Blood Products - Clinical Departments
advertisement

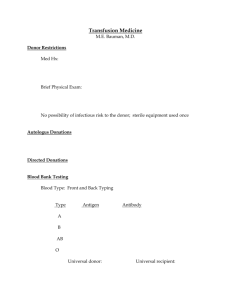
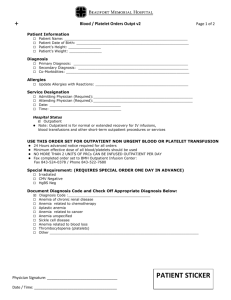
Blood Products: *All blood products containing erythrocytes are stored at 4degrees Celsius using a liquid anticoagulant preservative CPDCirtate binds ionized calcium and acts as an anticoagulant (causes hypocalcemia with PRBC administration to patients) Phosphate helps retard the breakdown of 2,3-diphosphoglycerate (helps offload oxygen to tissues) Dextrose serves as a fuel source for the erythrocytes Packed Red Blood Cells: Hgb conc 23-27 g/ dL Hct conc 60-80% Leukocyte Poor PRBC’s Separated by centrifugation, filters, never completely gone Used when pt with hx febrile, nonhemolytic transfusion reactions (caused by antibodies in recipient to donor’s leucocytes) Washed PRBC’s Washed with isotonic saline to leukocytes and residual plasma (which prevents allergic reactions caused by prior sensitization to donor plasma proteins). Blood Filters Trap small clots and decomposed platelets and fibrin coated leukocytes. Change every four units). Adverse Effects of Erythrocyte Transfusions: Acute Hemolytic Reaction (1 per 35,000) Human error, Result of antibodies in recipient binding to ABO surface antigen on donor RBC. Lysis ensues, rapid SIRS with hypotension and multiorgan failure. Symptoms can appear with only 5 mL infusion. Include fever, dyspnea, chest pain, low back pain. Can have consumptive coagulopathy. What to do: 1. stop transfusion immediately 2. infuse colloids for vascular volume expansion, can use crystalloids 3. obtain patient blood sample, inspect for pink-red hue of hgb. 4. voided urine specimen test for blood 5. send blood sample and donor blood for direct coombs. A positive test confirms hemolytic transfusion reaction, may be a false negative if most of donor erythrocytes have already lysed. Febrile Nonhemolytic Reactions (1 per 200) Results from recipient antibodies to donor leukocytes. Produced in response to prior transfusions or prior pregnancies, so often seen in multiparous women. Transfusion may be completed before fever appears, 1-6 hours. (later than hemolytic fever). Fevers rarely are due to bacterial contamination because of refrigeration, yersinia enterocolitica is most often isolated if this is the case. ( those contaminated with this organism are fatal 60% of the time). Future transfusions for nonhemolytic febrile reactions will not cause fever in over 75% of cases. Allergic Reactions: The sensitization to plasma proteins from prior transfusions. Urticaria (1 per 100) Most common hypersensitivity reaction Can treat with benadryl , do not need to stop transfusion. Anaphylaxis (1 per 1,000) More severe hypersensitivity reactions with wheezing Treat by stopping transfusion and treating anaphylaxis. Anaphylactic shock (1 per 50,000) IgA deficiency patients are more prone to allergic reactions and do not require prior exposure. (Those who develop anaphylaxis should be tested for underlying IgA deficiency). Sudden wheezing, hypotension are signs, duh, I know. Acute Lung Injury (1 per 5,000) Transfusion related acute lung injury (TRALI), is an inflammatory lung injury first apparent during or within 6 hours after start of transfusion. Donor antileukocyte antibodies bind to recipient granulocytes and sequester these donor leukocytes in patient’s pulmonary microcirculation. Promoting a granulocyte mediated acute lung injury manifesting like ARDS. Fatal in less than 10%, but is considered the leading cause of death from blood transfusions. Signs of TRALI dyspnea, hypoxemia develop during or within a few hours after transfusion begins. Fever common, hypotension less common. CXR eventually shows diffuse pulmonary infiltrates and intubation with mechanical ventilation usually necessary. The process usually resolves within one week. * Of note* RBC transfusions are a viscous lead, not a fluid load. Meaning they can not produce a hydrostatic pulmonary edema ( RBC’s can’t get out of the capillaries!) *Therefore what appears to be pulmonary edema shortly after a blood transfusion is ARDS. Transfusion Associated Immunomodulation Patients who receive blood transfusions have an increased incidence of nosocomial infections. This combined with the observation that blood transfusions improve survival of renal allografts has led to the proposal that blood transfusions promote immunosuppression in the recipient. Mechanism unknown. Platelets Each platelet concentrate should raise platelet count by 5,000 microliters They are usually given in multiples of 4 to 6 platelet concentrates. They can cause fever because they contain leukocytes from random donors. They can be stored up to 7 days but function declines after 3 days. After administration, function should last 8 days. How do they work? They form thrombosis. Function when vascular endothelium is damaged, platelets adhere to exposed collagen in the subendothelium. The platelets then release calcium, and this activates glycoprotein (IIb-IIIa) receptors on the platelet surface. These receprots bind irreversibly to von Willebrand factor in the surrounding endothelium, and this anchors the developing platelet plug. Glygoprotein receptors also bind fibrinogen, and fibrinogen bridges betweek platelets and result in platelet aggregation. Life cycle 10 days. Are cytoplasmic remnants of megakaryocytes without a nucleus. Platelet Disorders, Two categories: 1. Thrombocytopenia- abnormal numbers of functioning platelets. Count below 150,000 microliters. Counts below 100,000 to 5,000 can be tolerated if no structural lesion. 2. abnormal platelet adhering function. For example, uremia, due to impaired fibrinogen binding to platelets and abnormalities in von willebrand’s factor. Heparin Induced Thrombocytopenia HIT Heparin can combine to a heparin-binding protein (platelet factor 4, or PF4) on platelets to form an antigenic complex that induces the formation of IgG antibodies. These antibodies bind to platelets and form cross bridges that result in platelet aggregation. This can lead to a consumptive thrombocytopenia and clinically apparent thrombosis. Clinical Features; 1. 50% or greater reduction in platelet count that starts 5-10 days after first exposure to heparin. (IV heparin HIT can present as tachypnea, fever, chills, tachycardia, SOB). 2. The major complication of HIT is thrombosis, NOT bleeding. 75% of cases of HIT are accompanied by some type of thrombosis. 3. Greater chance with unfractionated heparin (1% medical patients) than LMWH. 4. can occur with very low doses of heparin such as heparin coated catheters. 5. SRA or serotonin release assay is an antibody assay that measures the release of C 14 labeled serotonin from platelets that are added to a sample of the patient’s serum. Can have false negative SRA, must use clinical scenario. The ICU Book, 3rd Edition, Paul L. Marino