Following are our point-by-point responses to Reviewer`s comments
advertisement

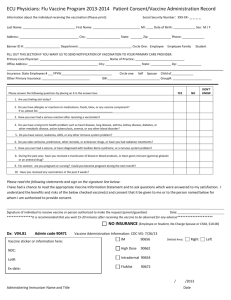
Following are our point-by-point responses to Reviewer’s comments: Author’s response to reviews Title: An Adjuvanted Inactivated Murine Cytomegalovirus (MCMV) Vaccine Induces Potent and Long-term Protective Immunities against a Lethal Challenge with a Virulent MCMV Authors: Huadong Wang (wanghd116@hotmail.com) Yanfeng Yao (yaoyanfeng1981@yahoo.com.cn) Chaoyang Huang (cyhuang1984@hotmail.com) Xingxing Fu (fuxingxing1@yahoo.com.cn) Quanjiao Chen (zuochqj@126.com) Hongbo Zhang (hongboflood@163.com) Jianjun Chen (chenjj126@126.com) Fang Fang (fangfangc@263.net) zhenyuan Xie (zhen1212@sina.com) Ze Chen (chenze2005@263.net, chenze2005@hotmail.com) Reviewer’s report (Second time) Title: An Adjuvanted Inactivated Murine Cytomegalovirus (MCMV) Vaccine Induces Potent and Long-term Protective Immunities against a Lethal Challenge with a Virulent MCMV Reviewer #1: Professor Luka Cicin-Sain Version: 3 Date: 20 November 2012 Response to referee’s comments 1 We thank the reviewers for their careful review and constructive comments. We have made extensive modifications of the manuscript according to the suggestions. Reviewer’s report: I have read the revised version of the manuscript. The authors of this manuscript have addressed adequately my major compulsory revisions 1, 3, and 5. 1. There appeared to be a misunderstanding about my question 4. The authors pasted their reply to their answer 2 of the reviewer #2, but did not address my concern about the non-specific induction of the immune system by their vaccine formulation. While the authors provide a detailed description of the purification conditions used to generate their antigen, they failed to recognize that their control groups have still not received any adjuvant in isolation. Therefore, it is not clear if the adjuvant alone would have resulted in protection against MCMV challenge, or if this effect was due to the increase in the induction of B-cell responses, as measured by ELISA. While I have not requested that the authors provide a formal proof of serum-mediated protection by adoptive transfer experiments, it is necessary that the authors show at least that immune protection is not enhanced in control groups with adjuvant-alone treatment. Thanks for the reviewer’s comment and suggestion. We understand reviewer’s concerning about the non-specific induction of the immune system by vaccine formulation and adjuvant alone would have resulted in protection against MCMV challenge. We agreed with reviewer that it is necessary to show that immune protection is not enhanced in control groups with adjuvant-alone treatment. We have conducted the suggested control experiments about adjuvant-alone treatment and mock vaccine. The results from adjuvant-alone treatment groups showed that administration with MF59, alum, chitosan alone intraperitoneally or intramuscularly couldn’t provide mice specific protection against lethal viral infection and anti-MCMV IgG was also not detected in three adjuvants alone treated mice (table 1, 4). The mice immunized with mock vaccine were not protected from lethal MCMV challenge and no anti-MCMV IgG was detected in these mice (table 1, 4). So the adjuvant-alone treatment or mock vaccine immunization neither induce specific anti-MCMV humoral immune response nor provide mice any protection against MCMV challenge. 2. The major omission in the new manuscript version is the lack of control experiments as required in my comment 2. Arguing that intraperitoneal immunization of mice is a common practice by referring to 10+ years old literature (which they failed to cite in the primary submission), is not a valid rationale to decline to perform vaccinations by a route that would mimic real-life settings, approximating clinical or veterinary medicine standards. Since the major advance of this article is the comparison of various adjuvants, and adjuvants may have effects which could vary by their site of application, it is imperative that the effect of the adjuvants on immune response as well as its toxicity are evaluated by an immunization route that may be used in clinical trials. Therefore, I am, unfortunately, still forced to advise against the publication of this article, unless the suggested control experiments have been performed. Thanks for the reviewer’s constructive suggestions. We agree with reviewer that the major advance of this article is the comparison of various adjuvants, and adjuvants may have effects which could vary by their site of application, it is imperative that the effect of the adjuvants on immune response as well as its toxicity are evaluated by an immunization route that may be used in clinical trials. We took the suggestions of administering the vaccine in different immunization route very seriously and performed a series of experiments to learn whether FI-MCMV vaccine administrated by intramuscular injection could provide similar protection as i.p. immunization route. The mice were immunized twice with 4 µg, 1µg and 0.25µg of the vaccine with or without an adjuvant by intramuscular route. The results from i.m. immunization experiments agreed with those from analysis by intraperitoneal immunization, whereas the overall protection effect of i.m. immunization was slightly inferior relative to i.p. route. Co-administration the FI-MCMV vaccine with adjuvant could significantly enhance the immune response in mice than the adjuvant-free vaccine and MF59 was more potent in immune enhancement relative to alum and chitosan. The corresponding results were presented in table 4 (page 30) of the revised manuscript. Level of interest: An article of limited interest Quality of written English: Acceptable Statistical review: No, the manuscript does not need to be seen by a statistician. Declaration of competing interests: I declare that I have no competing interests. Reviewer’s report (First time) Title: An Adjuvanted Inactivated Murine Cytomegalovirus (MCMV) Vaccine Induces Potent and Long-term Protective Immunities against a Lethal Challenge with a Virulent MCMV Reviewer # 1: Professor Luka Cicin-Sain Version: 2 Date: 6 August 2012 Response to referee’s comments 1 We thank the reviewer for a very careful review and very thoughtful comments. Following are our point by point response to the reviewer’s comments: The major compulsory revisions are: 1. The authors do a poor job in explaining the state of the art in experimental inactivated MCMV vaccines, and to place their advances in context. In fact, a protective effect of an immunization with a formalin-inactivated MCMV was shown in mice several times before. The authors do not refer to the seminal work by Tolpin et al. (Tolpin et al., J Infect Dis 1980, 142(4): 569-574) and the subsequent work by Morello et al. (Morello et al., J Virol 2002, 76 (10): 4822-4835) and Geoffroy et al. (Geoffroy et al., Vaccine 1996, 14(17-18): 1686-1694) neither in the introduction, nor in the discussion. In fact, Tolpin et al showed in 1980 that administration of two doses of formalin-inactivated MCMV reduced the mortality after challenge with a lethal SG-MCMV, and Morello showed that FI-MCMV and alum leads to higher antibody titers and decreased viral titer in spleen and salivary glands after lethal challenge in comparison to a vaccination without adjuvant. While these articles are referred in the material and method section, the citations are out of context, and do not allow the reader to appreciate which part of the current work is a repetition of previously published data. Thanks for the reviewer’s comment. The research on HCMV vaccine has been carried out for 30 years, but up to now no vaccine was approved for clinical use. As the reviewer mentioned, there were already several studies about the performance of inactivated MCMV vaccine in the animal experiments. As early as in 1980, Tolpin et al. reported that twice immunizations of mice with inactivated MCMV vaccine (immunizing dose around 107.7 pfu) could provide a protection rate of 89% against a low-level virus challenge (2 × LD50). However, most mice still developed mild or subclinical infections after challenge. In 1996, Geoffroy et al. inactivated MCMV with sodium periodate or β-propiolactone. They evaluated the immunogenicity of vaccine inactivated by these two inactivating agents by immunizing mice three times (immunizing dose around 107 pfu) and a following 5 × LD50 challenge. Although the protective rate of PI- or βI-MCMV reached 100%, the researchers discovered that the long-lasting protection offered was incomplete. In 2002, Morello et al. adopted an immunization strategy by combining pDNA pool and FI-MCMV (mixed with alum), in which DNA immunization was performed 3 times and FI-MCMV immunization twice. Their results demonstrated that this immunization strategy could provide effective protection. However, they only performed a sub-lethal challenge (< 1 × LD50). We have added these relevant information in the manuscript. From the above studies, we can see that the protection efficiency and efficacy of inactivated MCMV vaccine need further improvement. Adjuvant is non-specific immune-enhancing substance, which is a main focus of vaccine development. We designed our study to examine the protective effect of vaccine with adjuvant. In this study, our immunization strategy in combination with adjuvant effectively increased the efficacy of inactivated MCMV vaccine. Furthermore, we compared the protective immunity of three adjuvants (MF59, alum, and chitosan) and discussed the long-term protection of this vaccine. 2. The major novelty of the manuscript is the comparison of the protective capacity of various adjuvants. Therefore, the relevant information would be obtained by administering the vaccine in a format that is common in vaccine asministration, (i.e. subcutaneously, intramuscularly or intranasally). Unfortunately, the vaccine formulation was exclusively applied intraperitoneally, a route of immunization that is unlikely to be performed in clinical settings, and hence it is not possible to predict if MF59 would outperform the other adjuvants when applied locally. Thanks for the reviewer’s suggestion. In the mouse experiment for evaluating the protective effect of inactivated vaccine, intraperitoneal injection is a common route for vaccination. In addition, intraperitoneal injection was adopted in all the literatures mentioned by the reviewer in the first comment. We agree with the reviewer that it is interesting to compare different immunization routes, and we will carry related research in future study. 3. The authors claim that the adjuvant they used is safe. However, no information is provided about the monitoring of side-effects during immunizations. Hence it is not clear if the intraperitoneal application of the vaccine formulation induced fever, weight loss, or other symptoms typical of acute inflammation. Moreover, the method used makes it impossible to monitor for local inflammatory side effects at the site of immunization (see previous point). Thanks for the reviewer’s comment. Based on the advice, we have changed the conclusion in the beginning of the manuscript from “These results suggest that inactivated CMV vaccine is safe and effective. In addition, the adjuvanted CMV vaccine provided more effective and longer-term protection than the adjuvant-free vaccine.” to “These results show that inactivated CMV vaccine is effective, and the adjuvanted CMV vaccine provides more effective and longer-term protection than the adjuvant-free vaccine.” Actually, the safety of the adjuvant was observed by the symptoms in mice. In this study, normal gait, typical posture and behavior were observed in all study groups. Significant abnormal signs, such as piloerection, body weight loss, hypoactivity, and ascites, were not observed in immunized mice during the study. Moreover, in the long-term immunogenicity study, there were no abnormal signs or reactions observed in groups inoculated with the vaccine with or without adjuvant at month 6 after the vaccination, which further demonstrated the safety of the vaccine and adjuvant. 4. The authors claim that the adjuvanted CMV vaccine provides more effective protection than the adjuvant-free vaccine, but they omitted controls with formalin-treated lysates of mock-infected NIH-3T3 accompanied by adjuvants. Therefore, it is not clear if the improved immune protection resulted as a boost of the Ag-specific immune response, or is a result of nonspecific immunity provided by peritoneal inflammation caused by the injection of the adjuvant. Similarly, due to the absence of a mock-vaccinated control, it is not possible to define if the vaccine devoid of adjuvant induced any increase of the antibody titer over the baseline values. Thanks for the reviewer’s suggestion. In this study, we only harvested medium from the infected cells, after removal of cellular debris by low speed centrifugation (6500 g, 20 min, and 4°C) and subsequent inactivation, the virus was concentrated by centrifugation at 26,000g for 3h at 4°C. Virus pellets were resuspended in PBS and purified by ultracentrifugation at 72,000g in a swing-out rotor for 1 hr at 4 °C through a sucrose gradient. The MCMV vaccine was further confirmed by SDS PAGE and western blot analysis (see figure in the end of this document). In addition, in order to avoid the present of cellular proteins, we didn’t split the infected cells to obtain virus. According to Geoffroy’s report, through this procedure, cellular contamination of the viral material was found to be less than 2% (Arch Virol 1994, 135(1-2):61-74). Thus, we did not set controls with formalin-treated lysates of mock-infected NIH-3T3, we use unimmunized mice as control (table 2). In addition, Ab-positive cutoff values were set as mean ± 2SD of unimmunized sera in this study (table 1). The ELISA Ab titer was expressed as the highest serum dilution giving a positive reaction. Vaccination with inactivated MCMV vaccine alone could provide protection, whereas combination of adjuvant could enhance the protective effect. In our study, the adjuvants were proved to be able to improve the long-term protection. As for the immuno-mechanism, adjuvant not only induces the more long-lived effects of the adaptive immune response, but enhances innate immune response, affects the transient reaction of the innate immune response. An adjuvant-enhanced innate immune response leads to an enhanced adaptive immune response. So, the inflammation caused by the injection of the adjuvant maybe the available initiation to promote the effective immune response,and that is the sense of the inflammation resulted from adjuvant. In this study, we observed that the antibody titers in the adjuvanted group were higher than those in the corresponding vaccine alone groups, and the survival rates were higher in the adjuvanted vaccine groups. The stronger adaptive immue response was induced in groups administrated with adjuvanted vaccine, which indicated that the adjuvant had played its role successfully. In addition, MF59 and alum have been approved for marketing as adjuvant. We think that these two adjuvants might not able to provide protection alone. 5. The authors should also carefully and comprehensively check the English grammar and style, probably by inviting a native speaker to carefully peruse the manuscript. Thanks for the reviewer’s suggestion. We have asked professional English editing company recommended by the BMC infectious disease to check the English grammar of this manuscript. Fig SDS-PAGE and Western bloting of inactivated MCMV. (A) FI-MCMV proteins were separated by SDS-PAGE and stained with Coomassie blue (M: protein marker, lane 1: separated FI-MCMV protein bands). (B) The electrophoresed proteins were transferred to a PVDF membrane. The membrane was incubated with serum pooled from FI-MCMV vaccine immunized mice and then with HRP-conjugated secondary antibodies and enhanced-chemiluminescence detection (M: protein marker). Level of interest: An article of limited interest Quality of written English: Not suitable for publication unless entensively edited Statistical review: Yes, but I do not feel adequately qualified to assess the statistics. Declaration of competing interests: I declare that I have no competing interests. Reviewer #2: Professor Mark Schleiss Version: 2 Date: 23 August 2012 Response to referee’s comments 2 We thank the reviewer for a very careful review and very thoughtful comments. Following are our point by point response to the reviewer’s comments: Major Comments: 1. The authors could provide additional evidence that makes it more clear and certain that the vaccine was inactivated. There is a short sentence saying that plaque assay showed that the inactivation was successful, but few details are provided. Were any additional studied performed to ensure adequate formalin inactivation? This is particularly important for a translational goal of a human vaccine, where GMP issues would require rigorous proof of inactivation. Thanks for reviewer’s suggestion. As described in the manuscript, the viruses were inactivated by adding 37% formalin at a ratio of 1: 4000, and mixed thoroughly at 4°C for one week with stirring. The inactivation of the virus and vaccine was proved to be complete by three methods in this study. Firstly, the inactivated virus stock was used to infect NIH-3T3 cells. The 3T3 cells were incubated for 7 days, and no cytopathic effect (CPE) was observed. Secondly, the inactivated vaccine was confirmed to be completely inactivated by plaque assay. Thirdly, the inactivated vaccine was i.p. injected into mice, and no virus was isolated from the spleens, livers and salivary glands of mice. Based on these results, we could confirm that our viruses were completely inactivated by formalin. We added these information in manuscript. 2. Did the centrifugation steps to purify vaccine result in purification of actual virus particles? Were additional studies performed to be certain that there was no cellular protein present? This, too, would be a major regulatory issue for GMP purposes. If the inactivation process resulted in a vaccine that still consisted of particles, the vaccine is in some ways reminiscent of the work of Plachter (Gene Ther. 2003 Feb; 10:278-84; J Clin Virol. 2002 Aug; 25 Suppl 2: S75-85). It would be of interest to compare the inactivation techniques, the added benefit of adjuvant, and the vaccine procedures to the dense body work. Thanks for reviewer’s comment. We only harvested medium from the infected cells, after removal of cellular debris by low speed centrifugation (6500 g, 20 min, 4 °C) and subsequent inactivation, the virus was concentrated by centrifugation at 26,000g for 3hr, at 4 °C. Virus pellets were resuspended in a small amount of phosphate-buffered saline and purified by loading the virus onto a 15% sucrose/virus standard buffer (VSB) and centrifuge at 72,000g in a swing-out rotor for 1 hr at 4 °C (J Virol. 1983 Sep;47(3):421-33; Curr Protoc Immunol 2001, Chapter 19:Unit 19 17; Hum Reprod 2001, 16(10):2041-2049). The MCMV vaccine was further confirmed by SDS PAGE and western blot analysis (see figure in the end of this document). In addition, in order to avoid the present of cellular proteins, we didn’t split the infected cells to obtain virus. According to Geoffroy’s report, through this procedure, cellular contamination of the viral material was found to be less than 2% (Arch Virol 1994, 135(1-2):61-74). The preparation of the vaccine in this study was referred to previously reported methods as mentioned by reviewer. There might be a small quantity of dense body present in the prepared vaccine. Dense bodies are mainly composed of the tegument protein pp65, and a lipid bilayer envelope, comparable or identical to the viral envelope, which can induce potent immune responses. The presence of small quantity of Dense bodies in the MCMV vaccine did not influence the results of experiment. 3. The authors should state what the LD50 dose of SG virus was. How did this translate into PFU or actual titer of virus? This would be of interest for investigators who define inocula not by LD50, but by titer of virus. Thanks for reviewer’s comments. For lethal dose experiments, MCMV was serially passaged in BALB/c mice to restore the virulence. The SG-MCMV stock was titrated on 3T3 cells by plaque assay, which had a titer of 107.1 PFU/ml and a 50% lethal dose (LD50) in BALB/c mice following intraperitoneal infection of 105 PFU. In our study, challenge was performed with 5 × LD50 virus stock (5 ×105 PFU). Since the virulence of virus differs in each passage, its LD50 also changes and should be determined in each practical animal experiment. In this study, the 10th passage of SG-MCMV was used, its LD50 was determined based on the mortality rate of mice and its virus titer was obtained from cell experiments. 4. It would be of interest to compare the ELISA assay titers in vaccinated animals to the titers of “naturally seropositive” animals, or animals challenge with non-lethal doses of virus. Thanks for reviewer’s suggestion. We agree with reviewer that it will be interesting to compare the ELISA assay titers in vaccinated animals to the titers of "naturally seropositive" animals, or animals challenge with non-lethal doses of virus. Due to the difficulty in obtaining naturally seropositive mice, the complexity in genetic backgrounds of mice and huge individual differences, we think it is difficult to perform the comparison study. Since the ELISA titer is dependant on the vaccine immune dose and virus infective dose, we think that the ELISA assay titer induced by high dose of inactivated vaccine will be higher than that of non-lethal doses of virus. 5. It would be of interest to know what the neutralizing antibody titers were that were induced by immunization, and how these compared to naturally infected mice. Thanks for reviewer’s kind suggestion. Since the tendency of neutralizing antibody titer was previously reported to be consistent with that of serum IgG titer (Geoffroy et al., Vaccine 1996, 14(17-18):1686-1694; Morello et al., J Virol 2002, 76(10) :4822-4835), we only measured IgG antibody level induced by vaccination in this study. Since the MCMV naturally infected mice were hard to obtain, we did not design the comparison study. However, we will take this suggestion into consideration in our future study. 6. Did the authors examine the western blot profile against MCMV polypeptides in vaccinated animals? Thanks for reviewer’s comments. Since the genome of MCMV Smith is 230,278 bp in length, which is predicted to encode 170 ORFs (J Virol. 1996 Dec;70(12):8833-49). Analysis on the targeting protein or polypeptide of the antibody by Western blot will be huge work. In addition, the main purpose of this study is to compare the efficiency of different adjuvants. However, we agree with the reviewer and we will study the surface glycoprotein first in future. 7. The authors should clarify why chitosan was less protective than alum in terms of mortality, even though they were both equally immunogenic. The authors note, “adjuvant Alum could granulate antigens and also activate the innate immune pathway, creating an immune active environment at the injection site, thus promoting the co-immunized antigen to induce good antibody response ”, but while this statement is scholarly, there are no experiments in this study that specifically address this point. Thanks for reviewer’s suggestion. In our study, the IgG antibody levels induced in mice of chitosan group and Alum group were close, with the Chitosan group slightly lower than the Alum group. In addition, there was no significant difference in the survival rates of mice from these two adjuvanted groups three weeks after the second immunization. However, the antibody level of the Chitosan group was significantly lower than that of the Alum group at 6 month after the third immunization, which was corresponding to the low survival rate of the Chitosan group after the lethal challenge. Based on these observations, we speculate that the chitosan may be less efficient in inducing long-term immunity. We have cited the reported and confirmed results for the immunostimulation mechanism of Alum in this manuscript. We didn’t perform relevant experiments in this study. 8. Do the authors have any information on cell mediated immune responses? It may be that some of the differences identified from one adjuvant to another are related to differences in the cell mediated immune response. Thanks for reviewer’s suggestion. Generally, the inactivated vaccine will mainly induce humoral immune response. The differences of adjuvants in improving immune responses could be well illustrated by the antibody levels, we didn’t evaluate the cell mediated immune responses in this study. However, we couldn’t exclude that the cell mediated immune responses might have played a certain role. 9. The authors should comment on the work of Morello and Spector (for example, J Virol. 2002; 76: 4822-35) that demonstrate really very robust sterilizing immunity using various combination of formalin-inactivated vaccines. Although the authors do reference this work, there is not much comment on the difference in the magnitude of protection. Wang et al. reassuring saw a reduction in virus titer in organs of vaccinated versus unvaccinated animals, but the level of protection appears lower than that observed by Morello. Is there an explanation for this? Thanks for reviewer’s careful review. The magnitude of protection induced by the inactivated vaccine in our study was lower than that previously reported in Morello et al, which was mainly resulted by the difference in the challenge dosages used. In our study, we used high lethal dose of 5 × LD50 for challenge, whereas a sub-lethal dose below 1 × LD50 was used in Morello et al study. 10. Figures 1 and 2 do not have statistical information. This would enhance the figure. Were any of the differences observed considered to be statistically significant? The text of the paper does not make this clear, or how the authors tested for statistical significance in these comparisons. Thanks for reviewer’s suggestion. There were indeed significant differences between some experimental groups in Figure 1 and 2, and we didn’t clarify these in the Figures. According to the reviewer’s advice, we have made necessary modifications in these two figures in the manuscript. Minor comments: 1. The manuscript should have page numbers on it. Thanks for reviewer’s suggestion. We have added page numbers in the manuscript. 2. Methods section, “Detection of HCMV-specific antibody” should be corrected to “Detection of MCMV-specific antibody”. Thanks for the reviewer’s careful review. We have corrected the “Detection of HCMV-specific antibody” to “Detection of MCMV-specific antibody” in the manuscript. 3. Although it is a different model, in another rodent CMV there were interesting and significant differences in protection and immune response upon comparison of alum and Freund’s adjuvant (J Infect Dis. 2004; 189: 1374-81), underscoring the critical importance of adjuvant in optimization of a CMV vaccine. Thanks for reviewer’s suggestion. In this study, we have used MF59, alum and chitosan as adjuvants and compared their efficiencies in improving the immunization effects. We agree with the reviewer that adjuvant plays an important role in optimization of a CMV vaccine Level of interest: An article whose findings are important to those with closely related research interests Quality of written English: Needs some language corrections before being published Statistical review: No, the manuscript does not need to be seen by a statistician. Declaration of competing interests: I have no conflicts of interest related to this manuscript.