PLEURAL EFFUSIONS
advertisement

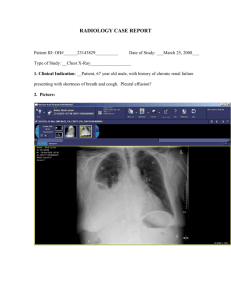
PLEURAL EFFUSIONS Anatomy and Dynamics of pleural Fluid Pleura: A thin membrane consisting of a single layer of mesothelial cells supported by a network of connective and fibroelastic tissue, lymphatics, vessel and investing the lungs and lining the cavities of the hemithoraces.The mesothelial cells are rich in microvilli, and their most important function is to deliver glycoproteins rich in hyaluronic acid with decrease friction between lung and chest wall. Parietal pleura: Receiving its blood supply from the systemic circulation and containing sensory nerve ending. Visceral pleura: Receiving its blood supply from the low pressure pulmonary circulation and containing no sensory nerve fibers. Pleural space: A potential space that is situated between parietal and visceral pleura and normally filled with 5-l0ml of serous fluid. Pleural fluid is formed primarily from the parietal pleura, and part of its turnover depends on the same starling forces that govern vascular and interstitial fluid exchange. The parietal pleura has a hydrostatic pressure similar to that of the systemic circulation (30 cm H2O) whereas that of the visceral pleura depends on the pulmonary circulation (10 cm H2O).0ncotic pleasure is similar in both(25 cm H2O),but the preassure within the pleural cavity is affected by the gravity gradient Thus the pleural space is heterogeneous with a nondependent portion where starling forces favor outpouring of fluid to the cavity and into parenchymal capillaries. The stomas or "lacuna," present over the parietal surface of the low mediastinum, low chest wall, and diaphragm, seem to empty into lymphatics. These subpleural lymphatics represent the major pathway for liquid and solute drainage. Alterations of this formation-resorption mechanism frequently result in the accumulation of pleural fluid. Increases in hydrostatic forces or decreases in oncotic pressures result in low protein "transudates". Increased outpouring by "capillaries or cells and/or blocking of lymphatics results in high protein "exudates". Parietal Pleural Hydrostatic pressure(30) Pleural Space Visceral Pleural 11 Pressureof pleural space 8 (5) 34 Permeability of systemic circulation(34) Permeabilityof pleural fluid (8) 5+8+30-34=9 34-(5+8+11)=10 The mechanisms that lead to accumulation of pleural fluid l.Increased hydrostatic pressure in microvascular circulation.(congestive heart failure) 2.Decreased oncotic pressure in microvascular circulation.(severe hypoalbuminemia) 3 .Decreased pressure in the pleural space.(complete lung collapse) 4.Increased permeability of the microvascular circulation.(pneumonia) 5.Impaired lymphatic drainage from the pleural space, (malignant effusion) 6.Movement of fluid from peritoneal space.(ascites) Common causes of pleural effusions Transudates 1.Generalized salt and water retention, e.g. congestive heart failure, nephrotic syndrome, hypoalbuminemia. 2.Ascites, e.g., cirrhosis, meigs' syndrome, peritoneal dialysis. 3.Vascular obstruction, e.g., superior vena cava obstruction. 4.Tumor Exudates 1.Infectious diseases, e.g., TB, bacterial pneumonias, and other infectious diseeses. 2.Tumor 3.Pulmonary infarction 4.Rheumatic diseases Hemorrhagic effusion 1.Trauma 2.Tumor 3.Pulmonary infarction 4.TB 5. Spontaneous pneumothorax Chylous effusion 1.Trauma 2.Tumor 3.TB 4.Thrombosis of the left subclavian vein Empyema ; 1.TB 2.Pulmonary infection 3.Trauma 4.Esophageal rupture Bilateral effusion 1 .Generalized salt and water retention e.g., congestive heart failure, nephritic syndrome. 2.Ascites. . • 3.Pulmonaiy infarction 4.Lupus erythematosus: rheumatoid arthritis 5.Tumor 6.TB TB is the most common cause of pleural effusion , especially in young people. Malignant pleural effusion is frequently met in aged people today. p1eura1 transudation is most commonly caused by congestive heart failure. Pleurisy Pleurisy is inflammation of the pleura due to either an infectious or noninfectious cause and it may occur with or with or without p1eura1 effusion. Dry or fibrinous pleurisy: without pleural effusion Humid or exudative pleurisy: with pleural effusion. Dry pleurisy is often followed by humid pleurisy. Diagnostic procedures (1) History and physical examination Pleural pain, dyspnea, tachypnea, mild outward bulging of the intercostal spaces, decreased tactile fremitus, dullness or flatness, decreased transmission of breath and vocal sounds in the area of the effusion, and occasionally pleural friction sound in its early stage (dry pleurisy). (2)Roentgenographic examination Blunting of the normally sharp costophyrenic angle, a concave shadow with its highest margin along the pleural surface, shift of the mediastinum and the trachus toward the normal side. (3) Ultrasonic examination To localize a small pleural effusion and determine the correct site for performance of a thoracentesis. (4)Thoracentesis To aspirate the effusion for laboratory examination: Appearance, specific gravity, protein content, cell counts, glucose, LDH lipid content. Rheumatoid factor (RF), Adenisine deaminase (ADA), Lupus pleuritis (LE) cells. Gram stain and culture, and cytologic examination, etc. (5) Pleural biopsy To obtain a specimen for histologic examination and culture. Differentiation of specific types of pleural effusion 1. Transudate and exudate Tab. 1. Differentiation of transudate and exudate Transudate Cause non-inflammatory Appearance light yellow, serous Transparency clear or slightly cloudy Specific Gravity <1.018 Coagulability unable Revalta test negative Protein content <25g/L Pleural P./Serum P. <0.5 LDH <200IU/L Pleural L./SerumL. <0.6 Exudate inflammatory, tumor,physical or chemical irritation yellow, purulent turdid often >1.018 able positive >25g/L >0.5 >200IU/L >0.6 2. Bloody Effusion Bloody effusion is exudative and blood-tinted (Serosanguineous) fluid may be produced by as few as 5000 red blood cells/ mm3. Malignancy, trauma, and pulmonary infarction are the most frequent caused of bloody plural effusion, although congestive heart .failure and infection can produce serosanguinenous effusions 3. Chylous Effusion Often caused by trauma granulomatous disease or tumor and with the fluid having a characteristic milky white .appearance and high fat content. Treatment Treatment for many pleural effusions, whether transudates or exudates is primarily for the underlying pulmonary or systemic disease: aspiration of fluid is usually indicated only to establish the diagnosis and is therapeutically unnecessary except to relieve dyspnea from a large effusion. Tuberculous pleural Effusion TB remains the most common cause of pleural effusion in young people. Etiology: Tubercle bacillus Pathogenesis: Host hypersensitivity to tubercular protein in pleural tubercles (delayed hypersensitivity) Pathology: congestiopn and edema of the pleura: Cellular infiltration and an increase in vascular permeability: a fibrinous, cellular exudate in pleural surfaces (dry pleurisy); and finally a significant accumulation of fluid which is rich in plasma protein and contains cell with predominance of lymphocyte. Clinical Manifestations Generalized symptoms of toxicity of TB: Fever, high sweat, fatigue and weight loss, etc. „ Those of pleural effusion: pleuritic pain, short breath and dyspnea, etc. Pleural fluid is exudative and usually reveals lymphocytosis. Rarely pleural fluid is blood stained The PPD or OT test usually positive. Diagnosis: Based on aforementioned findings and histologic examination for granulomas and culture of material obtained at biopsy of the pleura, together with Culture of pleural fluid. Treatment (1).Standard antituberculous regimens (long course of antituberculous chemotherapy or short course therapy) (2).Administration of corticosteroid during the first several weeks of treatment. (3). Thoracentesis Empyema Thick purulent fluid with more than 100,000 cells per cubic millimeter or fluid wlth pH values less than or equal to 7.20 should be treated as a presumptive empyema. The general objectives of therapy of empyema are the elimination of both the systemic and local infection-the evacuation of pus, the obliteration of the pleural space and reexpansion of the lung, and the restoration of normal pulmonary function. Treatment of acute empyema 1 Control of infection( systemic and local) 2.Repeated thoracentesis or drainage of the empyema. Chronic empyema is primarily treated operatively, i.e. decortication. Operative therapy is also indicated in empyema with associated bronchopleural fistula or with the ipsilateral ruined lung.