Chemo System Case - Martin L. Puterman
advertisement

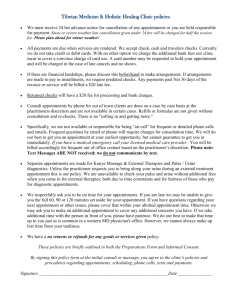
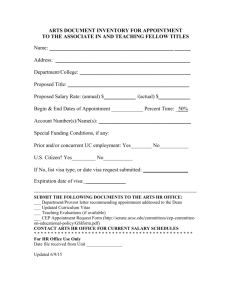
BC CANCER AGENCY’S CHEMOTHERAPY SCHEDULING CHALLENGES This case was prepared by Ruben Aristizabal, Pablo Santibañez, and Martin Puterman, members of the CIHR Team in Operations Research for Improved Cancer Care, for educational purposes. Version 2 October 28, 2011. BACKGROUND Cancer accounts for approximately 30% of deaths in Canada and is the most common cause of death. The Canadian Cancer Society estimates that there were 175,000 new cancer cases and 76,000 cancer-related deaths in 2010. Cancer is treated by surgery, radiation therapy and chemotherapy alone or in combination. Chemotherapy involves the oral and/or intravenous (IV) delivery of drugs which use a range of mechanisms to kill cancer cells or slow down cancer cell growth. This treatment usually affects the whole body, so that healthy cells can also be damaged and the patient often suffers serious and painful adverse effects. The British Columbia Cancer Agency (BCCA) delivers cancer care to British Columbian and Yukon residents. It is responsible for the entire spectrum of cancer care including prevention, treatment and rehabilitation. The agency has five centres across the province: one on Vancouver Island, one in Kelowna and three in the greater Vancouver area. The Vancouver Cancer Center (VCC) is the largest. The VCC Ambulatory Chemotherapy Care Unit (ACCU), which is often referred to as the “chemo unit” provides more than 14,000 appointments to over 2,000 patients each year. The ACCU, located on the 6th floor of the VCC, contains 9 treatment rooms and 33 treatment chairs. Each room is supervised by a nurse who administers chemotherapy to approximately seven patients each day. During the course of the treatment there is considerable interaction between the patient and nurse. Each patient’s chemotherapy treatment follows one or more of 200 different protocols. These protocols provide specific guidelines including treatment drugs, drug delivery instructions, frequency of appointments, estimated nursing time and appointment date flexibility (plus or minus 2 days at most). Typically, each protocol involves a series of chemotherapy appointments that are given on a weekly or monthly basis. Some protocols require treatment on consecutive days. In addition to the large number of treatments, another level of complexity in planning ACCU operations is the need to coordinate appointment schedules with other departments including the laboratory, the pharmacy, the radiation therapy units and the Ambulatory Care Unit (ACU). The ACU is the main point of contact between patients and their oncologists. After an initial consult when a protocol and chemo start date is determined, the patient visits his or her oncologist the day before each subsequent appointment to identify any complications that may require cancellation or modification of treatment. Also the ACU clerical unit is responsible for the first phase (see below) of booking a chemotherapy appointment. The ACCU scheduling process seeks to provide patients with timely and reliable notification of their appointments so as to eliminate any additional stress for the patient and their family. In fact a recent study showed that patient satisfaction was highly correlated 1 with appointment notification lead time. Of late, this complex task had become more arduous and lead times for patient notification have been decreasing. In the context of the patient focus of the BCCA, this problem has come to the attention of management on several occasions. Further, with a projected increase in case volumes, the time was ripe for a review of the scheduling process. AN EARLY MORNING HEADACHE On Monday morning, Sarah Rutherford, the ACCU manager, arrived at work and found a high priority e-mail in her inbox from the director of the Patient and Family Counseling Unit. The essence of the email was that the Counseling Department had received several recent inquiries from patients who had not been given appointment times for their upcoming chemotherapy appointments. As a result, patients and their families were finding it increasingly difficult to plan for their chemotherapy appointment and also being sure that the appointment date and time would not change at the last minute. This was especially problematic when there was transportation, shelter, child-care or family support arrangements involved. In response to this, Sarah mumbled to herself, “There must be a better way to schedule our patients. Having cancer is stressful and most certainly, our scheduling approach must not heighten this stress.” Sarah walked across the hall to chat with Anna Chu, one of three clerks responsible for preparing the daily ACCU schedule. Clearly there was not time for idle chat; Anna appeared to be under a lot of stress this morning. Anna was preparing the schedule for the upcoming Wednesday. The unit was staffed to treat 58 patients but there were already 50 patients pre-booked and 38 additional patients on the waiting list for Wednesday. There were 88 patients expecting treatment two days from now, roughly 30 more than the unit can handle. Some of these appointments would have to be changed. Additionally after developing the schedule, Anna and the other clerks would phone the patients and let them know Wednesday’s appointment times or if they had been waitlisted. While looking over Anna’s shoulder at the list of patients, Sarah thought to herself: “There must be better way to schedule patients to reduce these headaches for all involved.” Sarah could not keep this thought out of her mind. The current scheduling practices were not providing timely service and stressing out patients and staff. Sarah was determined to find a way to improve this situation. After returning to her office, Sarah decided to contact, Rick Sanchez, a BCCA operations consultant, who has played a major role in introducing some operational improvements in the radiotherapy unit. Rick was a charismatic individual with a business and engineering background who she had met a few times in the past. They set a meeting for Wednesday 8:00 am. WEDNESDAY’S MEETING “I need to understand the current situation before suggesting changes. Please walk me through the process before I spend some time on the unit seeing how things work.” Rick said. “The sooner the better”, Sarah replied as she closed her door. 2 As manager of the Chemotherapy Unit for more than fifteen years Sarah knew very well the steps that it takes to assign a chemo patient an appointment date and time: “Once a patient has been diagnosed with cancer, a patient is assigned an oncologist who after an initial consult develops a treatment plan based on the location of the tumour, the stage (severity) of the disease at diagnosis, and the patient’s general health. If the patient requires chemotherapy, the oncologist writes an order specifying the protocol to use and the date when the patient should start treatment. This may be as soon or possible, or several days or weeks in the future depending on the severity of the cancer and other recommended treatments. Orders for other exams and diagnostic tests are specified at this time as well. These orders are sent to a booking clerk in the ACU who schedules the appointment or appointments. To book a chemo appointment, the clerk needs to follow the protocol specific booking guidelines. For each protocol, the booking guidelines specify how much nursing and chair time are required to administer chemotherapy and any other time restrictions that need to be taken into account. The VCC chemo appointment scheduling system, which I and a colleague developed several years ago, classified appointment slots on the basis of our best assessment of how much nursing time was required to administer each treatment. We found that most appointments required 30, 45, 60, 90 or 120 minutes of nursing time. For example, the BRAJDAC protocol in which two different drugs are administered requires 45 minutes of nursing time, two hours of chair time, and must start before 14:30. In the past we have come to refer to these time slots as “CH Blocks” because that is how they are designated in our scheduling system (Figure 1). But it is important to emphasize that while an appointment may require 45 minutes of nursing time, the patient may occupy a chair for several hours while receiving his or her IV drug. ” Sarah stopped for a second to be sure Rick was following her. “Do you have any questions so far”? She asked. “Is there anything else I need to know about these appointment blocks?” Rick says while taking notes on his laptop. “Come to think of it, I could tell you a bit more about the appointment slots. We developed the idea several years ago when trying to produce a good schedule. It gave us some way to distinguish between appointments and account for the different needs for nursing time which is our tightest resource. I think it worked in the past but is not helping us now and may be the source of our problems. But appointments are very different. New patient appointments require about twice as much nurse interaction as subsequent appointments so we usually allocate CH90 or CH120 blocks for them. Also there are clinical trial appointments which have their own designation. We usually reserve a whole nurse/day for clinical trials but often we don’t need all of this time and are able to use it for last minute adjustments to slot in patients from the wait list.” Rick asked Sarah to provide him with further information about the scheduling process. “After the ACU clerk determines the type of slot required (CH30-CH180), she checks the VCC booking system to see if there is an available appointment on the specified date. Chemotherapy unit capacity varies by day of the week. For example, the capacity on Mondays is 2370 minutes of nursing time divided into thirteen 30-min slots; eighteen 45-min slots; eleven 60-min slots; three 90-min slots; and two 120-min slots. Each of these slots is scheduled at a pre-defined time during the day (see figure 1). For example to book a 3 BRAJDAC appointment, the booking clerk would check the Chemotherapy unit capacity on the targeted appointment date and look for a 45-min slot available before 14:30. If she can find such a slot, she books the appointment and mails an appointment card specifying the appointment date and time appointment to the patient. If she cannot find the type of slot needed (i.e. all suitable slots are already taken) the patient is placed in the waitlist and the appointment card is sent out indicating that the patient has been waitlisted for that day. Once the appointment card is sent to the patient the ACU clerk is no longer involved in managing this appointment. The scene now shifts to the ACCU. Two days before the appointment date, a clerk in the ACCU combines the list of pre-booked patients and the list of waitlisted patients to create the daily schedule. This involves four main steps: 1) Triage: The ACCU clerk and I review the list of pre-booked and waitlisted patients for the date we’re working on. We note the protocol and combine this with our personal knowledge of the patient to decide which patients absolutely need to be treated on this date. We call this the A list. We then prioritize the remaining appointments to the B list. 2) Reassignment: We assign appointment times to A list patients and try to fit in as many B list patients as possible. We move the remaining B list appointments to other dates based on the priorities we set in the triage step and the appointment date flexibility; 3) Nurse assignment: We then use the schedule template to assign specific nurses to shifts (columns in Figure 2); 4) Inform the patient: The clerk then calls patients who have their appointment changed or those on the wait list to inform them of their new appointment times. Even though the nurses’ schedules are meant to serve as a guideline and ensure an even workload distribution, we usually need to modify them in order to accommodate all the patients requiring treatment. At this point, accounting for all the appointment restrictions (conflicting appointments, nursing workload distribution, patient time needs/preferences and other departments’ workload and capacity) becomes a challenging task. Often we spend considerable time and energy trying to resolve these conflicts. Usually we produce a schedule but with a lot of stress and anxiety on our part.” Having finished her description, Sarah took a deep breath. Rick continued taking notes for a few more minutes and then said to Sarah, “This was very clear. I think I have a good understanding of how your system works. I will talk to the clerks and observe what is happening for a day or two and then develop a process map. I will share it with you to be sure that we’re on the same page before we start to look for process improvements”. The assignment: 1. Develop a process map for the chemo appointment scheduling process. shortcomings do you see? 2. What improvements would you recommend? Why? 3. How would you know if your proposed changes made a difference? What 4 Figure 1 - List of slots available on Mondays 5 Figure 2 - Pre-defined nursing schedule form 6