chapter outline
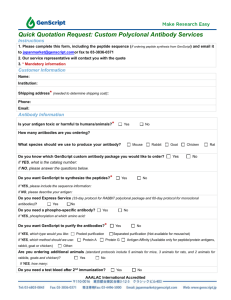
advertisement

35 Clinical Microbiology and Immunology CHAPTER OVERVIEW This chapter describes the field of clinical microbiology, which is concerned with the detection and identification of pathogens that are the etiological agents of infectious disease. Identification may be based on the results of some combination of morphological, physiological, biochemical, and immunological procedures. Time may be critical in life-threatening situations. Therefore, rapid identification systems and computers can be used to greatly speed up the process. The chapter closes with a discussion of in vitro antigen-antibody interactions. These are particularly useful in diagnostic procedures. CHAPTER OBJECTIVES After reading this chapter you should be able to: describe the functions and/or services performed by clinical microbiology laboratories discuss the types of procedures used to identify microorganisms in specimens describe molecular genetic techniques useful for identifying microorganisms in a clinical setting describe the various in vitro antigen-antibody interactions, and give examples of diagnostic tests based on them CHAPTER OUTLINE I. II. Overview of the Clinical Microbiology Laboratory A. Clinical microbiologists isolate and identify pathogens from clinical specimens to provide information to physicians B. Universal precautions for handling specimens have been established by the Centers of Disease Control and Prevention (CDC) 1. Specimen—human material that is tested, examined, or studied to determine the presence or absence of specific microorganisms a. Because of safety concerns, specimens must be handled carefully; universal safety precautions have been recommended by the CDC to address safety issues in specimen handling b. Specimens should be: 1) Representative of the diseased area 2) Adequate in quantity for a variety of diagnostic tests 3) Devoid of contamination, particularly by microorganisms indigenous to the skin and mucous membranes 4) Forwarded promptly to the clinical laboratory 5) Obtained prior to the administration of any antimicrobials Identification of Microorganisms from Specimens A. Microscopy 1. Direct examination of specimen, or examination of specimen after various staining procedures that are specific for types of bacteria, fungi, viruses, or protists 2. Bacteria a. Wet mounts for bright-field, phase-contrast, or dark-field microscopy; fluorescent microscopy with nucleic acid stains or labeled antibodies 315 b. B. C. D. E. Hybridomas produce monoclonal antibodies specific for a single epitope; these can be fluorescently labeled and used for rapid, accurate culture confirmation c. Immunofluorescence stains specimens with fluorescent dyes that emit visible colored light when excited 1) Direct immunofluorescence—after fixation to a slide, the specimen is stained with a fluorescently labeled antibody directed at cell surface antigens 2) Indirect immunofluorescence—after a known antigen is attached to a slide, a patient's serum (antiserum) is applied; if antibodies specific for the antigen are present, these can be detected with a fluorescently labeled secondary antibody 3. Fungi—light microscopy to observe hyphae and spores are diagnostic for fungi; lactophenol aniline blue stain often used 4. Parasites—direct microscopy to observe ova, trophozoites, and cysts; D'Antonio's iodine and Giemsa stain often used 5. Viruses—can be observed with electron microscopy Growth and biochemical characteristics 1. Bacteria a. Isolation and growth of bacteria are required before many diagnostic tests can be used b. Initial identity may be suggested by source of specimen; microscopic appearance and Gram reaction; pattern of growth on selective, differential, and other media; and by hemolytic, metabolic, and fermentative properties c. After pure cultures are obtained, specific biochemical tests can be done and a dichotomous key used for identification d. Rickettsias—identified by immunoassays or by isolation in specialized laboratories 2. Fungi—examination of cultures on selective media, often supplemented with antibacterial drugs 3. Parasites—generally not cultured 4. Viruses—identified by isolation in cell (tissue) culture, by immunodiagnosis, and by molecular detection a. Viral cultivation 1) Cell cultures—viruses are detected by cytopathic effects (observable morphological changes in host cells) or by hemadsorption (binding of red blood cells to infected cells) 2) Embryonated eggs—virus can be inoculated into allantoic cavity, amniotic cavity, or the chorioallantoic cavity; virus is detected by development of pocks on the chorioallantoic membrane, by development of hemagglutinins in the allantoic and amniotic fluid, and by death of the embryo 3) Laboratory animals (e.g., suckling mice)—observed for signs of disease or death Rapid methods of identification 1. Manual biochemical systems such as the API 20E system for enterobacteria a. Consists of 20 microtube inoculation tests b. Results are converted to a seven- or nine-digit profile number c. The number is compared to the API Profile Index to determine the name of the bacterium 2. Automated systems (Phoenix™, VersaTREK®, MicroScan® WalkAway) test pure cultures in miniaturized chambers for specific capabilities and antibiotic sensitivity 3. Monoclonal antibodies are available for the detection of many microorganisms; the antibodies can be specific to the species or strain level 4. Biosensors can be based on microfluidic antigen sensors, rapid PCR, sensitive spectroscopy systems, and liquid crystal amplification of immune complexes Bacteriophage typing—based on the fact that host range specificities of bacteriophages are dependent upon surface receptors on the bacteria Molecular genetic methods 1. Group of accurate measures including protein comparisons, enzyme characterizations, nucleic acid-base composition, nucleic acid hybridization, and nucleic acid sequencing 2. Nucleic acid-based diagnostic methods 316 a. DNA molecules that have been cloned from organism or prepared by PCR technology can be used in hybridization procedures b. Real-time PCR can monitor amplification of specific microbial genes; rRNA genes can be sequenced to identify bacterial strains (ribotyping) c. Genomic fingerprinting examines patterns produced from PCR amplification of repetitive sequences; plasmid fingerprinting—separation and detection of the number, molecular weight, and restriction patterns of different plasmids, that are often consistently present in a strain of bacteria III. Clinical Immunology A. Detection of antigens and antibodies may be valuable diagnostically; interpretation of immunologic test results can be difficult B. Serotyping—antigen-antibody specificity is used to differentiate among various strains (serovars) of an organism found in serum samples C. Agglutination—visible clumps or aggregates of cells or of coated latex microspheres; if red blood cells are agglutinated, the reaction is called hemagglutination 1. Widal Test—direct agglutination test for diagnosing typhoid fever 2. Latex agglutination tests are used in pregnancy tests and to diagnose mycotic, helminthic, and bacterial infections 3. Mycoplasmas are typically identified by hemagglutinin reactions, PCR, and antigen-antibody reactions 4. Viral hemagglutination inhibition tests are used to diagnose influenza and other viral infections 5. Agglutination tests can be used to measure antibody titer (the reciprocal of the greatest dilution showing agglutination reaction) D. Complement fixation—used to detect the presence of serum antibodies to a pathogen; currently used to diagnose certain viral, fungal, rickettsial, chlamydial, and protozoan diseases E. Enzyme-linked immunosorbent assay (ELISA)—involves linking enzymes to an antibody 1. Indirect immunosorbent assay—detects serum antibody a. Well of a microtiter plate is coated with antigen specific to the antibody of interest b. Test serum is added; if antibodies are present, they will bind antigen and will be retained after washing c. An antibody against the test immunoglobulin is added; the second antibody is conjugated to an enzyme and will only be retained in the well after washing if the test antibody is present in the well d. Substrate of the enzyme is added; reaction only occurs if conjugated antibody (and therefore test antibody) are present in the well; the colored product of the reaction can be detected spectrophotometrically 2. Double antibody sandwich assay—detects antigens in a sample a. Wells of a microtiter plate are coated with antibody specific to the antigen of interest b. Test sample is placed in well; if it contains the antigen of interest, the antigen will be retained in the well after washing c. Second antibody is added; it is conjugated to an enzyme and is specific to the antigen; the second antibody will be retained in the well after washing if the antigen was retained in the previous step d. Substrate of enzyme is added; reaction only occurs if conjugated enzyme (and therefore antigen) is present in the well; produces a colored product that can be detected F. Immunoblotting (Western Blot)—proteins are separated by electrophoresis, blotted into nitrocellulose sheets, then treated with solution containing enzyme-tagged antibodies G. Immunoprecipitation—soluble antigens form insoluble immune complexes that can be detected H. Immunodiffusion—involves the precipitation of immune complexes in an agar gel 1. Single radial immunodiffusion (RID) assay is quantitative 2. Double diffusion assay (Öuchterlony technique)—lines of precipitation form where antibodies and antigens have diffused and met; determines whether antigens share identical determinants I. Immunoelectrophoresis—antigens are first separated by electrophoresis according to charge, and are then visualized by the precipitation reaction; greater resolution than diffusion assay 317 J. K. Flow cytometry 1. Detects single or multiple microorganisms on the basis of a cytometric parameter or by means of fluorochromes 2. Flow cytometer forces cells through a laser beam and measures light scatter or fluorescence as the cells pass through the beam; cells can be tagged with fluorescent antibody directed against specific surface antigen Radioimmunoassay (RIA)—purified antigen labeled with a radioisotope competes with unlabeled antigen sample for antibody binding TERMS AND DEFINITIONS Place the letter of each term in the space next to the definition or description that best matches it. ____ ____ ____ ____ 1. 2. 3. 4. ____ 5. ____ 6. ____ 7. ____ 8. ____ 9. ____ 10. ____ 11. ____ 12. ____ 13. The insertion of a tube into a body canal or hollow organ A tubular instrument used for withdrawing or introducing fluids from or into a body cavity An observable change that occurs in cells as a result of viral infection Phenomenon that occurs because of an alteration of the membrane of a virus-infected cell so that red blood cells will adhere to it A method of identifying bacteria based on the bacteriophage that infect them A method of strain typing that involves preparing a Southern Blot of chromosomal DNA cleaved with restriction endonucleases, and then probing the blot with specific rRNA probes Visible aggregates or clumps formed by agglutination reactions An agglutination reaction-based test that is used to diagnose typhoid fever The agglutination of red blood cells by viruses A colorless substrate that is acted on by an enzyme to produce a colored end product A process in which a suspension of cells is forced through a laser beam; it can be used to detect, count, separate, and characterize cells in the suspension A process wherein a fluorescent dye is attached to an antibody and used to detect the antigen specific for that antibody The use of in vitro antibody-antigen reactions to differentiate strains of microorganisms a. b. c. d. e. f. g. h. i. j. k. l. m. agglutinates bacteriophage typing catheter chromogen cytopathic effect flow cytometry hemadsorption immunofluorescence intubation ribotyping serotyping viral hemagglutination Widal test FILL IN THE BLANK 1. 2. The major concern of the __________ __________ is to rapidly isolate and identify microorganisms from clinical specimens. Viral replication in cell cultures is detected in two ways: by the observation of __________ __________ (observable changes in cell morphology) and by ____________ (alterations in the plasma membrane that enable red blood cells to adhere firmly to virus-infected cells). 318 3. 4. 5. 6. One of the most widely used serological tests is the ____________. It involves the linkage of an antibody molecule to an enzyme whose activity can be detected by the formation of a colored product. When a precipitation reaction occurs in an agar gel, it is called . One assay based on this phenomenon is the assay. This assay is based on the diffusion of antigen out of a well into agar containing an antibody. In another assay, the __________ __________ assay, also known as the , antigens are placed in a set of wells in agar and antibodies are placed in another well. Both antibodies and antigens diffuse into the agar. Serological procedures used to differentiate different strains of microorganisms are called . An important example of this is the __________ __________, which is used to classify streptococci based on the antigenic nature their cell walls. One way of detecting these differences is the __________ __________, in which mixing antiserum with a solution of streptococci causes capsular swelling if the antiserum is specific for that particular serovar. Some mixtures of antigens are very complex, making it difficult to detect a particular antigen. In such cases, __________ is useful. In this process, antigens are first separated based on their electrical charge and then are visualized by precipitation reaction. MULTIPLE CHOICE For each of the questions below select the one best answer. 1. 2. 3. 4. 5. Which of the following is NOT normally used in the identification of microorganisms? a. microscopic examination b. growth or biochemical characteristics c. immunological techniques that detect antibodies or microbial antigens d. All of the above are used in the identification of microorganisms. Which of the following is NOT normally used to culture viruses? a. growth on artificial media b. growth in cell cultures c. growth in embryonated hen’s eggs d. growth in whole animals Which of the following is normally used to detect spirochetes in skin lesions in early syphilis? a. bright-field microscopy b. phase-contrast microscopy c. dark-field microscopy d. immunofluorescence microscopy Which of the following is NOT likely to be useful in the identification of bacteria? a. source of the culture specimen b. growth patterns on selective and differential media c. hemolytic, metabolic, and fermentative properties d. All of the above are useful in the identification of bacteria. What is the basic principle underlying plasmid fingerprinting? a. 6. 7. 319 Microbial isolates of the same strain contain the same number of plasmids with the same molecular weights. b. Microbial isolates of different strains have different plasmids (either in number, molecular weight, or both). c. Both (a) and (b) are correct. d. Neither (a) nor (b) is correct. Which of the following is NOT a reason that immunological tests for antibodies against a particular infectious organism might yield negative results? a. The person might not be infected with the particular organism. b. The organism might be poorly immunogenic and may not stimulate sufficient antibody production to be detectable. c. There might not have been sufficient time since the onset of infection for an antibody response to develop. d. All of the above might yield negative results. Which of the following is NOT true about the use of DNA:rRNA hybrids for identification as compared to the use of DNA:DNA hybrids? a. DNA:rRNA hybrids are more sensitive, and therefore, fewer microorganisms are required. b. DNA:rRNA hybrids are more specific, and they show less cross-hybridization to other species. c. 8. 9. DNA:rRNA hybrids are formed more rapidly; test requires two hours or less for results. d. All of the above are true about the use of DNA:rRNA hybrids as compared to the use of DNA:DNA hybrids. Which type of cell culture for cultivating viruses makes use of transformed cells, generally epithelial in origin? a. primary cultures b. secondary cultures c. semicontinuous cell cultures d. continuous cell cultures When complement binds to an antibodyantigen complex, it becomes used up and is no longer available to lyse sensitized red blood cells. This can be used diagnostically in an assay. What is this assay called? a. complement utilization assay b. complement titration assay c. complement fixation assay d. complement complexation assay 10. In one immunological assay, antigens are separated by electrophoresis through a polyacrylamide gel and then are transferred to a sheet of nitrocellulose. This is then probed with enzyme-tagged antibodies. What is this called? a. immunoprecipitation b. immunodiffusion c. ELISA d. immunoblotting 11. Immunological assays can be used to differentiate strains of microorganisms. What are these assays called? a. serotyping b. immunotyping c. isotyping d. antigen typing TRUE/FALSE ____ 1. The Gram stain is used for bacteria that have cell walls, while the acid-fast stain is used primarily for wall-less bacteria. ____ 2. Rickettsias are routinely isolated and identified by culture methods because these are relatively inexpensive and safe to use. ____ 3. Bacteria can usually be identified by morphological examination, and biochemical tests are only needed for confirmation of identification. ____ 4. Detection of an elevated antibody titer is used to indicate an active, ongoing infection. ____ 5. Strains of bacteria that are infected by different phage isolates are referred to as phagovars. ____ 6. Rapid ID systems such as the API 20E system identify bacteria based on substrate utilization characteristics. ____ 7. Ribotyping involves probing Southern Blots of endonuclease digested chromosomal DNA with rRNA genes probes. ____ 8. Immunoprecipitation reactions will occur as long as the antibody and antigen are present in nearly equal amounts. ____ 9. Radioimmunoassays do not need specific antibodies. ____ 10. Flow cytometry can use lasers to detect specific cells in a stream of suspended cells. CRITICAL THINKING 1. Nucleic acid-based detection methods have a great deal of power; however, microscopy and biochemical tests are still widely used. Why? Contrast these two approaches and compare them to current immunoassays for detection of pathogens. 320 2. There are a variety of rapid methods for microbial identification. Discuss several of these methods and how they might be applied. In recent years, the need for rapid tests has increased. Why? What kind of new technologies are being developed? ANSWER KEY Terms and Definitions 1. i, 2. c, 3. e, 4. g, 5. b, 6. j, 7. a, 8. m, 9. l, 10. d, 11. f, 12. h, 13. k Fill in the Blank 1. clinical microbiologist 2. cytopathic effect; hemadsorption 3. ELISA 4. immunodiffusion; single radial immunodiffusion (RID); double diffusion agar; Ouchterlony technique; 5. serotyping; Lancefield system; Quellung reaction 6. immunoelectrophoresis Multiple Choice 1. d, 2. a, 3. c, 4. d, 5. c, 6. d, 7. b, 8. d, 9. c, 10. d, 11. a True/False 1. F, 2. F, 3. F, 4. F, 5. T, 6. T, 7. T, 8. T, 9. F, 10. T 321