Peroxidation of intraveneous lipid emulsions
advertisement

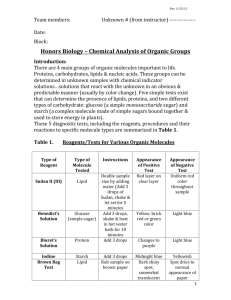
Peroxidation of Intravenous Lipid Emulsions Stefan Mühlebach, Ph.D. Chefapotheker, Apotheke Kantonsspital, CH 5001 Aarau (Switzerland) phone +41-62-838-53 50, fax +41-62-838-42 48, e-mail: stefan.muehlebach@ksa.ch Objectives To list the characteristics of lipid peroxidation (LPO) To identify the potential toxic risk of radical-mediated chemical reactions in vivo To enumerate factors influencing LPO in parenteral nutrition (PN) admixtures To report on the rationale of measures to reduce LPO in all-in-one admixtures in vitro related to PN compounding, storage, and final administration to the patient To identify different methods to measure LPO and its breakdown products To characterise the iodometric test method as a cost-effective candidate for compounding centres to document LPO in ready to use all-in-one bags Parenteral Nutrition and Lipid Peroxidation Parenteral nutrition (PN) contains all the nutrients necessary to meet the patient’s needs. Most patients on PN show severely disturbed organ functions or/and specific changes of metabolism (e.g. organ failure, post-aggression stress) requiring an adaptation of the nutrition regimen. The i.v. administration allows nutrients to be administered only in digested form and readily available for the basal energy and nitrogen metabolism. To minimise complications, improve tolerance and convenience, and allow home treatment all-in-one (AIO) admixtures have improved parenteral nutrition considerably. In total parenteral nutrition these complex AIO admixtures contain more than 50 different components and show only limited stability. In terms of effectiveness and safety that stability issue is of special clinical and pharmaceutical interest [1,2]. Triglycerides as main PN lipid source have only reduced water solubility. For their i.v. administration and for a good biological tolerance they have to be emulsified like chylomicrons using natural phospholipids. The oil particles of the resulting oil in water emulsion have to be distributed homogeneously. The typical mean fat droplet diameter is 0.2 –0.4 m. The negatively charged droplets are prone to undergo physical destabilisation leading eventually to irreversibly deteriorated emulsion systems with potentially fatal risks for the patient (embolism). Intravenous long chain triglycerides (LCT) contain high concentrations of essential polyunsaturated -3 and -6 fatty acids (PUFA) [e.g. soy bean oil: linoleic (-6 C18-2) and linolenic (-3 C18-3) acid; fish oil: EPA (-3 C20-5) and DHA (-3 C22-6)]. In presence of oxygen these PUFA show chemical instability forming reactive lipid peroxides (LPO) and radicals (Figure 1). In the presence of ambient air LPO is initiated by reactive singlet oxygen in vitro. After cleaving hydrogen from fatty acids a hydroxyl radical results. Radicals have a reactive unpaired electron favouring coupling with neighbouring chemicals and initiating chain reactions. The hydroxyl radical interacts with conjugated double bonds of a PUFA representing chemically vulnerable sites. The resulting PUFA radical is the initial event of an autocatalytic chain reaction producing lipid peroxide radicals and lipid hydroperoxides both potentially harmful chemicals. LPO is enhanced by increased temperature, exposure to light, or catalytic concentrations of micronutrients. The latter may also inhibit oxidation as radical scavengers (Figure 2). The resulting lipid hydroperoxides are still unstable intermediates fragmenting into products like aldehydes which may polymerise or represent toxic compounds (e.g. hydroxynoneal or malondialdehyde). LPO as a chemical degradation process is known since a long time ago for vegetable oils as rancidity. Only in the 1950s LPO was addressed in biology and medicine. Lipid Peroxides and Free Radicals in vivo The balance between formation and inactivation of free radicals in the body is an essential modulator of cell proliferation and apoptosis and eventually health and disease [3-6]. Therefore, radicals have desirable and noxious effects. Hydroxyl radical, the biologically most reactive compound, directly attacks lipid-containing membranes, proteins or DNA and produces tissue injury, organ dysfunction, or cancer. Nitric oxide is a stable radical with important signalling functions e.g. in the vascular relaxation of blood vessels (EDRF) and a potent antioxidant quenching agent neutralising lipid peroxide radicals responsible for membrane damage. Interacting with a lipid peroxide radical, NO° has a pro-oxidative function and forms a potent oxidising peroxynitrite. Superoxide O2-°, another physiologic free radical, is involved in inflammation, phagocytosis and cell growth. It may interact similarly with a lipid peroxide radical with NO° forming peroxynitrite (ONOO-) too. To preserve the important signalling effect of NO°, superoxide tissue concentration is kept low by the activity of the selenium-containing superoxide dismutase. Different defense systems exist to reduce an inappropriate oxidative attack or stress in vivo. There is an important distinction to be made between hydrophilic peroxides mainly inactivated by catalase and the more detrimental lipid peroxides. Vitamins like tocopherol (hydrophobic) and vitamin C (hydrophilic) are able to act as radical scavenger. Trace elements like selenium, copper, or iron are present as free metal ions or included in metallo-enzymes forming important bio-catalysts to inactivate or release radicals, e.g. free Fe2+ or Cu1+ ions, superoxide dismutase (zinc-, copper-, manganese-dependent), glutathione peroxidase (selenium), catalase etc. An increased lipid peroxidation may be measured through marker compounds like malondialdehyde (plasma), pentane (expired air) or a decrease of anti-oxidative micronutrients [7]. The anti-oxidative capacity of the body depends on presence of specific micronutrients (nutrition), enzyme maturation (age) but also on the extent of oxidative stress (pathologies). Pre-term infants, severely ill patients, or long-term home PN patients may be at specific risks when exposed to in vitro generated lipid peroxides. Therefore, there is a need to investigate in vitro LPO and the factors affecting its extent. In vitro Assessment of LPO in i.v. Lipids and AIO Admixtures LPO represents a complex cascade of unstable and partly volatile intermediate breakdown products (Figure 1). Hence, analytical assessment is difficult and a variety of analytical methods are used. The specific advantages and limitations of each method have to be evaluated. To document chemical stability of lipid containing PN admixtures cost effective and easy to handle methods are mandatory. Gas or liquid chromatography (GLC or HPLC) are rather expensive methods. They are standard in analytical labs but not routinely available in compounding units and hospital pharmacies. These chromatographic methods allow to determine a changing fatty acid profile or breakdown products as ultimate effect of lipid deterioration. These effects are not early manifestation of LPO [8]. The same holds for thiobarbituric assays or oxygensensitive electrodes, both with poor specificity for LPO. Ferrous oxidation-xylenol orange (FOX) analysis is a peroxide-sensitive spectrophotometric assay. In its original design using hydrophilic solvents the test detects peroxides in the water phase but no lipid peroxides [9]. In addition FOX may interact with vitamins like ascorbic acid or tocopherols present in PN admixtures. In contrast, a iodometric titration of a lipid extract represents a most direct method to determine lipid hydroperoxides. The method is a standard in the analysis of vegetable oils (pharmacopoeia). For parenteral lipids in different pharmacopoeias an upper limit of the peroxidation value [PV = mmol peroxides / L fat emulsion] of 5 mM is given. Starting from the Wheeler method [10] we established a lipid hydroperoxide assessment for i.v. lipid emulsions and AIO admixture [8]. This included a first lipid extraction step by chloroform-methanol 2:1 (Folch extraction). Test samples from 10 g lipid emulsion were incubated for 60 seconds with potassium iodide. The iodine formed was reduced by 0.01 N thiosulfate using an automated voltametric titration system (Dosimat). The reproducibility expressed by the coefficient of variation CV was 3.2% (n=48; PV < 0.1 mM); the test conditions had to be strictly defined; light-protection was necessary. The detection limit for lipid peroxides was 0.02 mM. One single test took about 15 minutes; the cost for chemicals was 2-3 Euros. These characteristics show the appropriateness of the method for a compounding unit. Factors Affecting LPO in vitro Conclusions for AIO Admixture Handling [8,11,12] The PV was dependent on the lipid used (PUFA concentration, content of -tocopherol). Exposure to ambient light is a powerful enhancer of LPO. Starting from the very low PV of a commercial 20% LCT lipid emulsion in glass containers with air displaced by nitrogen this value increased over 1 week by a factor of 40 when the lipid was filled into monolayered, air-permeable EVA bags and exposed to ambient daylight at room temperature. The PV limit given by the pharmacopoeia was reached within a week (Figure 3). The PV increase was accompanied by a pH drop. Light protection is an efficient measure to decrease a PV by a factor of 5-10. Cold storage temperature is an even more efficient LPO stabiliser. Micronutrients can heavily affect LPO. -Tocopherol is a potent antioxidant when present in low and usual concentrations of about 10-20 mg/L in parenteral soy bean lipid emulsions. Increasing the -tocopherol concentration to 160 mg/L showed a pro-oxidative effect. Addition of a daily portion of essential trace elements to an i.v. LCT lipid emulsion or a lipid-containing AIO admixture increased the PV significantly (Figure 3). The effect was more pronounced in pure lipid with a PV increase factor of 5-10 during a two weeks stress test at 40°C in a EVA bag. In conclusion LPO is a complex lipid deterioration reaction occurring in presence of air in vitro. For safety reasons PV in AIO admixtures should be maximally reduced. This will be reached when eliminating the oxygen content in the bag during compounding and storage (overwrapping with an oxygen absorber) storage of the admixture light-protected at 2-8°C trace elements are added to the AIO admixture only immediately before infusion and if compatibility is documented multivitamin addition is not allowed in the presence of trace elements. They may even provoke LPO. There are balanced commercial multivitamin products to be administered in a small volume infusion separately from the PN admixture. References 1. Driscoll DF. Clinical issues regarding the use of total parenteral nutrition admixtures. Ann Pharmacother 1990; 24: 296 2. Barnett MI, Cosslett JR, Duffield JR et al. Parenteral nutrition: pharmaceutical problems of compatibility and stability. Drug Safety 1990; 5(suppl 1): 101 3. Mühlebach S, Steger PJK. Lipid peroxidation of intravenous fat emulsions: a pharmaceutcal issue with clinical impact? Nutrition 1998; 14: 720 4. Guttrigde JMC, Halliwell B. The measurement and mechanism of lipid peroxidation in biological systems. Trends Biol Sci 1990; 15: 129 5. Freeman B A. Oxygen: the air-borne nutrient that both sustains and threatens life. Nutrition 2000; 16:478 6. Weisburger JH. Eat to live, not live to eat. Nutrition 2000; 16: 767 7. Neuzil J, Darlow BA. et al. Oxidation of parenteral lipid emulsion by ambient and phototherapy lights: potential toxicity of routine parenteral feeding. J Pediatr 1995; 123: 785-90 8. Steger PJK, Mühlebach SF. In vitro oxidation of iv lipid emulsions in different all-in-one bags assessed by an iodometric assay and gas-liquid chromatography. Nutrition 1997; 13: 133 9. Silvers K M, Darlow BA, Winterbourn CC. Lipid peroxides and hydrogen peroxide formation in parenteral nutrition solutions containing multivitamins. J Parent Enteral Nutr 2001; 26: 14-17 10. Wheeler DH. Peroxide formation as a measure of autooxidative deterioration. Oil Soap 1932; 9: 82 11. Steger PJK, Mühlebach SF. Lipid peroxidation of iv lipid emulsions in TPN bags: the influence of tocopherols. Nutrition 1998; 14: 179 12. Steger PJK, Mühlebach SF. Lipid peroxidation of iv lipid emulsions and all-in-one admixtures in total parenteral nutrition bags: the influence of trace elements. J Parent Enteral Nutr 2000; 25: 37