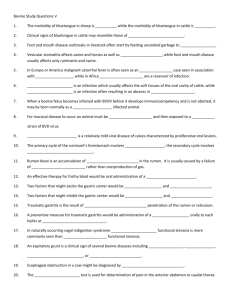
Bovine Viral Diarrhea
advertisement

Bovine Viral Diarrhea CAUSE: The bovine viral diarrhea (BVD) virus causes a number of disease syndromes in cattle. It was first recognized in North America in the 1940s. EFFECT: Depending on the stage of gestation when infected, BVD may result in early embryonic death, abortion, premature births, or the birth of weak young. Some clinically normal calves will be carriers of the disease, so-called persistently infected (PI) animals. BVD can also cause respiratory disease. In some situations, a severe and deadly form of disease, called mucosal disease, can result. How is BVD spread? The virus lives in nasal mucus and saliva and is spread by direct contact between cattle, either nose to nose, or nose to mouth. It can also be spread by fomites, e.g. on hands, clothes, and footwear. How can BVD be prevented? Test and isolate additions to your herd. Make sure your herd is properly vaccinated. Keep in mind that vaccination is not 100% protective. Test for and cull persistently infected heifers. What if there is an outbreak? Immediately separate affected and exposed animals from the rest of the herd. Even a well-prepared herd may succumb to BVD when introducing new animals if the right mix of naïve and shedding animals with the right mix of viral types meet. For more information on BVD, see: http://www.usjersey.com/Reference/BVDVfacts_UCDavis.pdf http://www.gov.on.ca/OMAFRA/english/livestock/dairy/facts/bovinevi.htm http://nyschap.vet.cornell.edu/module/bvd/bvd.asp Bovine Leukosis Virus CAUSE: The bovine leukosis virus (BLV) is a retrovirus that affects only cattle. EFFECT: Infection likely occurs in newborns, but only a small portion of infected animals will show clinical signs of the disease. In the lymphosarcoma form of disease, infected animals develop tumors in the uterus, abomasum, or thorax. In the leukemia form of disease, they have an abnormally high number of white blood cells in circulation. Advanced stages of the disease may be signaled by weight loss, decreased milk production, enlarged lymph nodes, paralysis in hind legs, and fever. How is Bovine Leukosis spread? The disease is blood borne and can be spread by direct transfer of blood from one animal to another by way of an insect vector (e.g. horseflies), contaminated needles, dehorners, or ear taggers. Vertical transmission is possible, from dam to calf, via colostrum. How can Bovine Leukosis be prevented? Test all farm additions to ensure that they are not infected with the disease. Use needles and rectal sleeves a single time on only one cow. Disinfect surgical instruments, dehorners, ear taggers between animals. Use colostrum from only test-negative dams. Does Bovine Leukosis affect people? No, this disease is not transmissible to humans. What if there is an outbreak? This disease is unlikely to present as an “outbreak.” However herds with this disease might consider management strategies to eliminate it from their herd in consultation with their veterinarian. For more information on BLV, see: http://www.oznet.ksu.edu/library/lvstk2/EP51.PDF http://nyschap.vet.cornell.edu/module/leukosis/section1/leukosis1.asp Johnes’s Disease CAUSE: Johne’s (pronounced “yo-nees”) Disease is caused by the bacterium Mycobacterium avium subspecies paratuberculosis (MAP) which infects the intestine and other tissues of cattle, sheep, and goats. EFFECT: Infected animals usually do not show signs of disease until years after first being infected. Clinical signs include foamy diarrhea and weight loss in the face of a good appetite. Milk production also declines. Animals showing clinical signs are soon culled. How is Johne’s Disease spread? Infection primarily occurs in youngstock who have consumed water and feed sources contaminated by fecal material from mature animals that are shedding the Johne’s organism. The infection can also be spread through colostrum. The bacterium that causes Johne’s can survive well in the environment. Contaminated manure spread on fields may be infectious for as long as a year. How can Johne’s Disease be prevented? Prevent the exposure of newborn and growing young stock to manure from the adult herd. Separate calves, lambs, or kids immediately from their dam and feed colostrum from a cow, ewe, or doe that tested negative for Johne’s. Herds that have a low incidence of Johne’s must be careful not to bring it in with new animals, including bulls, rams, or bucks. Does Johne’s Disease affect people? There are ongoing studies of the potential connection between Johne’s Disease in ruminants and Crohn’s Disease in humans. Given the nature of the Johne’s organism and slow progression of these diseases, it will be awhile before there are conclusive results. What if there is an outbreak? Johne’s is not highly contagious so its presence on a farm is unlikely to resemble an outbreak. However, Vermont supports Johne’s risk assessment and status programs through the Agency of Agriculture. For more information visit the Agency website. For more information on Johne’s Disease, see: http://www.vermontagriculture.com/VTCHIP/vchipresources.htm http://www.aphis.usda.gov/vs/nahps/johnes/ Photo: Johne’s Information Center, http://johnes.org/, used with permission. Neosporosis CAUSE: Neosporosis (nee AH spo ROE sis) is caused by Neospora caninum, a protozoan parasite similar to the ones that cause coccidiosis and toxoplasmosis. EFFECT: Neosporosis is associated with early embryonic loss and abortion in cattle. Fetuses carried to term may fail to thrive or appear normal but carry the infection. A related protozoan, Toxoplasma, causes abortions in sheep. How is Neospora spread? This disease is transmitted vertically, from one generation to the next, by cows passing the infection on to their offspring in utero. Carcasses, placentas, and aborted fetuses can spread the protozoan. Dogs are implicated in completing the cycle of development of the protozoan. (Cats complete the life cycle of Toxoplasma gondii.) Mechanisms of postnatal infection are unknown. How can Neospora be prevented? Ensure that all feed and water sources are protected from feces of dogs. Dispose of potentially infected carcasses, placentas, and fetuses immediately and appropriately. Does Neospora affect people? No, Neospora is not known to be transmissible to humans. What if there is an outbreak? Any time there are an unusual number of abortions or unexplained decline in conception rate, appropriate diagnostic tests should be done. Your veterinarian can advise you on managing the disease if neosporosis is diagnosed. For more information on Neospora, see: http://www.usaha.org/speeches/neocan97.html http://www.agr.gov.sk.ca/docs/livestock/beef/herd_health/Neosporosis01.asp Photo: Andrew Peregrine, Department of Pathobiology, Ontario Veterinary College, used with permission. Contagious Mastitis CAUSES: The major causes of contagious mastitis are Staphylococcus aureus, Streptococcus agalactiae, and Mycoplasma spp. EFFECT: General signs of mastitis (inflammation of the udder) are elevated somatic cell count (SCC) and decreased milk production. Economic losses result from lost milk due to the infection itself and from antibiotic treatment. How is contagious mastitis spread? Contagious mastitis organisms are more dependent on close contact with their host for survival than are organisms that cause what is termed “environmental” mastitis. Contagious mastitis can be spread from one cow to the next during milking routines by the milkers’ hands or by the milking equipment. How can contagious mastitis be prevented? Focus on keeping udders clean, using pre-dip, milking mastitic cows last, and treating as directed by your veterinarian based on culture and sensitivity results. Culture milk from new cows and fresh heifers to identify a problem before it can spread. Does contagious mastitis affect people? Contagious mastitis organisms rarely cause infections in humans, but may be harbored on hands. What if there is an outbreak? Strep. ag. can be eradicated from a herd by using appropriate antibiotic therapy. Staph. aureus, on the other hand, is quite resistant to antibiotic therapy. Staph-positive cows should be segregated into their own string. Mycoplasma, too, is resistant to antibiotic therapy. Cows with Myco should be culled. For more information on contagious mastitis, see: http://www.nmconline.org/contmast.htm Photo: http://www.austin.cc.tx.us/microbugz/19blood.html Ringworm CAUSE: Ringworm is not a worm, it’s a fungus that infects skin and hair follicles. Many different fungal organisms cause ringworm. The one most common in cattle is Trichophyton verrucosum. EFFECT: The infection causes brittle hair and raised, gray lesions on the skin, most commonly around the head and neck. How is Ringworm spread? Direct contact between healthy and infected animals will spread the disease. Also, spores from the lesions are shed via hairs or scabs. The spores can survive in the environment for years. How can Ringworm be prevented? Disinfecting and cleaning barns and equipment will help prevent ringworm. Use a strong detergent, then a 1 to 3 part bleach to water solution. Painting rough surfaces can reduce the spore load in the environment. Does Ringworm affect people? Yes, ringworm can infect skin anywhere on the body and often results in a classic red ring around the site of infection, hence the name. What if there is an outbreak? The infection will naturally resolve in young, otherwise healthy animals. Animals with abnormally functioning immune systems may have trouble fighting off the infection. Topical treatments are available, but rarely used. For more information on ringworm, see: http://www.agcom.purdue.edu/AgCom/Pubs/VY/VY-56.html http://www.cattletoday.info/diseases/ringworm.htm Cryptosporidiosis CAUSE: Cryptosporidiosis (KRIP toe spo RID ee O sis or Crypto) is caused by a protozoan parasite, Cryptosporidium parvum, that can infect animals and humans. EFFECT: Crypto invades the lining of the intestines, then proceeds through multiple reproduction cycles. The host may shed up to 1010 (10 billion) oocysts per day for 3 to 12 days in calves and 18 days, on average, in humans. Infected calves often have markedly watery diarrhea beginning at about a week of age. Signs of infection in humans include cramping and upset stomach as well as diarrhea and a slight fever. How is Cryptosporidium spread? The parasite spreads primarily by the fecaloral route through either contaminated feed or water. Environmental contamination by oocysts can be significant and leads to reinfection or infection of new animals in a pen that hasn’t been power-washed first. How can Cryptosporidium be prevented? It is very difficult to prevent infection with Crypto once it is established on a farm. Separate neonates from their dams immediately and prevent fecal cross-contamination of pens, feed and water buckets. Thoroughly clean and power-wash pens between animals to reduce the load of oocysts in the environment. Be sure not to spread contamination during bucket washing. The oocysts are resistant to chlorox at standard dilutions. Complete drying, UV irradiation, and repeated freeze-thaw cycles will kill the oocysts. Does Cryptosporidium affect people? Yes, Crypto can affect humans, especially those with no previous exposure. It is more severe in young or immunocompromised people. There is a lag period of 2 to 10 days between infection and development of symptoms, which may last for about 2 weeks. What if there is an outbreak? If found in humans, consult a healthcare provider. Farms where Cryptosporidium is endemic (commonly found) are unlikely to get rid of it. For more information on Cryptosporidium, see: http://www.uky.edu/Agriculture/AnimalSciences/dairy/extension/nut00054.pdf http://www.cdc.gov/ncidod/dpd/parasites/cryptosporidiosis/default.htm http://www.nalusda.gov/wqic/cryptfac.html Giardiasis CAUSE: Giardiasis (GEE are DYE us sis) is an intestinal illness caused by the tiny unicellular protozoan parasite Giardia lamblia. This parasite has been isolated from domestic and wild animals as well as humans. EFFECT: The protozoan inhabits and multiplies in the small intestine. Chronic diarrhea containing mucus is a classic sign of infection, but low levels of infection may produce no signs. How is Giardiasis spread? The parasite is shed in feces. Consumption of contaminated water or feed sources can infect others. Many animals including dogs, cats, beavers, and bears can carry the parasite without appearing ill. How can Giardiasis be prevented? Prevent contamination of water sources, waterers, and feed by manure of domestic and wild animals. Place wells an adequate distance from septic systems. Like Crypto, Giardia cysts are hardy in the environment, but bleach solutions, quaternary ammonium compounds, steam or boiling water will inactivate them. Can Giardiasis affect people? Yes, in humans, the symptoms start one to two weeks after being exposed to the parasite and can last up to six weeks. Common symptoms are stomach aches and diarrhea. What if there is an outbreak? Determine the source of the parasite if possible. Consult your veterinarian or physician for appropriate treatment recommendations. For more information on Giardiasis, see: http://www.cfsan.fda.gov/~mow/chap22.html http://www.cdc.gov/ncidod/dpd/parasites/giardiasis/factsht_giardia.htm For pictures, see http://www.biosci.ohio-state.edu/~parasite/giardia.html Salmonellosis CAUSE: Salmonellosis is caused by bacteria of the genus Salmonella. The most common types in cattle are S. typhimurium, S. dublin, and S. newport. EFFECT: The bacteria infects the digestive tract leading to fever, diarrhea, dehydration, decreased milk production, and death How is Salmonella spread? Salmonellosis is highly contagious, and is most commonly spread through contaminated feed and water. Manure from infected wildlife (birds, rodents, etc.) is a source of contamination. Young animals and animals with suppressed immune systems are at the highest risk. How can Salmonella be prevented? Isolate new animals before adding them to the herd. Do not allow rendering trucks near live animals, their feed, or barn. Make sure that calving pens are clean and dry. Sanitize all equipment between uses. Restrict animal access to open water sources, and make your facility unattractive to wildlife. Can Salmonella affect people? Yes. Salmonellosis results in fever, abdominal cramps, and other flu-like symptoms. The existence of antibiotic-resistant forms of the bacteria means treatment of even severe cases must be symptomatic (i.e., supportive therapy). What if there is an outbreak? Consult your veterinarian to go over biosecurity procedures to limit the spread of the disease. Antibiotics are rarely effective against Salmonellosis, making supportive therapy (fluids, electrolytes, etc) the best option for individual cases. For more information on Salmonellosis, see: http://www.vermontagriculture.com/VTCHIP/Salbro.pdf http://www.vetmed.wsu.edu/courses-jmgay/FDIUHerdSalmonella.htm Escherichia coli O157:H7 CAUSE: Escherichia coli, or E.coli, is a common bacteria that lives in the intestinal tracts of all humans and animals. Most strains are harmless commensals, but some like O157:H7 cause severe disease. EFFECT: E.coli O157:H7 produces powerful toxins that may cause severe bloody diarrhea and abdominal cramps (hemorrhagic colitis) and a complication where red blood cells are destroyed and cause kidney failure (hemolytic uremic syndrome). How is E. coli spread? Some cattle carry E. coli O157:H7 even though they don’t appear to be ill. Improper hygiene during meat preparation or improper cooking of meat can lead to human infection and disease. Food-borne outbreaks have also been linked to unpasteurized fruit juice and vegetables. How can E. coli be prevented? Ways to limit shedding of the organism from cattle going to slaughter are under investigation. By consuming pasteurized products, washing vegetables thoroughly, and cooking meats completely, people can minimize their risk of food-borne enteric disease like coliform diarrhea. Can E. coli affect people? Yes, E. coli infections in humans range from mild to severe. Usually the disease in self-limiting, but in the case of hemolytic uremic syndrome intensive care is needed. What if there is an outbreak? Cows are rarely ill even if they carry the pathogenic forms of E. coli. E. coli O157:H7 is primarily important in terms of public health. For more information on E. coli, see: http://www.cdc.gov/ncidod/dbmd/diseaseinfo/escherichiacoli_g.htm - Top http://www.cfsan.fda.gov/~mow/chap15.html Campylobacteriosis CAUSE: This intestinal disease is caused by a spiral-shaped bacterium of the genus Campylobacter. EFFECT: These bacteria live in the intestines of clinically normal animals but are the leading cause of bacterial enteritis (diarrhea) in people. How is Campylobacteriosis spread? Like E. coli, some cattle carry Campylobacter even though they don’t show any signs of illness. Improper hygiene during meat preparation or consumption of improperly cooked meat can lead to human infection and disease. Food-borne outbreaks have also been linked to unpasteurized milk. How can Campylobacteriosis be prevented? Proper food preparation and hand-washing before eating will prevent most food-borne illnesses including Campylobacteriosis. Can Campylobacteriosis affect people? Yes, this bacteria can cause diarrhea, fever, and cramping. Symptomatic treatment generally leads to recovery. What if there is an outbreak? Cows are rarely clinically ill even if they carry Campylobacter. This bacteria is more important in terms of public health. For more information on Campylobacteriosis, see: http://www.who.int/inf-fs/en/fact255.html http://www.cdc.gov/ncidod/dbmd/diseaseinfo/campylobacter_g.htm http://vm.cfsan.fda.gov/~mow/chap4.html Leptospirosis CAUSE: Leptospirosis is a highly contagious bacterial infection, caused by bacteria from the subgroup Leptospira interrogans. Serovars hardjo, pomona, grippotyphosa and others have been associated with cattle. EFFECT: In cattle, signs can range from mild (lowered milk and calf production) to severe (abortions, stillbirths, and liver damage). After infection, the bacteria localize in the kidneys or reproductive organs, and are shed in urine. How is Leptospirosis spread? Leptospirosis is most commonly spread by contact with the urine of infected animals. It can also be transmitted by wildlife, such as rodents and birds. How can Leptospirosis be prevented? Vaccinate cattle at least annually. Avoid contact with wildlife and prevent access to contaminated streams or ponds. Can Leptospirosis affect people? Yes, humans are susceptible to all strains of the disease, though transmission requires close contact with the urine of infected animals. Thus, it is an occupation risk for farmers and veterinarians. Signs can range from mild to severe, and can be fatal if untreated, especially if renal or hepatic failure occurs. The most common symptoms are headaches, fever, rash, and malaise. What if there is an outbreak? Antibiotic treatment early in the course of the disease can be successful. Vaccination in the face of an outbreak can limit the extent of the infection in a herd. For more information on Leptospirosis, see: http://www.merckvetmanual.com/mvm/index.jsp?cfile=htm/bc/51200.htm&wo rd=Leptospirosis http://www.ianr.unl.edu/pubs/animaldisease/g417.htm http://www.hse.gov.uk/pubns/indg84.htm Photo: http://www.petprospects.com/Gallery/Mammals/Small_Pets/rats.htm Listeriosis CAUSE: Listeria monocytogenes is an extremely environmentally resistant bacterium that tolerates a wide range of temperatures. It grows between 39 and 111°F (4 and 44°C). EFFECT: Listeria that are ingested or inhaled tend to cause septicemia (blood infections), abortions, or encephalitis, but may cause no signs at all. It is most commonly seen as a disease of the nervous system in cattle and described as “circling” disease. Listeriosis can also affect sheep and goats. How is Listeriosis spread? Listeria are found in soil and water. Animals can carry the bacteria without showing any signs of disease, thereby serving as asymptomatic reservoirs. It is spread primarily through contaminated feed (spoiled silage may be a culprit) or fecal-oral transmission. How can Listeriosis be prevented? Do not feed spoiled silage. Baylage (bagged round bales) are more often contaminated with Listeria. Dairy and meat processing plants must follow strict hygiene to avoid contamination of products. Can Listeriosis affect people? Yes. Although it is killed by proper pasteurization, Listeria in the processing plant may contaminate previously pasteurized dairy products during packaging. Even so, as a food borne disease it is most commonly associated with non-pasteurized products. It can also be acquired through direct contact with aborted materials or tissues during necropsy. Pregnant women are particularly susceptible to infection. What if there is an outbreak? The disease tends to be sporadic. If feed is suspected as the source of the outbreak, switch to another feed and destroy the contaminated feed. Aggressive antibiotic treatment early in the course of the disease may be curative. For more information on Listeriosis, see: http://cattletoday.info/diseases/listerosis.htm http://www.cdc.gov/ncidod/dbmd/diseaseinfo/listeriosis_g.htm Rabies CAUSE: Rabies is caused by a virus that affects the central nervous system. EFFECT: Since rabies affects the brain, the most common signs are behavioral changes or paralysis. Animals can show nervousness, aggression, inability to walk, and excessive salivation. Nocturnal animals will be seen wandering about during the day. Cows will abruptly stop making milk. How is Rabies spread? Rabies is spread by contact with the saliva or blood of infected animals, most commonly by bites. Raccoons, foxes, skunks, and bats may carry rabies. Wild animals, other than bats, usually only pose an indirect threat to human health. How can Rabies be prevented? Vaccinate all pets and domestic livestock over 3 months of age in areas where rabies is endemic in wildlife. This includes all of Vermont. Rabies was reported in a donkey, a horse, and a cow in Vermont in 2002. Use caution if an animal exhibits unusual behavior. Can Rabies affect people? Yes, rabies can be fatal to humans when an exposure is not recognized and post-exposure vaccination is not obtained. What if there is an outbreak? Usually only sporadic cases occur, even in unvaccinated populations. If rabies is suspected, call your veterinarian. If human exposure has occurred, call your public health department to determine whether a post-exposure inoculation series is needed. Tissue from the back of the brain must be submitted to confirm whether an animal died of rabies. For more information on Rabies, see: http://www.who.int/inf-fs/en/fact099.html http://www.cdc.gov/ncidod/dvrd/rabies/default.htm http://www.merckvetmanual.com/mvm/index.jsp?cfile=htm/bc/102200.htm&w ord=Rabies West Nile Virus CAUSE: West Nile Virus (WNV) is a mosquito-borne virus. EFFECT: WNV causes encephalitis, which may be fatal, in birds, horses, and humans. Signs in horses include ataxia, muscle weakness, depression, twitching and death. How is West Nile Virus spread? Mosquitoes contract the virus from birds, and then spread the virus to other birds, animals, or humans. Mammals are considered dead-end hosts for the virus, meaning even if infected they are not directly contagious to other mammals. How can West Nile Virus be prevented? Avoid exposure to adult mosquitoes. Eliminate mosquito habitat. (See page 45.) Can West Nile Virus affect people? Yes. According to the Center for Disease Control and Prevention, there were 4156 reported cases of human WNV in 2002, with 284 fatalities. What if there is an outbreak? Currently, there is no treatment for WNV beyond general supportive therapy (hospitalization, intravenous fluids, respiratory assistance, etc.). For more information on West Nile virus, see: http://www.aphis.usda.gov/lpa/pubs/fsheet_faq_notice/fs_ahwnv.html http://www.cdc.gov/ncidod/dvbid/westnile/index.htm http://environmentalrisk.cornell.edu/wnv/ Photo: USDA ARS Image Gallery, used with permission. Brucellosis CAUSE: Brucellosis is caused by bacteria of the genus Brucella. Several species of Brucella can infect different species of animals. The main threat in the US is to cattle, bison, and pigs. This disease is not present in any herds in Vermont. EFFECTS: Brucellosis results in decreased milk production, abortion, infertility, and lameness which cause economic losses to cattle owners. How does Brucellosis spread? The disease is most commonly spread by contact with aborted fetuses, placental materials, or vaginal discharges from infected animals. Can Brucellosis affect people? Yes, in humans, the infection is known as “undulant fever” or “Bang’s disease” and has symptoms similar to severe influenza. Pasteurization of milk and cooking of meat prevent food-borne transmission of Brucellosis. How can Brucellosis be prevented? Livestock imported into Vermont must test negative for Brucellosis. Many herds still vaccinate replacement heifers— indicated by a tattoo and orange metal id tag in the right ear. What if there is an outbreak? An outbreak is unlikely since the disease has been nearly eliminated from the US. Vermont is certified free of Brucellosis. For more information on Brucellosis, see: http://www.aphis.usda.gov/lpa/pubs/fsheet_faq_notice/faq_ahbrucellosis.html Photo: Ron Nichols, USDA Photography Center, used with permission. Bovine Tuberculosis CAUSE: This disease is caused by Mycobacterium bovis or Mycobacterium tuberculosis. This disease is not present in any herds in Vermont. EFFECT: The classic lesion of tuberculosis (TB) is a tubercle, or tumor-like lump filled with thick white pus. Tubercles and associated lymph nodes can grow quite large. In cattle and primates, lesions are most commonly found in the lungs and regional lymph nodes; in deer and poultry, lesions are most common in the intestines. How is Bovine TB spread? Bovine TB can be spread through the air by infectious droplets contacting eyes or nasal mucus membranes; by eating bacteria in contaminated food or water; or by contacting infected carcasses that have not been disposed of properly. Can Bovine TB affect people? Yes, in rare cases, bovine TB can be transmitted from infected animals to humans. Pasteurization kills the causative organism in milk. How can Bovine TB be prevented? Livestock imported into Vermont must test negative for tuberculosis. What if there is an outbreak? An outbreak is unlikely since the disease has been nearly eliminated from the US. Vermont is certified free of tuberculosis. For more information on Bovine TB, see: http://www.aphis.usda.gov/lpa/pubs/fsheet_faq_notice/fs_ahtb.html For information on the situation in Michigan, see: http://www.bovinetb.com/Index.asp Bluetongue CAUSE: Bluetongue is caused by a virus spread by biting midges. EFFECTS: The disease most seriously affects sheep, which may die. Cattle generally do not show visible symptoms, but they carry the disease for months after infection. How is Bluetongue spread? The disease is not contagious, but is spread by Culicoides midges, also known as biting gnats or no-see-ums. Biting midges in the northeast US do not spread the virus. How can Bluetongue be prevented? Cattle are the main mammalian reservoir of Bluetongue. Serologic testing can detect infection. Can Bluetongue affect people? Humans are not affected by this disease. Sheep are primarily affected, however, goats, deer, and cattle (rarely) can be infected. What if there is an outbreak? Bluetongue is unlikely to become a problem in New England. However, ruminant animals imported into the state must be tested. For more information on Bluetongue, see: http://www.merckvetmanual.com/mvm/index.jsp?cfile=htm/bc/54300.htm&wo rd=bluetongue http://www.aphis.usda.gov/vs/nahps/bluetongue/ http://www.dpi.qld.gov.au/health/3943.html For picture of a biting midge, see: http://www.socgenmicrobiol.org.uk/JGVDirect/18705/Figs/F1_pg.htm Anaplasmosis CAUSE: Anaplasmosis in cattle is caused by an organism called Anaplasma marginale that invades and multiplies in red blood cells. EFFECT: Anaplasmosis causes anemia and eventually death if not treated early in the course of disease. How is Anaplasmosis spread? It is transmitted by ticks or horseflies, or equipment such as needles or dehorners that are used on more than one animal. How can Anaplasmosis be prevented? Testing of imported animals will prevent the introduction of this disease into Vermont. Can Anaplasmosis affect people? No. What if there is an outbreak? It is extremely unlikely that there would be an outbreak of Anaplasmosis in New England. For more information on Anaplasmosis, see: http://cattletoday.info/diseases/anaplasmosis.htm http://www.merckvetmanual.com/mvm/index.jsp?cfile=htm/bc/10401.htm&wo rd=anaplasmosis Psoroptic Mange CAUSE: The scab mite, Psoroptes ovis, is seen in range and feedlot cattle in the central and western states of the US. EFFECTS: Although Sarcoptic and Chorioptic mange as well as Psoroptic mange are reportable cattle, Psoroptic mange can do the most harm to the affected animal. Extreme itchiness usually begins on the shoulders or rump and is followed by scabbing and crusting. Untreated calves may die. Weight loss, decreased milk production, and increased susceptibility to other diseases may occur in affected cattle. How is Psoroptic mange spread? The mite spreads through direct contact between affected and non-affected animals. How can Psoroptes be prevented? Do not bring affected animals into your herd. Can Psoroptes affect people? No. What if there is an outbreak? Treatment dips or other treatment must be conducted under the supervision of an accredited or federal veterinarian. For more information on Psoroptic mange, see: http://www.merckvetmanual.com/mvm/index.jsp?cfile=htm/bc/72001.htm&wo rd=psoroptes Vesicular Stomatitis CAUSE: Vesicular Stomatitis (VS) is caused by an RNA virus. Its host range, in order of decreasing severity of disease, is horses, donkeys, mules, cattle, swine, and humans. EFFECTS: The disease is characterized by vesicular lesions on the tongue, oral mucosa, teats, or coronary bands of horses, cattle, and swine. (This picture at left is actually of lesions of Foot and Mouth Disease [FMD]). FMD and VS cannot be distinguished by clinical signs alone. How is Vesicular Stomatitis spread? VS can be spread by a number of insect vectors as well as mechanical transmission (through equipment used on more than one animal) and direct contact with affected animals. How can Vesicular Stomatitis be prevented? Follow all regulations for the importation of animals. Do not bring in animals from herds known to have been affected with VS in the past three months. Vermont is currently free of this disease. Can Vesicular Stomatitis affect people? People who handle infected animals also can become infected with VS by aerosol or direct contact. It causes an influenza-like illness in people. What if there is an outbreak? Prevent contact between affected and nonaffected animals, control insects to prevent vector transmission, and avoid fomite transmission through people or equipment. Proper disinfection of equipment will limit transmission. For more information on Vesicular Stomatitis see: http://www.aphis.usda.gov/oa/pubs/vsdairy.html Photo: USDA Photography Center, used with permission. Mad Cow Disease CAUSE: Mad Cow Disease is caused by the consumption of infected ruminant-derived protein in ruminant rations. The causative agent is believed to be a prion. This disease has not been found in the US. EFFECT: Mad Cow Disease, or Bovine Spongiform Encephalopathy (BSE), causes deterioration of the brain and eventual death. Affected animals show changes in temperament, lack of coordination, decreased milk production, decreased body weight, and, ultimately, death. How is BSE spread? BSE is spread by the consumption of nervous tissue from infected animals. Currently, there is no evidence that BSE can be spread by contact between animals. However, there is some evidence that cows may pass the infection to their calves in utero. How can BSE be prevented? Do not feed prohibited meat, bone meal, or other ruminant-derived byproducts to cattle. The ruminant to ruminant feeding ban is the best defense against acquiring and spreading this disease. Can BSE affect people? A variant form of Creutzfeldt-Jakob’s Disease has been linked with the BSE outbreak in Great Britain and Europe. What if there is an outbreak? If a case is identified, as in Canada in the spring of 2003, expect trace back and slaughter of all related animals and animals potentially fed contaminated feed. For more information on Mad Cow Disease, see: http://cattletoday.info/diseases/bovine_spongioform_encephalopath.htm http://www.aphis.usda.gov/lpa/pubs/fsheet_faq_notice/fs_ahbse.html Chronic Wasting Disease CAUSE: Chronic Wasting Disease (CWD) is believed to be caused by a prion, similar to scrapie and Mad Cow Disease, that only affects deer and elk. EFFECT: CWD is a progressive, degenerative disease of the brain. Signs include loss of body condition, excessive salivation, behavioral changes, increased drinking and urinating, and eventually, death. How is CWD spread? Animals can contract the disease from one another or from a contaminated environment, but the exact mechanism of transmission is unknown. How can CWD be prevented? Elk and deer farmers should take part in CWD surveillance and control programs. Game hunters should look for signs of CWD in wild deer and elk, and report these signs to the proper authorities. Can CWD affect people? To date, no humans have been infected with CWD. However, the Center for Disease Control and Prevention deems it wise to avoid food products from infected animals. What if there is an outbreak? There is no treatment for CWD. Depopulation is the preferred method of control. For more information on CWD, see: http://www.aphis.usda.gov/vs/nahps/cwd/ Photo: Keith Weller, USDA ARS Image Gallery, used with permission. Mad Cow Disease vs. Foot and Mouth Disease Although these two diseases have very little in common, they are commonly mixed up by the general public. Here’s a run down of their major differences. Feature Mad Cow FMD Causative agent Infectivity Transmission Incidence of disease Incidence of death Time of illness relative to infection Visible lesions Immune response Humans affected? Prion Not contagious Transmissible via feed Low morbidity 100% mortality Virus Highly contagious Transmissible via aerosol High morbidity Low mortality Long incubation No gross lesions Not detectable Public health concern Short incubation Gross lesions present Strong host response Rare public health issue Transmissable Spongiform Encephalopathies (TSEs) Mad Cow Disease, Chronic Wasting Disease of elk and deer, and Scrapie of sheep and goats are all classified as transmissible spongiform encephalopathies (TSEs)—“Transmissible” because they are contagious (although not highly); “Spongiform” because the lesions in the brain leave microscopic “holes;” “Encephalopathy” because the disease primarily affects the central nervous system, i.e., the brain. Historically, these diseases could not be diagnosed in the live animal because there is no measurable immune response. Examination of brain tissue obtained immediately after slaughter was required. Newer tests allow examination of “deteriorated” tissue samples for the abnormal prion protein (PrPres) that is resistant to degradation by enzymes. Tests have been under development to detect PrPres in tissue from live animals, including third eyelid tissue, blood, and cerebrospinal fluid (CSF). Another test used to confirm the presence of infective material is a mouse assay, which takes over two years to complete, and may miss low levels of infection. The USDA APHIS is determined to eliminate TSEs from livestock in the US. The current scrapie control program has been in effect since 1992. Chronic Wasting Disease is under surveillance and Mad Cow Disease has not been found in this country although slaughter plant surveillance is ongoing.