SOP-PQAU001-007: Sterilization of Reusable Metal
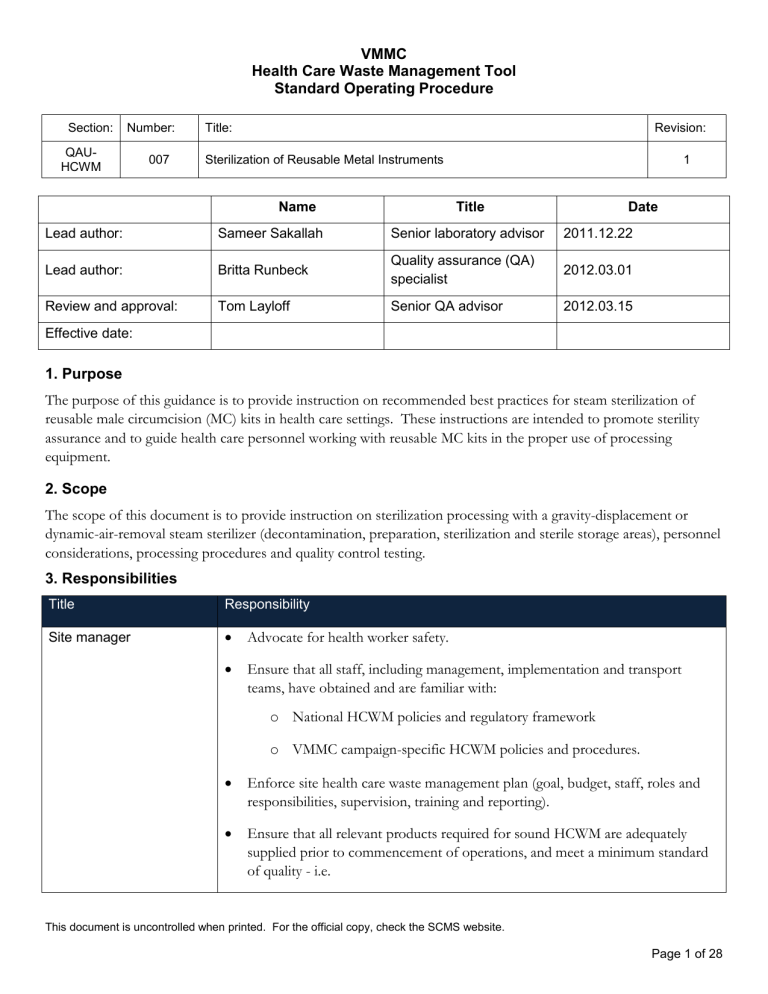
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Lead author:
Lead author:
Review and approval:
Effective date:
Title:
Sterilization of Reusable Metal Instruments
Name
Sameer Sakallah
Britta Runbeck
Tom Layloff
Title Date
Senior laboratory advisor 2011.12.22
Quality assurance (QA) specialist
2012.03.01
Senior QA advisor 2012.03.15
Revision:
1
1. Purpose
The purpose of this guidance is to provide instruction on recommended best practices for steam sterilization of reusable male circumcision (MC) kits in health care settings. These instructions are intended to promote sterility assurance and to guide health care personnel working with reusable MC kits in the proper use of processing equipment.
2. Scope
The scope of this document is to provide instruction on sterilization processing with a gravity-displacement or dynamic-air-removal steam sterilizer (decontamination, preparation, sterilization and sterile storage areas), personnel considerations, processing procedures and quality control testing.
3. Responsibilities
Title Responsibility
Site manager
Advocate for health worker safety.
Ensure that all staff, including management, implementation and transport teams, have obtained and are familiar with: o National HCWM policies and regulatory framework o VMMC campaign-specific HCWM policies and procedures.
Enforce site health care waste management plan (goal, budget, staff, roles and responsibilities, supervision, training and reporting).
Ensure that all relevant products required for sound HCWM are adequately supplied prior to commencement of operations, and meet a minimum standard of quality - i.e.
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 1 of 28
Section: Number:
QAU-
HCWM
007
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Title:
Sterilization of Reusable Metal Instruments
Infection control officer
Revision:
1 o Waste containers (color-coded bags, boxes, etc.) o Labeling tools and signage o Decontamination products and equipment o Temporary storage space o Visual aids o Control documents
Ensure that all levels of site staff, including the transport team, are adequately trained in all the proper HCWM procedures relevant to their scope of work prior to commencement of duty.
Identify waste container supply needs and report stockouts.
Ensure that a designated on-site route plan and collection schedule is designed and implemented for HCW.
Ensure that the waste is weighed correctly and control documents are correctly filled in and signed off upon collection for off-site transport.
Conduct quality audits and verify compliance with HCWM SOPs.
Ensure that all staff, including management, implementation and transport teams, have obtained and are familiar with: o National HCWM policies and regulatory framework o VMMC campaign-specific HCWM policies and procedures.
Enforce site health care waste management plan (goal, budget, staff, roles and responsibilities, supervision, training and reporting).
Ensure that all levels of site staff, including the transport team, are adequately trained in all HCWM procedures relevant to their scope of work prior to commencement of duty.
Train and ensure staff is properly following hand hygiene and surgical scrub
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 2 of 28
Section: Number:
QAU-
HCWM
007
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Title:
Sterilization of Reusable Metal Instruments
Revision:
1 procedures where applicable.
Advocate for health care worker safety.
Ensure that all relevant products required for sound HCWM are adequately supplied prior to commencement of operations, and meet a minimum standard of quality - i.e. o Waste containers (color-coded bags, boxes, etc.) o Labeling tools and signage o Decontamination products and equipment o Temporary storage space o Visual aids o Control documents
Ensure a clean and orderly environment at the site (supervisory).
Identify waste container supply needs and report stockouts.
Ensure that reporting systems (incident, injury-on-duty, needle stick injury, waste movement, etc.) are adopted and in place.
Ensure that all waste generated at source (point of origin) is correctly segregated and packaged, and that the packaging is safely closed off before collection for on-site transport (supervisory).
Ensure all aspects of sterile processing of reusable metal instruments and decontamination of disposable instruments) are competently performed by the
Orderlies, including: o Decontamination o Preparation o Packaging
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 3 of 28
Section: Number:
QAU-
HCWM
007
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Title:
Sterilization of Reusable Metal Instruments
Clinical staff
Revision:
1 o Sterilization o Sterile storage o Distribution of re-sterilized reusable metal instruments
Ensure decontaminated disposable metal instruments are securely stored
(supervisory).
Ensure that the waste is weighed correctly and control documents are correctly filled in and signed off upon collection for off-site transport.
Ensure that a designated on-site route plan and collection schedule is carefully designed and implemented for HCW.
Conduct quality audits and verify compliance with HCWM SOPs.
Follow health care waste management policies and procedures.
Practice safe operating procedures and wear appropriate PPE.
Follow general hand hygiene and surgical scrub procedures where applicable.
Ensure a clean and orderly environment at the site.
Apply Sharps Safety Best Practice.
Place sharps containers properly at designated locations.
Ensure that all waste generated at source (point of origin) is correctly segregated and packaged into appropriate color-coded containers, and that the packaging is safely closed off before collection for on-site transport.
Notify Orderly when waste container is ¾ full and is ready for collection and replacement.
Place contaminated metal instruments into presoak bath after use.
Notify Orderly if instrument presoak bath needs replacing.
Notify Orderly if there is a spill that requires cleaning and supervise and assist
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 4 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
Orderly
Transport team manager accordingly.
Know the health care waste management policies and procedures.
Practice safe operating procedures and wear appropriate PPE.
Follow general hand hygiene procedures.
Ensure a clean and orderly environment at the site.
Place sharps containers at designated locations.
Properly prepare sodium hypochlorite solutions as needed.
Collect sharps containers and other waste containers once they have reached their maximum capacity (no more than ¾ full) and take them to the temporary storage site.
Competently perform all aspects of sterile processing of reusable or disposable metal instruments, including: o Decontamination o Preparation o Packaging o Sterilization o Sterile storage o Distribution of re-sterilized reusable metal instruments
Store infectious and sharps waste in a secure location.
Ensure decontaminated disposable metal instruments are securely stored.
Properly clean up spills where needed.
Obtain and enforce relevant HCWM management policies and procedures and
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 5 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
Transport Team wearing of appropriate personal protective equipment (PPE).
Advocate for health worker safety.
Ensure that all levels of staff are adequately trained in all the proper HCWM procedures relevant to prior to commencement of duty.
Ensure supply of appropriate scale(s) dedicated solely to the purpose of weighing waste, as well as a budget for periodic calibration by an accredited third party to ensure that it is consistently accurate in operation.
Ensure staff is adequately trained on how to use and calibrate scale(s) for the purpose of weighing HCRW.
Ensure an adequate supply of required tools and first aid kits and spill containment kits to be kept on board the vehicle(s).
Conduct quality audits and verify compliance with relevant HCWM SOPs.
Obtain and apply relevant HCWM management policies and procedures and wear appropriate personal protective equipment (PPE).
Follow general hand hygiene where applicable.
Ensure that a designated route plan and collection schedule is carefully designed and implemented.
Ensure that all tools and first aid kits and spill containment kits on board vehicles are well-stocked.
4. Definitions
Term
Absorbent surgical towel
Asepsis
Bacterial count
Definition
Typically, a low-lint 100% cotton surgical towel women with a plain weave
Prevention of contact with microorganisms
Method of estimating the number of bacteria per unit sample, usually expressed as
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 6 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
Bioburden
Biological indicators (BIs)
Biological indicator control, positive
Bowie-Dick test
Challenge test pack
Chemical indicators (CIs)
Cleaning
Container system, rigid sterilization
Containment device
Contaminated
Decontamination
Decontamination area
Dynamic-air-removal steam sterilization
Gravity-displacement number of colony-forming units
Population of viable microorganisms on a product and/or a sterile barrier system
Test systems containing viable microorganisms providing a defined resistance to a specified sterilization process
Biological indicator, from the same lot as a test biological indicator, which is left unexposed to the sterilization cycle and then incubated to verify the viability of the test BI
Diagnostic test of a dynamic-air-removal steam sterilizer’s ability to remove air from the chamber and prevent air re-entrainment
Pack used in qualification, installation and routine quality assurance testing of hospital sterilizers
Devices used to monitor the presence or attainment of one or more of the parameters required for a satisfactory sterilization process, or specific tests of sterilization equipment
Removal of contamination from an item to the extent necessary for further processing or for the intended use
Sterilization containment device designed to hold medical devices for sterilization, storage, transportation and aseptic presentation of contents
Reusable rigid sterilization container, instrument case or organizing tray intended for use in health care facilities for containing reusable medical devices for sterilization
State of having been actually or potentially in contact with infectious agents
The process by which medical devices, instruments and equipment are rendered safe for personnel to handle
Area of a health care facility designated for collecting, retaining and cleaning soiled and/or contaminated items
One of two types of sterilization cycles in which air is removed from the chamber and the load by means of a series of pressure and vacuum excursions (prevacuum cycle) or by means of a series of steam flushes and pressure pulses above atmospheric pressure
Type of sterilization cycle in which incoming steam displaces residual air through a
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 7 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title: Revision:
QAU-
HCWM
007 steam sterilization
Sterilization of Reusable Metal Instruments 1
Hypochlorite solutions
Incubator
Infectious microorganisms
Installation qualification port or drain in or near the bottom of the sterilizer chamber
Widely used for decontaminating surgical instruments, laboratory equipment and spot disinfection of countertops and floors in health care facilities
Apparatus for maintaining a constant and suitable temperature for the growth and cultivation of microorganisms
Microorganisms capable of producing disease in the appropriate hosts
Process of obtaining and documenting evidence that equipment has been provided and installed in accordance with specifications
Microorganism
Operational qualification
Shelf life
Steam sterilization
Entity of microscopic size, encompassing bacteria, fungi, protozoa and viruses
Process of obtaining and documenting evidence that installed equipment operates within predetermined limits when used in accordance with its operational procedures
Performance qualification
Process of obtaining and documenting evidence that the equipment is installed and operated in accordance with operational procedures, consistently performs in accordance with predetermined criteria and thereby yields product meeting its specification
Personnel protective equipment (PPE)
Process challenge device
(PCD)
Processing area
Specialized clothing or equipment worn by an employee for protection against a hazard
Item designed to constitute a defined resistance to a sterilization process and used to assess performance of the process
Area of a health care facility in which decontaminated, clean instruments, and other medical and surgical supplies are inspected, assembled into sets and trays, and wrapped, packaged or placed into rigid sterilization container systems for subsequent sterilization
When the term is used with respect to a sterilized medical device, the period of time during which the item is considered safe for use
Sterilization process that uses saturated steam under pressure, for a specified exposure time and at a specified temperature, as the sterilizing agent
Sterile storage area Area of a health care facility designed to store clean and sterile items and protect them from contamination
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 8 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title: Revision:
QAU-
HCWM
Sterilization
007 Sterilization of Reusable Metal Instruments 1
Validated process used to render a product free from viable microorganisms
5. References
1.
American National Standards Institute/ Association for the Advancement of Medical Instrumentation
ST79: 2010 & A1:2010 & A2:2011, Comprehensive guide to steam sterilization and sterility assurance in health care facilities
2.
SOP-QAU00-006, Decontamination of Non-sharp Metal Instruments
3.
SOP-PQAU001-005, Decontamination of General Surfaces
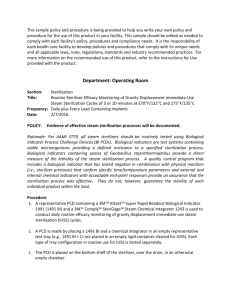
6. Procedures
6.1. Care and handling of contaminated reusable items
6.1.1 Personal protective equipment
When handling contaminated items, personnel should wear appropriate PPE, including gloves, rubber boots, aprons, long pants and long sleeves, and either a face shield or goggles and a procedure mask to protect the eyes, nose and mouth from accidental splashes.
6.1.2 Contaminated reusable items
Contaminated items should be contained during their transport from the point of use to the decontamination area. Containers, devices or carts must be marked with a biohazard label or other means of identifying contaminated contents. Red bags, bins with lids, enclosed or covered carts, rigid sterilization container systems, and impermeable bags are among the types of containers that may be used alone or in combination to transport contaminated items.
For guidance on safe handling and transport of contaminated reusable items, see Guidance on Proper
Decontamination, Storage, Transport and Disposal of Disposable Non-Sharp Metal Instruments.
6.2. Cleaning, decontamination and inspection
6.2.1 Cleaning and decontamination
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 9 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
Cleaning and decontamination should begin as soon as possible after the reusable medical instruments have been used. The first and most important step in the decontamination process is thorough cleaning and rinsing. Cleaning primarily removes rather than kills microorganisms. Because the cleaning process is not microbicidal, a subsequent disinfection or sterilization process might be necessary to ensure an item is safe for handling. After cleaning, instruments should be thoroughly rinsed to ensure loosened debris and detergents are adequately removed.
For specific information on the cleaning and decontamination processes, see SOP 006, Decontamination of
Non-sharp Metal Instruments. For guidance on creating a diluted sodium hypochlorite solution for cleaning and disinfecting medical instruments, see also SOP 005. Refer to Annexes 3 and 4 for visual aids.
Note: Cleaning and decontamination procedures should also be applied to the rigid sterilization container holding the medical instruments.
6.2.2 Inspection
Instruments should be carefully inspected for cleanliness and flaws or damage and dried before packaging.
If instruments reveal rust or damage, they should be disposed of appropriately and replaced with new instruments.
The rigid sterilization container should be inspected for any sharp edges or nicks that will puncture or tear the wrapper(s). The latching mechanism or closure on the rigid sterilization container should be checked to ensure it will remain secure.
6.3. Sorting and assembly, packaging and labeling of surgical instruments
6.3.1 Sorting and assembly of surgical instruments
The MC re-usable kit is made of the components listed in Tables 1A and 1B below. These components should be carefully identified and sorted using the table below as a guide.
Table 1A. MC reusable kit for forceps guided procedure
Product Qty
1
2
3
4
Autoclave storage box
Needle holder/driver
Suture scissor
Toothed tissue forceps
1
1
1
1
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 10 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
5
Title:
Sterilization of Reusable Metal Instruments
Mosquito clamp straight 4
6
7
Mosquito clamp curve
Forceps hemostatic cross clamp
1
1
Table 1B. MC reusable kit for sleeve or dorsal slit procedure
Product Qty
1
2
Autoclave storage box
Dissection dissecting scissors
1
1
3
4
5
6
7
Needle holder/driver
Suture scissor
Toothed tissue forceps
Mosquito clamp straight
Mosquito clamp curve
1
1
1
4
1
Revision:
1
8 Hemostatics clamps 2
Using the quantities indicated in Table 1 above, individual components of each MC kit must be placed securely into the sterilization box. The order of these instruments inside the box is not important, but the exact type and number of each instrument are very important.
6.3.2 Packaging
The primary functions of a package containing medical instruments are to allow the sterilization of the contents, to maintain the sterility of the contents until the package is opened, and to provide for the removal of the contents without contamination. To maintain sterility of a reprocessed male circumcision kit, the metal organizing tray must be wrapped with a woven fabric (reusable) or non-woven material (single-use disposable). These materials are described below.
Woven fabrics – usually 100% cotton, cotton-polyester blends, and synthetic blends
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 11 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
Nonwoven materials – made of plastic polymers, cellulose fibers or washed paper pulp bonded under pressure sheets, not woven on a loom. These are usually designed for single use.
6.3.2.1 Instrument placement
Before wrapping, all reusable components should be placed in the metal organizing tray and jointed instruments should be in the open or unlocked position.
6.3.2.2 Packaging properties
In general, an effective packaging material for steam sterilization should, at a minimum:
1.
Allow adequate air removal from and steam penetration of the package contents
2.
Provide an adequate barrier to microorganisms or their vehicles
3.
Resist tearing or puncture
4.
Allow a method of sealing that results in a complete seal that is tamper-evident and provides seal integrity
5.
Allow for ease of aseptic presentation
6.
Be free of toxic ingredients and non-fast dyes
7.
Be non-linting
8.
Be shown by value analysis to be cost-effective
6.3.2.3 Wrapping/folding
Packaging materials should be stored at room temperature (20°C to 23°C) and away from excessive humidity (30%–60%) at least two hours before use. This is to allow adequate steam penetration and to avoid superheating of the package contents.
All packaging materials should be examined regularly for holes, defects and extraneous matter.
Wrap the instrument box using one of the techniques provided in Annex 1 or Annex 2.
Wrappers should be snug to prevent low spots that could collect condensation on the exterior of the package. However, care should be taken not to wrap too tightly. Closures that restrict the expansion and contraction of the package during the sterilization process could interfere with air removal, steam penetration and steam removal.
If “wet packs” are observed, they should not be used. Instead, they should be reprocessed in a manner that ensures that excess moisture/condensation does not occur. They should be repackaged (including the outer wrapper and label).
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 12 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title: Revision:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments 1
Sterilization indicator tape should be used to secure wrapped packages. Other kinds of tape should not be used, nor should safety pins, paper clips, staples or other sharp objects.
Tip protectors are not recommended for use with the reusable MC kits.
The latching mechanism on rigid sterilization container systems should secure the lid so that it cannot move when locked.
6.3.3 Labeling of sterilized package
The user must be able to identify the contents of a package before it is opened; therefore, it is imperative that the package is labeled completely and correctly. Package labels should be capable of remaining securely affixed to packages throughout the course of their handling from sterilization to use. Sterilization indicator tape may be used for this purpose. If a marking pen is used to label wrapped packs, the ink should be nontoxic, and the labeling information should be written on the indicator tape. For paper-plastic pouches, the labeling information should be written only on the plastic side of the pouch.
The package label should include:
A description of the package contents
The expiration date or a shelf-life statement
The initials of the person assembling the package
The department where the package is to be sent after sterilization
Identification of the sterilizer and cycle number
The date of sterilization (load sticker)
6.4. Sterilization parameters for wrapped items
Steam entering packages containing metal instruments immediately condenses as its latent heat is transferred to the metal items. Over the course of the exposure period, all of the condensation might not return to a vapor and can remain trapped in the package in the form of water droplets. Condensation elimination is possible only with a sterilizer designed with heated drying capabilities. Inadequate drying could compromise the seal, the integrity or the barrier protection ability of the package, and, therefore, sterility might not be maintained. Care should be taken to ensure that all devices in a load have the same exposure time.
Sterilizers vary in design and performance, so cycle parameters should always be verified against the sterilizer manufacturer’s written procedures for the specific sterilizer and load configuration being used. In general, however, steam sterilization cycles typically used in health care facilities include the gravity-displacement cycle and two types of dynamic-air-removal cycles:
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 13 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title: Revision:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments 1
1.
The pre-vacuum cycle removes air from the chamber and load by pressure and vacuum excursions.
2.
The steam-flush pressure-pulse cycle removes air with a series of steam flushes and pressure pulses above atmospheric pressure.
Table 2 summarizes the most common temperature and time parameters for various types of loads.
Table 2. Minimum cycle times (in minutes) for steam sterilization cycles (wrapped instruments)*
Gravity-displacement steam sterilization cycles
Exposure time at
121 o C
Exposure time at
132 o C
Exposure time at
135 o C
30 15
10
Dynamic-air-removal steam sterilization cycles
Drying time
15-30
30
NA 4 20-30
3 16
*Consult the manufacturer’s recommendations for each specific sterilizer.
However, it must be emphasized that:
The sterilizer manufacturer’s operator manual should be consulted for specific exposure times, temperatures and drying times. The use of rigid sterilization container systems (like the reusable MC box) could affect exposure times in steam sterilizers, depending on the efficiency of air removal from and steam penetration into the container systems. It is important, then, to verify that containerized devices can be effectively sterilized by the cycle parameters selected.
Programmed cycle selections should be used.
Any differences between the programmed cycle parameters and the cycle parameters recommended by the medical device manufacturer should be investigated and resolved before the items are sterilized.
Procedures for correct cycle selection should be developed and implemented.
Processes should be audited to ensure compliance.
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 14 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments
6.5. Storage of sterilized instruments
Revision:
1
6.5.1 Sterile storage
Written procedures should stress minimizing the handling of all sterile items. Any items with torn packaging or with packaging that appears to be wet should not be used. If an item is dropped on the floor and the integrity of the package is compromised, it should be returned to the decontamination area for reprocessing. Additional considerations for the storage of sterile items include the following:
Sterility maintenance covers (dust covers) may be used to protect and extend the shelf life of properly packaged and sterilized items that could be subjected to environmental challenges of multiple handling before use.
A sterility maintenance cover should be clearly designated as such to prevent its being mistaken for a sterile wrap. Sterility maintenance covers are designed to provide protection against outside elements (e.g., dust), not to provide a microbiological barrier.
Only products specifically labeled as sterility maintenance covers should be used for this purpose.
Covers should be applied immediately after the sterilized products have cooled down and are completely dry.
Covers should be sealed using a heat sealer designed to seal plastic to plastic (or an alternative method that is similarly effective). Also, a self-sealing cover may be used.
The lot or load control number and expiration date should be visible through the sterility maintenance cover, or an additional label should be used on the sterility maintenance cover.
6.5.2 Storage facilities
Sterile items should be stored in a way that reduces the potential for contamination, and traffic should be controlled to limit access to sterile items to those individuals who know how to handle them properly.
Additional considerations for storage facilities of sterile items include the following:
The temperature in storage areas should be approximately 24°C and the relative humidity should not exceed
70%.
Sterile items should be stored at least 20 to 25 centimeters above the floor, at least 45 centimeters below the ceiling, and at least 5 centimeters from outside walls.
The items should be positioned so that packaging is not crushed, bent, compressed or punctured and so that their sterility is not otherwise compromised.
Sterilized items should not be stored next to or under sinks, under exposed water or sewer pipes, or in any location where they could become wet.
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 15 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
They should not be stored on floors, on windowsills or in areas other than designated shelving, counters or carts.
6.5.3 Shelf life
The shelf life of a packaged sterile item is event-related and depends on the quality of the packaging material, storage conditions, transport conditions and amount of handling. In general, stock should be rotated according to the principle “first in, first out.”
Note: SCMS recommends the shelf life of the reusable MC kit not exceed 90 days from the sterilization date.
6.6. Quality control measures
Sterilization process monitoring is an essential part of sterility assurance. Process monitoring consists of:
Monitoring of every package and sterilization load
Routine monitoring of sterilizer efficacy
Qualification testing of the sterilizer after installation, relocation, sterilizer malfunction, major repairs and sterilization process failures
Periodic product quality assurance testing
6.6.1 Monitoring of every package and sterilization load
6.6.1.1 Physical monitors
Physical monitors verify that the parameters of the sterilization cycle have been met. Physical monitors include time, temperature and pressure recorders; displays; digital printouts; and gauges. At the end of the cycle and before items are removed from the sterilizer, the operator should examine and interpret the chart or printout to verify that all cycle parameters were met and initial it to permit later identification of the operator.
6.6.1.2 Chemical indicators
Chemical indicators are designed to respond with a chemical or physical change to one or more of the physical conditions within the sterilizing chamber. CIs assist in detecting potential sterilization failures that could result from incorrect packaging, incorrect loading of the sterilizer, or sterilizer malfunctions. CIs do not verify sterility, but some types may allow detection of equipment malfunctions (e.g., air leaks, wet steam, inadequate temperature or time), and they may assist in identifying certain procedural errors. A CI is a monitoring tool to be used in conjunction with physical monitors and biological indicators to demonstrate the efficacy of the sterilization process.
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 16 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
The six classes of CIs and their specific performance requirements include:
Class 1 – Process indicators are intended for use with individual units (e.g., packs, containers) to indicate that the unit has been exposed to the sterilization process and to distinguish between processed and unprocessed units. These indicators are also referred to as external CIs.
Class 2 – Indicators for use in specific tests are intended for use in specific test procedures. For example, the Bowie-Dick test is used to verify the complete removal of air from a dynamic-air-removal (or pre-vac) steam sterilization cycle. Note: this indicator is not to be used on a gravity-displacement steam sterilizer.
Class 3 – Single-variable indicators are designed to react to one of the critical variables (time, temperature or steam penetration) and intended to indicate exposure to a sterilization process at a stated value of the chosen variable.
Class 4 – Multi-variable indicators are designed to react to two or more of the critical variables (time, temperature or steam penetration) and intended to indicate exposure to a sterilization process at stated values of the chosen variables.
Class 5 – Integrating indicators are designed to react to all critical variables (time, temperature and steam penetration), with the stated values having been generated to be equivalent to, or exceed, the performance requirements for biological indicators.
Class 6 – Emulating indicators are chemical indicators designed to react to all critical variables (time, temperature and steam penetration) of specified sterilization cycles, with the stated values having been generated from the critical variables of a specific sterilization process (i.e., dynamic-air-removal cycle at
132 o C for 4 minutes.)
6.6.1.2.1 Using external chemical indicators
To distinguish between processed and unprocessed items, a process indicator (Class 1 CI), in the form of sterilizer indicator tape or an indicating label, should be affixed or printed on each wrapped rigid sterilization container. The purpose of the external CI is to differentiate between processed and unprocessed items, not to establish whether the parameters for adequate sterilization were met.
6.6.1.2.2 Using internal chemical indicators
An internal CI should be placed within each wrapped rigid sterilization container to be sterilized.
This internal CI may be a Class 3, 4, 5 or 6 indicator. The class of CI chosen depends on how many critical process variables are to be monitored and how much information is desired about the sterilization process. The CI should be placed in the area of the rigid sterilization container considered least accessible to steam penetration.
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 17 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
The CI is retrieved at the time of use and is interpreted by the user. The user should be trained in and knowledgeable about the CI’s performance characteristics. If interpretation of the CI suggests inadequate steam processing, the package contents should not be used. The interpreter at time of use should inform the appropriate supervisor of inadequate steam processing and return the complete unused package, including load identification and the CI, to the sterilizing department.
If a CI is nonresponsive or inconclusive, it is possible that the entire load is not sterile (i.e., the sterilization process failed). It is also possible that errors in loading or packaging have resulted in sterilization failures in some, but not all, packages in the load. Therefore, a single nonresponsive or inconclusive CI should not be considered definitive evidence that the entire load is nonsterile. The sterilization department head must use professional judgment in deciding whether or not to recall the entire sterilized load. This decision should be based on the results of physical monitoring (time and temperature recordings), the results of internal CIs elsewhere in the load, and if applicable, the results of the BI. If these results are not yet available, the remaining packages from the same load should be quarantined until the results of the BI are known.
6.6.2 Routine monitoring of sterilizer efficacy
6.6.2.1 Biological indicators
Biological indicators consist of spores in or on a carrier, sometimes accompanied by incubation media. BIs provide the only direct measure of lethality of the sterilization process. They must be incubated for various periods of time (depending on the specific product) until it is determined whether the microorganisms grow
(i.e., they survived the sterilization process) or fail to grow (i.e., they were killed by the sterilization process).
Health care personnel should select BIs that consist of spores of Geobacillus stearothermophilus (formerly named Bacillus stearothermophilus). Data should be obtained from the manufacturers on the reliability, safety and performance characteristics of their products. BI manufacturers are required to provide written instructions on the storage, handling, use and microbiological testing of their products.
6.6.2.1.1 Using biological indicators
Biological indicators should be used within process challenge devices for routine sterilizer efficacy monitoring at least weekly, but preferably every day that the sterilizer is in use. BIs within PCDs should also be used for sterilizer qualification testing after sterilizer installation, relocation, malfunctions and major repairs or after sterilization process failures.
BI use provides evidence of efficacy by challenging the sterilizer with a large number of highly resistant bacterial spores. Biological monitoring provides the only direct measure of lethality of a sterilization cycle. Although the performance of Class 5 integrating CIs has been correlated to the performance of BIs, these sterilization monitoring devices do not contain spores and thus do not directly measure the lethality of a sterilization cycle.
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 18 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
6.6.2.1.2 Process challenge devices
A PCD is a device used to assess the effective performance of a sterilization process by providing a challenge to the process that is equal to or greater than the challenge posed by the most difficult item routinely processed. The PCD may contain: a.
A BI b.
A BI and a Class 5 integrating CI c.
A Class 5 integrating CI d.
A Class 6 emulating indicator
A PCD may be a user-assembled challenge test pack or test tray or a commercially available, disposable, pre-assembled challenge test pack. For commercial PCDs, it is important for health care personnel to obtain adequate information on their performance and intended use to ensure that they are suitable for the intended application and used correctly. PCD manufacturers should therefore provide written instructions for the use, storage, handling and testing of their products.
A user-assembled BI-challenge test pack should consist of 16 clean, preconditioned, reusable huck or absorbent surgical towels, in good condition, each of which is approximately 16 inches by 26 inches. (Preconditioning consists of holding the towels at room temperature 18°C–24°C [65°F to
75°F] and a relative humidity of at least 35% for at least two hours.) Each towel is folded into thirds and then folded widthwise in the middle. After they are folded, the towels are placed one on top of another, with folds opposite each other, to form a stack that is approximately 9 inches wide, 9 inches long, and 6 inches high (23 cm by 23 cm by 15 cm). One or more BIs are placed between the eighth and ninth towels in the approximate geometric center of the pack. The pack is then taped in a way that will yield the approximately 6 inches (15 cm) height. The pack should weigh approximately 3 lbs and should have a density of approximately 11.3 lbs per cubic foot. A wrapper should not be used for this PCD.
Note: The less frequently a sterilizer is used, the greater the chance that an unnoticed event could affect sterilization. Therefore, the sterilizer and the sterilization process should be regularly challenged with a PCD.
6.6.2.1.3 Placement of the PCD (BI challenge test pack)
Sterilizer efficacy is routinely monitored in a fully loaded chamber. The PCD (BI challenge test pack) should be placed flat (layers of towels horizontal if the 16-towel PCD is being used) in the area of the sterilizer chamber that is least favorable to sterilization (i.e., the area representing the greatest challenge to the BI). The sterilizer manufacturer should identify the exact location of this area, the
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 19 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number:
QAU-
HCWM
007
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
“cold point,” in the instruction manual. This area varies with sterilizer design but is normally in the front, bottom section of the sterilizer, near the drain.
6.6.2.1.4 Test procedure a) Before exposure to the sterilization cycle, label the PCD with the appropriate sterilizer lot and load information. b) Position the PCD in the sterilizer according to the sterilizer manufacturer’s instructions. c) Run a normal cycle according to the sterilizer and medical instrument requirements. d) Upon completion of the sterilization cycle and adequate cooling of the PCD, remove the BI(s) and record their identity. Ensure all BIs are accounted for. Incubate the BIs according to the manufacturer’s written instructions. e) Each day a test BI is run, incubate at least one BI from the same lot that has not been exposed to the sterilant as a control in each incubator to verify the presterilization viability of the test spores, the ability of the media to promote spore growth, and the proper incubation temperature. Upon completion of the incubation period, read and record the test and control results. If the control BI from a lot fails to grow, assume that the test BIs from that lot are nonviable or that improper incubation occurred. Therefore, the results from the test BIs should be considered invalid and the test repeated.
6.6.3 Acceptance criteria
An acceptable process is evidenced by negative results from all BIs in the PCD and appropriate readings from physical monitors and CIs, showing that the sterilization cycle was correct and complete. All monitoring results, including results from BI controls, should be interpreted by a qualified individual and included in the sterilizer records.
6.6.4 Sterilizer records
For each sterilization cycle, the following information should be recorded and maintained: a) Lot number b) Specific contents of the lot or load, including quantity, department and a specific description of the items
(e.g., towel packs, type/name of instrument sets) c) Exposure time and temperature d) Operator’s name or initials e) Results of the biological testing, if applicable f) Results of Bowie-Dick testing, if applicable
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 20 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title: Revision:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments 1 g) Response of the CI placed in the PCD (BI challenge test pack, BI challenge test tray, or CI challenge test pack), if applicable h) Any reports of inconclusive or nonresponsive CIs found later in the load
7. Distribution
1.
Knowledge tree
2.
Unit Intranet webpages
8. Documents
Annex 1. Sequential double-wrapping: square fold
Annex 2. Simultaneous double-wrapping: square fold
Annex 3. Sodium hypochlorite concentration table
Annex 4. Decontamination process for reusable voluntary medical MC kits, visual aids
Annex 5. Sterilization process for reusable voluntary medical MC kits, visual aids
Annex 6. Training evaluation checklist
9. Amendment history
Original lead author:
Name Title Date
Original section approval:
Original performance management approval:
Original management approval:
YYYY.MM.DD
Original effective date: YYYY.MM.DD Review period: Annual/quarterly
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 21 of 28
2
3
4
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments
10. Additional reviewers
Revision Name Title Date
1 Britta Runbeck 2012.02.29 Quality assurance specialist
Revision:
1
Comments
Revision and inclusion of quality control testing
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 22 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments
Annex 1. Sequential double-wrapping: square fold
Revision:
1
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 23 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments
Annex 2. Simultaneous double-wrapping: square fold
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Revision:
1
Page 24 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments
Annex 3. Sodium hypochlorite concentration table
Sodium hypochlorite concentration (3–5%)
Total volume of bucket/container
Liters
8
9
6
7
10
1
4
5
2
3
Amount of water
Liters
5.46
6.37
7.28
8.19
9.1
0.91
1.82
2.73
3.64
4.55
Amount of water
Milliliters
910
1,820
2,730
3,640
4,550
5,460
6,370
7,280
8,190
9,100
Amount of sodium hypochlorite
Liters
0.54
0.63
0.72
0.81
0.9
0.09
0.18
0.27
0.36
0.45
Amount of sodium hypochlorite
Milliliters
540
630
720
810
900
90
180
270
360
450
Total volume of bucket/container
Liters
8
9
6
7
10
1
4
5
2
3
Amount of water
Liters
5.76
6.72
7.68
8.64
9.6
0.96
1.92
2.88
3.84
4.8
Sodium hypochlorite concentration (6–10%)
Amount of water
Milliliters
960
1,920
2,880
3,840
4,800
5,760
6,720
7,680
8,640
9,600
Amount of sodium hypochlorite
Liters
0.04
0.08
0.12
0.16
0.2
0.24
0.28
0.32
0.36
0.4
Amount of sodium hypochlorite
Milliliters
240
280
320
360
400
40
80
120
160
200
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Revision:
1
Page 25 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title: Revision:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments
Annex 4. Decontamination process for reusable voluntary medical MC kits, visual aids
1
Annex 5. Sterilization process for reusable voluntary medical MC kits, visual aids
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 26 of 28
Section: Number:
QAU-
HCWM
007
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Title:
Sterilization of Reusable Metal Instruments
Revision:
1
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 27 of 28
VMMC
Health Care Waste Management Tool
Standard Operating Procedure
Section: Number: Title: Revision:
QAU-
HCWM
007 Sterilization of Reusable Metal Instruments 1
Annex 6. Training evaluation checklist
To ensure complete understanding, please answer the following questions on this SOP and work instruction, if applicable.
1. Does the reusable surgical male circumcision kit need to be wrapped before sterilization?
2. If the reusable surgical male circumcision kit is wet after completion of the sterilization cycle, is it acceptable for use or sterile storage?
3. What class of chemical indicator is placed on the outside of every unit to be sterilized?
4. What class (es) of chemical indicator are to be placed on the inside of every unit to be sterilized?
5. How often should a process challenge device be run in a sterilizer to test for routine sterilizer efficacy?
I confirm that I have read and understand this procedure: _______________________________
NAME SIGNATURE DATE
EMPLOYEE: _____________________ ______________________ _________________
ICO/TRAINER: _____________________ ______________________ __________________
This document is uncontrolled when printed. For the official copy, check the SCMS website.
Page 28 of 28