Service Specification and Admission Criteria
advertisement
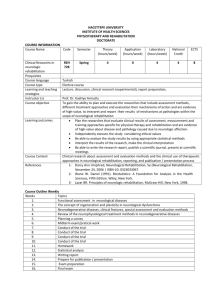
Service Specification and Admission Criteria Name of unit Location (Tel) Main groups treated Primary service description Inclusion criteria Exclusion criteria Main services offered Frank Cooksey Rehabilitation Unit, King’s College Hospital NHS Foundation Trust 4th Floor Riverside Building, Lewisham Hospital NHS Trust, Lewisham High Street, London SE13 6LH Tel: 0208 333 3365; Fax: 0208 333 3027 Patients who have reached their sixteenth birthday, who are recovering from: Acquired brain injury of any cause. Incomplete cervical spinal cord lesions, and incomplete or complete thoracic or lumber spinal cord lesions (of any cause), if a referral to a Regional Spinal Cord Injuries Centre (RSCIC) has been made but access is delayed, or if they have been declined. Peripheral neuromuscular disease e.g. Guillain Barré syndrome, critical illness neuropathy, polymyositis. Complex musculoskeletal injury and associated physical rehabilitation needs Neurological injury and amputation (Upper or lower limb) Post-acute intensive specialist in-patient neurological and complex rehabilitation for patients recovering from acquired disability. People with complex neurological disability (i.e. physical disability, often with cognitive and/or communication problems), who require more than one intensive therapy discipline (OT, PT, SLT) and/or psychology. These patients’ needs are such that they require an inpatient stay in a specialised unit to optimise their recovery. A capacity assessment must have been completed where indicated. Patients who require a short intensive and specialist physical rehabilitation, in the absence of a primarily neurological injury or illness Patients coming to the unit from home for intensive specialist physical rehabilitation following change of weight bearing status e.g. touch/ partial /full. Patients with the following; vac dressings/ pumps, ng tube, colostomy bags, peg feeding, external fixators on limbs, and spinal braces. The unit does not accept patients with the following problems, which are usually best managed in other centres (as indicated in brackets below): Patients who are ineligible to receive NHS-funded rehabilitation care Patients for whom no discharge destination has been agreed Persistent Vegetative States and Minimally Responsive States (RHND Putney) Patients with severe cognitive and behavioural problems without physical disability (Lishman Unit, BBIRU, Blackheath BIU) Severe behavioural problems which could not be managed in this environment e.g. requiring the need of 1:1 care (the Kemsley Unit, RHND Putney) Patients treated under the Mental Healthcare Act (BBIRU) Patients who are not medically stable Patients requiring ongoing respiratory monitoring, invasive or non-invasive respiratory support, or tracheostomy care Patients who do not to consent to a referral being to FCRU Patients who cannot commit to abstain from self-injurious behaviours for the duration of their inpatient rehabilitation stay e.g. substance and alcohol misuse Referring Trauma Consultant (e.g. Orthopaedic surgeon, plastic surgeon) declines to make a commitment to continue to provide care and ongoing management prior to acceptance or admission. Smoking is not permitted on the unit and patients who cannot commit to restrain themselves from smoking may find it difficult to adapt to the environment1 Inter-disciplinary rehabilitation programme including: Post acute rehabilitation for people recovering from acute insult or injury, to help them make the 1 FCRU is a non smoking unit. University Hospital Lewisham is a non-smoking site. FCRU staff may schedule time off the unit for patients wishing to smoke outside away from hospital grounds, no more than twice a day, if portering staff are available. Capacity Mean in-pt LOS Features of the service in relation to service specification standards Waiting time for admission Main outcome measures recorded Other reported outcomes Audit and Clinical governance transition from hospital back to home/community (LOS usually 1-3 months). Team comprises of Consultants in Rehabilitation Medicine, Consultant therapist in neuro-rehabilitation, nursing, physiotherapy, occupational therapy, speech and language therapy, psychology, and administrative staff Liaison with Younger Physical Disability services, and other community-based health services such as Headway, intermediate and continuing care therapy teams and social care agencies Rehabilitation follow-up (in a Rehabilitation Medicine clinic) and other medical and/or surgical follow-up as required. Total 15 beds : 2 x4-bed, 7 single rooms Usually 1-3 months, typically 8 weeks Inter-disciplinary programme with agreed short- and long-term goals, (which are patientdetermined, wherever possible) Goal-setting begins within two weeks of admission, and goals are reviewed at two week intervals Access to early prosthetic/ walking aid equipment e.g. PPAM aid, parallel bars Access to prosthetic services via clinic. Hydrotherapy for complex physical and neurological injuries. Discharge planning starts from point of admission, involving social services, PCTs, housing and relevant community rehabilitation and care teams, voluntary services etc. Preparation for discharge may include graded exposure to the community, for example weekend leave. Family and carer support offered as an integral part of the programme A key-worker is allocated to each patient to act as a case co-ordinator. Specialist equipment funding requirements are addressed, and negotiated with the patient’s local PCT or social services as necessary A family conference is held approximately 2-3 weeks into admission to discuss likely outcomes, discharge destination etc. Written information is provided to patient and family before and during stay A discharge summary and care plan are given to patient and family Assessment within two weeks of receipt of completed referral Admission typically 2-4 weeks from acceptance by the multidisciplinary FCRU team UK FIM+FAM (Functional Independence measure and Functional Assessment Measure) Other function- and impairment-based measures as appropriate (eg American Spinal Injuries Association , “ASIA”, for SCI) Rehabilitation Complexity Scale UK-ROC Discharge destination (against predicted discharge destination) Length of Stay Patient/family feedback questionnaire Adverse incidents and ‘near miss’ register Record of plaudits and complaints. All staff participate in yearly appraisal and objective-setting/ monitoring Multi-professional 360 Degree appraisal included every 2-3 years for medical staff Rolling audit of outcomes and patient feedback. Updated 26/04/2013, FCRU Team