This “toolkit” - American College of Obstetricians and Gynecologists
advertisement

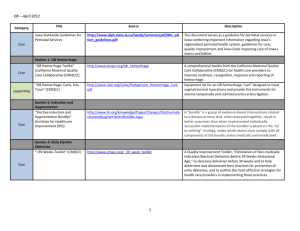
ACOG Medical Home Toolkit Introduction: This “toolkit” is intended to help members of an ob-gyn practice assess whether they might be interested in making the investment to become a medical home, to determine how significant the changes to their current practice will be, and to make the changes that will be required. The Patient Centered Medical Home (PCMH) is a health care setting that facilitates partnerships between individual patients, their personal physicians, and, when appropriate, the patient’s family. This partnership requires a greater commitment by both the patient and the medical practice than has been present in most doctor-patient relationships in the past. These are the main characteristics of a medical home: (1) The patient has a regular doctor or place of care that is chosen by the patient. (2) The medical home clinical staff knows the important information about the patient’s medical history, and that information is included in the medical record. (3) The medical is easy to contact by phone during regular office hours. (4) The doctor and staff at the medical home help coordinate care received from other doctors or sources of care. It is hoped and expected that patient care associated with the Medical Home will improve outcomes. Some Medical Home demonstration projects have specific requirements that are not included in this information. The expectations of stakeholders (third party payers, certification organization, and other medical specialties) vary. Nonetheless, ob/gyn practices interested in incorporating the Medical Home concept will share certain characteristics. This tool kit can help the practice meet regulatory requirements for accreditation as a Patient Centered Medical Home. Medical home demonstration projects generally include a change in the payment system, rewarding practices for making the changes that are necessary to become medical homes. Medical home projects often describe multiple “tiers,” rewarding practices based on the extent of their progress toward making the changes in their infrastructures that are required to become PCMHs. For more general background information and description of the Medical Home practice model, see the article Medical Home –Answers to Some Questions on ACOG’s web site at http://www.acog.org/departments/dept_notice.cfm?recno=19&bulletin=5027 1 Name: Practice: Date: You will need to enable macros to fill in the forms in this Word document. How to Use ACOG’s Medical Home Tool Kit This tool kit guides users through six categories. Please complete each section before proceeding to the next. I. Patient/Practice Partnership Support II. Clinical Care information III. Care Delivery Management IV. Community Resources & Linkages V. Performance Measurement and Improvement VI. Payment & Finance Each category includes a brief description of what is expected of a practice that serves as a Patient Centered Medical Home. There is a checklist that can be used to identify areas where the practice is already successful, and to help identify areas that need improvement. There is also space for you to write notes to remind yourself of what members of the practice team need to do. It is expected that this information can be useful to help you understand what changes will be needed to make your practice a patient centered medical home, and to know whether you are interested in making those changes. *************************************************** I. Patient/Practice Partnership Support Addresses patient access and communication Step 1: Consider the following aspects of care and communication to assess how well your practice performs. Create a practice policy and include this information in a brochure and/or website which incorporates the following: 1. Roles and Responsibilities – Include photos and job descriptions for each practitioner and employee in the practice (nurses, medical assistants, ultrasound techs, receptionists, billing personnel). Describe their roles in the practice and the appropriate contact person for various problems patients may encounter, i.e. who to contact and by what means for prescription refills, appointments, referrals, medical leave forms, billing questions. Does your policy state clearly the roles and responsibilities of patients – for example contacting the pharmacy for prescription refills, showing up for appointments in a timely manner… 2. Appointments – Think through your daily schedule and determine the most patient-centered method for assuring efficiency and on-time appointments in the practice. Can patients expect 2 3. 4. 5. 6. same-day visits for urgent problems? How can patients best communicate their particular needs to front office staff? Having a Personal Clinician – Can women expect a personal clinician in your practice? How do they access their clinician during office hours? What should they do if their provider is unavailable? About Emergencies and Urgent Situations – What are the steps to take for after hour emergencies? For non-emergent issues? Define expectations for your patients and their families regarding practice policies – for example, prescriptions will not be refilled on weekends or after hours in order to ensure patient safety and avoid medication errors. Secure Patient Friendly Communications – Does the practice maintain multiple methods for women to interact with office staff and clinicians? These may include: Phone contact with clear information about when to expect call-backs (is your phone system user-friendly or are there multiple “phone trees” making access time-consuming and difficult) E-mail with stated response times Interactive web communications and feedback time standards/expectations Fax back communications with timely responses Phone or video conference appointments Are there charges associated with any of these methods which may not be covered by current insurance plans? Under a medical home prospective payment all of these services are expected and would be included in the Per Member Per Month (PMPM) payment for medical home. If ACOG Fellows create a medical home as a universal standard for patients, these services may be offered as uncovered but more convenient possibilities for patients. Other Special Services – Describe any other special services provided by the office (e.g. nursemidwifery, advanced practice nursing, genetic counseling, pre-pregnancy visits, lactation consultant, weight management, mental health support) Step 2: Assess how you promote patient access and quality communication within your medical home. Communication Checklist Check the communication standards that your practice currently employs Assignment of patients to a personal provider or consistent clinical care team Coordination of visits with multiple clinicians or multiple tests on the same day (i.e. well-woman care and mammograms, labs, immunizations) Triage process to determine the timing and urgency of visits Schedule patients on the same day that they call – system to assess the urgency of referrals/consultations – abnormal Pap smear versus pelvic pain… Schedule same day appointments using practice triage Schedule same day appointments based upon patient request Offer physician, nurse or other clinical telephone advice during office hours Provide urgent phone advice within a specified time (call back) Physician/provider phone support is available 24/7 Provide secure email consultation with specified hours/response time Offer a web site with all practice information and policies (is it interactive?) 3 Provide language support services for patients with limited English Identify health insurance resources for uninsured patients Note areas and actions for improvement: ************************************************************************ II. Clinical Care information This section addresses standards for practice organization and the use of clinical information. Your practice needs a well-organized medical record with clear documentation of visits, results and referrals. You must be able to document not only that you are providing health assessments for your patients, but also that you are tracking them. In the complete medical home you will be able to provide outreach to patients to optimally manage their health. Outreach projects rely on a complete and integrated medical record. Sources of information for providing preventive care to women ACOG Committee Opinion #452, Primary and Preventive Care: Periodic Assessments, available on the members-only side of the ACOG web site at http://www.acog.org/publications/committee_opinions/co452.cfm The 2009 CDC adult immunization schedule can be found at http://www.cdc.gov/vaccines/recs/schedules/adult-schedule.htm. The HHS webpage on screening and immunizations for women is http://www.womenshealth.gov/prevention See www.guidelines.gov for review of current evidenced based guidelines. On this website, the various guidelines are organized by the organizations submitting the guidelines. ACOG guidelines for screening are included on this website. Step 1: Consider the following standards for the organization of clinical care information. Determine whether your practice has these elements in place for each patient, and each patient visit or contact. This will include obstetric patients, problem focused visits, routine well woman visits, and surgical cases. It must be shown how this information is identified at the time of the routine visit and then tracked so that the testing occurs. Processes must be in place to ascertain whether preventive health strategies and urgent care instructions are followed. An up-to-date problem list with current ICD 9 codes Medical Record: Allergies, Medications, Past Medical History, Past Surgical History, Family History, Social History 4 Periodic Assessment: Nutrition, Physical Activity, Sexual Activity, Use of Complimentary and Alternative Medications, Use of Drug, Alcohol and Tobacco Progress note templates that incorporate American College of Obstetricians and Gynecologists Guidelines BMI with height and weight Blood Pressure Physical Examination: including secondary sexual characteristics, breast exam, pelvic exam, skin exam Preventive Health Screening Strategy: Vaccinations, Cervical Cancer Screen, Colon Cancer Screen, Breast Cancer Screen, Sexually Transmitted Disease Screen, Cholesterol Screen, Contraception Plan, Vitamin Use, Intimate Partner Violence Assessment, Psychosocial Screen, Diabetes Screen, Obstetric Risk Linkage. Urgent Visit Screening: appropriate laboratory and radiological studies After Visit Summary: information from the medical record for patient to keep for her own health tracking purposes Step 2: Develop a patient tracking system in your medical record. The ideal system will allow input of all test results, track results, and allow outreach so that follow up can be arranged. It will allow analysis over time to interpret the impact of health care strategies that you have implemented. Electronic Medical Records can be very effective for helping perform these tasks. Develop patient tracking system Lab tracking for all results (cervical cancer, colon cancer, ultrasound, mammograms and breast abnormalities) Prevention Health Tracking (vaccines, cholesterol, cervical cancer, colon cancer, breast cancer, obstetric ultrasound) Process for tracking tests, referrals and resolution of abnormal results Reproductive life plan in the patient record that reflects patient reproductive choices over time Obstetric linkage between pregnancy, delivery, interconception and subsequent pregnancy Identification of and systematic tracking of quality goals. This will include, when applicable, measures for: Obstetrics care in first trimester Preventive health screen Post partum visit Drug tobacco and alcohol program for at risk patients Preconception health discussion Depression screening Domestic violence screening 5 Note areas and actions for improvement: ************************************************************************ III. Care Delivery Management The practice promotes clinical care that is consistent with your patient’s preference, clinical practice guidelines, and scientific evidence The practice of Obstetrics and Gynecology relies on outpatient preventive health care and urgent care, inpatient and outpatient gynecology, office-based and hospital-based surgical procedures and inpatient obstetrics. This section helps you assess and develop clinical care consistent with scientific research and patient desires. Patient safety is an important element of office-based practices. Identify a safety plan for your office and for office-based procedures. Check the following planned, proactive and comprehensive management strategies your practice currently uses for each patient. Identify the activities or tasks that your practice does. Appointment management: Track requests and availability by types of appointments Availability of same-day appointments Track how long after the requested time patients wait for both for urgent and routine appointments Use historical data to determine the number of appointments needed to meet the demands of your patient panel Have and use a policy for notifying patients of delays or cancellations made by the practice Online access for patient-directed appointment system Patient Communication Strategy: Have in place a means of reminding patients of appointments through the Internet or through phone messages or through the USPS A patient newsletter – either electronic or paper Offer care management for special conditions Receipt of all lab and test results is confirmed All patient communication is documented in the medical record Referral/Consultation: Patients are often referred to specialists in other fields. In the Medical Home, you are providing the core care and consulting with specialists around your patient’s needs. You must be able to document care agreements with these specialists, and show that you are managing the patient’s care. Documented agreements with these colleagues are critical. You must be able to show that there is a tracking system in place for patient management. 6 A method of specifying and documenting expectations (consultation, treatment, transfer of care, etc.) of specialists to whom patients are referred Co-management or collaborative agreements define shared roles with other providers Means of tracking patients who have been referred, including who they are referred to and the results of that referral. It is the responsibility of the Medical Home to ensure that ALL pertinent information about a patient’s condition and care is in the medical record that they maintain, not just information about treatment at the medical home practice Surgery Scheduling: Patients may receive care in surgery centers, in the gynecology service in a hospital, in labor and delivery and in your own office or clinic. It is important to document the process for requesting surgical time, tracking access to care, and providing the care. The date requested by the patient for surgical procedures is tracked and compared to actual date The practice tracks surgery wait times – scheduled vs. actual The practice offers information to patients on surgery preparation The practice provides the patient with information on post operative assessment, so they know what to expect and what to notify the practice about A well defined informed consent process New Patient: As patients enroll in your practice, you need to provide an efficient intake process that includes a system for incorporating their past medical records into your system. There is a simple and efficient means for the patient to provide necessary information needed to enroll at the practice. Providing on-line access is preferred. Enrollment includes intake history The first visit is “seamless”, almost identical to established patients Established policies and procedures for medical record transfer both into and out of the practice Patient Safety Project: You must be able to show that you have effectively initiated and followed a process that does the following: Document patient safety policies and guidelines Provide staff training on those policies and guidelines Provide office based decision tree for triaging patients Note areas and actions for improvement: ********************************************************** 7 IV. Community Resources & Linkages A Patient Centered Medical Home for Women successfully links patients and their families with community resources. The practice maintains a catalogue of accurate, readily available resources for patients and their families. Check the following information to determine which resources your practice provides to your patients and their families. This list is only a suggestion of some useful resources that should be provided; your practice may include additional resources and linkages. Resources & Linkages Checklist Family assistance – maintain and make available to patients a current list of local charity support options for food, housing, utility, clothing, and transportation. Community health resources – make patient aware of resources outside of the practice, such as mental health counseling, women’s shelters, family counseling, and public health clinics Condition specific patient education materials/training within the practice –provide as needed Patient self-management tools/guidance – provide or refer patients for Diabetes Training, Weight Loss, Prenatal Classes, Infant Care, etc Language appropriate services and resources – arrange for interpreter or translation services as needed Home care/respite help – assist patients and their families in locating these services within her community when needed Web based health information – provide patients with easy access to accurate information on health and medical issues that they may be facing. ACOG’s Patient Education pamphlets can be accessed at http://www.acog.org/publications/patient_education. The National Network of Libraries of Medicine offers links to information on a variety of health topics, in English at http://nnlm.gov/outreach/consumer/chweb.html, and in a variety of other languages at http://nnlm.gov/outreach/consumer/multi.html. Note areas and actions for improvement: ********************************************************** V. Performance Measurement and Improvement A Women’s Medical Home a practice must develop methods of measuring performance that can quantitatively measure quality and patient safety. Appropriate measurement may require additional staff resources. If electronic order entry is utilized appropriately, the task can be accomplished more easily with the use of an electronic health record, as most existing software products can generate 8 reports that can summarize care administered or recommended. This allows tracking without extensive logs or chart review. Identifying appropriate quality measurements should be a team effort utilizing administrative, allied professionals and physicians. This QI Team is to be charged with the responsibility of identifying important elements of care, assigning a threshold of acceptance and establishing an effective peer review program. The physician-led QI Team should meet periodically to evaluate identified practice performance measures and communicate corrective action practice recommendation to the appropriate staff. A successful Women’s Medical Home should design and implement quality measurements for important aspects of care provided by all physicians and allied health professionals, using nationally identified quality measurements. Identify the most important measures for your practice. One should not attempt to measure every item of patient care. Doing so creates difficulties in compiling and evaluating data and strains the staffing resources of the medical home. Good sources of guidelines for women’s health care are identified in Part II of this toolkit. Some examples of common measurements of ambulatory care within the women’s medical home are: Documentation of age and risk appropriate screening for sexually transmitted diseases, cervical cancer, colorectal cancer, breast cancer, osteoporosis, lipid disorders, diabetes mellitus. Documentation of appropriate immunizations from review of chart immunization log. Most electronic health records software maintain such logs. Documentation of screening and counseling for life style related disorders such as eating disorders, including obesity, and tobacco abuse as outlined elsewhere in this toolkit. Appropriate prenatal screening, prenatal care, intrapartum, and postpartum care. System of reporting and reviewing medication errors and reactions. System of reporting and evaluation of adverse incidents related to office based surgery. System of reporting oversights in patient notification and follow-up of abnormal laboratory and imaging results. Documentation of physician oversight of clinical management performed by allied health practitioners. System of reporting and evaluation of patient complaints associated with clinical care. The women’s medical home should implement a survey to get the perspective of your patients. The patient survey can be performed periodically in paper format, but can often more easily be performed electronically. By using existing survey software such as www.SurveyMonkey.com , a women’s medical home can use e-mails or website links to solicit feedback on patient satisfaction. The practice should communicate this patient generated performance survey information to physicians and support staff. Electronic surveys allow for tracking performance over time, with benchmarking comparisons of individual clinician and staff performance. Depending on the size of your practice and available resources, you may augment the survey with other methods of generating feedback such as face to face interviews, advisory or focus groups, or formal practice performance consultation. 9 The check list below can serve as a guide as a practice establishes procedures to monitor and improve quality of care and quality of patients’ experiences. Quality Improvement Checklist: Identify the members of the QI team. This will include the lead clinicians in the practice, as well as those who will be responsible for gathering and reporting the results. The size of the team will depend on the size of the practice. Conduct an office patient safety survey to assess the current culture of safety in the practice. A survey for this purpose is available on the AHRQ survey at http://www.ahrq.gov/qual/patientsafetyculture/mosurvindex.htm Develop a practice survey for patients to complete. Conduct survey and analyze the results. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) provides access to a Clinician & Group Survey as well as several documents designed to assist users in administering the survey and analyzing the results. You can also develop your own survey. If you develop your own survey, include questions about their experience getting with the specific services that you offer, such as: Rate the quality of the information you received about childbirth options. Rate the physician’s sensitivity to my concerns about childbirth. Rate access to and timeliness of appointments Identify measures to implement in your QI process. The practice should include tracking appropriate recognized quality measures. The Physician Consortium for Practice Improvement lists their quality measures at http://www.ama-assn.org/ama/pub/physician-resources/clinical-practiceimprovement/clinical-quality.shtml. Develop and use systems to report and track medication errors, adverse incidents related to office surgery, and oversights in patient notification and follow-up of abnormal laboratory and imaging results. Communicate results to physicians and support staff. This will include methods to track practice performance over time. Identify gaps and opportunities to improve. Use the QI team to identify process changes to improve results – for the patient survey, the quality measures, and the practice culture of safety. Repeat the measurements and the process. The QI measures will be continually measured. The patient survey should be conducted periodically, perhaps a couple of times a year or annually. 10 Additional Patient Safety and Quality Improvement Resources A good starting point for finding resources to help with this endeavor is ACOG’s Patient Safety and Quality Improvement web page at http://www.acog.org/departments/dept_web.cfm?recno=28 . A new edition of Quality Improvement in Women’s Health Care is expected by May 2010. Webtreats: These websites, selected by the ACOG resource center, provide valuable suggestions for performance measures, patient safety and quality improvement. Several emphasize safety and performance evaluation in the ambulatory setting http://www.acog.org/departments/dept_notice.cfm?recno=20&bulletin=4226 Patient safety in obstetrics and gynecology ACOG Committee Opinion #286, October 2003 Partnering with Patients to Improve Safety ACOG Committee Opinion #320, November 2005 Safe use of Medication ACOG Committee Opinion #331, April 2006 Guidelines for Women’s Health Care – ACOG, 3rd Edition Guidelines for Prenatal Care –ACOG 6th Edition Note areas and actions for improvement: ********************************************************** VI. Payment & Finance A variety of payment mechanisms may be applied to medical homes. These mechanisms vary according to payer source, geographic location, and the structure of individual medical home models. All are based on achievement of tiered scoring benchmarks, determined by accruing points within each of the required standards. Payment for a specific tier is contingent upon meeting all recognition criteria for that tier. 11 Medical home reimbursement typically blends traditional fee-for-service reimbursement with additional payment methodologies. A model may incorporate all four methodologies, or some combination of one or more: 1) Care coordination payment. These prospective payments are bundled care management fees added onto an existing fee schedule. Payment is made at regular intervals, usually monthly or quarterly, on a per patient basis. This payment would be in addition to fee-for service payments. 2) Fee-for-service (FFS) enhancements. These are not prospective, as the payments link to existing FFS agreements. As in traditional fee-for-service, they are dependent on reporting of services after they are rendered. Examples include direct reimbursement for care coordination CPT codes in lieu of a prospective payment, or additional payment for selected Evaluation & Management (E&M) codes. 3) Performance-based reimbursement. This component is based upon meeting goals for quality and evidence-based practice, and may include specific measures relating to clinical outcomes, patient satisfaction, or cost of care. 4) Practice overhead payment. Reimbursement may be available for practice infrastructure upgrades that are necessary for transformation into a patient-centered medical home. Payment may be made through an upfront “start up,” or as a prospective bundled fee contingent upon ongoing medical home qualification. Unlike older reimbursement models under capitation or “Pay for Performance,” medical home payment models are more comprehensive. The intent is to recognize the true practice transformation that defines a medical home, rather than isolated cost-saving or clinical reporting measures. The degree of financial risk a practice undertakes when transforming to a medical home depends upon: the existing practice structure and infrastructure sophistication; the specific medical home qualification and reimbursement model under consideration; the degree to which individual parameters under the medical home model are amenable to negotiation; and commitment of practice members to achieve and maintain medical home qualification. Checklist for Medical Home Payment and Finance. Do the following: Determine whether there are active medical home models or demonstration projects in your area. Assess degree to which existing practice characteristics meet medical home requirements Assess reimbursement mechanisms available within local MH models Assess current practice fixed and variable costs. Determine current patient demographics, acuity, and volume, and payer mix. Assess existing IT resources in the practice. What is needed to meet Medical Home requirements vs. what you currently have. Determine the incremental costs and financial benefits of transformation to a medical home? Use these methods: Net present value Opportunity cost 12 Note areas and actions for improvement: ********************************************************** Conclusion Congratulations for completing the practice assessment. It is expected that this information will help your practice determine whether you want to make the changes that will be required to transform into a Patient Centered Medical Home. Such a transformation requires a continuous team effort, with commitment of everyone in the practice, including physician and non-physician staff, patients, and their families. 13