Oral Health Promotion Strategic Plan 2012-2017
advertisement

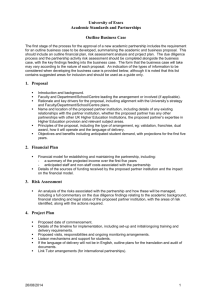
Oral Health Promotion Strategic Plan 2012-2017 1 Evidence Based OHST Capacity Whole of Life Advocacy Oral Health Services Tasmania Advocate for oral health integration in all policies, legislation, health plans, settings and programs Oral Health Promotion Strategic Plan 2012 to 2017 Continue to support water fluoridation for all reticulated water supplies Promote fluoride and preventive strategies across whole of life Facilitate a population health approach with enhanced health literacy Ensure all state wide resources are developed using consistent evidence based messages Vision ‘Improving Quality of Life through Oral Health Care’ Identify local oral health champions Build the capacity of the workforce Identify, develop and implement economic and consistent statewide programs Build health intelligence Mission Maximise access to quality; client centred oral health services for those clients who have the greatest need of our care Partnerships Provide best practice oral Promote and integrate oral health into all appropriate partnerships, settings and opportunities health programs to empower individuals and communities to manage their own quality of life through good oral health o Advocate: Oral health as an integral part of general health o Promote a whole of life approach o Increase the capacity of OHST to meet changing needs o Use evidence based programs to deliver effective, efficient and outcome focused interventions o Build sustainable partnerships Emphasise a population health approach 2 ORAL HEALTH SERVICES TASMANIA - Improving Quality of Life through Oral Health Care o o Maximise access to quality; client centred oral health services for those clients who have the greatest need of our care. Provide best practice oral health programs to empower individuals and communities to manage their own quality of life through good oral health ORAL HEALTH PROMOTION STRATEGIC PLAN 2012-2017 Oral Health Services Tasmania (OHST) has developed a health promotion strategy that is underpinned by the Australian National Oral Health Plan 2004 -2013 (ANOH) which recognises the need for: Oral health to be seen as an integral part of general health A population health approach, with a strong focus on promoting health and the prevention and early identification of oral disease Access to appropriate and affordable services – health promotion, prevention and early intervention and treatment Education to achieve a sufficient and appropriately skilled workforce, and communities that effectively support and promote oral health Address oral health inequities for the most vulnerable communities The Oral Health Services Tasmania (OHST) health promotion plan will complement and support the care that OHST provides and will initially target pregnant women, young children and families within the community. Disadvantaged, indigenous and other special needs groups within the community will be addressed in stage two, with considered relevance to the needs of the Tasmanian population and individuals both geographically and economically. The plan provides a coordinated, equitable, and supporting structure for the state of Tasmania that will work towards: Empowering all Tasmanians, especially the most vulnerable to be active partners in managing their own oral health and wellbeing. The OHST Health Promotion Plan will use the five fundamental principles of the Ottawa Charter to guide health promotion planning and action for the Tasmanian community: Build healthy public policy; create supportive environments; strengthen community action; develop personal skills; and reorient health services. The plan will also use a population health and targeted approach to: Use evidence-based practice and information to guide programs Understand the determinants of health and how they affect health outcomes and behaviour Address Inequities: maximise access to quality client centred oral health services for those patients who have the greatest need of our care; Utilise partnerships and alliances across all areas both local and state Encourage action across the continuum: Individual to system change Respond to cultural change and integrate oral health promotion into practice and service Support environments where healthy choices are encouraged Encourage community participation and engagement The OHST Health Promotion Plan is informed by the Tasmanian Department of Health and Human Services (DHHS) Strategic Directions 2009-2012, OHST Business Plan (2011-12), DHHS Working in Health Promoting Ways Strategic Framework, DHHS A Healthy Tasmania, 2011 Victorian Evidence Based Oral Health Promotion Resource and the NSW Oral Health Promotion Framework for Action 2010. 3 Background Oral health is fundamental to overall health, wellbeing and quality of life. A healthy mouth enables people to eat, speak, seek employment and socialise without pain, discomfort or embarrassment which increases their quality of life. Dental disease, although almost entirely preventable, is the second most costly diet-related disease in Australia and the economic impact is comparable with that of recognised common chronic diseases including heart disease and diabetes.1 Oral health is closely linked to general health and directly impacts on the well being of the individual and the community. Oral health shares many common risk factors with a range of chronic conditions such as cancer, diabetes and cardiovascular disease. 2 Disadvantaged groups in the population are known to experience the impacts of oral disease more frequently,3 and research shows that oral disease is strongly associated with socio economic status. 4 It is the poor and disadvantaged in the community that can least afford to access services and experience opportunities to change. In comparison to other Australian states, Tasmanian people are less well off, have the highest unemployment rates and highest average age, a high incidence of chronic disease, smoke more, highest age, have lower formal education and health literacy levels and the lowest average weekly full time ordinary earnings in all of the states and territories.5 Many factors cause oral disease. Determinants such as diet and hygiene, smoking, alcohol, income distribution, education, employment status, cultural beliefs, housing, personal health practices, and access to services and interventions6 all affect the opportunities and overall health and wellbeing of the community. Promoting oral health is not just about treating the disease, but understanding and promoting the overall health of the community, and addressing inequalities in oral health.7 Early childhood is the time when most lifetime habits are established. It offers the greatest opportunity for prevention of disease, which in turn, can contribute to better health in adulthood. 8 Nearly 52% of Tasmanian children aged 5-6years of age and 53.4% of 12 year old have some experience of dental decay.9 Research has shown that high levels of dental caries in childhood and social differences in access to oral care in children under five predicts greater oral disease in adulthood.10 11 Evidence also indicates that good oral health behaviours attained in early years will translate to good oral health outcomes and behaviours in adult life.12 There are significant and persistent high levels of oral disease among Australian adults with over 25 percent of adults having untreated decay.13 Periodontal disease is the fifth most prevalent health problem in Australia, with higher prevalence in lower socio economic groups.14 Over 670 Australians die of oral cancer each year.15 Tasmania has the lowest national clinical dental workforce capacity16 and with continuing economic restraints it is important that a more strategic and integrated partnership approach to early intervention and preventive initiatives be implemented that will more effectively address the causes of poor oral health, rather than continuing to address the symptoms in isolation. Current evidence suggests that good oral health outcomes occur when oral health preventive action and evidence based health promotion initiatives occur throughout people’s lives, starting from the prenatal and early childhood period, with emphasis on disadvantaged, indigenous and other special needs groups within the community. 4 Oral Health Promotion Strategic Plan 2012-2017 1. Improve awareness that oral health is an integral part of general health and wellbeing throughout the whole of life. Objectives 1.1 Advocate and ensure that oral health is integrated in health plans, policies legislations, programs and settings at all levels Strategies Establish and maintain relevant partnerships across and within all levels of government, health care providers, community sector groups, other agencies and communities to ensure oral health is integrated and included in all appropriate health plans, policies and curriculums. Encourage all OHST staff to improve advocacy opportunities for oral health in their everyday relationships. Ensure that OHST supports and promotes legislation, regulation and setting- based strategies. 1.2 Continue to support water fluoridation for all reticulated water supplies Maintain representation and advocacy for Tasmanian water fluoridation Support and promote water fluoridation Provide latest research on water fluoridation and topical fluoride to general health workers and OHST workforce Provide consistent evidence based fluoride messages to all the population Promote drinking tap water 2. Promote oral health using a whole of life approach, targeting groups most at risk Objectives Strategies 2.1 2.2 Promote fluoride and preventive strategies across the whole of life Facilitate a population health approach and enhanced health literacy Provide and support evidence based whole of life programs that will promote and embed the accepted message of twice daily brushing with appropriate fluoride tooth paste, spit out but don’t rinse to the individual and the whole community. Develop appropriate and consistent clinical protocols for use at the chair side. Promote and support clinical and evidence based information for all preventive and minimal interventions. Provide information across the population Develop linkages with groups that address the underlying and shared risk factors such as cancer, cardiovascular disease, diabetes and smoking. Consider and support multi-sectoral partnerships, environments and approaches that address the underlying determinants of oral health. Expand and/or implement early intervention and prevention programs. Utilise peer group initiatives. 5 Objectives Strategies 2.3 Ensure all state wide resources are developed using consistent evidence based messages Develop or rebrand resources which are supportive of evidence based programs and that are considerate of health literacy guidelines. Develop a simple suite of evidence based oral health messages that will be aligned with the national oral health messages. Encourage use of consistent, state wide resources to build a coordinated approach to marketing. 2.4.1 Pregnant women in the home and health care settings Develop appropriate partnerships and a program with health care providers and organisations to improve the oral health of pregnant women in the home and in the health care setting. Improve care coordination for pregnant women with chronic disease and high risk complex care. Develop appropriate communication strategies for working with pregnant women. 2.4.2 Infants and Preschool Children and their parents Integrate oral health issues and messages into state wide early childhood policies and programs. Develop and maintain appropriate programs with early childhood individuals, families, targeted communities and organisations. Develop targeted strategies for high risk children. 2.4.3 School aged children and families Develop and support appropriate settings based approaches and partnerships within education, sporting, youth and community organisations. Develop appropriate communication strategies for working with school aged children and their parents at the chair side Support school based and settings approach programs that link to the home environment, use peer leaders and target high risk children and families 2.4.4 Adolescents and Young adults 2.4.5 Older adults in the home and residential settings 2.4.7 Aboriginal and Torres Strait Islander people Integrate oral health issues into state wide youth policy. Develop appropriate partnerships with education, sporting, youth and health individuals and organisations to improve the oral health outcomes in these settings. Develop oral health information in consultation with young adults. Develop an appropriate communication strategy for use at the chair side. Develop and expand on programs that focus on the oral health risk factors of the older adult in the community and in residential care. Support and advocate for the expansion of the Better Oral Health in Residential Care Project. Continue to encourage and support training of aged care workers and appointing oral care champions for older people in residential care, with a focus on individualised oral health care plans. Develop an appropriate communication strategy for chair side intervention. Support aboriginal health workers and staff to become oral health champions. Support and develop programs in partnership with the indigenous community. 6 2.4.8 2.4.9 People from culturally and linguistically diverse populations Integrate oral health issues into state wide policy for people from a culturally and linguistically diverse (CALD) background, in particular refugees Build significant relationships with people from a CALD background and with organisations that support them. Provide culturally appropriate oral health information, in consultation with the community. People with special needs Support health and welfare workers and carers to be oral health champions. Build and sustain appropriate partnerships. Investigate developed resource and programs for people with special needs. Develop appropriate communication strategies for working with people with disabilities. Develop appropriate partnerships to improve the oral health outcomes in special needs settings. 3. Increase the capacity of OHST to meet changing needs. Objectives Strategies 3.1 Identify local oral health champions to: 3.2 Build the capacity of the workforce to utilise all opportunities for oral health interventions and advocacy Work within a coordinated and consistent state wide team framework. Identify appropriate community programs, based on local needs and inequities. Encourage a team based approach to oral health, building on strengths and capabilities within the team. Build and encourage appropriate local partnerships and stakeholder networks to identify and provide capacity building for oral health promoters in the community. Analyse local health data, community profiles and identify target population groups. Promote relationship building within local communities with general health providers. Focus on prevention and early intervention and the importance of engagement with marginalised families and populations. Provide training in motivational interviewing, anticipatory guidance and nutrition updates to build capacity. Provide supportive, consistent information and programs for individual and community health promotion interventions. Provide training for all Oral Health Services Tasmania (OHST) staff of the ‘determinants of health’ impact on service access and oral health outcomes for our most vulnerable groups. To empower individuals and the community to participate in decisions about their oral health. Provide appropriate training and access to evidence based research, guidelines and programs. 7 4. Use evidence based programs to deliver the most effective, efficient and outcome focused interventions. Objectives Strategies 4.1 Identify, develop and implement economic and consistent state wide programs. Select and prioritise appropriate programs and strategies. Support the findings of the National Consensus suite of evidence based messages. Build evaluation into all stages of interventions to build and expand evidence base. 4.2 Build health intelligence to assist with locality based inequities. Source and develop community profiles for all areas of the state to assist with addressing locality based inequities and to enable interventions to be targeted Identify and map ‘at risk’ communities and target groups Evaluate and monitor performance of programs 5. Build sustainable partnerships 5.1 Promote and integrate oral health into all appropriate partnerships, settings and opportunities. Identify, develop and maintain appropriate partnerships with health, education, sporting, youth, welfare and aged care, all levels of government, industry, community sector groups and agencies within the community. Build capacity of appropriate partners to be oral health champions Work with targeted communities to address their needs, build their capacity and enable them to make informed decisions about their own oral health Form collaborative partnerships between providers of oral health and general health to improve: o Knowledge of the links between oral and general health o Identification of oral health conditions, risk assessment skills and referral pathways o Care coordination o Potential linkages for oral health services with primary health care partners Prioritise and support settings approaches that link to the home and community. (eg. MWEW primary and early childhood, Family Food Patch and TSCA Cool Cap program) Promote and support peer group initiatives Form collaborative partnerships with other programs with shared risks, populations and goals. Support partners and programs that address social determinants and inequalities within the population. 5.2 Emphasise a population health approach. 8 References NACOH, 2004, Healthy Mouths healthy lives: Australia’s National Oral Health Plan2004-2013. Adelaide, National Advisory Committee on Oral Health, Australian Health Minister’s Advisory Council. 2Irwin, C., Mullaly, B.,Ziada,H.,Byrne,P.J., and Allen, E. 2008. Periodontics and Systemic Conditions – Is there a link? 3 Sanders AE and Spencer AJ Oral Health Inequalities and Psychosocial Factors. Presented at 33rd Public Health Association of Australia annual conference 2001 1 4 Sheiham,A. and Watt, R.G. 2000. The Common Risk factor approach: a rational basis for promoting oral health. Community Dent. Oral Epidemiology 28:399-406 Australian Bureau of Statistics, 2011, Health @ a glance, 2011, Cat no. 4841.0, viewed 11 November 2011 Sheiham, A, and Watt, R.G 2005. Editorial: Oral health, general health and quality of life. Bulletin of the World Health Organisation 7 Roger JG. Evidence Based Oral Health Promotion Resource. Prevention and Population Health Branch, Government of Victoria, Department of Health, Melbourne. 2011 8 Heckman, J.J. (2006). Investing in Disadvantaged Young Children is Both Fair and Efficient. Presented to the Committee for Economic Development, the Pew Charitable Trusts, PNC Financial Services Group, New York City, January 10, 2006 9 Australian Institute of Health and Welfare 2011. Dental decay among Australian children. Research report series no. 53. Cat. no. DEN 210. Canberra: AIHW. 10 Tickle M, Threlfall AG, Milsom KM, Blinkhorn AS. The occurrence of dental pain and extractions over a three year period in a cohort of children aged 3-6 years. Journal of Public Health Dentistry. doi:10.1111/j.1752-7325.2007.00048.x 5 6 11Australian Institute of Health and Welfare 2011. Dental decay among Australian children. Research report series no. 53. Cat. no. DEN 210. Canberra: AIHW. Wind M, Kremers S, Thijs C and Brug J 2005 Toothbrushing at school: effects on tooth brushing behaviour, cognitions and habit strength, Health education, vol.105, No 1, pp.53-61 13 Roberts-Thomson K and Do L. 2007, Oral health status, Australia’s dental generations: the National Survey of Adult Oral Health 2004-06, (G D Slade, A J Spencer, K F Roberts-Thomson Eds.), Canberra, Australian Institute of Health and Welfare (DentalStatistics and Research Series No. 34). 81-142 14Rogers JG. Evidence Based Oral Health Promotion Resource. Prevention and Population Health Branch, Government of Victoria, Department of Health, Melbourne. 2011 15 ABS, 2009, Cause of death, Australia,2007, Catalogue number 3303.0. Canberra, Australia Bureau of Statistics 16 AIHW Dental Statistics and Research Unit 2008. The National Survey of Adult Oral Health 2004–06: Tasmania. Cat. no. DEN 180. Dental Statistics and Research Series no. 44. Canberra: Australian Institute of Health and Welfare 12 9