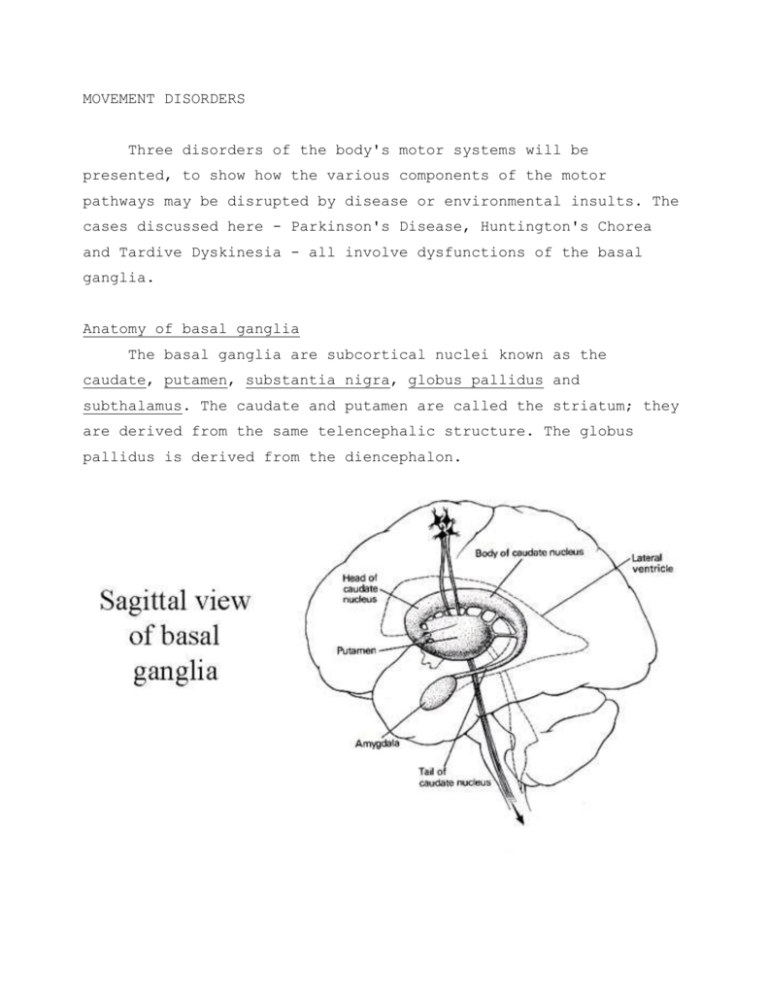
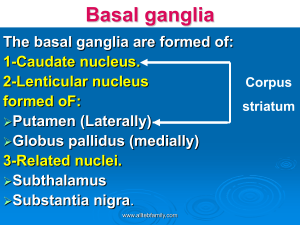
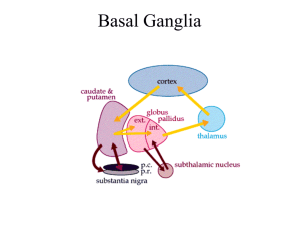
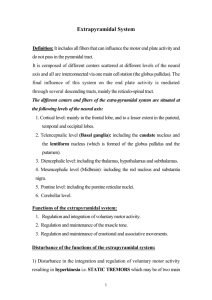
MOVEMENT DISORDERS Three disorders of the body's motor systems will be presented, to show how the various components of the motor pathways may be disrupted by disease or environmental insults. The cases discussed here - Parkinson's Disease, Huntington's Chorea and Tardive Dyskinesia - all involve dysfunctions of the basal ganglia. Anatomy of basal ganglia The basal ganglia are subcortical nuclei known as the caudate, putamen, substantia nigra, globus pallidus and subthalamus. The caudate and putamen are called the striatum; they are derived from the same telencephalic structure. The globus pallidus is derived from the diencephalon. The caudate nuclei are two large, ring-shaped structures extending from the putamen to the amygdala on each side of the brain. In transverse section (Figure 2), the caudate can be seen just below the lateral ventricle. Also visible are the putamen, globus pallidus and subthalamic nucleus. A schematic of the neural connections between the basal ganglia is shown in Figure 3. These ganglia are highly interconnected and play a significant role in the regulation of muscle tone and motor function. Parkinson's Disease Parkinson's disease, or paralysis agitans, affects approximately 500,000 patients in the US. Symptoms include a rhythmic tremor at rest, increased muscle tone or rigidity – sometimes of the cogwheel type, slowness of initiation of movement (akinesia) and slow execution of movement (bradykinesia), drooling, slowness of thinking, and depression. The classical three symptoms are tremor, rigidity and poverty of movement. The pathophysiology of Parkinson's includes (1) degeneration of the nigrostriatal pathway, which is dopaminergic. The CalneLangston theory suggests that ingestion of enviromental toxins accelerates the normal rate of killing of domaminergic neurons (see handout); (2) degeneration of raphe nuclei (see Figure 5): These are primarily serotonergic neurons that project widely to the nervous system, and apparently have a diffuse modulatory role in sleep and wakefulness; (3) degeneration of neurons in the locus ceruleus: The LC and the raphe nucleus are involved in anxiety production, through norepinephrine-containing neurons. Degeneration may cause depression; (4) degeneration of the motor nucleus of X; this sometimes causes drooling. Some chemical changes with parkinsonism include a reduction of dopamine, serotonin, and norepinephrine. Most of the catecholamine in the brain, including dopamine, is located in the basal ganglia. Parkinson patients have very low levels of these biogenic amines at autopsy. Treatment is with L-DOPA (dihydroxyphenylalanine), but it only controls some of the symptoms and not the course of the disease. Parkinsonism has also been successfully treated with transplantation of fetal nigral tissue into the striatum of patients. The masked facies of parkinsonism is shown in Figure 7. The facial muscles show an unusual immobility. The eyes have a staring appearance, and ocular movements or blinking are rare. Huntington's Chorea Chorea means involuntary, purposeless and irregular movements of the body affecting proximal or distal joints. It may include unpredictable grimacing, twitching or writhing of the limbs and head. It is a symptom of basal ganglia disease. Huntington's Chorea appears at an age of 30-40 years, and includes symptoms of chorea and dementia. It is autosomally dominant, and affected patients usually succumb due to respiratory difficulties within 15 years of onset. The pathophysiology of Huntington's Chorea includes degeneration of intrastriatal (caudate and putamen) GABAergic neurons. Chemical changes include a reduction of choline acetyltransferase, glutamic acid decarboxylase, and GABA (gamma aminobutyric acid). Tardive Dyskinesia The symptoms are involuntary movements, esp. of face & tongue. This condition is caused by long-term treatment with antipsychotic drugs - phenothiazines e.g.chlorpromazine and butyrophenones e.g. haloperidol (Haldol). The pathophysiology of tardive dyskinesia is that chronically administered antipsychotic drugs block dopaminergic cells, and then the cells become hypersensitive to dopamine. Antipsychotics exert calming effect by blocking dopaminergic cells in the cortex and elsewhere. Unfortunately, they also do the same thing in the basal ganglia, producing rhythmic movements as a side effect. Klawans (1973) proposed that dopamine antagonists used as antipsychotics cause upregulation of dopamine receptors in the striatum. When the antagonists are withdrawn, the hypersensitivity to dopamine causes excessive movement. About 20% of patients in who have been in long-term treatment develop TD. The new drug clozapine appears to have less of this effect.