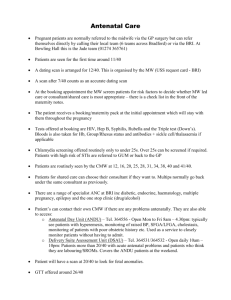
Northern Health Routine Antenatal Visits for Shared Maternity Care
advertisement

Northern Health Routine Antenatal Visits for Shared Maternity Care: Summary This reflects minimum visits. Additional visits should be arranged as appropriate. For more detail on antenatal visits please refer to the Shared Maternity Care Guidelines 2010 on GP Access www.nh.org.au Location Initial GP consultation Timing (approximately) Usually 4 -10 weeks Who sees GP Notes Indicate request for Shared Maternity Care in referral Fax referral to outpatients FAX-8405 8761 Please ensure that copies of any investigations ordered by the GP are sent with the patient to the first hospital visit. Antenatal screening tests: MSU Blood Group/Antibodies FBE Hep B Serology Rubella VDRL Glucose Challenge Test Hep C Serology HIV Vitamin D level TFT Consider: Dating US Ferritin Haemoglobin electrophoresis/DNA analysis for Alpha Thalassaemia Varicella Antibodies Chlamydia (urine) GTT Pap test if due Discuss testing for fetal abnormalities Combined First Trimester Screening (this is generally not available via the hospital) Second Trimester Maternal Serum Screening Fetal morphology ultrasound 1st Hospital Visit 10-16 weeks Midwife and Consultant SMCA 16 weeks GP D:\116106239.doc Consider tests for fetal abnormalities/genetic carrier status CVS/amniocentesis Cystic Fibrosis testing Fragile X testing Others as relevant Note: It is preferable that initial investigations are ordered by the GP with copies of results sent with the woman to the first hospital visit. If they have not been done, they will be arranged at the first hospital visit Standard antenatal examination Second Trimester Maternal Serum Screen at 14+ weeks organised by Northern Health 18-20 week fetal morphology ultrasound arranged by Northern Health Smoking & illicit drug use screening. Genetic counselling arranged if indicated Standard antenatal examination Review of pregnancy record entries Ensure testing for Down Syndrome has been discussed/organised Ensure fetal morphology ultrasound has been discussed/organised Hospital 20 weeks SMCA 24 weeks Hospital 28 weeks Consultant GP Consultant Standard antenatal examination Review and document investigation results including fetal morphology ultrasound Standard antenatal examination Review and document investigation results including fetal morphology ultrasound Standard antenatal examination Fetal Movement Chart Glucose Tolerance Test (if abnormal Glucose Challenge Test at first visit) SMCA 30 weeks SMCA 32 weeks SMCA This is replaced by a hospital visit for women requiring anti-D Hospital 34 weeks 36 weeks GP GP GP Consultant FBE, Rh Antibodies Anti D if required Standard antenatal examination Review and document investigation results Standard antenatal examination Review and document investigation results Standard antenatal examination Review and document investigation results Anti-D (if required) Standard antenatal examination GBS swab For women with past history of caesarean section: discussion with the hospital Doctor and decision regarding vaginal birth after caesarean (VBAC) or elective caesarean is finalised at this visit SMCA 37 Weeks SMCA 38 weeks SMCA 39 weeks Hospital 40 weeks to delivery Post delivery Week 6 GP GP GP Consultant GP Standard antenatal examination Review and document investigation results Standard antenatal examination Review and document investigation results Standard antenatal examination Review and document investigation results Standard antenatal examination Review and document investigation results Cardiotocograph (CTG) as per arranged by hospital Amniotic Fluid Index (AFI) as per arranged by hospital Patient to make own appointment Northern Health consultant visit only if significant complication of pregnancy or request for sterilisation/IUD Schedule visits 18/11/10 Referral for OGTT given to patients with Gestational Diabetes, GP to follow up result 2 of 2