Deprivation of Liberty Safeguards Policy
advertisement
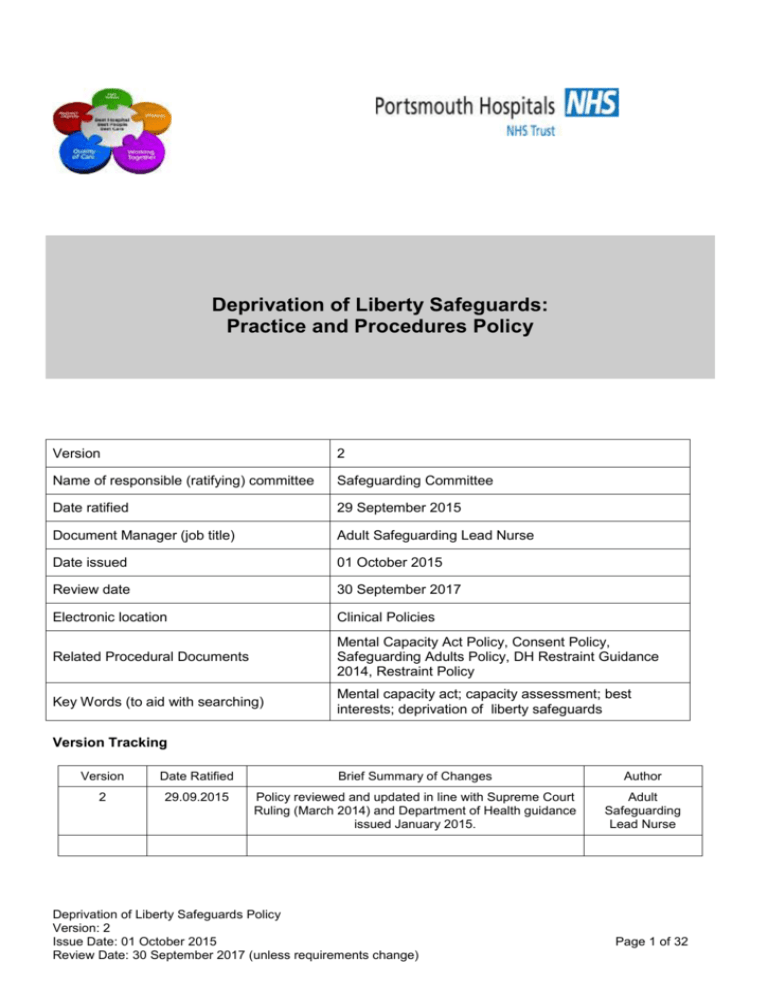
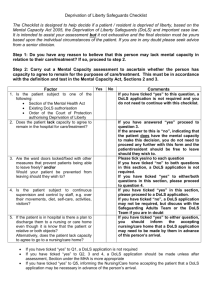
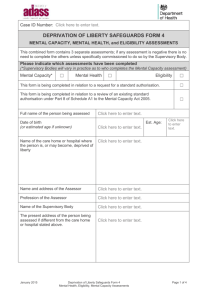
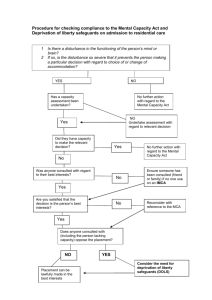
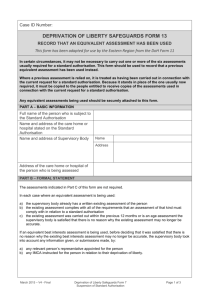
Deprivation of Liberty Safeguards: Practice and Procedures Policy Version 2 Name of responsible (ratifying) committee Safeguarding Committee Date ratified 29 September 2015 Document Manager (job title) Adult Safeguarding Lead Nurse Date issued 01 October 2015 Review date 30 September 2017 Electronic location Clinical Policies Related Procedural Documents Mental Capacity Act Policy, Consent Policy, Safeguarding Adults Policy, DH Restraint Guidance 2014, Restraint Policy Key Words (to aid with searching) Mental capacity act; capacity assessment; best interests; deprivation of liberty safeguards Version Tracking Version Date Ratified Brief Summary of Changes Author 2 29.09.2015 Policy reviewed and updated in line with Supreme Court Ruling (March 2014) and Department of Health guidance issued January 2015. Adult Safeguarding Lead Nurse Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 1 of 32 CONTENTS QUICK REFERENCE GUIDE…………………………………………………………………………………..3 1. INTRODUCTION…………………………………………………………………………………………5 2. PURPOSE…………………………………………………………………………………………………..5 3. SCOPE………………………………………………………………………………………………………6 4. DEFINITIONS………………………………………………………………………………………………6 5. DUTIES AND RESPONSIBILITIES………………………………………………………………………7 6. PROCESS 6.1. DETERMINE IF A DOLS IS REQUIRED……………………………………………………………7 6.2. APPLYING FOR A DOLS AUTHORISATION……………………………………………………….8 6.3. COMPLETING THE DOLS APPLICATION FORMS………………………………………………10 6.31. WHO COMPLETS THE FORMS……………………………………………………….…..10 6.32. WHERE TO SEND THE FORMS…………………………………………………….…….10 6.4. WHO TO NOTIFY……………………………………………………………………………………..12 6.5. WHAT HAPPENS NEXT…………………………………………………………………………….12 6.51. DOLS IS GRANTED…………………………………………………………………………....13 6.52. DOLS IS REFUSED……………………………………………………………………………13 6.6. A PATIENT DIES WHILST SUBJECT TO A DOLS AUTHORISATION………………….……14 6.7. UNAUTHORISED DEPRIVATIONS OF LIBERTY………………………………………………...14 7. TRAINING REQUIREMENTS…………………………………………………………..……………….15 8. REFERENCES AND ASSOCIATED DOCUMENTATION…………………………………….……15 9. EQUALITY IMPACT STATEMENT……………………………………………………………….……15 10. MONITORING COMPLIANCE WITH, AND EFFECTIVENESS OF, PROCEDURAL DOCUMENTS……………………………………………………………………………………………17 APPENDIX 1: DOLS FORM 1 – STANDARD AND URGENT DOLS REQUEST………………….18 APPENDIX 2: DOLS FORM 2 - FURTHER REQUEST FOR A FURTHER STANDARD AUTHORISATION…………………………………………………………………………………………25 APPENDIX 3: GUIDANCE FOR COMPLETING DOLS APPLICATION FORMS …………………27 Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 2 of 32 Patient lacks mental capacity to consent to hospital accommodation and meets the Acid Test and admission is likely to last more than a matter of days or there are high risk DOLS triggers QUICK REFERENCE GUIDE (1) Application Process for DOLS Authorisation (from 05/10/2015) The Standard DOLS Authorisation Expires and a DOLS is still required Complete DOLS Form 2 Trust DOLS signatories (team with clinical responsibility for the patient): ST3 and above Out of hours: Duty Matron Hospital@Night An Urgent DOLS Authorisation comes into force as soon as the DOLS application is completed and signed. Email copy of form to: Complete DOLS Form 1 pages 1-6 Explanation to patient and relatives PHT DOLS Group mailbox Retain original form in medical notes Ensure patient is given a copy of all DOLS documentation prior to them leaving hospital Email updates to PHT DOLS Group mailbox if: Patient is discharged / dies DOLS no longer required (Include reason) A ‘death in DOLS’ (Valid Urgent or Standard Authorisation) = a death in State Custody. The Coroner must be informed. Ensure your email includes confirmation that Coroner has been notified. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) DOLS GRANTED Await outcome of DOLS Office Assessments. ‘Lapsed’ Urgent DOLS You can lawfully detain the patient in hospital until: Their mental capacity to consent / refuse to being accommodated in hospital returns They are transferred to another care provider / discharged to a safe destination You would no longer prevent them from leaving hospital The Standard DOLS authorisation expires DOLS NOT GRANTED Work in the patients Best Interests: Continue to accommodate and treat in the patients Best Interests Complete ‘lapsed DOLS’ datix Request priority assessment from DOLS Office if any high risk DOLS triggers Page 3 of 32 Consider alternatives to treatment and accommodation Seek senior clinical / legal advice if unsafe to be discharged Allow to leave hospital taking all reasonable care to ensure safety e.g. TTO’s, inform GP Ask for 2nd opinion (DOLS and/or Mental Health) QUICK REFERRENCE GUIDE (2) The Acid Test A person may be considered to be deprived of their liberty if they lack the mental capacity to consent to accommodation in hospital (or care home) if: The person is subject to continuous supervision and control •Is the oversight continuous? (The person does not need to be in direct line of sight) •Does the care regime amount to supervision? •Is there a clear element of control? AND The person is NOT free to leave •The patient (or their relatives) does NOT need to request discharge The patient does NOT have to make meaningful attempts to leave Would you stop them if they tried to leave hospital? (Allowing the person to leave the ward (e.g. to the shop) but not to leave the hospital grounds would still be a deprivation of their liberty). •Does the care regime amount supervision? •Is there a clear element of control? to High Risk triggers for applying for DOLS / Taking a Lapsed DOLS to the Court of Protection • Patient (or family) stating they wish to leave hospital • Repeated use of physical or chemical restraint to prevent the person leaving / control behaviour • Family attempting to remove the person from hospital against medical advice Restrictions on family / friend contact • LPA believed to be acting in their own interests rather than the patients Best interests • Serious conflict between professionals and / or family regarding Best Interests • Nursing 'special' required for non-clinical reasons • Adult Safeguarding concerns Re-assess mental capacity of the person to make their own decision Please seek senior clinical advice Deprivation of Liberty Safeguards Policy Version: 2 Legal advice can be obtained 24/7 of a serious issue arises out of hours Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 4 of 32 1. INTRODUCTION The Deprivation of Liberty Safeguards (DOLS) were introduced in April 2009 and are part of the Mental Capacity Act 2005 (MCA). These safeguards are an important way of protecting the rights of vulnerable people. Depriving a person of their freedom may breach a person’s human right to liberty Article 5 (1) European Convention of Human Rights and Article 5(4), the right to have the lawfulness of detention reviewed by a court. The safeguards protect people who lack the ability to make certain decisions for themselves and ensure their freedom is not inappropriately restricted. Whilst every effort should be made to avoid depriving a person of their liberty, in certain circumstances it can be a necessary requirement to enable provision of effective care or treatment. The DOLS authorisation provides the legal framework and protection, when a deprivation of liberty is considered to be unavoidable, by allowing hospitals (and care homes) to accommodate a person in their best interests as defined by the MCA. Care must always be taken to ensure that if deprivation of liberty cannot be avoided, it should be for no longer than is necessary. DOLS are underpinned by the five key principles of the Mental Capacity Act: A presumption of capacity - every adult has the right to make his or her own decisions and must be assumed to have capacity to do so unless it is proved otherwise; The right for individuals to be supported to make their own decisions - people must be given all appropriate help before anyone concludes that they cannot make their own decisions; That individuals must retain the right to make what might be seen as eccentric or unwise decisions; Best interests – anything done for or on behalf of people without capacity must be in their best interests; and Least restrictive intervention – anything done for or on behalf of people without capacity should be the least restrictive of their basic rights and freedoms. In 2014 the Supreme Court reviewed the circumstances of three people (“P v Cheshire West and Chester Council and another” and “P and Q v Surrey County Council”). Previously the Courts had ruled all three people were not deprived of their liberty, however the Supreme Court ruling overturned this, determining that all 3 were in fact deprived of their liberty. The Supreme Court ruling introduced the ‘Acid Test’ to determine whether or not someone is being deprived of their liberty and applies when an individual lacks capacity to make a decision about being accommodated in hospital: Is the person subject to continuous supervision and control? The oversight must be continuous (though does not have to be ‘in line of sight’), must amount to supervision, and have a clear element of control. AND Is the person free to leave? The person may not be asking to go or showing by their actions that they want to leave but the issue is about how staff would react if the person did try to leave or if relatives/friends asked to remove them. 2. PURPOSE The guidance within this policy is intended to ensure the Trust discharges its duty under the MCA and DOLS legislation and meets the requirements of its registration with the Care Quality Commission. This policy outlines the legal framework around DOLS and gives guidance on the local policies, practice and procedures that should be followed by Portsmouth Hospitals NHS Trust staff when working with individuals who may lack mental capacity or are(or may become) deprived of their liberty. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 5 of 32 All persons working in a professional or paid role with people who may lack mental capacity have a legal duty to have regard to the Mental Capacity Act Code of Practice. Staff should view this guidance as supplementary to the statutory Mental Capacity Act Code of Practice and the DOLS Code of Practice. http://pht/Departments/safeguarding-adults/default.aspx 3. SCOPE All staff working within the Trust are likely to come into contact with vulnerable people who may lack the mental capacity to consent to care or treatment where it may be necessary to deprive that person of their liberty, in their best interests, in order to protect them from harm. This policy applies to persons aged 18 years and over only. In circumstances where a person aged 17 years or under may be deprived of their liberty please contact either the Child Safeguarding department on ext. 4314 or the Legal Department on ext. 6527 for advice (or via Hospital Duty Manager out of Hours). Assessing mental capacity and making decisions for those unable to do so for themselves is an interdisciplinary and/or multidisciplinary issue. Therefore, this policy applies to all permanent, locum, agency and bank staff of Portsmouth Hospitals NHS Trust and the MDHU (Portsmouth), including doctors, nurses, allied health professionals, support staff, social care professionals and managers. Whilst the policy outlines how the Trust will manage DOLS it does not replace the personal responsibilities of staff with regard to issues of professional accountability for governance. In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety. 4. DEFINITIONS DOLS - Deprivation of Liberty Safeguard: a legal authorisation that allows a managing authority (hospital or care home) to deprive someone who lacks mental capacity of their liberty. Mental capacity: Mental capacity is the ability of an individual to make decisions about specific aspects of their life. Mental Incapacity: an inability to make a specific decision at a particular time due to “an impairment or disturbance in the functioning of their mind or brain”. A person may be assessed as lacking capacity if they have any impairment of the brain or mind, and are unable to do one or more of the following : Understand information given to them Retain that information long enough to be able to make a decision Weigh up the information available to make a decision Communicate their decision Managing Authority: the organisation responsible for the care home or hospital applying for the DoLS authorisation i.e. Portsmouth Hospitals NHS Trust. Supervisory Body / Authority: the Local Authority which covers the person’s normal place of residence. Local Authorities are responsible for considering a DoLS request, arranging the required independent assessments and agreeing or denying a DoLS authorisation. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 6 of 32 5. DUTIES AND RESPONSIBILITIES Chief Executive will ensure that the Trust complies with relevant legal and statutory requirements related to the Deprivation of Liberty Safeguards. All Consultants should have a working knowledge of the MCA Code of Practice and DOLS legislation, will act as decision makers and are responsible for ensuring their teams complete the relevant assessments and documentation. They will also provide guidance within their teams. All Managers must be aware of Trust Policy and Guidelines and ensure their staff comply with the requirements of these documents. The Learning and Development Department will facilitate the collection of training data and support training and induction programme delivery. Clinical Service Centre Management Teams will identify key clinicians to undertake additional training and ensure effective cascade of key information to staff groups. Medical staff (ST3 and above) are designated signatories for the DOLS application. Duty Matrons and Hospital@Night can act as designated DOLS signatories out of hours if required. Individual members of staff must ensure they follow this policy. Safeguarding Adult Lead Nurse is responsible for collation of DOLS data, reporting of any known instances of an unauthorised DOLS and completion of the required CQC DOLS notifications. They will also provide advice and training to Trust staff to ensure compliance with MCA. CSC Safeguarding Operational Leads will act as a first line of contact and information resource within their area and across the Trust, providing advice, support and education as required. 6. PROCESS 6.1 Determine if a DOLS Authorisation is required (See table 1) A DOLS authorisation can only be granted to a person who lacks mental capacity to make a decision about hospital accommodation due to a mental disorder (disturbance / disorder of the mind). The mental disorder must directly relate to the person inability to make the relevant decision. (Department of Health (DH) guidance states that unconsciousness in itself is not considered to be a mental disorder). It is important to bear in mind that, while the deprivation of liberty might be for the purpose of giving a person treatment, a DOLS authorisation does not itself authorise treatment. Treatment that is proposed following authorisation of deprivation of liberty may only be given with the person’s consent (if they have capacity to make that decision) or in accordance with the wider provisions of the MCA. The Supreme Court ruled that the following factors are no longer relevant to whether or not someone is deprived of their liberty: the person’s compliance or lack of objection; the suitability or relative normality of the placement (after comparing the person’s circumstances with another person of similar age and condition); the reason or purpose leading to a particular placement. It is always necessary in each case to consider further: 1. Whether the Deprivation of Liberty lasts more than a negligible period of time. The DOLS Code of Practice suggests that unless a Standard DOLS Authorisation will be required then an application may not be necessary. ‘Negligible’ is not defined in law and in the short term, Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 7 of 32 Table 1 Is a DOLS indicated? (Adult patients over 18 years of age only) Has the person got a mental disorder? YES: assess mental capacity to make the decision about hospital accommodation. NO: A DOLS authorisation cannot be used. Did the person give consent to the care and treatment regime e.g. the patient gives advance consent whilst they still have capacity (surgery, elective procedures etc). YES: A capacitous person has consented to the care and treatment regime. No further action required. NO: continue to the next question Is there reason to doubt the patient’s mental capacity to make decisions about being accommodated in hospital? YES: continue to next question Does the Mental Health Act apply? YES: A DOLS authorisation should not be used. Apply the relevant MH Section now. NO: apply the Acid Test. Is the Acid Test met? Is the person subject to continuous supervision and control? The oversight must be continuous (though does not have to be ‘in line of sight’), it must amount to supervision, and have a clear element of control. AND Is the person free to leave? The person may not be asking to go or showing by their actions that they want to but the issue is about how staff would react if the person did try to leave or if relatives/friends asked to remove them. YES: The patient is being deprived of their liberty. Can the necessary care / treatment be provided in another setting or manner that would avoid depriving the person of their liberty? If care could be provided elsewhere but this option is not currently available (e.g. awaiting placement in care home) the answer is NO NO: Determine if a DOLS is required now or whether the powers of the MCA alone can be utilised. DOLS high Risk Triggers present? YES: Seek senior advice and consider DOLS application immediately. NO: A DOLS authorisation cannot be used. NO: A DOLS authorisation cannot be used. YES: A DOLS authorisation cannot be used NO: The patient is being deprived of their liberty YES: make alternative arrangements. DOLS will not be required as the person will not be deprived of their liberty. NO: Consider using the powers of the MCA alone. *Anticipated to regain mental capacity within 7 days OR Predicted Discharge Date of less than 7 days YES: Use the MCA. Complete Trust MCA Admission form. No: Apply for DOLS. *The DOLS Code of Conduct suggests that an urgent authorisation should not be used where there is no expectation that a standard deprivation of liberty authorisation will be needed. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 8 of 32 For example: • When treatment of the underlying physical illness is expected to lead to rapid resolution of the mental disorder such that a standard deprivation of liberty authorisation would not be required. It would not be appropriate to give an urgent authorisation simply to legitimise the short-term deprivation of liberty. • When a person is in an accident and emergency unit or a care home, and it is anticipated that within a matter of a few hours or a few days the person will no longer be in that environment 2. the powers of the MCA alone can be utilised. In the absence of high risk DOLS triggers (see below)Trust guidance is up to 7 days. 3. Whether the person is able to give consent to the deprivation e.g. the patient gives advance consent whilst they still have capacity. DOLS High Risk trigger factors Patient (or family) stating they wish to leave hospital Repeated use of physical or chemical restraint to prevent the person leaving / control behaviour Family attempting to remove the person from hospital against medical advice Restrictions on family / friend contact LPA believed to be acting in their own interests rather than the patients Best interests Serious conflict between professionals and / or family regarding Best Interests Nursing 'special' required for non-clinical reasons Adult Safeguarding concerns Does the Mental Health Act 1983 apply? When a person lacking mental capacity is in a hospital or care home receiving treatment for a mental disorder and is/is likely to have their liberty deprived, consideration should be given to use the provisions of the Mental Health Act rather than DOLS. If the person fits the criteria for a mental health section to be applied then that should be the chosen route. A mental health section does not normally allow treatment of a physical problem or illness that is unrelated to their mental health condition. In these circumstances a DOLS may be required, but the law is complex so senior clinical and legal advice should be sought. Factors that may indicate use of the Mental Health Act rather than DOLS include: • The patient’s lack of capacity to consent to treatment and care is fluctuating or temporary and the patient is not expected to consent when they regain capacity. This may be particularly relevant to patients having acute psychotic, manic or depressive episodes; • A degree of restraint needs to be used which is justified by the risk to other people but which is not permissible under the MCA as it cannot be said to be proportionate to the risk to the patient; and There is some other specific identifiable risk that the person or others might potentially suffer harm as a result. For example, if there is a risk that the person may need to be returned to the hospital or care home at some point in a manner that would not be authorised under DOLS. DOLS and Critical Care (E5 ward only) Due to level of chemical restraint (sedation), observation and monitoring that occurs when someone requires admission to a Critical Care unit (Intensive Care) it could be considered that the majority of patients cared for within this environment will meet the Acid Test. There is varied practice across the country with regard to DOLS applications in this situation, and Case Law does not yet give clear guidance. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 9 of 32 Taking into consideration the DH stance on unconsciousness, until further guidance is issued Trust guidance in relation to DOLS in critical care (E5 ward) can be seen in Table 2: Table 2: DOLS in Critical Care (E5 ward) DOLS Application will not normally be made when: DOLS Application should be considered when: A capacitous patient has consented to an elective procedure in the knowledge that admission to the critical care unit is likely / a possibility. Continuous sedation is discontinued. Lack of capacity to consent to ongoing hospital accommodation persists and exceeds Trust guidance on using the powers of the MCA alone i.e. 7 days. Day 1 = the day sedation is discontinued. OR A patient is admitted to critical care in an emergency situation and mental capacity for admission cannot be immediately assessed e.g. due to unconsciousness / severity of sudden illness and capacity cannot be assessed due to on-going continuous sedation. AND Next of Kin are in agreement with treatment and care plan. OR There is conflict between professionals and next of kin / family regarding care and treatment of the patient. OR High risk DOLS triggers during the MCA period, as per Table 1. AND Any patient who has not triggered a DOLS application should be reviewed at least every 28 days. When can’t a DOLS be used? The person is under 18 years of age; The person has made a valid and applicable Advance Decision refusing a necessary element of treatment for which they were admitted to hospital (see MCA Policy) The use of the safeguards would conflict with a decision of the persons attorney or Deputy of the Court of Protection; The patient lacks capacity to make decisions on some elements of the care and treatment they need, but has capacity to decide about a vital element and has already refused it or is likely to do so. If the main reason is to restrict contact with individuals who may cause the person harm. If it is believed to be in a person’s best interests to limit contact an application should be made to the Court of Protection. 6.2 Applying for a DOLS Authorisation There are two types of DOLS authorisation: • Urgent Authorisation – An Urgent DOLS must be applied if the person is being deprived of their liberty at this point in time. This is applied by a Managing Authority (i.e. the Trust) and is effective immediately once the form is completed and signed. It lasts a maximum of 7 calendar days (day 1 being the day of application). An application for a standard DOLS must be made at the same time in order to trigger independent DOLS assessment (Appendix 1 pages 1-6) . Without this, the urgent DOLS may be considered unlawful. In exceptional circumstances at the request of the DOLS office only, an Extension to an Urgent DOLS can be granted for a further period of 7 days. (see Appendix 1 page 7) Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 10 of 32 • Standard Authorisation – this is granted by a supervisory body (Local Authority DOLS Office) following independent assessment. This is always used in conjunction with an urgent authorisation but could be applied for on its own in anticipation of a future need for DOLS e.g. elective surgery for someone who is under a DOLS in a care home. If granted, a standard DOLS will have an expiry date, with a maximum of 1 year being granted. The time granted is dependent on the individual circumstances. Before granting an urgent authorisation, the managing authority should try to speak to the family, friends and carers of the person. Their knowledge of the person could mean that deprivation of liberty can be avoided. The managing authority should make a record of their efforts to consult others. In the situation where the person to be admitted is already subject to a DOLS authorisation in a care home, then it is very likely that the Trust will need to apply for DOLS authorisation in order to effect admission. For elective cases this can be applied for in advance of the planned admission date and it is the admitting clinicians’ responsibility to ensure this is completed. 6.3 Completing the DOLS application forms. Within the acute hospital, it is most common that a deprivation of liberty occurs suddenly and unexpectedly e.g. an emergency admission situation or as a result of a clinical deterioration. In these circumstances, when the deprivation is already occurring and cannot be avoided, the Trust as the managing authority must apply an Urgent DOLS Authorisation and request a Standard DOLS. Once DOLS forms are completed and signed it is legal to prevent the person leaving hospital. Form 1 Form Name Standard Request, Urgent When To put in place Urgent DOLS and Authorisation and Extension to Urgent request a Standard DOLS To request a Standard DOLS in advance Extension of the Urgent DOLS (only completed request of DOLS Office) 2 Further Request for a Further Standard Authorisation Current Standard DOLS Authorisation is coming to an end and the person needs to remain in hospital, deprived of their liberty past the current DOLS expiry date) The application forms can be completed electronically or by hand. Unless the signatory has an ‘electronic signature’ then forms will need to be printed and signed by hand. Guidance on completing the forms can be found in Appendix 3. 6.31 Who completes the DOLS forms? It is the responsibility of the clinical team caring for the patient to apply for a DOLS Authorisation. The care team should not be referring to other services for this. Trust signatories for DOLS forms are: Medical staff (ST3 grade and above) Duty Matron and Hospital@Night can also act as designated signatories if required out of hours Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 11 of 32 6.32 Where to send the forms DOLS application forms are sent to the relevant DOLS Office who arrange for independent assessments to be undertaken. In order to improve data security and monitoring, as of the 5th October 2015 this process will be managed centrally: The clinical team must email completed DOLS applications to: PHT.DOLS@porthosp.nhs.uk Do not put the forms in the internal mail system. Applications will be forwarded via secure email to the relevant DOLS office. The original forms should then be filed in the patient’s medical record. 6.4 Who to notify The patient - must be given a copy of the DOLS forms and have it explained to them, including the right to appeal. It may not be appropriate to do this at the time of the application, however, they must be given a copy prior to discharge and this should be documented in the patient’s medical records. The patients family / Next of Kin – Must be informed of the application being made, that it is a legal requirement for the Trust to do so, and that they will be contacted by an independent DOLS assessor. CSC management team (Care Quality Commission (CQC) - It is a requirement of the Trust’s registration with that the CQC are informed of all DOLS applications and outcomes. This is managed centrally by the Trust Adult Safeguarding Office). 6.5 What happens next? The Supervisory Body (DOLS Office) makes arrangements for the required assessments to be undertaken. Clinical staff should support this assessment process but are not required to undertake the assessments themselves. Access to the medical records should be made available to the assessors. Normal care and treatment of the patient, including discharge planning should continue during the assessment period. Where the patient also lacks mental capacity to make decisions about treatment options then, in line with the MCA, decisions must be made in their best interest. If for any reason the DOLS office does not complete the required assessments within the 7day Urgent Authorisation period and an Urgent Extension is not granted then the DOLS can be considered ‘lapsed’. In these circumstances it is essential to continue to accommodate and treat the person in their Best Interests as defined by the MCA: Contact DOLS office and request a priority assessment if any DOLS high risk triggers are present. If a priority assessment is not undertaken, senior clinical and legal advice should be taken to consider if the case needs to be referred to the Court of Protection. Ward staff should complete an internal incident form (Datix). This should be flagged as Adult Safeguarding highlighting a lapsed DOLS due to non-assessment by the DOLS Office. Conduct regular reassessment of patient’s mental capacity to make a decision about remaining in hospital. Conduct regular reassessments to see if the person still meets both elements of the Acid Test. DOLS Office contact Numbers Portsmouth DOLS Office: 023 9268 8666 – for residents in postcodes PO1-PO6 Southampton DOLS Office: 023 8083 4776 – for residents of Southampton City Hampshire DOLS Office: 01962 845213 – all other Hampshire postcodes Visitors to the area: seek assistance from Portsmouth DOLS Office Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 12 of 32 On completion of the assessment process, the Supervisory Body will either grant or deny the DOLS Authorisation. The DOLS Office will send the outcome forms to the ward and these forms must be filed in the medical record. A copy of these forms will also be sent to the Trust Safeguarding Office. 6.51 A Standard DOLS Authorisation is granted The care plan should include ongoing review of the treatment plan and the need for a continuing DOLS Authorisation. A patient held under DOLS may be kept in Portsmouth Hospitals for the proposed treatment and care until: The course of treatment is completed and the patient now longer needs to remain in hospital and can return to their normal place of residence Arrangements have been made for on-going care to continue in another location e.g. care home or specialist hospital The DOLS is judged to no longer be required. The clinical team must inform the DOLS Office and Trust Adult Safeguarding office. The DOLS expires. If continuing treatment and care is required in circumstances that amount to a deprivation of liberty then a further Standard Authorisation will be required. DOLS form 2 should be completed and sent to the DOLS Office as detailed above. The person’s mental capacity returns and they are able to make their own decision about continuing with treatment and care. In this circumstance the DOLS is no longer valid, even if the person decides to leave hospital or refuses to comply with treatment and care against medical advice. A DOLS Authorisation is specific to the Managing Authority and the address where the person will be held. Therefore it is permissible to transfer a patient who is held under a DOLS to another ward within the same location and belonging to the same provider. If the patient is transferred between different Trust hospitals e.g. Petersfield, Gosport and Queen Alexandra then a new Urgent/Standard application must be made. It is recommended that any ward moves are undertaken for clinical reasons only or as part of the anticipated patient journey (e.g. to move from intensive care to a ward when this level of care is no longer necessary; from MAU to the relevant specialty ward; to facilitate the provision of a side room if this was deemed essential). Any ward move should be undertaken in the person’s best interest and it is recommended that patients under a DOLS Authorisation are not outlied. 6.52. A Standard DOLS Authorisation is refused If the authorisation is refused or cannot be granted because the qualifying criteria have not been met, then the treatment and care plan should be reviewed again to see if less restrictive alternatives can be put in place. In this way the patient may consent to remain in hospital and undergo treatment. Alternatively consideration could be given to whether a different treatment option or care location can be arranged which would be acceptable to the patient e.g. change of antibiotics to allow administration to take place in the community, a less invasive or aggressive therapy, transfer to a facility closer to family. If the patient refuses all options presented then clinical staff should take steps to reduce the risks of discharge e.g. discharge medications, liaison with GP, social care and other community services, informing next of kin etc. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 13 of 32 However if there are major concerns about the patients safety should they leave hospital and fail to comply with what is deemed essential treatment and care, senior clinical and legal advice should be sought. In some cases application to the Court of Protection may be required. Requests for legal advice should be made through the Trust Legal Services office ext. 6527 or via Hospital Duty Managers out of hours. 6.6 A patient dies whilst subject to a DOLS Authorisation A DOLS Authorisation is considered to be a form of lawful state detention. Therefore in the event of the person dying the Coroner must be informed, as this will be considered a death in custody. The following should be reported: Anyone who dies under the 7-days Urgent DOLS Authorisation Anyone who dies under a Standard DOLS Authorisation You do not need to report when: x x A DOLS Authorisation has been refused following DOLS office assessments (unless there are other reasons for doing so) Lapsed DOLS: A DOLS has been applied for and the Urgent Authorisation has lapsed due to lack of assessments by the DOLS Office even though in their Best Interests we continue to ‘detain’ the person in hospital (unless there are other reasons for doing so). The Clinical team caring for the patient is responsible for reporting the death to the Coroner. Staff will need to be sensitive to the impact this may have on next of kin, family and friends. The next of kin must be informed of the requirement to report to the Coroner and that an inquest will be held. This is a legal requirement and does not in itself imply that there is anything ‘untoward’ with the circumstances of their loved ones death or the care and treatment provided. An inquest does not always necessitate a post mortem to be performed, however this decision will be made by the Coroner. A Registered Nurse may not verify the death of someone who is under a DOLS Authorisation even if the death is ‘expected’ and would otherwise by permissible under the ‘Policy for when an Adult Dies’. 6.7. Unauthorised Deprivations of Liberty If a public body does not have the authority to deprive an individual of their liberty they will be acting unlawful contrary to the Human Rights Act 1998. Consequences of failing to obtain an authorisation may expose the Trust not only to a claim before the courts but also to sanction from regulators and / or the Ombudsman. If staff are concerned that an unauthorised deprivation of liberty has occurred or is likely to occur within the Trust then a senior clinician should review the situation as a matter of urgency. Steps should be taken to avoid/prevent any further/potential deprivation of liberty. In order to achieve this it may be necessary to apply an Urgent Authorisation or review the steps outlined in Table 1. Any unauthorised deprivation of liberty must be reported as an adverse incident on Datix and graded as Amber. A Safeguarding Alert must also be raised and the relevant CSC Management team must be informed as a matter of urgency . Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 14 of 32 All unlawful DOLS will be reported to the CQC and external Safeguarding partners. The Trust Adult Safeguarding office will coordinate these notifications with the Governance Department and the relevant CSC Management Team. If there is a concern that a deprivation of liberty may be occurring in non-Trust accommodation then staff should discuss the concerns with their line manager as soon as possible and the Managing Authority of the care home of hospital. The Supervisory Authority should also be notified. 7 TRAINING REQUIREMENTS Introductory Level: All trust staff will have a basic DOLS awareness. This will be achieved via the essential update programme. Enhanced Level: All inpatient based clinical staff who deliver direct patient care Designated Trust DOLS signatories Security staff Enhanced level training is available internally via classroom-based sessions and is delivered by Trust and CSC Adult Safeguarding Leads. Training is also available in partnership with our external health and social care partners. Details are available from Safeguarding Leads. Each line manager has the responsibility to ensure their staff are afforded the opportunity to undertake all essential skill training. 8 REFERENCES AND ASSOCIATED DOCUMENTATION Mental Capacity Act 2005. Deprivation of Liberty Safeguards: A guide for hospitals and care homes. DH. 2009 What are the Mental Capacity Act 2005 Deprivation of Liberty Safeguards. DH. 2008 Mental Health Act 2007. The Mental Capacity Act 2005 Deprivation of Liberty Safeguards and you. Easy Read. DH. 2009 Deprivation of Liberty Safeguards Code of Practice to supplement the main Mental Capacity Act 2005 Code of Practice. Ministry of Justice. 2008 Identifying a deprivation of liberty: a practical guide. The Law Society. 2015 Update on the Mental Capacity Act and DOLS following the 10 March 2014 Supreme Court Judgement. (Letter) Niall Fry, MCA-DOLS policy Lead. Department of Health. January 2015 9 EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly. Our values are the core of what Portsmouth Hospitals NHS Trust is and what we cherish. They are beliefs that manifest in the behaviours our employees display in the workplace. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 15 of 32 Our Values were developed after listening to our staff. They bring the Trust closer to its vision to be the best hospital, providing the best care by the best people and ensure that our patients are at the centre of all we do. We are committed to promoting a culture founded on these values which form the ‘heart’ of our Trust: Respect and dignity Quality of care Working together No waste This policy should be read and implemented with the Trust Values in mind at all times. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 16 of 32 10 MONITORING COMPLIANCE WITH, AND THE EFFECTIVENESS OF, PROCEDURAL DOCUMENTS Monitoring of compliance with this guidance will be undertaken at two levels: one at a corporate level related to corporate function and response and at a divisional level related to compliance at practice level. Results will be reported to the Safeguarding Committee. Minimum requirement to be monitored Lead Tool Frequency of Report of Compliance Reporting arrangeme nts Lead(s) for acting on Recommendation s 85% of all Trust staff will have completed Introductory Level training. CSC Management Teams Report from Learning and Development Department Quarterly Safeguarding Committee Adult Safeguarding Lead Nurse 85% of identified staff groups have completed Enhanced Level training CSC Management Teams Report from Learning and Development Department Quarterly Safeguarding Committee Adult Safeguarding Lead Nurse 85% of staff sampled will be aware of where to seek advice within the Trust with regard to DOLS issues Safeguarding Operational Leads Audit ( sample of 10 staff per specialty) Annually Safeguarding Committee CSCs Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 17 of 32 APPENDIX 1: DOLS Form 1 - Standard and Urgent DOLS Request Case ID Number: DEPRIVATION OF LIBERTY SAFEGUARDS FORM 1 REQUEST FOR STANDARD AUTHORISATION AND URGENT AUTHORISATION Request a Standard Authorisation only (you DO NOT need to complete pages 6 or 7) Grant an Urgent Authorisation (please ALSO complete pages 6 and 7 if appropriate/required) Full name of person being deprived of liberty Sex Date of Birth (or Est. Age estimated age if unknown) Relevant Medical History (including diagnosis of mental disorder if known) Sensory Loss Communication Requirements Name and address of the care home or hospital requesting this authorisation Telephone Number Person to contact at the care home or hospital, (including ward details if appropriate) Name Telephone Email Ward (if appropriate) Usual address of the person, (if different to above) Telephone Number Name of the Supervisory Body where this form is being sent How the care is funded Local Authority please specify NHS Self-funded by person Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Local Authority and NHS (jointly funded) Funded through insurance or other Page 18 of 32 REQUEST FOR STANDARD AUTHORISATION THE DATE FROM WHICH THE STANDARD AUTHORISATION IS REQUIRED: If standard only – within 28 days If an urgent authorisation is also attached – within 7 days PURPOSE OF THE STANDARD AUTHORISATION Please describe the care and / or treatment this person is receiving or will receive day-to-day and attach a relevant care plan. Please give as much detail as possible about the type of care the person needs, including personal care, mobility, medication, support with behavioural issues, types of choice the person has and any medical treatment they receive. Explain why the person is or will not be free to leave and why they are under continuous or complete supervision and control. Describe the proposed restrictions or the restrictions you have put in place which are necessary to ensure the person receives care and treatment. (It will be helpful if you can describe why less restrictive options are not possible including risks of harm to the person.) Indicate the frequency of the restrictions you have put in place. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 19 of 32 INFORMATION ABOUT INTERESTED PERSONS AND OTHERS TO CONSULT Family member or friend Name Address Telephone Anyone named by the person as Name someone to be consulted about their welfare Address Telephone Anyone engaged in caring for the Name person or interested in their welfare Address Telephone Any donee of a Lasting Power of Name Attorney granted by the person Address Telephone Any Personal Welfare Deputy Name appointed for the person by the Court of Protection Address Telephone Any IMCA instructed in Name accordance with sections 37 to 39D of the Mental Capacity Act Address 2005 Telephone Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 20 of 32 WHETHER IT IS NECESSARY FOR AN INDEPENDENT MENTAL CAPACITY ADVOCATE (IMCA) TO BE INSTRUCTED Place a cross in EITHER box below Apart from professionals and other people who are paid to provide care or treatment, this person has no-one whom it is appropriate to consult about what is in their best interests There is someone whom it is appropriate to consult about what is in the person’s best interests who is neither a professional nor is being paid to provide care or treatment WHETHER THERE IS A VALID AND APPLICABLE ADVANCE DECISION Place a cross in one box below The person has made an Advance Decision that is valid and applicable to some or all of the treatment The Managing Authority is not aware that the person has made an Advance Decision that may be valid and applicable to some or all of the treatment The proposed deprivation of liberty is not for the purpose of giving treatment THE PERSON IS SUBJECT TO SOME ELEMENT OF THE MENTAL HEALTH ACT (1983) Yes No If Yes please describe further e.g. application/order/direction, community treatment order, guardianship OTHER RELEVANT INFORMATION Names and contact numbers of regular visitors not detailed elsewhere on this form: Any other relevant information including safeguarding issues: PLEASE NOW SIGN AND DATE THIS FORM Signature Print Name Date Time I HAVE INFORMED ANY INTERESTED PERSONS OF THE REQUEST FOR A DoLS AUTHORISATION (Please sign to confirm) Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 21 of 32 RACIAL, ETHNIC OR NATIONAL ORIGIN Place a cross in one box only White Mixed / Multiple Ethnic groups Asian / Asian British Black / Black British Not Stated Undeclared / Not Known Other Ethnic Origin (please state) THE PERSON’S SEXUAL ORIENTATION Place a cross in one box only Heterosexual Homosexual Bisexual Undeclared Not Known OTHER DISABILITY While the person must have a mental disorder as defined under the Mental Health Act 1983, there may be another disability that is primarily associated with the person. This is based on the primary client types used in the Adult Social Care returns. To monitor the use of DoLS, the HSCIC requests information on other disabilities associated with the individual concerned. The presence of “other disability” may be unrelated to an assessment of mental disorder or lack of capacity. Place a cross in one box only Physical Disability: Hearing Impairment Physical Disability: Visual Impairment Physical Disability: Dual Sensory Loss Physical Disability: Other Mental Health needs: Dementia Mental Health needs: Other Learning Disability Other Disability (none of the above) No Disability RELIGION OR BELIEF Place a cross in one box only None Not stated Buddhist Hindu Jewish Sikh Muslim Any other religion Christian (includes Church of Wales, Catholic, Protestant and all other Christian denominations) Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 22 of 32 ONLY COMPLETE THIS SECTION IF YOU NEED TO GRANT AN URGENT AUTHORISATION BECAUSE IT APPEARS TO YOU THAT THE DEPRIVATION OF LIBERTY IS ALREADY OCCURING, OR ABOUT TO OCCUR, AND YOU REASONABLY THINK ALL OF THE FOLLOWING CONDITIONS ARE MET URGENT AUTHORISATION Place a cross in EACH box to confirm that the person appears to meet the particular condition The person is aged 18 or over The person is suffering from a mental disorder The person is being accommodated here for the purpose of being given care or treatment. Please describe further on page 2 The person lacks capacity to make their own decision about whether to be accommodated here for care or treatment The person has not, as far as the Managing Authority is aware, made a valid Advance Decision that prevents them from being given any proposed treatment Accommodating the person here, and giving them the proposed care or treatment, does not, as far as the Managing Authority is aware, conflict with a valid decision made by a donee of a Lasting Power of Attorney or Personal Welfare Deputy appointed by the Court of Protection under the Mental Capacity Act 2005 It is in the person’s best interests to be accommodated here to receive care or treatment, even though they will be deprived of liberty Depriving the person of liberty is necessary to prevent harm to them, and a proportionate response to the harm they are likely to suffer otherwise The person concerned is not, as far as the Managing Authority is aware, subject to an application or order under the Mental Health Act 1983 or, if they are, that order or application does not prevent an Urgent Authorisation being given The need for the person to be deprived of liberty here is so urgent that it is appropriate for that deprivation to begin immediately before the request for the Standard Authorisation is made or has been determined AN URGENT AUTHORISATION IS NOW GRANTED This Urgent Authorisation comes into force immediately. It is to be in force for a period of: days The maximum period allowed is seven days. This Urgent Authorisation will expire at the end of the day on: Signed Print name Date Time Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 23 of 32 REQUEST FOR AN EXTENSION TO THE URGENT AUTHORISATION If Supervisory Body is unable to complete the process to give a Standard Authorisation (which has been requested) before the expiry of the existing Urgent Authorisation An Urgent Authorisation is in force and a Standard Authorisation has been requested for this person. The Managing Authority now requests that the duration of this Urgent Authorisation is extended for a further period of DAYS (up to a maximum of 7 days) It is essential for the existing deprivation of liberty to continue until the request for a Standard Authorisation is completed because the person needs to continue to be deprived and exceptional reasons are as follows (please record your reasons): Please now sign, date and send to the SUPERVISORY BODY for authorisation Signature D a t e RECORD THAT THE DURATION OF THIS URGENT AUTHORISATION HAS BEEN EXTENDED This part of the form must be completed by the SUPERVISORY BODY if the duration of the Urgent Authorisation is extended. The Managing Authority does not complete this part of the form. The duration of this Urgent Authorisation has been extended by the Supervisory Body. It is now in force for a further days Important note: The period specified must not exceed seven days. This Urgent Authorisation will now expire at the end of the day on: SIGNED (on behalf of the Supervisory Body) Signature Print Name Date Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Time Page 24 of 32 APPENDIX 2: DOLS FORM 2 - FURTHER REQUEST FOR A FURTHER STANDARD AUTHORISATION Case ID Number: DEPRIVATION OF LIBERTY SAFEGUARDS FORM 2 REQUEST FOR A FURTHER STANDARD AUTHORISATION Full name of person deprived of their liberty being Sex Date of Birth (or estimated age if unknown) Est. Age Name and Address of Managing Authority (care home or hospital) requesting this authorisation Person to contact at the care Name home or hospital, (include ward Telephone details if appropriate) Email Ward (if appropriate) THE PURPOSE OF THE AUTHORISATION is to enable the following care and / or treatment to be given: Please describe the care and / or treatment this person is receiving or will receive day-to-day and attach a relevant care plan. Please give as much detail as possible about the type of care the person needs, including personal care, mobility, medication, support with behavioural issues, types of choice the person has and any medical treatment they receive. THE DATE FROM WHICH THE STANDARD AUTHORISATION IS SOUGHT: A further Standard Authorisation is required to start on this date so it is force immediately after the expiry of the existing Standard Authorisation. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 25 of 32 OTHER RELEVANT INFORMATION Please include details of any changes previously given in Form 1 e.g. in the care plan, medical information, person’s behaviour or visitors. Signature Print name Date Time I HAVE INFORMED ANY INTERESTED PERSONS OF THE REQUEST FOR A FURTHER STANDARD AUTHORISATION (Please sign to confirm) Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 26 of 32 APPENDIX 3: GUIDANCE ON COMPLETING DOLS APPLCATION FORMS FORM 1: STANDARD REQUEST, URGENT AUTHORISATION AND EXTENSION TO URGENT In the acute hospital setting it is likely that a deprivation of liberty occurs as an ‘emergency’ and cannot be predicted and a DOLS Authorisation applied for in advance. In these circumstances it is necessary to apply for both an Urgent and Standard DOLS Authorization. Page 1: This page will take you through the person’s basic details. It is helpful to assessors if you can summarise relevant medical history, give details of any sensory loss and in particular describe the person’s communication needs as this will help the assessor prepare and enable them to consider whether any aids are needed or in fact whether an interpreter may be needed. However, the presence of sensory loss or communication needs is not necessarily indicative of a lack of capacity. Page 2: Purpose of the Authorisation - this provides two essential pieces of information. A description of the care and treatment - in other words: Why do you need to accommodate the person in the care home or hospital? It asks you to describe in detail the care and/or treatment the person is receiving. It is helpful to assessors if this is as detailed as possible rather than a vague statement such as “24 hour care”. Secondly you are asked to explain why the person meets the acid test for a deprivation of liberty. The following information may be helpful: http://www.39essex.com/docs/newsletters/deprivation_of_liberty_after_cheshire_west__a_guide_for_front-line_staff.pdf http://www.cqc.org.uk/sites/default/files/20140416_supreme_court_judgment_on_deprivation_of_li berty_briefing_v2.pdf http://www.39essex.com/content/wpcontent/uploads/2014/02/deprivation_of_liberty_in_the_hospital_settingv3.pdf In this section you need to describe all the measures you are taking which have led you to make a request for an Authorisation: • describe the environment the person is in • who has determined where they live • whether it is a temporary or permanent arrangement • how are they monitored by staff leading you to conclude they are under continuous or complete supervision and control and are not free to leave. When describing all the restrictions it is helpful to say how frequently they are taking place. For example it is better to say: “Mrs X has to be reassured and redirected by staff at least 4-5 times a day as she is distressed and wants to leave.” rather than: “Mrs X says she wants to leave.” Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 27 of 32 It is better to say: rather than: “1:1 support is in place at all times of day, when John is in his room or moving around the building, when he has meals or takes part in social events. However at night there is less support as there is a sleeping night and no checks are made beyond the routine checks.” “John has 1:1 support.” Page 3: What is an Interested Person? An interested person is any of the following: The relevant person’s spouse or civil partner; Where the relevant person and another person of the opposite sex are not married to each other but are living together as husband and wife - the other person; Where the relevant person and another person of the same sex are not civil partners of each other but are living together as if they were civil partners - the other person; The relevant person’s children and step children; The relevant person’s parents and step parents; The relevant person’s brothers, sisters, half-brothers, half-sisters, step brothers and step sisters; The relevant person’s grandparents or grandchildren. The form also asks for other people such as anyone caring for the person or interested in their welfare. This could include social workers or care staff. Page 4: IMCA – Advance Decision – Mental Health Act IMCA: It is necessary for the Managing Authority to inform the DoLS team if the person will need an IMCA to support them. The DoLS team at the Supervisory Body will make the referral but you need to state whether the person has anyone appropriate to consult with. Advance Decisions: There is also a question about any Advance Decisions to refuse treatment the person may have made that you are aware of. Mental Health Act 1983: If you are aware of any aspect of the Mental Health Act that applies to the person, for example they may be subject to a Guardianship Order, then this is where you need to include that information, with as much detail as you are able to provide. Once you sign and date the form you will also be asked to confirm that you have advised any interested persons of the request for a DoLS Authorisation. Communication with close family members is very important from the beginning. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 28 of 32 Page 5: Important Data Collection This information is required for the quarterly DoLS returns to the Health and Social Care Information Centre. Please note this information is based on the Adult Social Care collection and the disability here does not refer to mental incapacity but to any other disability that may apply to the person. Page 6: Urgent Authorisation – complete only where the need for the deprivation of liberty is so urgent that it is in the best interests of the person for it to begin while the application is being considered. Although the original intention was that an Urgent Authorisation would be for “sudden unforeseen needs” in practice this has not been the case and Managing Authorities often use Urgent Authorisations. There is an expectation that in the vast majority of cases it should be possible to plan ahead and make sure that a Standard Authorisation is requested ahead of the need for the deprivation of liberty to begin. An Urgent Authorisation should only be given where the need for the deprivation of liberty is so urgent that it is in the best interests of the person for it to begin while the application for a Standard Authorisation, which is expected to be necessary, is being considered. There are some situations where an Urgent Authorisation is generally not needed, such as: • Someone has developed a mental disorder as a result of a physical illness which can be treated and treating it will rapidly resolve the mental disorder. An example of this would be someone currently confused due to a urinary tract infection, but when treated with antibiotics the confusion usually resolves within a negligible period of time. • Where a person is in accident and emergency or a care home and it is anticipated that in a matter of hours the person will no longer be there. The tick boxes are straightforward as all of the details will have been provided earlier in the form. The Urgent Authorisation can be given for a period of up to seven calendar days and comes into force at the time it is signed. Page 7: Request for an Extension of the Urgent Authorisation Complete page 7 only of requested to do so by the DOLS Office. The intention of adding the request for an extension of an Urgent Authorisation to the initial form is to identify this at the beginning due to the unprecedented numbers of applications following the Supreme Court Judgement: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/300106/DH_Note_re _Supreme_Court_DoLS_Judgment.pdf The DoLS Code of Practice describes that an Urgent Authorisation can be extended if there are “exceptional reasons” why the Standard Authorisation cannot be dealt with within the seven days. The Code of Practice gives an example of when an extension may be justified as an assessor not being able make contact with someone who it is essential to speak to. The Supervisory Body must decide what it considers to be “exceptional reasons”. The Code is very clear about the following: • A decision about exceptional reasons must be soundly based and defensible; • It would not usually be justified due to staff shortages; • An Urgent Authorisation can only be extended once. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 29 of 32 FORM 2: REQUEST FOR A FURTHER STANDARD AUTHORISATION A Further Standard Authorisation is a new request for the same person. When an existing DoLS Authorisation is coming to an end the Managing Authority must review whether it is still necessary. It is possible, at any stage, that things have changed and the person no longer needs such a restrictive environment. In this case the Managing Authority needs to request a Review to cease the DoLS Authorisation (Form 9 – Standard Authorisation Ceased). If however, having reviewed the person’s current situation, the Managing Authority concludes that the Authorisation needs to continue then a Further Authorisation should be requested. This can be done up to 28 days in advance and should not be left to the last moment. The amount of information needed when a Further Request for Authorisation is being made, is much less than the initial requirement as the Supervisory Body will have already received a great deal of personal details and comprehensive information and will have carried out the necessary assessments to grant an initial Authorisation. This form is short and should assist Managing Authorities to request further authorisations in a timely way. The main focus of this form is on two essential pieces of information: 1) The purpose of the deprivation of liberty, in other words why the person is still a resident or a patient and a description of the current care or treatment arrangements 2) An opportunity to update any changes to the care or treatment plan and the restrictions in place, update information and record changes since the previous Authorisation was given. Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 30 of 32 Equality Impact Screening Tool To be completed and attached to any procedural document when submitted to the appropriate committee for consideration and approval for service and policy changes/amendments. Stage 1 - Screening Title of Procedural Document: Deprivation of Liberty Safeguards: Practice and Procedures Policy Date of Assessment 24 September 2015 Responsible Department Risk Management Dept Name of person completing assessment Anne Taylor Job Title Adult Safeguarding Lead Does the policy/function affect one group less or more favourably than another on the basis of : Yes/No Age No Disability No Comments Learning disability; physical disability; sensory impairment and/or mental health problems e.g. dementia Ethnic Origin (including gypsies and travellers) No Gender reassignment No Pregnancy or Maternity No Race No Sex No Religion and Belief No Sexual Orientation No If the answer to all of the above questions is NO, the EIA is complete. If YES, a full impact assessment is required: go on to stage 2, page 2 More Information can be found be following the link below www.legislation.gov.uk/ukpga/2010/15/contents Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 31 of 32 Stage 2 – Full Impact Assessment What is the impact Level of Impact Mitigating Actions (what needs to be done to minimise / remove the impact) Responsible Officer Monitoring of Actions The monitoring of actions to mitigate any impact will be undertaken at the appropriate level Specialty Procedural Document: Specialty Governance Committee Clinical Service Centre Procedural Document: Clinical Service Centre Governance Committee Corporate Procedural Document: Relevant Corporate Committee All actions will be further monitored as part of reporting schedule to the Equality and Diversity Committee Deprivation of Liberty Safeguards Policy Version: 2 Issue Date: 01 October 2015 Review Date: 30 September 2017 (unless requirements change) Page 32 of 32