Abstract - UWE Research Repository
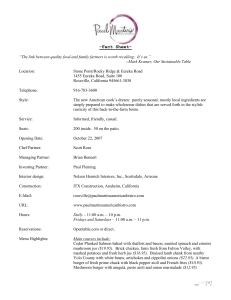
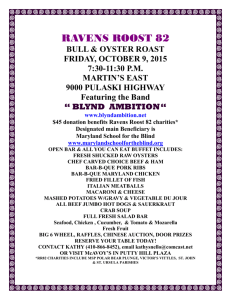
advertisement

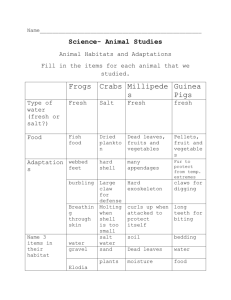
Manuscript Title: Evaluation of a Method Allowing Preservation of Fresh Lymph Nodes for Flow Cytometric Immunophenotyping. Running Title: Preservation of Fresh Lymph Nodes for FCI. Authors: Ms. Patricia Brincat MSc. Haematology (University of the West of England) Haematology Laboratory Pathology Department Mater Dei Hospital Malta Dr. James Degaetano Histopathology Laboratory Pathology Department Mater Dei Hospital Malta Dr. Craig Donaldson Centre for Research in Biosciences Department of Applied Sciences University of the West of England, Bristol United Kingdom Corresponding Author: Patricia Brincat Haematology Laboratory Pathology Department Block B, Level 1, Mater Dei Hospital, Tal-Qroqq, MSIDA MALTA MSD 2020 Tel: (+356) 25456350 Fax: (+356) 25456359 E-mail: patricia.farrugia@gov.mt Key Words: Flow Cytometric Immunophenotyping; Haematolymphoid Neoplasia; Lymph Nodes; Cryopreservation Abstract Background: Flow cytometric immunophenotyping (FCI) of lymph nodes (LN) requires fresh unfixed tissue, with analysis being carried out within few hours post surgery. This study evaluated a novel method for fresh LN preservation, in order to allow histomorphology-based FCI. Methods: This study was carried out prospectively on 30 LN with suspected involvement by Haematolymphoid Neoplasms (HLN). FCI was performed on each fresh and post cryopreserved LN cell suspension. Percentage positivities (PP) and Mean Fluorescent Intensities (MFI) were calculated on both preparations for a combination of T and B-lymphoid antigens together with viability. Results: The cryopreservation method applied within this study did not affect significantly PP and had minor impact on MFI of the mentioned antigens. Overall there was minimal decrease in PP and MFI on the cryopreserved cells when compared to fresh cells, for most antigens with only a mild increase in apoptotic cells. However these changes were not diagnostically significant, since both reactive processes and HLN present within cryopreserved LN could be identified and differentiated. Viability was more than 75% for all cryopreserved LN composed of haematolymphoid cells. Conclusions: The method presented in this study confers the possibility of storing fresh LN biopsies for later FCI, thus allowing a morphology-based immunophenotypic approach. This would allow a more sensitive, specific and cost-effective management of LN specimens, whilst maintaining the important benefits provided by FCI. Key Terms: Flow Cytometric Immunophenotyping; Haematolymphoid Neoplasia; Lymph Nodes; Cryopreservation. Introduction Immunophenotyping of Haemotolymphoid Neoplasms HLN presenting in solid tissues such as lymph nodes (LN) is an important aspect in the identification and classification of these malignancies. The major drawback of FCI on LN is the requirement of fresh, unfixed tissue1, with FCI being performed prior to histomorphological evaluation. Lack of histomorphological guidance necessitates the use of a broad monoclonal antibody (moab) panel with possible waste of reagents, instrument and technologist’s time resulting in increased expenses to the patient and the health care system. Additionally, FCI may be carried out unnecessarily since the panel selected may not be useful in diagnosing the patient’s medical condition2,3. For FCI to be cost effective and efficient, an initial morphological evaluation of the tissue should ideally precede FCI, providing specific indications on the need for FCI and also a morphology-based panel selection. The Clinical and Laboratory Standards Institute (CLSI) guidelines (2007)4 state that any chemically fixed tissue would be unsuitable for FCI. Such pre-requisite implies that tissue samples have to be assayed within a few hours after surgery. It is not recommended to postpone FCI on fresh tissue until after the histological examination is complete, since time delay adversely affects cell viability5. Histopathological and immunohistochemical analysis of LN may be sufficient for the diagnosis of HLN. However FCI may still be required particularly for those morphologically challenging neoplasms. Identification of clonal B-cell populations can also prove difficult by immunohistochemistry due to nonspecific staining of kappa and lambda light chains. The aim of this study is to develop a method to preserve cells from fresh LN tissue for FCI, mainly for the detection of HLN, thus allowing a morphology based approach. This study will evaluate if such a method impacts on antigen detection, both quantitative (percentage positivity), and also qualitative (antigenic expression intensity), together with overall cell viability. Materials and Methods Specimens: A prospective study was carried out on 30 fresh, consecutive LN from patients with suspicion of HLN, arriving at the Histopathology Laboratory, Mater Dei Hospital (Malta). No specific selection criteria were applied and all fresh LN were included in the study. Once surgically removed, LN reached the laboratory within few hours post-surgery. Fresh LN were transported to the laboratory wrapped in sterile saline-soaked gauze. These were cut transversely and excessive fat was trimmed from the periphery. Tissue Processing: The tissue section for FCI was suspended in RPMI 1640 medium (Sigma-Aldrich). Cells from the tissue were recovered in RPMI media by gentle dissociation using a scalpel. The homogenate was filtered through a 100µm wire mesh; cells washed once in 2.0ml RPMI, centrifuged at 1800g for 3 minutes and resuspended in fresh RPMI. Each suspension was divided into two tubes; one to be stained directly by moab (cell count 10-12 x 109/L) and another to be cryopreserved (cell count 12-15 x 109/L). Cryopreservation of single cell suspension: Cell suspension to be cryopreserved and a cryovial were placed on an ice block and 200µL of RPMI were added to the cells. Then 200µL of cold Fetal Calf Serum (FCS, Gibco) were added to the cells. Six hundred (600µL) of 20% of dimethyl sulfoxide (Sigma Aldrich) were added drop wise to the cells swirling the tube continuously while keeping the cells cool. The cell suspension was then transferred to the cryovial and frozen to -80°C using a Cryo 1°C freezing container (Nalgene) filled up with isopropyl alcohol, which provided repeatable, -1°C/minute cooling rate. The frozen cells were stored at 80°C for a minimum of 10 days and a maximum of 20 days. Cells were not subjected to any lysing agent. Thawing of single cell suspension: The cryovial containing the frozen cell suspension was placed in a 37°C waterbath for rapid thawing. Once thawed, cells were transferred to a 15ml tube and suspended in thawing medium (RPMI enriched with FCS). To approximately 2.0mL of cell suspension, 10ml of thawing medium were added drop wise. The thawed cells were then washed once in RPMI, centrifuged at 1800g for 3 minutes and resuspended in cell wash (cell count 12-15x109/L). Cells were ready for moab staining and FCI as described below. Monoclonal antibody staining of single cell suspensions and FCI: Cell suspensions were stained with 3 colour fluorochrome-conjugated antibodies (Table 1). Each cell suspension was tested for viability utilising 7-Aminoactinomycin D (7-AAD) and an isotype control was run with each sample (IgG1FITC/IgG2aPE). All antibodies, viability dye and isotype control were obtained from Becton Dickinson Biosciences (BD). Tubes were analysed on a 4 colour, dual-laser FACSCalibur FC, (BD Immunocytometry Systems, San Jose, CA). For each sample 10,000 events were acquired and analysed using Cell Quest Pro software (BD). The flow cytometer was calibrated before each LN analysis using BD Calibrite 3 Beads, thus ensuring uniformity in day-to-day analysis. Percentage Positivity: Flow cytometric analysis of LN-derived cells was carried out for identification of the phenotypic properties and viability of haematolymphoid cells. For each LN, FCI was performed on both fresh and cryopreserved cells and results compared. Percentage positivity (PP) was obtained using low Side Scatter (SSC)/CD45 gating for all antigens except kappa/lambda, where SSC/CD19 was used. Mean Fluorescent Intensity: Quantification of antigen expression intensity was calculated using the Mean Fluorescence Intensity (MFI) for all the antigens, on both fresh and cryopreserved cells. Antigen expression intensity was calculated as the mean fluorescence, along a linear scale and represented as histogram expressing MFI. Intensity values were calculated on low SSC/CD45 lymphocyte gate for all antigens except kappa and lambda, which were calculated on low SSC/CD19 lymphocyte gate. Statistical Analysis Statistical Analysis was carried out using SPSS v11.01 software. The degree of linear correlation between fresh and cryopreserved was carried out using Pearson’s Correlation Coefficient. The paired t-test was used to evaluate the difference between results obtained on fresh and cryopreserved samples (p-value of <0.05 was taken as significant difference between the two methods). The Intra Class Correlation (ICC) was used as a measure of agreement between the two methods (ICC value of >0.7 considered as an agreement). Results Out of the 30 LN anaylsed fresh and post cryopreservation, 28 had a population of more than 75% of the total cells expressing strong CD45 and low SSC, with variable presence of CD45 negative cells, with variable presence of CD45 negative cells including epithelial, non haematological cells. The other 2 LN had a population with low CD45 and high SSC, compatible with non-haemopoietic cells. The latter were diagnosed exclusively by histomorphology and IHC, since the study was not intended to investigate antigenic expression on non-HLN, the data obtained from such LN was excluded from any statistical analysis carried out in relation to T and B-lymphoid antigens. Antigenic expressions for the LN analysed can be seen in Table 4. CD45 Antigenic Expression Correlation analysis of CD45 PP showed linear correlation between fresh and cryopreserved cells (r: 0.849, p: <0.001). CD45 showed a statistically significant difference between fresh and cryopreserved cells (p: 0.003), with -7.03% mean difference (Figure 1). However measure of agreement analysis, revealed an ICC value of 0.7543, indicating constant agreement in expression of this antigen between the two preparations. MFI for CD45 on fresh cell suspensions correlated very well with that obtained from cryopreserved cells (r: 0.766, p: <0.001). No statistically significant difference was seen in the MFI of CD45 between the fresh and cryopreserved analysis (p-value: 0.621). Additionally, measurements of agreement showed that CD45 MFI on fresh cells consistently agreed with MFI on cryopreserved cells (ICC: 0.7653), on both reactive and neoplastic LN. B and T-Lymphoid Antigenic Expressions on Fresh and Cryopreserved LN Surface antigens CD4/CD8; CD3/CD5; CD19/CD10; CD20/CD23 were quantified as PP out of the total CD45 positive/low SSC cells. Kappa/lambda were quantified as PP out of the total CD19 positive/low SSC cells. Correlation analysis showed a linear relationship between PP for the antigens tested on both fresh and cryopreserved LN (CPL) (Table 2). Measure of agreement analysis on PP of the above antigens showed strong agreement between the two methods (Table 2).The MFI of all antigens was not markedly affected by cryopreservation since correlation analysis and measure of agreement analysis showed that MFI values obtained on fresh cell suspensions correlated very well with those obtained on cryopreserved cells (Table 3). Viability Viability on the fresh cells was between 75 and 96% (mean 88.2%) on all cases except one involved with metastatic tumour. Viability post thawing was between 70 and 94% (mean 83.5). Correlation analysis carried out to assess the viability of cells within fresh and CPL suspensions showed that there was remarkable correlation between the two preparations (r: 0.882 and p: <0.001). Statistical analysis carried out to assess significant difference between the viability on fresh and cryopreserved cells showed a statistically significant difference (p: 0.004). However measure of agreement analysis, gave an ICC value of 0.8166, clearly demonstrating strong agreement between the two methods. Discussion Lymphoma diagnosis requires a multi disciplinary approach and FCI has proved to play a critical role in antigen identification and lineage assignment together with providing diagnostic and prognostic information. The fact that FCI of LN has to be carried out on fresh, unfixed tissue entails that analysis is performed within a few hours post surgery. The possibility of storing fresh LN biopsies while maintaining intact the phenotypic properties of its constituents has important advantages. Primarily it allows a morphology-based immunophenotypic approach, leading to a more sensitive, specific and cost-effective management. This study evaluated a method by which fresh LN can be preserved for the time necessary for histological examination to be ready, so that a more directed immunophenotypic approach can be taken. Lymphocyte Antigenic Expression CD45 expression showed good correlation between fresh and cryopreserved cells, with minimal increase in percentage positivity between CPL and fresh as expected, since the CPL cell suspension had a cell count higher (12-15 x 109/L) than the fresh LN cell suspension (10-12 x 109/L). Additionally cryopreservation did not significantly compromise the expression intensity of CD45. Such findings are of utmost importance since CD45 is considered to have a central role in FCI investigating HLN, due to its ability to differentiate between cells of haempoietic origin from non haemopoietic ones and also indicates the stage of maturation of the cells. Studies have also outlined the important role of CD45 MFI in differentiating between diagnostically challenging mature lymphoid neoplasms, such as CLL and MCL. Although these two B-cell neoplasms have distinct phenotypic characteristics, some cases may present with phenotypic shifts making differential diagnosis problematic. The typical phenotype of MCL is the co-expression of CD5/CD19/CD20 and lack CD23, however atypical CLL may also present with such phenotype. Therefore CD45 MFI could be used to differentiate between these two neoplasms (Carulli et al 2008) 6. Within this study results demonstrate that cryopreservation (1) had no substantially adverse effects on CD45 expression and intensity and (2) had minimal impact on cell loss. The intact expression of this marker confers the possibility that this antigen is used as a gating marker together with differentiating cellular ontogeny and identifying neoplastic phenotypes of cells. Within this study CD45 was used as a gating marker together with Side Scatter (SSC) (Figure 3). The cryopreservation method applied within this study had no major effects on the light scatter parameters, both forward scatter and side scatter. B-cell and T-cell Antigens FCI of cryopreserved cell suspensions showed patterns very similar to FCI carried out directly on fresh tissue. Although highly correlated CD10 PP showed a significant difference between the fresh and cryopreserved results (p: 0.07). This could be attributed to the fact that most LN examined had very low percentage of CD10 positive cells (0%-34%, mean: 9.6%). This difference did not impact on diagnosis of HLN on CPL (Figure 3). In fact the LN involved with Follicular Lymphoma had a CD10 positivity of 34% on fresh and 27% on CPL. Alternatively, PP for all B-cell antigens including CD10 showed strong agreement between both methods. Excellent correlation in PP between fresh and cryopreserved cells was seen for all T-lymphocyte antigens. Mean Fluorescent Intensity MFI for the different antigens analysed in this study were evaluated in order to assess whether cryopreservation affected significantly cellular antigen quantification. Correlation analysis showed that there is linear relationship between MFI obtained by the two methods. Difference analysis for MFI between fresh and cryopreserved cells showed no significant difference for all B-lymphoid antigens, except for CD23 (p: 0.041). These results illustrate that MFI are higher on the fresh cells and the cryopreservation/thawing process tends to lower MFI of CD23, as was also reported by Deneys et.al., (7) post cryopreservation of peripheral blood. Although a discrepancy was observed on CD23 MFI between the two preparations, such difference did not impact in any way on the final interpretation of both reactive and neoplastic LN. Measurement of agreement in MFI for all B-lymphoid antigens showed reproducibility between fresh and cryopreserved antigenic expression, however a lack of agreement was observed for CD19 and kappa analysis. Such a disagreement in CD19 MFI may have a diagnostic effect, as reported by several publications which outlined the importance of CD19 intensity expression for differentiating HLN8,9,10. Light chain analysis on both fresh and CPL gave very distinct patterns and were interpretation was very clear. The difference in MFI seen for kappa did not interfere in any way in the final interpretation and clonality could be established in both reactive process and also when there was light chain restriction in cases of HLN. T-lymphoid antigens, CD4 and CD8 also seem to be down regulated by cryopreservation, and this may impact on the diagnosis of T-cell HLN. However PP of the latter were unaffected by the method and therefore the impact on diagnosis and differentiation of T-cell neoplasia may be minimal. Viability Good correlation and strong agreement in cell viability was obtained between fresh and CPL suspensions. The significant difference seen between the two preparations (p: 0.004) is probably due to some inevitable loss in cell viability, induced by the cryopreservation process. Guidelines issued by the CLSI (4) recommend cell viability of more than 75% for reliable immunophenotypic analysis. The results obtained from this study show that the cryopreservation method applied maintains haemopoietic cell viability, a crucial feature for reliable FCI of HLN. Such findings provide evidence that cryopreservation is a reliable method, suitable for fresh LN cell suspensions and has minimal impact on both T and B-lymphoid lineages, light chain expression detection and CD45 analysis. MFI values can be successfully evaluated and utilized on the cryopreserved cells for most antigens. Viability is maintained up to the critical standards required for reliable diagnostic FCI. No differences were observed in the expression of the different markers between reactive and neoplastic processes. Since the number of HLN neoplasia included in this study is relatively small, the method could be applied to investigate if it has any effect on antigenic expression exclusively on HLN. Although the current study investigated fresh unfixed lymph node tissue, when the method was applied to fresh tonsils, antigenic preservation was also maintained and both PP and MFI correlated very well. Such data was not included because the sample size for other lymphoid tissue biopsies is too low. The method investigated in this study eliminates the use of a broad panel of antibodies. Having histomorphological and immunohistochemical guidance on the presence and the possible type of HLN enhances the sensitivity and specificity of the technique, limiting costs and time employed to reach a final diagnosis. Another major advantage of a morphology-based FCI approach is that such an analysis is carried out only when indicated. In conclusion, this study showed that cryopreservation of cell suspensions obtained from fresh LN is a reliable method which does not compromise the relative percentages of B and T-lymphoid markers and the total number of cells. Antigenic expression intensities were also maintained for most markers tested and can eventually be identified and quantified by multicolor FCI. The results obtained within this study clearly indicate that the two methods are interchangeable, thus conferring the possibility of storing fresh LN specimens, allowing a histomorphology based immunophenotypic approach. Acknowledgments The authors acknowledge Dr. Paul White and Dr. Neville Calleja for their statistical assistance. Ms. Sharon Falzon for her assistance and advice. The management of the Pathology department and all the staff at the Haematology and Histopathology departments within Mater Dei Hospital, Malta for their support. References 1. Kaleem Z. Flow cytometric analysis of lymphomas: current status and usefulness. Archives in Pathology Laboratory Medicine 2006; 130: 1850-1858. 2. Wood B.L., Arroz M., Barnett D., DiGiuseppe J., Greig B., Kussick S.J., Oldaker T., Shenkin M., Stone E., Wallace P. 2006 Bethesda International Consensus Recommendations on the Immunophenotypic Analysis of Hematolymphoid Neoplasia by Flow Cytometry: Optimal Reagents and Reporting for the Flow Cytometric Diagnosis of Hematopoietic Neoplasia. Cytometry Part B (Clinical Cytometry) 2007; 72B:S14–S22. 3. Braylan R.C., Orfao A., Borowitz M.J., Davis B.H. Optimal number of reagents required to evaluate hematolymphoid neoplasias: results of an international consensus meeting. Cytometry (Communications in Clinical Cytometry) 2001; 46: 23-27. 4. Stetler-Stevenson M.A., Ahmad E., Barnett D., Braylan R., DiGiuseppe J.A., Marti G., Menozzi D., Oldaker T.A., Orfao A., Rabellino E., Stone E.C., Walker C. Clinical Flow Cytometric Analysis of Neoplastic Hematolymphoid Cells; Approved Guideline – Second Edition. Clinical and Laboratory Standards Institute, 2007 Document H43-A2. 5. Nguyen D., Diamond L.W. & Braylan R.C. Flow cytometry in Hematopathology. USA: Humana Press; 2003. 6. Carulli G., Cannizzo E., Zucca A., Budaa G., Orciuolo E., Marini A., Petrini M., CD45 expression in low-grade B-cell non-Hodgkin’s lymphomas. Leukemia Research 2008; 32: 263–267. 7. Deneys V., Thiry V., Hougardy N., Mazzon A.M., Leveugle P., De Bruyere M. Impact of cryopreservation on B cell chronic lymphocytic leukaemia phenotype. Journal of Immunological Methods 1999; 228: 13–21. 8. D’Arena G., Musto P., Cascavilla N., Dell’Olio M., Di Renzo N., Carotenuto M. Quantitative Flow Cytometry for the Differential Diagnosis of Leukemic B-Cell Chronic Lymphoproliferative Disorders. American Journal of Hematology 2000; 64: 275–281. 9. Sanchez M.L., Almeida J., Vidriales B., Lopez-Berges M.C., Garcia-Marcos M.A., Moro M.J., Corrales A., Calmuntia M.J., San Miguel J.F., Orfao A. Incidence of phenotypic aberrations in a series of 467 patients with B chronic lymphoproliferative disorders: basis for the design of specific four-color stainings to be used for minimal residual disease investigation. Leukemia 2002; 16: 1460–1469. 10. Ray S., Craig F.E., Swerdlow S.H. Abnormal patterns of antigenic expression in follicular lymphoma: A flow cytometric study. American Journal of Clinical Pathology 2005; 124: 576-583 Table 1: Table summarises the different monoclonal antibody combinations, together with their respective fluorochromes and gating markers. FITC PE PerCP (Gating marker) Tube 1 CD4 CD8 CD45 Tube 2 CD5 CD3 CD45 Tube 3 CD19 CD10 CD45 Tube 4 CD20 CD23 CD45 Tube 5 Kappa Lambda CD19 FITC; fluorescein isothiocyanate, PE; phycoerythrin and PerCP; peridinin chlorophyll protein. Table 2: Summary of correlation, statistical differences and measurement of agreement obtained for percentage positivities on the different antigens tested. Antigen Pearson’s Correlation Coefficient r-value Paired t-test p-value Significance 2-tailed (p-value) Mean Difference Intraclass Correlation Coefficient 95% CI Lower Upper 95% Confidence Interval Lower Upper CD4 0.966 <0.001 0.945 0.07 -2.03 2.17 0.9661 0.9280 0.9842 CD8 0.883 <0.001 1.000 0.00 -0.94 0.94 0.8854 0.7672 0.9453 CD5 0.890 <0.001 0.894 0.25 -3.55 4.05 0.8926 0.7812 0.9489 CD3 0.958 <0.001 0.761 0.39 -2.23 3.01 0.9587 0.9128 0.9806 CD20 0.932 <0.001 0.874 0.25 -2.96 3.46 0.9344 0.8633 0.9691 CD23 1.000 <0.001 0.118 1.50 -0.40 3.40 0.9653 0.9259 0.9839 CD10 0.986 <0.001 0.007 1.15 0.34 1.95 0.9696 0.9126 0.9876 CD19 1.000 <0.001 0.629 -0.61 -3.15 1.94 0.9519 0.8992 0.9774 Kappa 0.936 <0.001 1.000 0.00 -2.42 2.42 0.9366 0.8677 0.9702 Lambda 0.972 <0.001 0.193 -1.18 -2.99 0.63 0.9673 0.9310 0.9847 CD45 0.849 <0.001 0.003 -7.03 0.7543 Table 3: Summary of correlation, statistical differences and measurement of agreement obtained for MFI on the different antigens tested. Antigen Pearson’s Correlation Coefficient r-value p-value Paired t-test Significance 2-tailed (p-value) Mean Difference Intraclass Correlation Coefficient 95% Confidence Interval 95% CI Lower Upper Lower Upper CD4 0.932 <0.001 0.016 22.04 4.51 39.56 0.9181 0.8048 0.9638 CD8 0.959 <0.001 <0.001 481.14 283.53 678.75 0.9252 0.5832 0.9759 CD5 0.939 <0.001 0.172 26.39 -12.17 64.95 0.9367 0.8686 0.9702 CD3 0.901 <0.001 0.418 65.46 -97.76 228.68 0.8988 0.7950 0.9517 CD20 0.727 <0.001 0.369 116.82 -145.43 379.08 0.7230 0.4874 0.8611 CD23 0.898 <0.001 0.041 136.54 5.77 267.30 0.8309 0.6534 0.9198 CD10 0.962 <0.001 0.332 11.32 -12.19 34.83 0.9532 0.9024 0.9779 CD19 0.582 0.002 0.121 -105.54 -240.95 29.88 0.5576 0.2493 0.7656 Kappa 0.713 <0.001 0.493 -50.96 -201.58 99.65 0.5759 0.2646 0.7785 Lambda 0.753 <0.001 0.816 43.25 -334.49 420.99 0.7390 0.5083 0.8704 CD45 0.766 <0.001 0.621 0.7653 Table 4: Table representing immunophenotype of the LN specimens analysed. Haematolymphoid Neoplasia CLL DLBCL FL MCL T-NHL Hodgkin’s Lymphoma Reactive Hyperplasia Immunophenotype No. of Cases Pos: CD5, CD20, CD19, CD23, Kappa Neg: CD10, Lambda, CD3, CD4, CD8 Pos: CD20, CD19, Lambda Neg: CD10, CD23, Kappa, CD5, CD3, CD4, CD8 Pos: CD20, CD19, CD10, Kappa Neg: CD23, Lambda, CD5, CD3, CD4, CD8 Pos: CD5, CD20, CD10, Lambda Neg: CD23, Kappa, CD3, CD4, CD8 Pos: CD4, CD5, CD3 Neg: CD8, CD19, CD10, CD20, CD23, Kappa, Lambda T-cell predominance with some B-cell markers present and no light chain restriction Variable expression of all T-cell and B-cell markers with no light chain restriction 1 1 1 1 1 2 21 Figure 1: Bar chart representing a comparison between fresh and cryopreserved mean percentage Haematolymphoid Neoplasia Immunophenotype No. of Cases positivities, for all the tested markers. 120.0 Percent Positivity 100.0 80.0 60.0 Fres h Lymph Nodes Cryopres erved Lymph Nodes 40.0 20.0 45 AA D CD a La m bd a 19 Ka pp 10 CD 23 CD CD 3 20 CD 5 CD 8 CD CD CD 4 0.0 Axis Title Figure 2: Bar chart representing a comparison between fresh and cryopreserved mean fluorescent intensities, for all tested antigens. 7000 Mean Fluorescent Intensity 6000 5000 4000 Fresh Lymph Nodes 3000 Cryopreserved Lymph Nodes 2000 1000 0 CD4 CD8 CD5 CD3 CD20 CD23 CD10 CD19 Kappa Lambda CLL Pos: CD5, CD20, CD19, CD23, Kappa Neg: CD10, Lambda, CD3, CD4, CD8 1 DLBCL Pos: CD20, CD19, Lambda Neg: CD10, CD23, Kappa, CD5, CD3, CD4, CD8 1 FL Pos: CD20, CD19, CD10, Kappa Neg: CD23, Lambda, CD5, CD3, CD4, CD8 1 MCL Pos: CD5, CD20, CD10, Lambda Neg: CD23, Kappa, CD3, CD4, CD8 1 T-NHL Pos: CD4, CD5, CD3 Neg: CD8, CD19, CD10, CD20, CD23, Kappa, Lambda 1 Hodgkin’s Lymphoma T-cell predominance with some B-cell markers present and no light chain restriction 2 Reactive Hyperplasia Variable expression of all T-cell and B-cell markers with no light chain restriction 21 Table 4: Table representing immunophenotype of the LN specimens analysed. A B Figure 3: A case of MCL analysed on fresh (A) and cryopreserved cells (B), with minimal variation in phenotypic pattern between the two. Such concordance is also seen for the other LN analysed. FCI gave a phenotype suggestive of MCL involvement within the LN, with the typical antigenic expression pattern of CD5+/CD20+/CD23-/CD10- and light chain restriction.