Medicines Policy - Gunthorpe Primary School
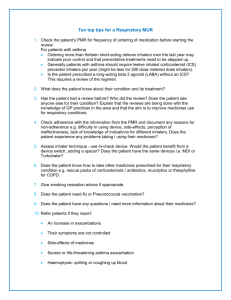
advertisement

MEDICINES IN SCHOOL POLICY Reviewed February 2013 The aim of this policy is to effectively support individual children with medical needs and to enable pupils to achieve regular attendance. This has been revised within Acts of Parliament and follows all legal requirements. Parents should not send a child to school if they are unwell Gunthorpe School is not an extension of Accident & Emergency. If your child sustains an injury it is your duty of care to ensure you take your child to their local A + E or GP. We can only deal with first aid issues that occur on site. Where a child has a long term medical need a written health care plan will be drawn up with the parents, health professionals and designated school staff. Parents must inform the school and GOSH Club about any particular needs before a child is admitted or when a child first develops a medical need. A care plan will be drawn up. RESPONSIBILITIES Parents and Carers If the school staff agree to administer medication on a short term or occasional basis, the parent(s) are required to complete a Consent Form Verbal instructions will not be accepted. If it is known that pupils are self-administering medication in school on a regular basis, a completed Consent Form is still required from the parent(s). For administration of emergency medication, a Care Plan must be completed by the parent(s) in conjunction with the school nurse and school staff. Minor changes to the Care Plan can be made if signed and dated by the parent(s). If, however, changes are major, a new Care Plan must be completed. Care Plans should be reviewed annually. The parent(s) need to ensure there is sufficient medication and that the medication is in date. The parent(s) and carer(s) must replace the supply of medication at the request of relevant school/health professional. Medication should be provided in an original container with the following, clearly shown on the label: • Child’s name, date of birth; • Name and strength of medication; • Dose; • Expiry dates whenever possible; • Dispensing date/pharmacists details. School Staff Some teaching unions advise school staff not to administer medication to pupils, the unions also accept that sometimes it is done; if so they advise that the teacher has access to information, training and that appropriate insurance is in place. In practice, head teachers may agree that medication will be administered or allow supervision of self-administration to avoid children losing teaching time by missing school. Each request should be considered on individual merit and school staff have the right to refuse to be involved. It is important that school staff who agree to administer medication understand the basic principles and legal liabilities involved and have confidence in dealing with any emergency situations that may arise. Regular training relating to emergency medication and relevant medical conditions should be undertaken. HEALTH CARE PLANS The Health care Plan should be completed by Parent(s), designated school staff and health professionals.. It should include the following information, and an example is in annex 1. details of a child’s condition special requirement e.g. dietary needs, pre-activity precautions and any side effects of the medicines what constitutes an emergency what action to take in an emergency what not to do in the event of an emergency who to contact in an emergency the role the staff can play STAFF TRAINING When training is delivered to school staff, the school must ensure that a training record is completed for inclusion in the Health and Safety records. This will be primarily appropriate for the use of Epipens (for allergies), although other conditions/procedures may also be included from time to time. This is for both insurance and Audit purposes. STORAGE When items need to be available for emergency use, e.g. asthma pumps and Epipens, they may be kept in a designated room according to the size/layout of the building, or with the pupil, as appropriate. It is not necessary for a locked cupboard to be used, but such items should be easily available for the use of pupils and/or staff. When prescription items are held by the school for administration by school staff they should be stored in a fixed lockable cupboard/cabinet, with restricted access to keys. CLASS 1 and 2 DRUGS When Class 1 and 2 drugs (primarily “Ritalin” prescribed for Attention Deficit Syndrome) are kept on school premises, a written stock record is also required in order to comply with the Misuse of Drugs Act legislation. This should detail the quantities kept and administered, taken and returned on any educational visit, and returned to the parent/carer, e.g. at the end of term. ANTIBIOTICS Parent(s) should be encouraged to ask the GP to prescribe an antibiotic which can be given outside of school hours wherever possible. Most antibiotic medication will not need to be administered during school hours. Twice daily doses should be given in the morning before school and in the evening. Three times a day doses can normally be given in the morning before school, immediately after school (provided this is possible) and at bedtime. If there are any doubts or queries about this please contact your school nurse. It should normally only be necessary to give antibiotics in school if The dose needs to be given four times a day, in which case a dose is needed at lunchtime. Parent(s) must complete the Consent Form and confirm that the child is not known to be allergic to the antibiotic. The antibiotic should be brought into school in the morning and taken home again after school each day by the parent. (Older children may bring in and take home their own antibiotics if considered appropriate by the parent(s) and teachers.) Whenever possible the first dose of the course, and ideally the second dose, should be administered by the parent(s). All antibiotics must be clearly labelled with the child’s name, the name of the medication, the dose and the date of dispensing. In school the antibiotics should be stored in a secure cupboard or where necessary in a refrigerator. Many of the liquid antibiotics need to be stored in a refrigerator – if so; this will be stated on the label. Some antibiotics must be taken at a specific time in relation to food. Again this will be written on the label, and the instructions on the label must be carefully followed. Tablets or capsules must be given with a glass of water. The dose of a liquid antibiotic must be carefully measured in an appropriate medicine spoon, medicine pot or oral medicines syringe provided by the parent. The appropriate records must be made. Record keeping. If the child does not receive a dose, for whatever reason, the parent must be informed that day. ANALGESICS (PAINKILLERS) For pupils who regularly need analgesia (e.g. for migraine), an individual supply of their analgesic should be kept in school. It is recommended that school does not keep stock supplies of analgesics e.g. paracetamol (in the form of soluble), for potential administration to any pupil. Parental consent must be in place. CHILDREN SHOULD NEVER BE GIVEN ASPIRIN OR ANY MEDICINES CONTAINING ASPIRIN. OVER THE COUNTER MEDICINE (EG HAYFEVER REMEDIES) These should be accepted only in exceptional circumstances, and be treated in the same way as prescribed medication. Parent(s) must clearly label the container with child’s name, dose and time of administration and complete a Consent Form. DISPOSAL OF MEDICINE Parents are responsible for ensuring that date expired medicines are returned to a pharmacy for safe disposal. They should collect medicines held by the school at the end of each term. RESIDENTIAL VISITS On occasion it may be necessary for a school/centre to administer an “over the counter” medicine in the event of a pupil suffering from a minor ailment , such as a cold, sore throat while away on an Educational Visit . In this instance the parental consent form ( EV4 ) will provide an “if needed” authority, which should be confirmed by phone call from the Group Leader to the parent/carer when this is needed, and a written record is kept with the visit documentation. This action has been agreed by the Council’s Insurance and Legal Sections. REFUSING MEDICINE When a child refuses medicine the parent should be informed the same day and be recorded accordingly. Staff cannot force a child to take any medicine. SELF MANAGEMENT Children are encouraged to take responsibility for their own medicine from an early age. A good example of this is children keeping their own asthma reliever. TRAVEL SICKNESS It has also been agreed by the Council’s Insurance and Legal Sections that, in the event of a pupil suffering from travel sickness (by coach or public transport) the following procedure may apply: DAY VISITS (e.g. to a museum or exhibition) The pupil should be given the appropriate medication before leaving home, and when a written parental consent is received he/she may be given a further dose before leaving the venue for the return journey (in a clearly marked sealed envelope with childs details, contents, and time of medication). Medication is to be kept in the charge of a named member of staff, and the parental consent is signed by that staff member before inclusion in the visit documentation. GUIDELINES FOR THE ADMINISTRATION OF EPIPEN BY SCHOOL STAFF An Epipen is a preloaded pen device, which contains a single measured dose of adrenaline (also known as epinephrine) for administration in cases of severe allergic reaction. An Epipen is safe, and even if given inadvertently it will not do any harm. It is not possible to give too large a dose from one dose used correctly in accordance with the Care Plan. An Epipen can only be administered by school staff that have been designated as appropriate by the head teacher and who has been assessed as competent by the school nurse or doctor. Training of designated staff will be provided by the school nurse or doctor and a record of training undertaken will be kept by. Training will be updated at least once a year. 1. There should be an individual Care Plan and Consent Form, in place for each child. These should be readily available. They will be completed before the training session in conjunction with parent(s), school staff and doctor/nurse. 2. Ensure that the Epipen is in date. The Epipen should be stored at room temperature and protected from heat and light. It should be kept in the original named box. 3. The Epipen should be readily accessible for use in an emergency and where children are of an appropriate age; the Epipen can be carried on their person. 4. Expiry dates and discoloration of contents should be checked by the school nurse termly. If necessary she may ask the school doctor to carry out this responsibility. The Epipen should be replaced by the parent(s) at the request of the school nurse/school staff. 5. The use of the Epipen must be recorded on the child’s Care Plan, with time, date and full signature of the person who administered the Epipen. 6. Once the Epipen is administered, a 999 call must be made immediately. If two people are present, the 999 call should be made at the same time of administering the Epipen. The used Epipen must be given to the ambulance personnel. It is the parent’s responsibility to renew the Epipen before the child returns to school. 7. If the child leaves the school site e.g. school trips, the Epipen must be readily available. GUIDELINES FOR MANAGING ASTHMA People with asthma have airways which narrow as a reaction to various triggers. The narrowing or obstruction of the airways causes difficulty in breathing and can usually be alleviated with medication taken via an inhaler. Inhalers are generally safe, and if a pupil took another pupil’s inhaler, it is unlikely there would be any adverse effects. School staff, who have volunteered to assist children with inhalers, will be offered training from the school nurse. 1. If school staff are assisting children with their inhalers, a Consent Form from parent(s) should be in place. Individual Care Plans need only be in place if children have severe asthma which may result in a medical emergency. 2. Inhalers MUST be readily available when children need them. Pupils should be encouraged to carry their own inhalers. If the pupil is too young or immature to take responsibility for their inhaler, it should be stored in a readily accessible safe place e.g. the classroom. Individual circumstances need to be considered, e.g. in small schools; inhalers may be kept in the school office. 3. It would be considered helpful if parent(s) could supply a spare inhaler for children who carry their own inhalers. This could be stored safely at school in case the original inhaler is accidentally left at home or the child loses it whilst at school. This inhaler must have an expiry date beyond the end of the school year. 4. All inhalers should be labelled with the child’s name. 5. Some children, particularly the younger ones, may use a spacer device with their inhaler; this also needs to be labelled with their name. The spacer device needs to be sent home at least once a term for cleaning. 6. School staff should take appropriate disciplinary action if the owner or other pupils misuse inhalers. 7. Parent(s) are responsible for renewing out of date and empty inhalers. 8. Parent(s) should be informed if a child is using the inhaler excessively. 9. Physical activities will benefit pupils with asthma, but they may need to use their inhaler 10 minutes before exertion. The inhaler MUST be available during PE and games. If pupils are unwell they should not be forced to participate. 10. If pupils are going on offsite visits, inhalers MUST still be accessible. 11. It is good practice for school staff to have a clear out of any inhalers at least on an annual basis. Out of date inhalers, and inhalers no longer needed must be returned to parent(s). 12. Asthma can be triggered by substances found in school e.g. animal fur, glues and chemicals. Care should be taken to ensure that any pupil who reacts to these are advised not to have contact with these. GUIDELINES FOR MANAGING HYPOGLYCAEMIA (HYPO’S OR LOW BLOOD SUGAR) IN PUPILS WHO HAVE DIABETES Diabetes is a condition where the person’s normal hormonal mechanisms do not control their blood sugar levels. In the majority of children the condition is controlled by insulin injections and diet. It is unlikely that injections will need to be given during school hours, but some older children many need to inject during school hours. All staff will be offered training on diabetes and how to prevent the occurrence of hypoglycaemia. This might be in conjunction with paediatric hospital liaison staff or Primary Care Trust staff. Staff who have volunteered and have been designated as appropriate by the head teacher will administer treatment for hypoglycaemic episodes. To prevent “hypo’s” 1. There should be a Care Plan and Consent Form in place. It will be completed at the training sessions in conjunction with staff and parent(s). Staff should be familiar with pupil’s individual symptoms of a “hypo”. This will be recorded in the Care Plan. 2. Pupils must be allowed to eat regularly during the day. This may include eating snacks during class time or prior to exercise. Meals should not be unduly delayed e.g. due to extra curricular activities at lunchtimes or detention sessions. Off site activities e.g. visits, overnight stays, will require additional planning and liaison with parent(s). To treat “hypo’s” 1. If a meal or snack is missed, or after strenuous activity or sometimes even for no apparent reason, the pupil may experience a “hypo”. Symptoms may include sweating, pale skin, confusion and slurred speech. 2. Treatment for a “hypo” might be different for each child, but will be either dextrose tablets, or sugary drink, chocolate bar or hypostop (dextrose gel), as per Care Plan. Whichever treatment is used, it should be readily available and not locked away. Many children will carry the treatment with them. Expiry dates must be checked each term, either by a member of school staff or the school nurse. 3. It is the parent’s responsibility to ensure appropriate treatment is available. Once the child has recovered a slower acting starchy food such as biscuits and milk should be given. If the child is very drowsy, unconscious or fitting, a 999 call must be made and the child put in the recovery position. Do not attempt oral treatment. Parent(s) should be informed of “hypo’s” where staff have issued treatment in accordance with Care Plan. If Hypostop has been provided The Consent Form should be available. Hypostop is squeezed into the side of the mouth and rubbed into the gums, where it will be absorbed by the bloodstream. The use of Hypostop must be recorded on the child’s Care Plan with time, date and full signature of the person who administered it. It is the parent’s responsibility to renew the Hypostop when it has been used. DO NOT USE HYPOSTOP IF THE CHILD IS UNCONSCIOUS. Reviewed February 2013 ANNEX 1 Health Care Plan Request for child to carry his/her medicine Parental request for administration of medicines Health Care Plan Name of school/setting Child’s name Group/class/form Date of birth Child’s address Medical diagnosis or condition Date Review date Family Contact Information Name Phone no. (work) (home) (mobile) Name Phone no. (work) (home) (mobile) Clinic/Hospital Contact Name Phone no. G.P. Name Phone no. Describe medical needs and give details of child’s symptoms Daily care requirements (e.g. before sport/at lunchtime) Describe what constitutes an emergency for the child, and the action to take if this occurs Follow up care Who is responsible in an emergency (state if different for off-site activities) Form copied to Request for child to carry his/her medicine THIS FORM MUST BE COMPLETED BY PARENT/GUARDIAN If staff have any concerns discuss request with school healthcare professionals Name of School/Setting: Child’s Name: Group/Class/Form: Address: Name of Medicine: Procedures to be taken in an emergency: Contact Information Name: Daytime Phone No: Relationship to child: I would like my son/daughter to keep his/her medicine on him/her for use as necessary. Signed: Date: If more than one medicine is to be given a separate form should be completed for each type of medicine. Parental Request for School to Administer Medicine The school will not give your child medicine unless you complete and sign this form. Name of Child: Date of Birth: Year Group Medical condition/illness: Medicine Name/Type of Medicine (as described on the container): Dosage and method: Timing: Special Precautions: Are there any side effects that the school/setting needs to know about? Self Administration: Yes / No Contact Details Name: Daytime Telephone No: Relationship to Child: I agree to conditions overleaf Signed Note to school staff - please keep completed forms (delete as appropriate) Medicines in school When children are ill we feel the best place for them is at home. Teacher organisations stress that teachers should on no account administer medicines to children. We do however acknowledge our roll in ‘loco parentis’ and will accept some medicines but only with strict provisos: Asthma inhalers should be named and kept with the class teacher but children should know how to use them. Medicines can only be administered during break and lunch time. The school cannot accept responsibility for a child missing a dosage or leaving their medication at school. We accept that children often have to take antibiotics for a short period. We suggest that where necessary one measured dose is sent for lunchtime, which together with doses before and after school usually achieves the required prescription. We do not think painkillers are appropriate in school unless required as treatment by a doctor. All medicines must be handed to the class teacher, named and accompanied by clearly written instructions as to timing and dosage. School should be notified of specific cases of allergy and health problems. So that we can keep our medical records up to date. This policy is reviewed by governors and communicated to staff and parents on an annual basis and can also be found on the school website