Although previous viral disease is commonly invoked as a
advertisement

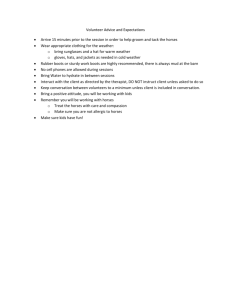
Inflammatory airway disease: Definitions and diagnosis in the performance horse Melissa R. Mazan, DVM, Diplomate ACVIM Small airway inflammatory disease, bronchiolitis, small airway disease, allergic airway disease – with a multitude of names, the definition of inflammatory airway disease remains fluid. Although low-grade inflammation of the small airways recognized as a common cause of poor performance in young to middle-aged, athletic horses, it is only recently that the clear distinction has been made between heaves, or recurrent airway obstruction, and what is most commonly known as inflammatory airway disease (IAD). Workers in the field continue to debate whether IAD is a discrete disease entity, or whether it is merely a part of the continuum of airway inflammation that, left untreated, will progress inexorably to the more well-characterized syndrome of recurrent airway obstruction (RAO, or heaves). There appears to be a consensus that horses with IAD are: generally young, although middle-aged horses may be affected, have impaired performance that may go unnoticed at rest or during light work, , have mild to moderate airway inflammation, which may involve neutrophils, mast cells, eosinophils or lymphocytes, have variable clinical signs, including cough, nasal discharge, and abnormal lung sounds , may have endoscopic evidence of tracheobronchial mucous accumulation, and may have normal lung function at rest, but show evidence of airway hyperreactivity on exposure to non-specific agents such as histamine or evidence of flow limitations on forced expiratory maneuvers. Until a rigorous definition of IAD is developed and adhered to, the prevalence of IAD will vary according to the individual researcher’s case definition. One study involving 965 Standardbreds in active racing found that 22% had evidence of mucopus at the trachea or bronchial bifurcation when examined endoscopically – although these were termed ‘COPD’ horses, undoubtedly these horses properly belong in the IAD group. Similarly, 27% of actively racing Thoroughbreds in Sweeney’s study had > 20% neutrophils in tracheal aspirate fluid, and were characterized as having IAD. Chapman, looking at Thoroughbred racehorses in training, found that a remarkable 55% of two-year olds could be classified as having lower airway disease on the basis of finding mucus in the trachea on endoscopy and inflammation on examination of transtracheal aspirate fluid, and abattoir studies have shown up to 37% of horses with histopathologic evidence of airway inflammation. Airway inflammation, regardless of whether it causes overt signs of respiratory disease, appears to be very common in performance horses. For the purposes of this paper, we will adhere to the definitions of IAD and RAO developed by the International Workshop on Equine Chronic Airway Disease. With RAO, horses have demonstrated lower airway obstruction, characterized by peak pleural pressures of at least 15 cm H2O, induced by an environmental challenge, largely reversible by use of a bronchodilator or return to nonchallenge environment, and accompanied by an increase in BALF neutrophils during challenge. In contrast, IAD refers to a nonseptic airway disease in younger, athletic horses that does not have a clearly defined allergic etiology. When we look at the data, we find that many studies involving horses with what was traditionally known as COPD or heaves, and is now more properly referred to as RAO, did not conform with these guidelines, and many of the horses would more properly be characterized as having IAD. Most workers agree that IAD is a disease of younger horses expected to perform athletic work, and as such is distinct from the picture of the dyspneic horse with overt RAO: other reported clinical signs vary widely. One of the most common findings in IAD is exercise intolerance, with or without overt signs of respiratory disease. One study found that 76% of horses referred either for routine physical examination or poor performance, and without any clinical signs or history of respiratory disease, had evidence of airway inflammation based on endoscopy and TTA findings. Horses appear to have remarkable respiratory reserve; thus subclinical airway disease may simply result in mild abnormalities on auscultation and endoscopy, and occasional coughing. Clinical signs that can be reliably detected using scoring systems usually are accompanied by significant mechanical dysfunction of the respiratory system, and are characteristic of the horse with RAO, and not IAD. The prevalence of cough in IAD horses is hard to estimate, as many studies use the presence of cough as an inclusion criterion. Other studies have shown that cough may be seen less than 16% to 50% of the time. Other clinical signs that are seen frequently include prolonged respiratory recovery, nasal discharge after exercise, respiratory embarrassment at exercise, worsening of signs during hot, humid weather, and inability to perform work during collection. Racehorses with IAD are typically described as fading during the last ¼ of the race. No single cause of IAD has been identified, although there has been plentiful speculation about the role of environment, viral disease, bacterial infection, air pollution, and genetic predisposition. Although horses with IAD do not seem to experience bouts of overt airway obstruction on exposure to an allergenic environment, organic dust associated with stabling is likely the most important contributing factor. Sweeney noted that the racehorses in her study lived in conditions of poor ventilation, and speculated that covert inflammatory disease may be instigated by the organic dusts, especially mold, in hay. Others have noted that there is more mucopus in the tracheas of horses kept in poorly ventilated conditions, and in one study, Thoroughbred racehorses in training, housed on straw, were found to be twice as likely to suffer from lower airway disease as those kept on shredded paper. More recently, Holcombe and coworkers showed that yearlings had a significantly higher number and percentage of neutrophils (PMNs as high as 18%) in BALF when they were stabled versus when they were at pasture. Although none of these horses had any clinical signs of respiratory disease or evidence of exercise intolerance, they were not in work, and subtle signs of performance impairment could easily have gone undetected. Dust levels in the horse’s breathing zone can be as high as 25 mg/m 3 – a level that would be considered unacceptable by any human workplace, and likely contributes to the development of airway neutrophilia as a nonspecific response to airway irritation. Increased levels of endotoxin in hay and grain dust also likely contribute to the development of airway neutrophilia. It is unclear at this time whether a true allergic response is developing in these horses – whether, if we could follow the natural history of horses with IAD, they eventually become horses with a dependable obstructive response to molds found naturally in the horse’s environment. 1 Although previous viral disease is commonly invoked as a predisposing factor in the development of IAD, little evidence exists to implicate viral disease. As in human asthmatics, viral respiratory disease has been shown to cause airway hyperreactivity for a period of time after infection, perhaps due to denuding of the respiratory epithelium. However, no known virus was associated with poor performance and respiratory disease in 68% of cases in the United Kingdom. Interestingly, however, one study showed that horses with heaves, as well as horses with previous respiratory viral disease, had increased IgE and IgA antibody to mold antigens when compared to horses with other chronic respiratory disease; this tempts further speculation as to the role of viral disease in the development of chronic airway inflammation. Recently, there has been considerable speculation as to the role of bacterial infection in IAD, particularly in young racehorses. A strong relationship between inflammation of the lower respiratory tract and the presence of streptococcal species as well as positive correlation between bacterial counts in TTA fluid and measures of airway inflammation was shown in one study. However, it is important to maintain a distance between association and causation, and increased numbers of bacteria may reflect impaired airway clearance rather than a causative role for the bacteria. The role of bacterial and viral infection in IAD remains unclear at this time. Horses sample the ambient air on a continual basis: it seems logical that air pollution might contribute to the development of IAD. In one study, clinically normal horses exposed to ozone had significant increases in the glutathione redox ratio as well as total iron levels – both markers of exposure to oxidizing agents - in the pulmonary epithelial lining fluid, and there was a strong correlation between airway inflammation score and the glutathione redox ratio in horses examined for poor performance but without overt airway disease. In contrast, horses living in urban environments have been shown to have less airway reactivity, although greater levels of iron in the BALF, than do horses living in rural environments. At this time, there is insufficient evidence to state definitively that exposure to air pollution increases the risk of developing IAD, but there is clearly a need for greater investigation. There may be a genetic tendency toward devellop9ing IAD. Studies have shown that humans displaying non-specific airway reactivity have an increased chance of developing clinical asthma, and it may be that horses display a similar tendency. Evidence supporting this idea exists in Hoffman’s finding that young foals without prior evidence of airway disease display a spectrum of airway reactivity on exposure to histamine aerosol, and Marti’s finding that horses with chronic bronchiolitis – which in its milder form is compatible with IAD – have a greater likelihood of having a similarly affected offspring. We will not know until widespread field-testing can be done in order to follow large populations of horses over many years. Although heaves has been clearly shown to be an allergen mediated disease, in which horses manifest a Th2-type cytokine response, and environmental challenge can produce a consistent exacerbation of disease, there is no such convincing evidence of an allergic response in horses with IAD. However, the presence of elevated numbers of mast cells in BALF of horses with poor performance and the association of BALF mastocytosis with airway hyperreactivity, as well as immunohistochemistry studies showing more IgA-containing cells and occasionally increased numbers of IgM and IgG-containing cells in the airways of horses with IAD is suggestive of a degree of allergic response and a heightened immune response. It is most likely that there are multiple factors contributing to the likelihood of an individual developing IAD – a critical level of risk factors or exposure is probably necessary for the disease to manifest itself. There are multiple methods of documenting airway inflammation. The least specific method is tracheoscopy – visualization of mucus in the trachea gives little information, however, as to the nature and the exact origin of the inflammation. However, it does lend itself easily to large studies in the field. Many workers have used, and continue to use tracheal aspirate cytology to describe the nature of inflammation in IAD. Although TTA can certainly be used to explore the presence of inflammation and has been used to document neutrophilia, mastocytosis, and eosinophilia in young performance horses, the question of the nature and exact origin again presents itself. Studies have shown poor correlation between TTA and BAL cytology; with TTA harvesting primarily neutrophils and epithelial cells, whereas BAL harvests primarily alveolar macrophages and lymphocytes in normal horses. Consequently, to avoid the problem of neutrophil count sensitivity to the collection method the recent International Workshop on Equine Chronic Airway Disease recommended use of BAL to characterize horses with chronic airway disease. Different pictures of inflammation emerge from various BAL studies, leading to speculation that different genetic predispositions and environmental exposures are important to the inflammatory phenotype. In comparison with healthy horses, BAL cytology in horses with IAD has shown, variably, both increased neutrophilia and lymphocytosis, neutrophilia and lymphopenia neutrophilia and mastocytosis, and eosinophilia. Horses with IAD have airway inflammation that may involve increases in nucleated cells, or may also involve lymphocytosis. This is distinguished from RAO by the relatively low percentage of abnormal cells in IAD – whereas horses with RAO may exhibit almost entirely neutrophils in the BALF, horses with IAD seldom have greater than 10-15% neutrophils. In our laboratory, we have established that horses with IAD will have airway inflammation BAL cytology characterized by any one of the following: mast cells > 2%, PMNs> 5%, or eosinophils> 1%. Histopathologic studies of IAD are sparse, but useful information can be ‘teased’ from COPD studies that on inspection included horses suffering from what we would more appropriately term IAD. Bronchiolar biopsies of athletic young horses with lower airway inflammation have shown inflammatory mucosal cellular infiltrates and luminal exudates, bronchiolar hyperplasia, and goblet cell metaplasia. Interestingly, in this study, 80% of supposedly normal horses had minimal evidence of peribronchiolitis – raising the question, of course, of what constitutes normal. O’Callaghan, while directing his concern to EIPH, nevertheless found plentiful evidence of multifocal, small airway –centered disease on post-mortem examination of young racehorses. These findings included thickened walls due to increased quantities of mucosal and peribronchiolar connective tissue, mononuclear bronchiolar cuffs, and extension of non-ciliated bronchiolar epithelial cells into alveolar ducts. Lakritz, looking at lung tissue of clinically normal, young Thoroughbred horses in training, found evidence of increased collagen, disruption of the epithelial basement membrane, and duplication of the epithelial basement membranes, suggesting previous airway inflammation and epithelial injury, which correlated 2 with an increased interstitial pattern on radiographs. An ultrastructural study of young horses with ‘mild COPD’ in one study found a decreased number of typical Clara cell granules and goblet cell metaplasia before the bronchioles began to show signs of inflammation typical of RAO. Although the authors state that there was good correlation between histopathology and a battery of pulmonary function tests, auscultation, bronchoscopy, blood gas, and BAL in these horses, it is a lasting disappointment that the results of the ancillary testing remain unpublished. These data in sum certainly suggest that the histopathologic lesion of IAD is not only local bronchiolar inflammation, but also remodeling and thickening of the bronchioles themselves, which lends itself to at least low-grade airway obstruction. The esophageal balloon/pneumotach method for measuring lung function tends not to detect airway obstruction even in horses with RAO in remission. However, use of the forced oscillatory technique and forced expiratory maneuvers have shown the existence of low-grade obstruction of the small airways of some horses with IAD. The mechanical behavior of the respiratory system has been shown to differ with sampling frequencies in asthmatic humans, and a pattern of decreasing respiratory system resistance with increasing frequency, termed ‘negative frequency dependence of resistance’, has been interpreted as evidence of underlying small airway obstruction despite baseline measurements within the expected range. In the lung function laboratory at TUSVM we have found that horses with IAD as a group have significantly higher values for respiratory system resistance at the lower frequencies (1-3 Hz) and mild frequency dependence of resistance compared to controls, although the baseline measurement of respiratory system resistance may still frequently fall within the normal range. Both Young and Mazan have demonstrated the existence of frequency dependence of resistance in horses with overt heaves, and suggest that it implies the existence of airway obstruction. The question, of course, remains as to the physical meaning of this physiological phenomenon. Does this represent static airway obstruction in parallel airways, or does it represent a failure of the elastic tissue to defend the airway from closure? Couetil has used a method for forced expiratory maneuvers to demonstrate that considerable flow limitations existed in a horse with mild heaves in which clinical examination and lung mechanics data were normal, and measures of forced expiratory flow (FEF95%) was lower in horses with IAD than in normal horses; this further supports the idea that the esophageal balloon/pneumotach method of measuring lung mechanics, as with humans, is insensitive to subclinical, low-grade small airway obstruction. The finding that reduction of the diameter of the bronchiolar lumen by epithelial hyperplasia was found to be inversely correlated with O2 uptake capacity and tidal volume is strongly supportive of the existence of airway obstruction in IAD. Consequently, without dynamic, frequency dependent tests of lung function, forced maneuvers, or bronchoprovocation, it seems that we are failing to document a common feature of small airway obstruction in horses with IAD simply because our testing devices are not sufficiently sensitive to these changes. Horses with clinical signs compatible with IAD also exhibit signs of airway hyperreactivity when they are exposed to nonspecific agents such as histamine aerosol. Similar airway hyperreactivity is seen prominently in human asthmatics, both during periods of remission and during exacerbations of disease. The basis for airway hyperreactivity remains hotly debated among pulmonary physiologists. It is likely a multifactorial phenomenon, which has been associated with airway wall thickening undetectable by conventional lung function testing, airway inflammation, and autonomic nervous system dysfunction. There is a paucity of information concerning the mediators of airway hyperreactivity in horses with IAD, although the presence of elevated levels of leukotriene C4 levels has been documented. In our laboratory, horses with a clinical history and signs compatible with IAD have significantly greater airway reactivity than controls, although some control horses display airway hyperreactivity. How does IAD affect performance? This is a question whose answer depends on the methods of the particular investigator. A practitioner with a primarily pleasure horse or show hunter clientele might report a very low incidence of IAD in younger horses, because their level of exercise is not likely to force a diagnosis through signs of exercise intolerance. A racetrack practitioner, on the other hand, would be far more likely to detect exercise intolerance due to lower airway disease in young horses because the level of expected athletic output is much higher, and the horses have a greater likelihood of being examined endoscopically. Indeed, researchers looking at Standardbred racehorses found that those with excessive tracheal mucus performed at a lower level than those with no mucus found on endoscopy. Persson, looking at Standardbred trotters and saddle horses with what was effectively inflammatory airway disease, found that IAD does affect ventilatory capacity – but that this had a different manifestation in racehorses as opposed to saddle horses. Not only were the saddle horses significantly older than racehorses when airway disease was detected, but affected racehorses had decreased minute volume and an increased red blood cell to body weight ratio, whereas the affected saddle horses manifested tachycardia during exercise. These differences in physiological response to exercise in were likely influenced by the demands placed on racehorses versus those placed on riding horses. Moreover, using bronchiolar biopsy, Persson was able to demonstrate that oxygen uptake and pulmonary ventilation correlated inversely with the morphological grade of small airway disease and the height of the bronchiolar epithelium – the last finding suggesting that the extent of obstruction may determine the extent of exercise impairment. Similarly, Couetil and Nyman found in separate studies that horses with IAD undergoing a treadmill stress test demonstrated a more severe impairment of gas exchange during peak exercise than did normal horses. Other studies have found that horses with obvious evidence of airway inflammation do not necessarily have a history of exercise intolerance. This may reflect the difficulty of diagnosing low-grade respiratory impairment, and the trainer’s failure to recognize poorer performance than nature intended, however, rather than the benign nature of the underlying disease. Inflammatory airway disease in young horses has thus far given us far more questions than answers, and much work remains to be done. If we can discover the mechanism of airway hyperreactivity, the stimulus for inflammation, and the role that genetics and environment plays in IAD, we may be able to modify the development of disease in young horses. The suspicion that IAD, left untreated, will eventually develop into the crippling disease, RAO, only heightens our concern, and our stimulus to solve the many mysteries of IAD. 3 4