Pleural Effusion
advertisement

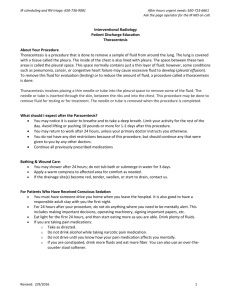
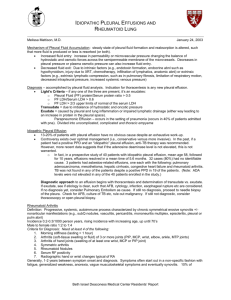
Critical Care Nursing Theory Pleural effusion Pleural Effusion - The pleural space is a potential space between the visceral pleurae that lines the lungs and the parietal pleurae that lines the interior chest wall. - There is a continuous flow of fluid from the parietal pleura of the chest wall to the visceral pleura, and the fluids eventually absorbed by the pulmonary lymphatics. - The pleural cavity is only a potential space because in health the two layers of pleura are separated by only a thin film of serous fluid, sufficient to prevent friction between them during breathing. The serous fluid is secreted by epithelial cells of the membrane. Pathophysiology 1- An increased rate of fluid formation, 2- A decreased rate of fluid removal, 3- Both. The causative mechanisms:1- Increased pressure in subpleural capillaries or lymphatics, 2- Increased capillary permeability, 3- Decreased colloid osmotic pressure of the blood, 4- Increased intrapleural negative pressure, 5- Impaired lymphatic drainage of the pleural space. Types of pleural effusion:1- Transudative pleural effusion. 2- Exudative pleural effusion. Pathophysiology and Etiology May be either transudative or exudative. Transudative effusions occur primarily in noninflammatory conditions; is an accumulation of low-protein, low cell count fluid. Dr. Sahar Hossni El-Shenawi- Assistant Professor Of Critical Care Nursing 1 Critical Care Nursing Theory Pleural effusion Exudative effusions occur in an area of inflammation; is an accumulation of high-protein fluid. Occurs as a complication of: o Disseminated cancer (particularly lung and breast), lymphoma. o Pleuropulmonary infections (pneumonia). o Heart failure, cirrhosis, nephrosis. o Other conditions: sarcoidosis, systemic lupus erythematosus (SLE), peritoneal dialysis. - Mechanisms that produce these effusions include 1- Ischemia-induced increased pleural capillary permeability, 2- Imbalance in vascular and pleural space hydrostatic pressures, 3- Pleuropulmonary hemorrhage. - A hemothorax is a bloody exudative pleural effusion and is diagnosed by a pleural fluid-to-blood hematocrit ratio greater than 50%. - Hemothorax can result from 1- Trauma is the most common cause of a hemothorax 2- Invasive procedures (placement of central venous catheter, thoracentesis), 3- Pulmonary infarction, malignancies, 4- A ruptured aortic aneurysm. 5- As a rare complication of anticoagulation therapy. Assessment ● Subjective findings:- Shortness of breath and pleuritic chest pain, depending on the amount of fluid accumulation. ● Objective findings:1- Tachypnea and hypoxemia if ventilation is impaired, 2- Dullness to percussion, Dr. Sahar Hossni El-Shenawi- Assistant Professor Of Critical Care Nursing 2 Critical Care Nursing Theory Pleural effusion 3- Decreased breath sounds over the involved area. Diagnostic Studies - A lateral decubitus chest radiograph is the best demonstration of free pleural fluid. - Diagnostic thoracentesis (aspiration of fluid from the pleural space) when a pleural effusion is suspected on the basis of physical examination and is confirmed radiologically, it is necessary to obtain a sample of pleural fluid for diagnosis. - The laboratory tests performed on the pleural fluid obtained by thoracentesis (Evaluation of the pleural fluid is necessary to distinguish transudative from exudative effusions.) Test Red blood cell count >100,000/mm3 Hematocrit >50% of peripheral blood White blood cell count (WBC) >50,000–100,000/mm3 >50% Neutrophils >50% Lymphocytes >10% Eosinophils >5% Mesothelial cells Glucose <60 mg/dL Amylase >200 units/dL pH <7.2 Comment Trauma, malignancy, pulmonary embolism Hemothorax Grossly visible pus, otherwise total WBC less useful than WBC differential Acute inflammation or infection Tuberculosis, malignancy Most common: hemothorax, pneumothorax; also benig Asbestos effusions, drug reaction, paragonimiasis; tuberculosis less likely Infection, malignancy, tuberculosis, rheumatoid Pleuritis, esophageal perforation, pancreatic disease, malignancy, ruptured ectopic pregnancy Isoenzyme profile: salivary–esophageal disease, malignancy (especially lung) Isoenzyme profile: pancreatic–pancreatic disease Infection (complicated parapneumonic effusion and empyema), malignancy, esophageal rupture, rheumatoid Dr. Sahar Hossni El-Shenawi- Assistant Professor Of Critical Care Nursing 3 Critical Care Nursing Theory Triglyceride >110 mg/dL Microbiological studies Cytology Pleural effusion or lupus pleuritis, tuberculosis, systemic acidosis, urinothorax Chylothorax Etiology of infection Diagnostic of malignancy - When the distance between the pleural fluid line to the inside of the chest wall on lateral decubitus view is less than 1 cm:- It is difficult to obtain the pleural fluid by thoracentesis - The pleural effusion is not likely to be clinically significant. - The associated risk of pneumothorax outweighs the benefit of the thoracentesis. Management - Treatment of the underlying cause is necessary. - Removal the pleural effusion by thoracentesis or chest tube placement may be indicated depending on the etiology and size of effusion. (The primary indication for therapeutic thoracentesis is relief of dyspnea.) Thoracentesis In thoracentesis, a needle is inserted into the pleural space - To remove air, fluid, or both; - To obtain specimens for diagnostic evaluation; - To instill medications. A chest radiograph, coagulation studies, and patient education are essential before a thoracentesis. Some patients may require medication to reduce anxiety. Unlike bronchoscopy, thoracentesis requires the cooperation of the patient; Therefore, a local anesthetic, rather than moderate sedation, is used to minimize the pain and discomfort that accompanies the procedure. Dr. Sahar Hossni El-Shenawi- Assistant Professor Of Critical Care Nursing 4 Critical Care Nursing Theory Pleural effusion During the procedure, the patient is placed either in a chair or on the edge of the bed in an upright position with arms and shoulders raised so that the ribs lift and separate, allowing easier needle insertion. If a patient is unable to lift his or her arms, sitting on the bed with the arms placed above the head on a table is an alternative position. During thoracentesis, the nurse’s primary functions are:1- Provide comfort for the patient, 2- Perform ongoing assessment of the patient’s respiratory system, 3- Dress the wound with sterile dressings on completion of the procedure, 4- Send labeled laboratory specimens as ordered. - Post-thoracentesis nursing care includes assessment for complications, including pneumothorax, pain, hypotension, and pulmonary edema. Dr. Sahar Hossni El-Shenawi- Assistant Professor Of Critical Care Nursing 5 Critical Care Nursing Theory Pleural effusion Positioning the patient for a thoracentesis. The nurse assists the patient to one of three positions and offers comfort and support throughout the procedure. (A) Sitting on the edge of the bed with head and arms on and over the bed table. (B) Straddling a chair with arms and head resting on the back of the chair. (C) Lying on unaffected side with the bed elevated 30-45 degrees. Nursing Diagnosis Ineffective Breathing Pattern related to collection of fluid in pleural space Nursing Interventions Maintaining Normal Breathing Pattern Institute treatments to resolve the underlying cause as ordered. Assist with thoracentesis if indicated. Maintain chest drainage as needed. Provide care after pleurodesis. o Monitor for excessive pain from the sclerosing agent, which may cause hypoventilation. o Administer prescribed analgesic. o Assist patient undergoing instillation of intrapleural lidocaine if pain relief is not forthcoming. o Administer oxygen as indicated by dyspnea and hypoxemia. o Observe patient's breathing pattern, oxygen saturation, and other vital signs, for evidence of improvement or deterioration. Dr. Sahar Hossni El-Shenawi- Assistant Professor Of Critical Care Nursing 6 Critical Care Nursing Theory Pleural effusion Patient Education and Health Maintenance Instruct patient to seek early intervention for unusual shortness of breath, especially if he has underlying chronic lung disease. Evaluation: Expected Outcomes Reports absence of shortness of breath Dr. Sahar Hossni El-Shenawi- Assistant Professor Of Critical Care Nursing 7