significant genera
advertisement

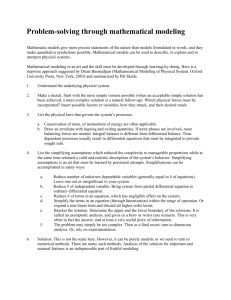
UNM-SOM Clinical Note Global Grading Template History General 1 PE 4 5 6 7 8 9 10 Adequate documentation of symptoms & findings Similar data grouped together Adequate congruence between symptoms, findings and assessment and plan Clear portrayal of symptoms & findings Recorded in logical sequence Similar data grouped and labeled Clear, explicit and correct congruence between symptoms, findings and assessment and plan Significant/critical symptom information omitted One or more essential positive and negative elements of the history omitted Significant erroneous information included. Symptom information is presented with necessary detail Most of the pertinent positive and negative elements of the history included. Complete symptom information presented with advanced level of detail (i.e. risk factor assessment, well-characterized pain assessment) All pertinent positive and negative elements of the history included Vital signs and/or general description of patient omitted Physical examination information is presented in inadequate detail Body systems noted that do not derive from patient history Essential body system(s) omitted Significant positive & negative findings omitted Assessment 3 Vague or confusing wording/documentation Information poorly organized Significant incongruence between symptoms, findings and assessment and plan Plan 2 Vital signs and general description of patient included o (If omitted, there are no important omissions in other areas of the note) Documents physical examination findings of appropriate body systems Includes documentation of most of the significant positive and negative findings Vital signs and general description of patient included Documents physical examination findings from pertinent body systems, coherent with history, in appropriate detail Includes all significant positive and negative findings Assessment Synthesis: Absent or mere reiteration of history & findings Interpretation of Data: Differential diagnosis omitted (0 or only 1 diagnosis) Differential contains highly unlikely diagnoses Diagnoses inconsistent with Hx and PE findings Assessment Synthesis: Accurately reflects clinical situation but few appropriate semantic qualifiers o (If omitted, there are no important omissions in other areas of the note) Interpretation of Data: Differential diagnoses reasonable but may be inappropriately rank ordered, too narrow or excessively broad in scope Assessment Synthesis: Succinct summary accurately and comprehensively reflects clinical situation using appropriate semantic qualifiers Interpretation of Data: Differential diagnoses in correct rank order DDx comprehensive but appropriately targeted DDx includes any serious illness with effective intervention, albeit less common Plan omitted Plan inconsistent with history, physical findings, or differential Plan could result in patient harm Ambiguous or nonspecific plan items Extraneous or unnecessarily expensive recommendations included. Plan generally consistent with the history, physical findings and differential Evaluation plan insufficiently detailed before moving to therapy items Recommended interventions will not result in unnecessary harm Avoids most non-indicated diagnostic tests Suggests indicated diagnostic tests which demonstrate consideration of cost containment Well organized plan, clearly congruent with patient history, physical findings and differential Maximal use of well chosen, precisely targeted, cost effective evaluations and interventions Minimally invasive but optimally informative evaluations ©2005 University of New Mexico School of Medicine, Assessment & Learning Programs, Revised 06/05/2007