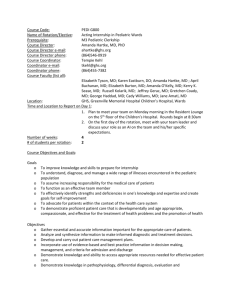
PICU Montef - St. Barnabas Hospital
advertisement

St. Barnabas Hospital Department of Pediatrics Required PL-2 Pediatric Intensive Care Rotation At Montefiore Medical Center Goals and Objectives Revised June 2009 The following will describe the educational goals and objectives of the Pediatric Intensive Care Unit rotation for St. Barnabas PL-2 residents. Patient Care 1. Obtain and interpret information relevant to the critically ill pediatric patient. 2. Evaluate and manage, under supervision of an intensivist, patients with signs and symptoms that present commonly to the intensive care unit. 3. Use a logical and effective approach to the assessment and daily management of critically ill children and their families, under the guidance of an intensivist, using evidence-based decision making and problem solving skills. 4. Perform a physical examination of the critically ill child and identify normal and abnormal findings. 5. Use and interpret clinical tests commonly used in the pediatric intensive care unit: a. CBC with differential, platelet count, RBC indices b. Blood chemistries: electrolytes, glucose, calcium, magnesium, phosphate c. Renal function tests d. Tests of hepatic function (PT, albumin) and damage (ammonia, bilirubin, liver enzymes) e. Serologic tests for infection (e.g., hepatitis, HIV) f. C-reactive protein, erythrocyte sedimentation rate. g. Therapeutic drug concentrations h. Coagulation studies: platelets, PT/PTT, fibrinogen, FSP, D-dimers i. Arterial, capillary, and venous blood gases j. Detection of bacterial, viral, and fungal pathogens k. Urinalysis l. CSF analysis m. Gram stain n. Stool studies o. Toxicologic screens/drug levels p. Other fluid studies (e.g. pleural fluid, joint fluid) q. Chest x-ray, Abdominal series, Skeletal survey, Cervical spine films r. CT scans of abdomen, chest and head s. MRI scans t. Basic concepts of cerebral blood flow studies 6. Use and interpret physiologic monitoring and special technology that are commonly used in the pediatric intensive care unit under the supervision of an intensivist: a. Central venous pressure monitoring b. Invasive arterial blood pressure monitoring c. Intracranial pressure monitoring d. Pulse oximetry e. End-tidal carbon dioxide monitoring 7. Utilize appropriately or be familiar with the following treatment and techniques in the intensive care unit, including monitoring effects and anticipating potential complications specific to each therapy: a. Oxygen administration by cannula, masks, hood b. Positive pressure ventilation including non-invasive modalities such as nasal/mask BiPAP/CPAP, bag and mask ventilation c. Principles of ventilator management, intubation and extubation procedures and criteria d. Analgesics, sedatives, and paralytics e. Enteral and parenteral nutrition f. Blood and blood product transfusions g. Vasoactive drugs (pressors and inotropes) Medical Knowledge 1. Know and/or access medical information efficiently, evaluate it critically, and apply it appropriately to the care of patients in the pediatric intensive care unit. 2. Demonstrate knowledge of the etiology and management of common conditions in the critically ill child. a. Cardiovascular: Acute life-threatening event, bradycardia, cardiopulmonary arrest, congestive heart failure, cyanosis, hypertension, hypotension, poor capillary perfusion, rhythm disturbances, tachycardia b. Endocrine: Signs and symptoms suggestive of hypo- and hyperglycemia and adrenal insufficiency/crisis c. GI: Abdominal distension, hematemesis and melena, icterus, peritoneal signs, vomiting d. Hematologic:, Pallor, petechiae, purpura, uncontrolled bleeding e. Infectious Diseases: Endotoxic shock, fever f. Neurologic: Acute weakness, altered mental status, coma, delirium, encephalopathy, seizures, tetany, thermoregulatory abnormalities g. Renal: Anuria, hematuria, oliguria, polyuria, severe electrolyte disturbance h. Respiratory: Apnea, cyanosis, dyspnea, hemoptysis, hypercarbia, hyperpnea, hypoxemia, increased or decreased respiratory effort, poor air movement, pulmonary edema, respiratory failure, stridor, tachypnea, wheezing Practice-Based Learning and Improvement 1. Use scientific methods and evidence to investigate, evaluate, and improve one’s patient care practice in PICU setting. 2. Establish and become actively involved in a feedback process, which includes open discussion with preceptors and other faculty members, ample time to respond to feedback, and opportunity to implement a plan of action with specific goals aimed at overall improvement. 3. Facilitate the learning of students and other health care professionals in the PICU. Interpersonal Skills and Communication 1. Provide sensitive support to patients with serious illness and to their families, and arrange for ongoing support or preventive services if needed. 2. Maintain comprehensive, timely, and organized medical records. 3. Communicate and collaborate effectively as part of a functional team with physicians, other health care professionals, staff, and students. Professionalism 1. Conduct oneself in a respectful and professional manner when interacting with patients and their families with careful awareness and consideration of their culture, age, race, gender, sexual preference, and disabilities. 2. Demonstrate a commitment to acquiring the knowledge base expected of general pediatricians caring for seriously ill children under the guidance of an intensivist. 3. Demonstrate knowledge, skills and attitudes needed for continuous self-assessment. 4. Practice ethically and within medical-legal constraints in the care of critically ill children. 5. Collaborate respectfully with staff and health care professionals. 6. Recognize the limits of one’s knowledge and expertise and take steps to avoid medical errors. Systems-Based Practice 1. Understand key aspects of health care systems, cost control, and mechanisms for payment as they relate to the intensive care setting 2. Advocate on behalf of patients experiencing challenges with health care system complexities 3. Implement appropriate discharge plans, including involvement of social work services and/or visiting nurse services if necessary 4. Participate in the detection and critical evaluation of medical errors in order to make corrections in practice strategies and thereby prevent future occurrences. Evaluation Any problems or concerns regarding the resident’s performance in the Pediatric Intensive Care Unit will be immediately be brought to the attention of the St. Barnabas Hospital Pediatric Residency Program Director in order to affect corrective measures. At the completion of the rotation Pediatric Critical Care faculty will assess the educational accomplishments of the resident and forward a completed evaluation form to the St. Barnabas Pediatric Residency Program Director. The St. Barnabas PL-2 resident will complete an evaluation of the Pediatric Intensive Care rotation regarding clinical experience, faculty supervision and didactic program. While on the Pediatric Intensive Care Unit rotation, the St. Barnabas PL-2 resident will assume duties and responsibilities equivalent to those of other residents rotating at the Pediatric Intensive Care Unit in the same year of training. The St. Barnabas resident will be fully integrated into daily activities of the Pediatric Intensive Care Unit. The St. Barnabas PL-2 resident on the Pediatric Intensive Care Unit rotation will have the same access to resources and facilities, including but not limited to library and medical records as other residents rotating in the Pediatric Intensive Care Unit. The resident hours will be consistent with the requirements and limitations of the ACGME Duty Hours and New York State 405 regulations.