Online Figure 1 Flow diagram of the selection process according to
advertisement

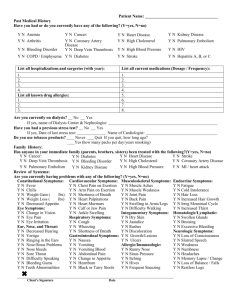
Online Figure 1 Flow diagram of the selection process according to the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) statement. Online Figure 2 Publication bias assessment for 30-day outcomes. Online Figure 3 Individual and summary odds ratios with 95% confidence intervals (CI) for 30-day ischemia-driven revascularization in ACS patients treated with bivalirudin vs heparins stratified by protocol use of GP inhibitors. ACUITY, Acute Catheterization and Urgent Intervention Triage Strategy trial; BRIGHT, Bivalirudin versus Heparin Monotherapy and Glycoprotein IIb/IIIa Plus Heparin for Patients with AMI Undergoing Coronary Stenting; HORIZONS-AMI, Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction Trial; ISAR-REACT 4, Intracoronary Stenting and Antithrombotic Regimen: Rapid Early Action for Coronary Treatment 4; REPLACE-2, the Randomized Evaluation of PCI Linking Angiomax to Reduced Clinical Events-2; BAT, Bivalirudin Angioplasty Trial (aka. HAS, Hirulog Angioplasty Study); BRAVE-4, The Bavarian Reperfusion Alternatives Evaluation 4 Trial; EUROMAX, European Ambulance Acute Coronary Syndrome Angiography HEAT-PPCI, How Effective are Antithrombotic Therapies in Primary PCI; M-H, Mantel-Haenszel method. Online Table 1. Outcomes definitions Study ACUITY* ARMYDA-7-BIVALVE BRAVE-4* Major bleeding (1) Intracranial or intraocular bleeding unrelated to CABG; (2) Haemorrhage at the access site requiring intervention; (3) Access site haematoma Ø ≥5 cm; (4) Any decrease in the haemoglobin level of ≥4 g/dl; (5) Overt bleeding with a decrease in the haemoglobin level ≥3 g/dl; (6) Reoperation for bleeding; (7) Transfusion. (1) Intracranial bleeding; (2) Overt bleeding with a decrease in the haemoglobin level ≥5 g/dl; (3) TIMI major bleeding. HORIZONS-AMI definition: (1) Intracranial or intraocular bleeding; (2) Access site haematoma Ø ≥5 cm or requiring intervention (3) Any decrease in the haemoglobin level of ≥4 g/dl; (4) Overt bleeding with a decrease in the haemoglobin level ≥3 g/dl; (5) Reoperation for bleeding; (6) Transfusion. BRIGHT Type 3 or 5 bleeding as per BARC definitions † EUROMAX* (1) Intracranial, retroperitoneal, or intraocular bleeding unrelated to CABG surgery; (2) Access-site haemorrhage requiring radiologic or surgical intervention; (3) Any decrease in the hemoglobin level of ≥4 g/dl (4) Overt bleeding with a decrease in the hemoglobin level ≥3 g/dl; (5) Reintervention for bleeding; (6) Transfusion. Type 3-5 bleeding as per BARC definitions † (1) Intracranial or intraocular bleeding; (2) Access site hematoma Ø ≥5 cm or requiring intervention; (3) Any decrease in the haemoglobin level of ≥4 g/dl; (4) Overt bleeding with a decrease in the haemoglobin level ≥3 g/dl; (5) Reoperation for bleeding; (6) Transfusion. REPLACE 2 definition: (1) Retroperitoneal, intraocular, or intracranial haemorrhage; (2) Any decrease in the haemoglobin level of ≥4 g/dl; (3) Overt bleeding with a decrease in the haemoglobin level ≥3 g/dl; (4) Blood transfusion (≥2 units of packed red blood cells or whole blood). REPLACE 2 definition: (1) Retroperitoneal, intraocular, or intracranial haemorrhage; (2) Any decrease in the haemoglobin level of ≥4 g/dl; (3) Overt bleeding with a decrease in the haemoglobin level ≥3 g/dl; (4) Blood transfusion (≥2 units of packed red blood cells or whole blood). TIMI major bleeding. NA REPLACE 2 definition: (1) Retroperitoneal, intraocular, or intracranial haemorrhage; (2) Any decrease in the haemoglobin level of ≥4 g/dl; (3) Overt bleeding with a decrease in the haemoglobin level ≥3 g/dl; (4) Blood transfusion (≥2 units of packed red blood cells or whole blood). (1) Retroperitoneal, or intracranial haemorrhage; (2) Overt bleeding with a decrease in the haemoglobin level ≥3 g/dl; (3) Transfusion of ≥3 units of blood. HEAT-PPCI HORIZONS-AMI* ISAR-REACT 3 ISAR-REACT 4* PROTECT-TIMI 30* Ray et al. REPLACE-2* TIMI-8 NACE Composite of: (1) All-cause death; (2) MI; (3) Unplanned revascularization for ischemia; (4) Major bleeding. NA Composite of: (1) All-cause death; (2) Recurrent MI; (3) Unplanned revascularization of the infarct related artery; (4) Definite ST; (5) Stroke; (6) Major bleeding Composite of: (1) All-cause death; (2) Re-infarction; (3) TVR; (4) Ischemic stroke. (5) Bleeding events. Composite of: (1) Death; (2) Re-infarction; (3) Ischemia-driven revascularization; (4) Stroke. (5) Non-CABG major bleeding. NA Composite of: (1) All-cause death; (2) MI; (3) Unplanned revascularisation for ischemia; (4) Non-CABG major bleeding. Composite of: (1) All-cause death; (2) MI; (3) Urgent TVR; (4) In-hospital major bleeding. Composite of: (1) All-cause death; (2) Large recurrent MI; (3) Urgent TVR; (4) Major bleeding. NA NA Composite of: (1) All-cause death; (2) MI; (3) Urgent repeat revascularization; (4) Major bleeding. Composite of: (1) All-cause death; (2) Nonfatal recurrent MI; (3) Major haemorrhage. * studies assessing separate major bleeding outcome according to the criteria of the Thrombolysis in Myocardial Infarction (TIMI) study group: (1) intracranial, or (2) clinically significant overt signs of hemorrhage associated with a drop in hemoglobin of > 5 g/dL (or, when hemoglobin is not available, an absolute drop in hematocrit of > 15%; (3) if CABG related: fatal bleeding or perioperative intracranial bleeding or reoperation following closure of the sternotomy incision for the purpose of controlling bleeding or transfusion of > 5 units of whole blood or PRBCs within a 48 hour period (cell saver transfusion will not be counted in calculations of blood products) or chest tube output > 2 L within a 24 hour period. † The Bleeding Academic Research Consortium (BARC): Type 0: no bleeding; Type 1: bleeding without need for hospitalization or treatment; Type 2: bleeding requiring diagnostic studies, hospitalization, or treatment by a healthcare professional; Type 3a: bleeding includes any transfusion with overt bleeding and overt bleeding plus a hemoglobin drop of ≥3 to <5 g/dL (provided the hemoglobin drop is related to bleeding); Type 3b: bleeding includes overt bleeding plus a hemoglobin drop of ≥5 g/dL (provided the hemoglobin drop is related to bleeding), cardiac tamponade, bleeding requiring surgical intervention for control (excluding dental/nasal/skin/hemorrhoid), and bleeding requiring intravenous vasoactive drugs; Type 3c: bleeding includes intracranial hemorrhage and intraocular bleeding compromising vision; Type 4: bleeding is coronary artery bypass grafting (CABG)–related (within 48 hours); Type 5: fatal bleeding. MACE, major adverse cardiac events; NACE, net adverse clinical events; ACUITY, Acute Catheterization and Urgent Intervention Triage Strategy trial; CABG, coronary artery by-pass grafting; MI, myocardial infarction; ARMYDA-7-BIVALVE, Anti-Thrombotic Strategy for Reduction of Myocardial Damage During Angioplasty–Bivalirudin vs Heparin Study; TVR, target vessel revascularisation; ST, stent thrombosis; BRAVE-4, The Bavarian Reperfusion Alternatives Evaluation 4; HORIZONS-AMI, Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction Trial; BRIGHT, Bivalirudin versus Heparin Monotherapy and Glycoprotein IIb/IIIa Plus Heparin for Patients with AMI Undergoing Coronary Stenting; EUROMAX, European Ambulance Acute Coronary Syndrome Angiography; HEAT-PPCI, How Effective are Antithrombotic Therapies in Primary PCI; ISAR-REACT 3, Intracoronary Stenting and Antithrombotic Regimen: Rapid Early Action for Coronary Treatment 3; REPLACE-2, the Randomized Evaluation of PCI Linking Angiomax to Reduced Clinical Events-2; PCI, percutaneous coronary intervention; ISAR-REACT 4, Intracoronary Stenting and Antithrombotic Regimen: Rapid Early Action for Coronary Treatment 4; PROTECT-TIMI 30, A Randomized Trial to Evaluate the Relative Protection Against Post-Percutaneous Coronary Intervention Microvascular Dysfunction, Ischemia, and Inflammation Among Antiplatelet and Antithrombotic Agents-Thrombolysis in Myocardial Infarction 30; TIMI-8, The Thrombolysis in Myocardial Infarction 8 Trial; NA, not assessed. Online Table 2. Bias assessment Table 2. Risk of bias of included randomized controlled trials. STUDY MULTICENTER ADEQUATE ALLOCATION TRIAL SEQUENCE CONCEALMENT GENERATION ACUITY Y Y N ARMYDA-7Y Y UNCLEAR BIVALVE BRAVE-4 Y UNCLEAR, 1:1 N BRIGHT Y UNCLEAR, 1:1:1 N EUROMAX Y Y, 1:1 N HEAT-PPCI N UNCLEAR UNCLEAR HORIZONSY Y, 1:1 UNCLEAR AMI ISAR-REACT 3 Y Y Y ISAR-REACT 4 Y Y Y PROTECT-TIMI Y Y, 1:1:1 N 30 RAY MJ ET AL. N UNCLEAR UNCLEAR REPLACE-2 Y Y Y TIMI-8 Y UNCLEAR UNCLEAR PATIENT BLINDING PHYSICIAN BLINDING N N N N ADJUDICATION OF OUTCOMES BLINDING Y Y INCOMPLETE DATA OUTCOME ADDRESSED? SELECTIVE OUTCOME REPORTING FREE OF OTHER BIAS N N N N N N N N N N Y UNCLEAR Y Y Y UNCLEAR Y Y Y Y UNCLEAR N N N N Y Y Y Y Y Y Y N Y Y N Y Y Y Y Y Y N N N Y Y Y N Y Y N Y Y UNCLEAR Y Y Y Y Y N N N Y Y Y Y Y N N Y Y