Toxic Alcohols - CriticalCareMedicine
advertisement

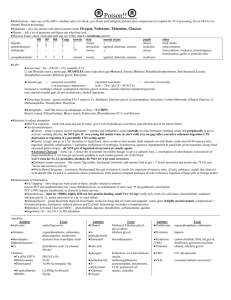
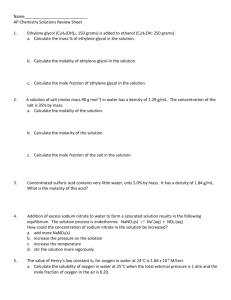
Chapter 153 – Toxic Alcohols Methanol Sources: antifreeze, windshield wiper fluid, carburetor fluid, sterno, glass cleaner, paint thinner Toxic Dose: 0.15 cc/kg of 100% methanol Pharmacology Absorption: Rapidy absorbed with peak levels 30-60 minutes postingestion. Volatile at room air → inhalational toxicity Metabolism: ◦ Metabolized by alcohol dehydrogenase to formaldehyde, which is metabolized to formic acid by aldehyde dehydrogenase. ◦ ADH metabolism is 1st order at lower levels and zero order at higher levels, resulting in prolonged ↑ methanol levels with larger ingestions ◦ Ethanol has higher affinity for alcohol dehydrogenase than methanol, so metabolism is delayed ◦ Formic acid is metabolized to CO2 + H2O through a folatedependent pathway Elimination: Small amount excreted in the lungs Pathophysiology Methanol → irritation of the gastric mucosa Formic acid: ◦ Optic neuropathy: Muller cells (glial cells) in the retina metabolize methanol to formic acid. The formic acid disrupts cellular metabolism → calcium influx, microtubule dysfunction and mitochrondial dysfunction. ◦ Putaminal necrosis: Postulated similar mechanism as optic Methanol metabolism neuropathy ◦ Iron binding: Formic acid binds to Fe → cytochrome dysfunction with ↑ anaerobic respiration (↑ lactate) ◦ Non-specific cellular injury: lipid peroxidation, ↑ free radicles, ↓ antioxidant reactions Clinical Presentation Symptom onset: Low affinity for ADH → latent period of 12 – 24 hrs. ↑ if EtOH co-ingestion, ↓ if lg ingestions. Early symptoms: ◦ CNS ↓ LOC, confusion, ataxia ◦ HEENT Visual disturbances (central scotoma, snowstorm blindness), disc edema, RAPD ◦ GI AP, vomiting Late symptoms: ◦ CNS Seizures, coma ◦ Resp Tachypnea ◦ Metab Metabolic acidosis Ethylene Glycol Sources: de-icing fluid, brake fluid, coolant, antifreeze Toxic Dose: 0.2 cc/kg of 100% ethylene glycol Pharmacology Absorption: Rapidly absorbed when ingested with peak levels 1-4 hrs post-ingestion Distribution: Lg Vd (like water) Metabolism/Elimination ◦ 25% excreted unchanged by kidneys ◦ ◦ Remainder is converted to glycoaldehyde, which is then converted to glycolic acid by aldehyde dehydrogenase. Glycolic acid is metabolized to glyoxylic acid, which is then broken down into: ▪ Glycine (cofactor pyridoxine) ▪ Oxalic acid ▪ α hydroxy β ketoadipate (cofactor Mg2+ and thaimine) Pathophysiology Glycolic acid, glyoxylic acid and glycoaldehyde cause nephrotoxicity (ATN) Oxalic acids forms crystals with Ca2+ → involvement of various systems: ◦ GU: Crystal nephropathy ◦ CNS: Deposition of crystals in parenchyma, BVs → punctate hemorrhage, edema and aseptic meningoencephalitis ◦ HEENT: Deposition of crystals in retina → visual changes ◦ MSK: Crystal deposition → myonecrosis Glycolic acid → anion gap metabolic acidosis Inhibition of citric acid cycle → ↑ lactate (mild contribution to acidosis) Clinical Presentation Acute Neurologic Stage (30 min – 12 hrs) ◦ CNS ataxia, confusion, nystagmus ◦ GI emesis, AP Cardiopulmonary Stage (12-24 hrs) ◦ CVS tachycardia, myocardial depression (hypotension) ◦ Resp tachypnea (d/t acidosis + ARDS) ◦ Metab ↓ Ca2+ d/t binding with oxalic acid ◦ MSK myositis → rhabodomyolysis Renal Stage (24 – 72 hrs) ◦ GU AKI d/t ATN +/- pigment nephropathy, crystal nephropathy Delayed Neurologic Sequelae Stage (6 – 12 days) ◦ CNS Cranial neuropathy is most common, but other abnormalities can occur (varying severity) Diagnosis Osmolar Gap (Normal < 10 mmol/L) Alcohols → freezing point depression Calculated osmoles = Na x 2 + glucose + BUN To estimate the contribution by ethanol, multiply the alcohol level x 1.25 – always check EtOH level. Causes of ↑ OG: ◦ ◦ ◦ ◦ ◦ ◦ OG Alcohols: ethanol, ethlyene glycol, methanol, isopropyl alcohol, propylene glycol Sepsis & MODS Ketotic states: AKA, DKA, SKA Hyperlipidemia Hyperproteinemia Osmotic diuretics ↓'s as toxic alcohol is metabolized Anion Gap (Normal < 14) AG = Na – (Cl + HCO3-) Causes of ↑ anion gap Congenital: Inborne errors of metabolism Acquired: ◦ Ketones: DKA, SKA, AKA ◦ Uremia: renal failure ◦ Lactate: ▪ ↑ lactate production: hypoperfusion, cellular toxins (Fe, CO, CN, H2S), hypermetabolic states (seizures, hyperthermia), toluene ▪ ◦ ↓ lactate metabolism: liver disease, metformin Toxins: toxic alcohols, ASA, paradehyde Toxic Alcohol Levels Measures level of parent compound, not metabolite, so may be falsely low if presenting late Urinalysis Presence of crystals (calcium oxalate crystals) is suggestive of ethylene glycol toxicity (occurs in < 50%) Urinary fluorescence: Antifreeze additive may appear in urine, but high rate of false positive and false negatives EKG ↑ QTc may be d/t hypocalcemia with ethylene glycol poisoning Management ABC's: Standard ACLS. Check chemstrip (especially in children). Decontamination: Not effective d/t rapid absorption + dangerous d/t ↓ LOC Specific Therapy: Sodium Bicarbonate: Toxic products are weak acids so normalization of serum pH → ↑ ionized form of acids, which do not cross physiologic membranes (ion trapping). Indicated when serum pH < 7.3 ◦ Methanol: trapping of formate in the serum (↓ cellular uptake) + trapping of formate in urine (↑ excretion) ◦ Ethylene glycol: trapping of glycolate in the urine (↑ excretion) Ethanol: Competitively inhibits alcohol dehydrogenase, which a much greater binding affinity then either methanol or ethylene glycol. ADH blockade → very slow metabolism of toxic alcohols by other means. ◦ Dosing: ▪ Loading dose is 0.8 g/kg (For PO: Proof = percent EtOH x 2) ▪ Maintenance dose: Non-drinker: 0.6 – 1.5 cc/kg/hr (10% EtOH) Drinker: 1.5 – 2 cc/kg/hr Hemodialysis: 3 – 5 cc/kg/hr ◦ Target level: Serum EtOH > 100 mg/dL ◦ Complications: hypoglycemia, volume overload, ↓ LOC Fomepizole: Long acting competitive inhibitor of alcohol dehydrogenase ◦ Indications: ▪ History: Known ingestion ▪ Dosing: Given q12 h x 4 doses Adjunctive Treatments: Goal to shunt metabolism of toxic alcohols down less ◦ Ethylene glycol: vitamin B6, thiamine ◦ Methanol: folate or folinic acid (leukovorin) Dialysis: Indications for dialysis: ◦ Absolute levels: Methanol > 15 mmol/L or ethylene glycol > 8 mmol/L ◦ Hemodynamic instability ◦ Metabolic acidosis (pH < 7.25) that is refractory to treatment ◦ Electrolyte imbalance not responsive to conventional therapy ◦ End-organ toxicitiy: ▪ Renal impairment ▪ Coma or severe obtundation ▪ Visual abnormalities Isopropanol Sources: rubbing alcohol, de-icer, solvents Toxic Dose: 2-4 cc/kg of 100% isopropanol Indications for Antidotal Therapy Recent ingestion with OG > 10 Methanol level > 15 mmol/L and ethylene glycol level > 8 mmol/L Strong clinical suspicion + 2 of pH < 7.3, HCO3- < 20, OG > 10 and/or oxlate crystals in urine toxic pathways by providing substrate Pharmacokinetics Absorption: rapidly absorbed Metabolism/Elimination ◦ Hepatic metabolism to acetone by alcohol dehydrogenase. T1/2 of acetone is 20 hrs. T1/2 of isopropanol is 3-7 hrs (shorter in children) ◦ 20% excreted unchanged in the urine Clinical Presentation Early CN confusion, altered LOC, ataxia GI gastritis (may be significant) Late CNS CVS GU MSK Metab ↓ LOC, coma hypotension (with lg ingestions) renal failure d/t ATN (rare) atraumatic rhabomyolysis Ketosis without acidosis (isopropanol → acetone) Investigations Typical laboratory findings are an elevated osmol gap without acidosis. False ↑ creatinine can occur b/c of cross-reactivity with acetone. Watch for hypoglycemia, especially in children. Management Generally supportive – no role for ethanol or fomepizole IHD indicated if refractory hypotension (rare) or level > 400 mg/dL Benzyl Alcohol Sources: preservative in bacteriostatic NS and other IV medications Pharmacokinetics: Metabolized to benzoic acid Clinical Presentation: Neonates with excessive doses develop gasping baby syndrome: ↓ LOC, hypotension, metabolic acidosis, gasping respirations, hepatic & renal failure → MODS → death Glycol Ethers Sources: brake fluids, solvents Pathophysiology: May be metabolized to ethylene glycol, particularly in significant overdoses Management: As for ethylene glycol Propylene Glycol Sources: dilutent for many drugs (dilantin, diazepam), anti-freeze Pathophysiology: Metabolized to lactate and pyruvate → anion gap metabolic acidosis Clinical Presentation: May cause hypotension (cause of hypotension with IV dilantin) Management: Supportive Diethylene Glycol Sources: power steering fluid, brake fluid Pathophysiology: Parent compound → renal failure (cortical necrosis) Metabolized to hydroxyethoxy acetic acid, which can cause an anion gap metabolic acidosis Management: Hemodialysis