We are all aware that UV light has proved very effective in the
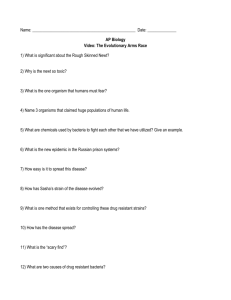
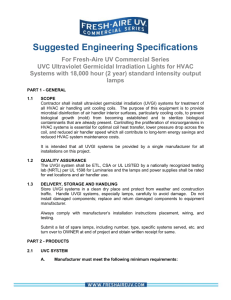
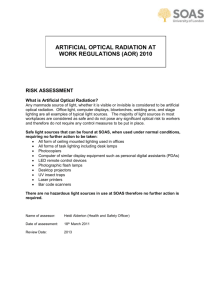
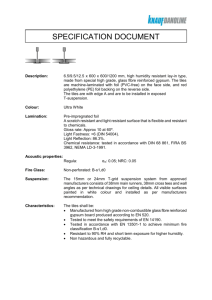
advertisement

1 Controlled use of UVC radiation prevents the spread of drug resistant Tuberculosis We are all aware that UV light and the ozone produced by interaction of UVC with light has proved very effective in the purification of water, making it potable without the disadvantages of adding chemicals such as chlorine, and avoiding the unpleasant final taste. UVGI (Ultraviolet Germicidal Irradiation) can be equally effective in sanitizing air (first reported use was in the 1930s) and killing harmful bacteria and microbes, including TB. In all these cases it is UVC which is used. Sunlight provides irradiation at ground level of longer wavelength UVA and UVB which are used by holiday makers for obtaining a sun tan. Another short waveband in the near ultraviolet is used in special hospital cots to cure Bilirubin in newly born infants. While UVA and UVB have their own problems such as the possible eventual emergence of skin cancer, UVC (225 to 302nm but usually 254 nm) is highly dangerous to both the eyes (photokeratoconjunctivitis) and the skin (erythema) but we are shielded against the solar radiation by the ubiquitous ozone layer. UVC is produced during welding and welders use both protective shielding glass in their helmets and gloves to protect against its effect, and the welding sites within a factory should be protected against prying eyes by effective curtains. In the case of air one of UV’s major tasks is to prevent the spread of Mycobacterium tuberculosis (M.tb) or TB as it is more commonly known as. In the era of Sanatoria, patients were wheeled out during sunlight hours to benefit from the less powerful effects of the rest of solar UV. There is some controversy about the effectiveness of ultraviolet light in combating the spread of airborne bacilli and over the years both successes and failures have been recorded. It has never been clinically proven that UVC prevents the spread of TB and other diseases and research funding dried up more than fifty years ago when it looked as if the world had beaten the scourge once and for all. Experiments in 1961 showed that a UV system eliminated TB bacilli from hospital ward exhaust air but a 1954 study showed a failure to reduce the spread of the disease in London schools. However more evidence suggests that it is effective if implemented correctly. The leading hospital today in the USA for treating drug resistant TB has used UVGI for more than twelve years and has the highest success rate, showing the fewest number of conversions from normal TB to one of the drug resistant forms. The spread of the disease was also curtailed in America’s shelters for the homeless though this programme of experiments was terminated before conclusion, as TB had been eliminated using drugs developed at that time! The apparent failures that took place are explained by some experts as the cloning of UVGI systems without regard to operating conditions. The resurgence of TB around the world has seen a change of pattern for experiments and new opportunities for drug manufacturers. TB is still being diagnosed in the same way it was in 1882 and no new TB drugs have been released in over forty years. TB has experienced a resurgence in recent years and is often a hallmark of HIV/AIDS, causing sufferers not to seek medical attention because of the social stigma. The new problem which has hit the world, including South Africa (and elsewhere as highlighted by a recent airline incident where a person having drug resistant TB travelled on several flights despite being warned not to), is the emergence of highly drug resistant forms of TB. This has placed a new emphasis on preventing the spread of TB from patient to others (remember totally healthy people are just as susceptible). Statistics show that in one 2 Controlled use of UVC radiation prevents the spread of drug resistant Tuberculosis year’s time an infected person could transfer the disease to 10 to 15 close contacts. The situation in South Africa is particularly bad and the World Health Organisation has asked this country to improve infection controls in hospitals as health facilities risked becoming a breeding ground for XDR-TB (eXtremely Drug Resistant TB) if patients and staff are not adequately protected from those infected. As a result some local hospitals are experimenting with UVGI used in room fittings (see below). In a report by the Health Minister to parliament (June 2007) it was disclosed that out of 403 cases identified with XDR-TB some 265 had already died, emphasizing just how deadly the infection is. South Africa has the world’s seventh largest TB population where the estimated number of TB cases in the world was almost 9 million in 2005. In South Africa it has been realized that hospitals are still being designed the way they were two decades ago and the TB pandemic of today is not being addressed in the design of new facilities. To investigate the relationship between design and disease spread, a new facility (known colloquially as AIR, and under the joint control of the MRC and CSIR with overseas consultants) has been constructed at Witbank and guinea pigs are used as humans surrogates (they closely resemble humans in their response to TB). This year one of the topics under research will be the effectiveness of UV radiation in preventing the spread of the disease, particularly the MDR (Multi Drug Resistant) and XDR variants. It is hoped that the output of this study will allow the design of more effective TB wards where infection of others (both patients and medical staff) is minimised. An advantage by the way of UV irradiation is that it doesn’t distinguish between regular and drug resistant TB, killing the bacteria of both with equal abandon. UVGI can be used in hospital wards, waiting areas and other environments in one of two ways. It can be fitted into an air extraction system which already has very effective filtering or it can be used in light fittings to irradiate the upper part of a room. The filtration method only works where the building has been designed for this task and this is not usually the case for makeshift TB wards established as the pandemic spreads. The UV lamps are safe as they are placed out of sight in the ducts and calculations can be made on the UV irradiance required to kill 90% or more of the TB bacteria. Remember that the duct must also contain a high efficiency filtration unit capable of removing the rest. The clean air can be ducted to the outside or returned to its site of origin to remove any residual bacteria on a second pass. The upper air light fittings are a cost-effective way of controlling the spread of bacteria in an already constructed ward or waiting room and the rest of this article will focus on this method. The 1994 CDC (Centre for Disease Control and Prevention) guidelines of 1994 relied on upper air studies that were over 30 years old. To address this issue a comprehensive study was carried out in the USA in 2002 using modern UVGI louvered fittings that created a band of UV irradiation in the upper layer of the room with an average depth of some 0.3 m. The recommendation of the study was that the irradiance should be in the region of 50 µW cm-2 in order to reduce airborne concentrations within the room by 90%. The effectiveness of the system was evaluated using a heated mannequin to simulate the human body with safe test TB surrogates being used. To be effective the air circulation in the room must be such that the heated air expelled by the patient coughing must rise and 3 Controlled use of UVC radiation prevents the spread of drug resistant Tuberculosis go through the UV irradiated layer. The level of irradiance required to kill the bacteria varies (various research results show a variance in kill factor which varies by an issue of five) and Professor Leuschner of the University of Pretoria uses the more generally accepted figure of 108 µW / cm2 so as to achieve a survival fraction of 10% in 10 seconds exposure to the radiation. The lamps used are louvered (or contain baffles) so as to direct the UV radiation up so that patients are not exposed either directly or indirectly and cannot view the UV lamps directly. Leuschner, who is involved in testing of the fittings for local companies, uses a figure of 6 µW/cm2 as being a safe level of exposure to 254 nm radiation (0.2 µW/cm2 has been used by others as safe at the 1.5 metre level). UV lamps are not like normal fluorescent bulbs and output decreases with time, the lamps requiring renewal before they are finished. The installation must be monitored regularly over time using a calibrated UV meter in order to ensure both effectivity and safety. It is possible for example that louvers are damaged and allow ultraviolet light into the room in which they are located. Regarding location the recent experiment in the USA used directly above and room corner fittings to ensure that all contaminated air was exposed. Using the results generated by a test laboratory such as that of Leuschner it can be calculated where lamp fittings should be located to ensure total coverage of upper air by UV irradiation greater than the kill factor. Despite all the questions surrounding upper air disinfectation, hospitals within South Africa are installing them on the presumption that some form of prevention of the spread of TB is better than none. Some light fitting manufacturers are fitting suction fans at the end of the lamp housing in order to improve upper air mixing. Specifically guidelines are necessary for the light fittings, the position and number of lamps and ensuring that the air flow in the room is adequate to ensure the necessary upper air interaction with the active UV radiation. Other considerations include humidity, as previous studies have indicated decreased effectiveness under higher humidity levels. Above all else the lamps must be regularly monitored for UV irradiance using a UV meter and readings must be taken to ensure that patients are not directly exposed from any normal position in the room. Perhaps part of the system monitoring could be automated with a control panel indicating which lamps are operating below effective levels. TBarticle 1697 words