the TB protcol for doctors and nurses
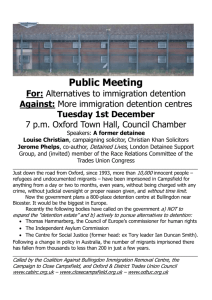
advertisement

Tuberculosis Protocol for Nurses and Doctors When a detainee presents with symptoms suggestive of TB the following should be considered: New transfer or admission? 1. 2. 3. 4. 5. 6. Are there old notes/results at previous centre? What are the concerning symptoms? Are you concerned about the possibility of open active TB? Is the patient genuine? How long has he been in this country? Is it worth liaising with health care at the previous centre now? 7. What is required to minimise risk to others? Detainee with a Known Diagnosis Where a patient with a known diagnosis of open active TB arrives who has been on treatment for less than two weeks or where a patient arrives with treatment from the community and doubt exists about compliance that detainee should not pass reception and admission should not be allowed to the centre. Health care should advise Immigration that the person requires segregated single room accommodation in a centre with such facility and ongoing medical assessment. Where doubt remains the duty medical officer should be advised of the situation Where a detainee with known TB comes from another centre on treatment and; it is confirmed with the previous centre health care staff that he/she has complied with medication for a minimum of two weeks there is NO concern about possible drug resistance having considered the risk factors he/she may be admitted thereafter to this centre. Where there has been non- compliance or there is any question whatsoever of possible drug resistance to treatment he/she should NOT be admitted to the centre. Detainee requiring Assessment/Investigation Where it is required to segregate a detainee pending assessment or investigation and such appropriate accommodation is not available within Dungavel. He/She should not be allowed into the centre. Immigration should be advised that the individual requires medical assessment involving isolation/segregation in a centre with appropriate single room accommodation. Detainee in Residence Where a patient already in residence reports symptoms where it is felt that a differential diagnosis of TB is possible after consultation with the Medical Officer it may be appropriate to proceed with investigation. Such investigation can be done while the detainee remains in segregation at Dungavel if such accommodation is available. Where such accommodation is not available it may then be necessary to liaise with the duty consultant in infectious disease with a view to hospital referral. Signs and Symptoms of possible TB Infection 1. 2. 3. 4. 5. 6. 7. 8. 9. Cough Sputum/ haemoptysis Chest pain Shortness of breath Night sweats Pyrexia Weight Loss Anorexia General Malaise Where there is concern: 1. 2. 3. 4. 5. Isolate/segregate Sputum samples x 3 on consecutive days to lab Chest XR if not already available FBC, U&Es, LFTs, C-reactive protein, ESR If no facility to isolate liaise with Dr to consider referral to infectious diseases. NB: An abnormal CXR is often found with no symptoms but the reverse is rare. Pulmonary TB is unlikely in the absence of any radiographic abnormality. Where the bloods are normal particularly the CRP, sputums are negative and CXR negative the diagnosis of open active pulmonary TB is most unlikely. The patient need then not stay in isolation as directed by the duty medical officer. Where it has not been possible to obtain sputums because the patient does not have productive spit and the bloods and CXR are normal again open active pulmonary TB is not likely and the detainee need not stay in further isolation. This should be directed by the duty medical officer. DRUG RESISTANCE There is increasing drug resistance to TB in various parts of the world. Risk factors to be for developing drug resistant TB Off and on treatment for possible reactivations Immunocompromised eg HIV, alcohol abuse, immuno suppressant therapy Poor compliance Prescribing patterns eg monotherapy, adding single drugs to failing regimes Diagnosis abroad eg Eastern Europe, Russia Detainees should on most occasions only require transfer to hospital for investigation where clinical suspicion remains after baseline investigations have been carried out or where it has not been possible to carry out baseline investigations (e.g. lack of facility) or where it has not been possible to obtain sputum’s etc and some of the other investigations show abnormality e.g. a concerning report on CXR, or raised CRP. Dungavel Isolation/Segregation Facilities The centre as at April 2006 does not have suitable medical isolation facilities for specific airborne infectious diseases such as open active pulmonary TB. However each individual case will be taken on its merit and where it is felt appropriate by nursing or medical staff it may be possible to temporarily segregate an individual pending further assessment and management. This can be on a short term basis only. The location decided upon must be in discussion with duty nurse, duty medical officer and DCM. Health care advice to residential staff is paramount and must take precedence. All efforts will be made to cause minimum residential disruption while minimizing risk to other detainees and staff. Where it is considered that no suitable location is available within the centre Immigration will be advised of this and further relocation discussed i.e. another centre or if clinically appropriate hospital. Examples of possible temporary segregation facilities are top floor RTU and secure unit. Rooms opening directly off corridors are NOT appropriate facilities for airborne diseases. Actual location will be discussed on an as required basis.