Eating Disorders Outline
advertisement
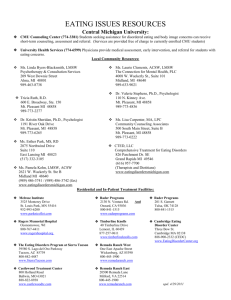
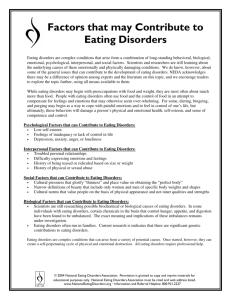
Eating Disorders Outline AN = the pursuit of thinness; phobic response to the fear of eating. This results in a dramatic restriction of food intake. Also referred to the “weight-gain phobia”. What the eating behavior looks like. Mood issues related to AN. Appetite Issues. Subtypes of AN: restricting subtype (limits food intake but does not engage in binge eating or purging (e.g. self-inducted vomiting, or misuse of laxatives, diuretics, or enemas); and bingeeating/purging subtype. BN = dyscontrol over eating. normal-weight or overweight individuals who display followed by compensatory behavior. recurrent eating binges Sense of loss of control Feelings of shame, anxiety, depression Self-damaging behavior AN and BN – related to compulsive dieting? Polivy and Herman (1993). Evidence for this? Other Eating syndromes: EDNOS; binge eating disorder (BED). The Restricter/Binger Distinction History of AN and BN Thomas Morton cases in 1689 Marce and simultaneous reports of Sir William Gull and Charles Lasegue (1860). Gull = introduction of the term AN. Marce = “hypochondriacal delirium” and Lasegue = “hysteria”. 1970s BN is introduced. “bulimos” Epidemiology Eating Disorders Outline Prevalence of AN in Western school-aged females .5 to 1%. BN 1-2%. In subthreshold forms, diagnosed using less-stringent criteria. BN develops later than AN, during the transition to adulthood. Rare in males – 1/10th as common in men as women. Racial issues. Incidence went from 0.35 to 4.06 per 100,000 Stereotypes Comorbidity: affective, anxiety, substance-abuse, and personality disorders. 25-50% AN = concurrent major depression 50-75% will suffer depression sometime in their lifetime Binge/purge syndromes = similar rates. BN 41% of bulimics are clinically depressed. Other reports talk about concurrent and lifetime rates of depression to be 20 and 38%, respectively. Garfield (1995) Major depression across restricter and binger/purger anorexics to be 30% for restricters and 53% for bingers/purgers. 69% of BN were noted to show signs of comorbid seasonal affective disorder. 25% of those with SAD also have ED, most often BN. Why the overlap? Anxiety Disorders: AN = 20% to 75%. In BN, 13-60%. The specific disorders include GAD, social and simple phobias, agoraphobia, panic disorder, and esp. OCD. The structure of the EDs resemble OCD Lifetime prevalence of OCD in ED women – 15-70% in AN and 10=-30% in BN. Substance-abuse disorders 10-55% of BN patients = abuse substances. 25-40% of female alcoholics show some form of ED Why the overlap? Holderness et al (1994) Eating Disorders Outline Dissociative disorders Personality Disorders Retrospective studies looking at premorbid personality in ED sufferers = “soft” evidence Rastam (1992) Etiology: multidimensional Sociocultural context Gardner and Garfinkel (1980) Lee, Ho, and Hsu (1993) Biological Factors: Genetics: (Strober et al, 1990). Twin data: Treasure and Holland (1995) Temperamental Traits: Strober (1991) Humphrey (1991) Neurobiology: 1) Norepinephrine 2) Cholecystokinin (CCK) 3) Serotonin Neuropsychology Psychological and Developmental Factors: Individual Psychological Features Bruch (1973) Crisp (1980) Psychometric findings on ED Problems with impulsivity Eating Disorders Outline Newton and colleagues (1993) Body-Image Disturbances Dietary Restraint Polivy, Herman and others Heatherton and Baumeister (1991 Family Factors: Family Dynamics Palazolli (1978 Family models of BN Johnson (1991) Humphrey (1991) Sexual Trauma An example of an integrative model