Psychiatric co-morbidities in autistic spectrum disorders.
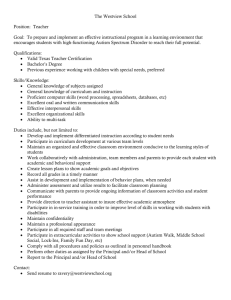
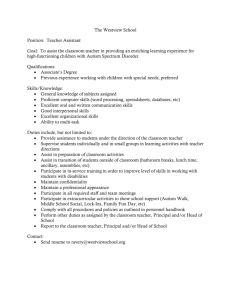
advertisement

Eleri Clissold London Division Essay Prize 2012 The Royal College of Psychiatrists London Division Essay Prize 2012 Suffering in silence Psychiatric co-morbidities in autistic spectrum disorders Name: Eleri Clissold Medical school: King’s College London Email: eleri.clissold@kcl.ac.uk Word count: Total 4,449 Abstract: This essay briefly summarizes the current literature regarding depression in those with autistic spectrum disorders (ASD) and in doing so illustrates the urgent need for further research in this area. The prevalence of depression in ASD remains unclear although is likely to be significantly greater than in the general population. Presentation is complex and heterogeneous. Challenges in the diagnosis of depression in ASD are broadly two-fold; 1) features of ASD which overlap with depression and 2) features limiting the expression of depression. This is complicated by the absence of a specific diagnostic framework for this condition. Many areas of depression in ASD remain poorly understood including treatment and aetiology; however it is thought that depression in this group responds to conventional anti-depressive therapy. This essay briefly explores the role which stigma and a lack of support may play in the development of depression in ASD. Conclusion: There is a dire need for a sizeable and reliable evidence base in this area, this would significantly reduce preventable suffering in this group. The possibility that social factors may be driving such suffering requires urgent exploration. Eleri Clissold London Division Essay Prize 2012 Introduction Autism has come a long way from Kanner’s “infantile schizophrenia”1 and misguided notions of “refrigerator mothers” 2 to a well-recognized pervasive developmental disorder. Today the National Autistic Society has over 20,000 members and educational interventions, such as the Picture Exchange Communications System, have transformed the prospects of many3-5 (p.37). The prevalence of autism has grown steadily over the last four decades and shows no sign of abating with 1% of school children currently estimated to suffer some form of autism6. With this in mind research into this area has never been timelier. The numerous and frequent physical co-morbidities associated with autistic spectrum disorders (ASD) are well documented in the literature. However it is only within the last decade that psychiatric co-morbidities have begun to receive due recognition in both research and clinical practice, with meta-analyses of what sparse data exists and clear, concise calls for further research7,8. This essay will briefly review literature concerning depression in ASD which is widely considered the most common and best documented of autism’s psychiatric co morbidities8. In doing so the aim is to highlight the alarming lack of literature on the subject and speculate as to consequences and causes of this trend. Autistic spectrum disorders (ASD) in this context will refer to autism, PDD-NOS (Pervasive Developmental Disorder Not Otherwise Specified, when the diagnostic criteria for autism are partially fulfilled), high-functioning autism (HFA) and Asperger’s syndrome (AS). This essay will assume the ICD-10 definition, that autism involves a developmental impairment recognised before the age of three years with three key areas of psychopathology; communication, social interaction, and stereotyped, repetitive behaviour. Additional common problems include temper tantrums, aggression towards self or others, phobias, disturbed sleep, and abnormal eating patterns. Where learning disability (LD) is referred to this is assumed to mean an IQ of below 709. Given the limited material concerning depression in ASD this discussion will lay aside extensive nosological debate on the role of AS within the autistic spectrum (see Matson & Wilkins10) and consider the entire autistic spectrum including AS, across all age groups. It is important to note the vast variation within the autistic spectrum, from non-verbal and highly dependent to those with AS or HFA with little to no LD and who may be in employment or may be parents11. For the purposes of this essay this variation will only be taken into account where existing material on the subject allows. It is likely that in practice the presentation and needs of those with ASD and depression will vary as greatly as the autistic spectrum itself. Throughout this essay the term depression will refer to isolated or recurrent episodes of classical mild, moderate or severe depression in the absence of mania. Clinically this classically presents with low mood (with diurnal variation), reduced energy and a decrease in activity. Additional symptoms include reduced concentration, libido, interest, and capacity for enjoyment, marked tiredness after minimum exertion, disturbed sleep and appetite, ideas of guilt or worthlessness and low self-esteem and self-confidence9. Prevalence The prevalence of depression and autism in any age group is yet to be conclusively established. Some commentators have estimated the figure as high as 65%12 although 5-34% is a more accepted range8(p.105). This sizeable variation Eleri Clissold London Division Essay Prize 2012 is likely due to the dramatic differences in methodology; study setting, sample size, diagnostic criteria, sampling techniques and study period. A recent literature review noted that the largest study had just 85 participants with most studies either published as case reports or clinic studies with around 20 participants8(p.108). In the absence of large scale, population based studies the precise prevalence of co-morbid depression in ASD will remain unclear. With such variation in methodology it could be argued that there may not be a significant relationship between depression and autism, however numerous case reports, small scale studies and an abundance of anecdotal evidence over the past 60 years strongly suggests a high frequency of coexistence7. Furthermore Kim and colleagues13 found a prevalence rate of depression of 16.9% in children aged 10-12 years with HFA and AS when followed up over six years. This result was significant when compared to a control group in the community. In the same year point prevalence of depression in the UK was in the range of 3-7%14 and was thought to be 1.8% in pre-pubertal school aged children in 199515. The prevalence of depression in the general population appears to be substantially lower than all estimates of depression in autistic populations8. It therefore seems reasonable to assume a trend worthy of further investigation exists. Presentation Depression in ASD embodies the same features as depression in the general population although the way those features are expressed in ASD is extremely variable16. Some diagnostic challenges are identical to those faced in diagnosing co-morbid depression in LD, although many are related to features unique to autism17. Commonly reported symptoms are increased irritability or crying and sad facial expressions. However facial expressions in ASD are characteristically neutral or difficult to interpret and both verbal and non-verbal communication is limited. Communication difficulties are especially pronounced around mentalizing and expressing complex emotions such as shame and embarrassment. In combination these factors impair the expression of depressive symptoms18-20. Consequently cases are almost exclusively reported by a third party - parent, carer or health care professional (see Ghaziuddin & Tsai21 for an exception) - and often present when the disease has progressed significantly22. Other common symptoms are changes in sleep and appetite, most often although not exclusively, insomnia8. However sleep disturbance is a common feature of ASD in the absence of psychiatric co-morbidities. A recent study found 37.5% of children with autism suffered from chronic sleep problems compared to just 8.6% of controls and that those in the control group were more likely to remit over time23. Similarly loss of interest, social withdrawal and psychomotor retardation have been cited as symptoms of depression in ASD, however the social dysfunction and abnormal patterns of speech commonly observed in autism may well enhance or obscure such symptoms. Other less common depressive symptoms in HFA and AS include suicidal ideation, attempted or completed suicide and alcoholism20,22 Some symptoms notably associated with the autistic spectrum have been shown to increase or begin with the onset of depression, namely aggression, injury to self, total withdrawal and oppositional behaviour (e.g. refusing to leave home). Although it is important to note that other factors – such as stress, change in routine or physical illness – and not solely depression may result in an increase in such behaviours8. Eleri Clissold London Division Essay Prize 2012 Paradoxically there has been speculation as to whether depression may decrease other maladaptive behaviours. Obsessions and repetitive behaviours are key features of autism, playing a crucial role in diagnosing the condition as one of three key areas of psychopathology in the ICD-10 criteria9. Repetitive behaviours can vary from simple echolalia and hand flapping to more complex ritualistic behaviours. Such behaviours have been shown to predict the severity of autism and can cause substantial parental anxiety24,25. If these maladaptive behaviours decrease in frequency, this will often be viewed as an improvement in the individual rather than a feature of a depressive illness. Although there is little evidence behind this theory cases have been reported of depressed individuals losing interest in repetitive behaviours and obsessional themes26. Complex behaviours unique to autism and features related to LD muddy the waters when it comes to identifying depression. Clearly the presentation of depression in the autistic spectrum is multi-faceted and not yet fully understood. Mis-diagnosis or a failure to diagnose is therefore understandably a significant risk. Diagnosis In spite of such significant risks no specific diagnostic criteria of any kind, selfreported or third-party, exists. In the absence of such a framework it is likely that an approach in clinic similar to that advocated by Lainhart & Folstein27 may be taken. Firstly deterioration in activity, behaviour, language or cognition is considered. This is then placed in the context of that individual’s baseline interests and activity, and a pattern established. Finally a mental state is taken, directly or by collateral history, with particular interest paid to symptoms of depression particular to autism. In light of this it is understandable that some commentators consider it essential for all psychiatrists to have an in-depth understanding of ASD28. Studies have previously attempted to use a number of different pre-existing scales with varying degrees of success. The Beck Depression Inventory29 and the Hamilton rating scale for depression30 arguably constitute the gold standard in assessing and monitoring depression. However they’re seldom used in the context of autism as, although core in classical depression, feelings of guilt, anxiety, suicidality and reduced concentration levels are infrequently reported symptoms of depression in ASD8. Unsurprisingly where these scales have been administered several items were unrecordable. Even when adapted, many questions remained challenging for the individual in question or for their carers to answer on their behalf, such as subjectively rating mood21. Equally by these frameworks assessment of interest in activities, social withdrawal, psychomotor retardation, sleep and appetite may be misleading whilst autism-specific maladaptive behaviours remain unassessed8. Conversely, reflecting the significant variation in abilities within the autistic spectrum, selfreporting scales have been used with some success in AS. One account reports how the structured nature of the Children’s Depression Inventory (a derivative of the Hamilton30 rating scale for depression) and the ability to explain his mood using numbers appealed to the individual’s style of thinking31. Other studies have used semi-structured interview tools based on DSM-III-R criteria; the Diagnostic Interview for Children & Adolescents32, the revised Ontario Child Health Study33 and the Kiddie Schedule for Affective Disorders & Schizophrenia34. Although specific to children they screen for a number of psychiatric conditions and again Eleri Clissold London Division Essay Prize 2012 fail to account for features of depression unique to autism8. Similarly the Disability Assessment Schedule35 and the Reiss scale36 consider a wide range of behavioural abnormalities (including non-verbal communication and social interaction), are specific to LD, carer-rated and retrospective although again screen for a wide array of psychiatric conditions. Seemingly no scale or rating system ticks all the required boxes, however a more recent diagnostic criterion for LD may hold promise. This framework ignores complex emotions and suicidal ideation, focusing instead on other DSMIV criteria such as loss of confidence, tearfulness, increased reassurance seeking and challenging behaviours37. Stewart et al8 concluded that modifying the DC-LC was essential, and suggested suitable adjustments to the scale, namely; recurrent thoughts of death (not simply fears of dying), incontinence and an increase in aggression (towards self or others). Treatment Given the uncertainty in prevalence and highly variable presentation it follows that randomised control trials of anti-depressant therapy in this patient group are lacking. However, the existing evidence is encouraging. Both depressive symptoms and behavioural problems have been observed to improve with pharmacological treatment38,39. Isolated cases have also been noted of successful treatment with electro-convulsive therapy and cognitive behavioural therapy40. There have also been reports of depression only being recognised once antidepressant treatment has been administered8. This could mean that depressive symptoms in ASD are a variant presentation of this common affective disorder and therefore less likely to form part of the autistic phenotype. Predisposing, precipitating & perpetuating factors The role of affective disorders within the autistic phenotype has been the subject of much debate and without a clear understanding of the genetic basis of autism it’s likely that this debate will remain unresolved41. Until genetic predisposition is better understood it seems prudent if not essential to question the role of other precipitating and perpetuating factors. A well-established feature of autism is the tendency for minor environmental change to cause extreme distress. This distress and subsequent resistance to the unexpected is thought to be due to a difficulty in understanding environmental change leading to fear and uncertainty42. It is unsurprising therefore that high levels of anxiety have been noted in this group43. Depression and anxiety have a complex relationship and studies in non-autistic populations have shown anxiety to underlie many cases of depression44. Reproducing this work in those with ASD would certainly be of merit. Equally there is limited research into the impact of life events, social circumstances and quality of life on depression in this group8. It should be noted that in all likelihood precipitants of depression in the general population are likely apply to those with ASD e.g. bereavement or loss, loneliness, feeling a failure and sexual frustration. Many of these precipitants may be more commonly experienced by those with ASD due to pressures on the family and complex social circumstances resulting from autism22. Affective disorders are thought to occur at a higher rate in parents of children with autism than in parents of non-autistic children. Although this has caused much academic Eleri Clissold London Division Essay Prize 2012 interest into a potential genetic link between parental affective disorder and autism, this phenomenon is far from understood40. There is also an abundance of qualitative evidence suggesting that perceived stigma and lack, or perceived lack, of social support are major precipitants (e.g. Mickelson45, 2001; Gray & Holden23, Gray46). Testament to this is the fact that over 50% of children are not in the kind of schooling environment their parents believe would support them best and one fifth of have been excluded from school at some point47. Depression is thought to be more common in those with HFA and AS as opposed to other forms of autism because of a deeper insight into the condition and a heightened sense of this social isolation and stigma7,39. Depression in ASD is thought to peak during late adolescence and early adult years and a direct link between high levels of peer victimization and suicidal ideation has been shown in this group16,20. 40% of young people with ASD have experienced some form of bullying, some have even been accused of harassment in their attempts to form relationships. Autism advocacy groups cite lack of support as a major obstacle and cause of mental illness for those with autism in the UK, with only around a third of autistic adults in England reporting that they feel adequately supported. Despite 61% of those out of employment saying they would like to work just 15% of adults with autism are currently employed5,46,48. With over whelming social isolation, a lack of support, unemployment and subsequent low self-worth it’s clear that social factors have a major role in depression in ASD. Conclusion Throughout this essay a lack of high quality data - in prevalence, presentation, treatment and aetiology - has been a theme. This has posed a significant problem in attempting to draw meaningful conclusions, although clearly illustrates the principal argument of this essay: that there is evidence to suggest that extensive research in this area is urgently needed. Depression has consistently been estimated at a significantly higher rate in autistic groups than in the general population. By its very nature ASD places pressure on carers and health care professionals to recognize and report psychiatric co-morbidities however diagnosis is complex and fraught with pitfalls, especially for clinicians without an in-depth knowledge of the autistic spectrum49. In addition most studies use child or adolescent samples when it’s widely agreed that adolescents and young adults are more prone to depression than children16. All this considered and in the absence of a suitable diagnostic framework it seems entirely likely that the prevalence of this condition may be higher than many studies estimate. As a result individuals with autism may be silently suffering the debilitating effects of depression in the face the effective treatment. Reports of diagnoses being made on the basis of therapeutic trials of antidepressants are further support of this. Thorough scientific exploration of this area would also be of nosological merit. Conclusively establishing the role of affective disorders in the autistic phenotype seems highly unlikely until the genetic basis of autism is better understood. That said it stands to reason that a solid understanding of how social factors influence the development of affective disorders in those with ASD could help strongly inform hypotheses in this area. Eleri Clissold London Division Essay Prize 2012 Similarly Klin and colleagues13 attempted to use depression as a means of distinguishing AS from HFA. Despite significant advances in the disability right’s movement and in understanding autism, those effected by autism face alarming levels of stigma and social isolation. It seems some of the most pressing work lies around establishing the precise relationship between stigma, social support and mental health in this population. If depression is being driven even in part by a social phenomenon then social interventions - campaigns, policies and education become as or even more important than pharmacological treatments, as an element of this suffering is then preventable rather than merely treatable. Just fifteen case reports of co-existent ASD and depression have been documented in the literature over six decades. In spite of a clearly documented high parental rate of affective disorders there has been little speculation as to the link between parental depression and depression in children with ASD. Kanner himself noted a tendency to “momentary fits of depression” within his original cohort1 and yet psychiatric co-morbidities have been neglected in the literature, especially when compared to physical co-morbidities of ASD. Could we be prejudiced as a medical profession? Or perhaps hold a misconception that depression doesn’t affect those with severe LD? This is clearly something that warrants extensive further consideration. This essay inevitably raises more questions than answers although has clearly demonstrated a pressing need for research surrounding depression in ASD, particularly with regards to prevalence and social precipitants. Eleri Clissold London Division Essay Prize 2012 Acknowledgements Many thanks to the staff, patients and families at the King’s College London Child & Adolescent Psychiatry unit for igniting my interest in neuropsychiatry. In particular thank you to my supervisor Dr M.T. Lax-Pericall for her guidance in writing this essay. Eleri Clissold London Division Essay Prize 2012 References 1. Kanner, L., 1943. Autistic disturbances of affective contact. Nerv Child, 2, pp.217–50. Kanner, L., 1968. Reprint. Acta Paedopsychiatr, 35(4), pp.100–36. 2. Kanner, L., 1949. Problems of nosology and psychodynamics in early childhood autism. American Journal of Orthopsychiatry, 19(3), pp.416–26. 3. Bondy, A.S., Frost, L.A., 1994. The Picture Exchange Communication System. Focus Autism Other Developmental Disabilities, 9(3), pp.1-19. 4. The National Autistic Society, 2011. About Us. Online. Available at: http://www.autism.org.uk/news-and-events/about-the-nas/our-story.aspx [Accessed: Dec 1st 2011] 5. Rosenblatt, M., 2008. I Exist: the message from adults with autism in England. London: The National Autistic Society, p3, 6. Baron-Cohen, S., Scott, F.J., Allison, C., Williams, J., Bolton, P., Matthews, F.E., 2009. Prevalence of autism-spectrum conditions: UK school-based population study. The British Journal of Psychiatry, 194, pp.500-509. 7. Ghaziuddin, M., Ghaziuddin, N., Greden, J., 2002. Depression in Persons with Autism: Implications for Research and Clinical Care. Journal of Autism and Developmental Disorders, 32, p.4. 8. Stewart, M.E., Barnard, L., Pearson, J., Hasan, R., O'Brien, G., 2006. Presentation of depression in autism and Asperger syndrome : A review. Autism, 10, p.103. 9. WHO, 2010. International Classification of Disease (ICD-10). Online. Available at: http://apps.who.int/classifications/icd10/browse/2010/en#/V [Accessed: 27th Nov 2011] 10. Matson, J.L., Wilkins, J., 2008. Nosology and diagnosis of Asperger’s syndrome Research. Autism Spectrum Disorders, 2, pp.288–300. 11. Semple, D., Smyth, R., 2009. Oxford Handbook of Psychiatry. Ed 2, Oxford: Oxford University Press. 12. Ghaziuddin, M., Weidmer-Mikhail, E., Eidemer-Mikhail, L.E., Ghaziuddin, N.,1998. Comorbidity of Asperger Syndrome: A Preliminary Report. Journal of Intellectual Disability Research, 42, pp.279–83. 13. Klin, A., Pauls, D., Schultz, R., Volkmar, F., 2005. Three Diagnostic Approaches to Asperger Syndrome: Implications for Research. Journal of Autism and Developmental Disorders, 35(2), pp.221-234. 14. SANE, 2000. Depression and manic depression. Available at: http://www.samaritans.org/your_emotional_health/publications/depression_an d_suicide.aspx [Accessed on: 29th Nov 2011] 15. Angold, A., Costello, J., 1995. The epidemiology of depression in children and adolescents In: Goodyer, M., ed. The Depressed Child and Adolescent – Developmental and Clinical Perspectives. Cambridge: Cambridge University Press, pp. 127-47. 16. Tantam, D., Prestwood, S., 1999. A mind of one's own: a guide to the special difficulties and needs of the more able person with autism or Asperger syndrome. 3rd ed. London: National Autistic Society 17. Ghaziuddin, M., Tsai, L., Ghaziuddin, N., 1992. Comorbidity of Autistic Disorder in Children and Adolescents. European Child and Adolescent Psychiatry, 1(4), pp. 209-213. 18. Bieberich, A.A., Morgan, S.B., 1998. Brief Report: Affective Expression in Children with Autism or Down Syndrome. Journal of Autism and Developmental Disorders, 28, pp.333–8. Eleri Clissold London Division Essay Prize 2012 19. Capps, L., Yirmiya, N., Sigman, M., 1992. Understanding of Simple and Complex Emotions in Non-Retarded Children with Autism. Journal of Child Psychology & Psychiatry & Allied Disciplines, 33, pp.1169–82. 20. Shtayermman, O., 2007. Peer victimization in adolescents and young adults diagnosed with Asperger’s Syndrome: a link to depressive symptomatology, anxiety symptomatology and suicidal ideation. Issues in Comprehensive Pediatric Nursing, 30, pp.87–107. 21. Ghaziuddin, M., L., Ghaziuddin, N., 1991. Fluoxetine in Autism with Depression. Journal of the American Academy of Child & Adolescent Psychiatry, 30: 508–9. 22. The National Autistic Society, 2011. Mental Health & Asperger’s Syndrome. Online. Available at: http://www.autism.org.uk/working-with/health/mentalhealth-andasperger-syndrome.aspx [Accessed: Dec 2nd 2011] 23. Sivertsen, B., Posserud, M., Gillberg, C., Lundervold, A., Hysing, M., 2011. Sleep problems in children with autism spectrum problems: a longitudinal populationbased study. SAGE and The National Autistic Society, 15(3), pp.1–15. 24. Bodfish, J.W., Symons, J.F., Parker, D.E., Lewis, M.H., 2000. Varieties of Repetitive Behaviour in Autism: Comparisons to Mental Retardation. Journal of Autism and Developmental Disorders, 30(3), pp.237-243. 25. Gray, D.E., Holden, W.J., 1992. Psycho-social well-being among the parents of children with autism. Australia and New Zealand Journal of Developmental Disabilities, 18(2), pp.63-93. 26. Gillberg, C., 1985. Asperger’s Syndrome and Recurrent Psychosis: A Case Study. Journal of Autism and Developmental Disorders, 15, pp.389–97. 27. Lainhart, J.E., Folstein, S.E., 1994. Affective disorders in people with autism: a review of published cases. Journal of Autism and Developmental Disorders, 24(5), pp.587-601. 28. Attwood, T., 1998. Asperger's syndrome: a guide for parents and professionals. London: Jessica Kingsley. 29. Beck, A.T., Ward, C.H., Mendelson, M., Erbaugh, J., 1961. An Inventory for Measuring Depression. Archives of General Psychiatry, 4, pp.561–71. 30. Hamilton, M., 1960. A Rating Scale for Depression. Journal of Neurology, Neurosurgery & Psychiatry, 23, pp.56–62. 31. Barnhill, G.P., 2001. Social Attribution and Depression in Adolescents with Asperger Syndrome. Focus on Autism and Other Developmental Disabilities, 16, pp.46–53. 32. Herjanic, B., Campbell, J.W., 1977. Differentiating Psychiatrically Disturbed Children on the Basis of a Structured Interview. Journal of Abnormal Child Psychology, 5, pp.127–35. 33. Kim, J.A., Szatmari, P., Bryson, S.E., Steiner, D.L., Wilson, F.J., 2000. The Prevalence of Anxiety and Mood Problems among Children with Autism and Asperger Syndrome. Autism, 4, pp.117–32. 34. Puig-Antich, J., Orvaschel, H., Tabrizi, M.A., Chamber, W., 1980. Schedule for Affective Disorders and Schizophrenia for School-Age Children: Epidemiological Version (Kiddie- SADS-E). 3rd ed. New York: New York State Psychiatric Institute and Yale University School of Medicine. 35. Holmes, N., Shah, A., Wing, L., 1982. The Disability Assessment Schedule: A Brief Screening Device for Use with the Mentally Retarded. Psychological Medicine, 12, pp.879–90. Eleri Clissold London Division Essay Prize 2012 36. Reiss, S., 1990. Reiss Scales for Children’s Dual Diagnosis (Mental Retardation and Psychopathology). Worthington, OH: International Diagnostic Systems Inc. 37. Royal College of Psychiatrists, 2001. DC-LD: Diagnostic Criteria for Psychiatric Disorders for Use with Adults with Learning Disabilities/Mental Retardation. Occasional Paper Royal College of General Practitioners, 48. 38. Perry, D.W., Marston, G.M., Hinder, S.A.J., Munden, A.C., Roy, A., 2001. The Phenomenology of Depressive Illness in People with a Learning Disability and Autism. Autism, 5, pp.265–75. 39. Tsakanikos, E., Costello, H., Holt, G., Bouras, N., Sturmey, P., Newton, N.J., 2006. Psychopathology in Adults with Autism and Intellectual Disability. Autism Dev Disord, 36, pp.1123–1129. 40. Wachtel, E.L., Griffin, M., Reti, I.M., 2010. Electroconvulsive Therapy in a Man With Autism Experiencing Severe Depression, Catatonia, and Self-Injury. The Journal of ECT, 26 (1), pp.70-73. 41. Yirmiya, N., Shaked, M., 2005. Psychiatric disorders in parents of children with autism: a meta-analysis. Journal of Child Psychology and Psychiatry, 46(1), pp.69–83. 42. Groden, J., Cantela, J., Prince, S., Berryman, J., 1994. The Impact of Stress and Anxiety on Individuals with Autism and Developmental Disabilities, in Schopler, E., Mesibov, G.B., (eds) Behavioural Issues in Autism. New York: Plenum. 43. Gillott, A., Furniss, F., Walter, A., 2001. Anxiety in High-Functioning Children with Autism. Autism, 5, pp.277–86. 44. Kendler, K.S., Neale, M.C., Kessler, R.C., Heath, A.C., Eaves, L.J., 1993. A Longitudinal Twin Study of Personality and Major Depression in Women. Archives of General Psychiatry, 50(11), pp.853–62. 45. Mickelson, K.D., 2001. Perceived stigma, social support, and depression. Pers Soc Psychol Bull, 27(8), pp.1046-1056. 46. Gray, D., 2002. “Everybody just freezes. Everybody is just embarrassed”: Felt and enacted stigma among parents of children with high functioning autism. Sociology of Health and Illness, 24(6), pp.734-749. 47. Batten, A., 2006. Autism and education: the reality for families today. London: The National Autistic Society, p3. 48. Redman, S., 2009. Don't Write Me Off: Make the system fair for people with autism. London: The National Autistic Society, p8. 49. Howlin, P., Moorf, A.,1997. Diagnosis in Autism: A Survey of Over 1200 Patients in the UK. Autism, 1(2), pp.135-162. Eleri Clissold London Division Essay Prize 2012 Bibleography Ghaziuddin, M., Tsai, L., 1991. Depression in Autistic Disorder. British Journal of Psychiatry, 159, pp.721–3. Green, J., Gilchrist, A., Burton, D., Cox, A., 2000. Social and Psychiatric Functioning in Adolescents with Asperger Syndrome Compared with Conduct Disorder. Journal of Autism and Developmental Disorders, 30, pp.279–93. Tsiouris, J.A., Cohen, I.L., PATTI, P.J., Korosh, W.M., 2003. Treatment of Previously Undiagnosed Psychiatric Disorders in Persons with Developmental Disabilities Decreased or Eliminated Self-Injurious Behavior. Journal of Clinical Psychiatry, 64(9), pp.1081–90. Wing, L. (2002). The autistic spectrum: a guide for parents and professionals. London: Constable and Robinson