Abdominal Assessment - My Illinois State
advertisement

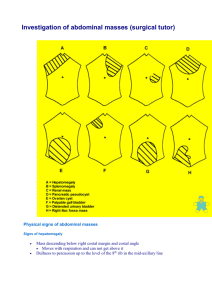
Abdominal assessment 1 MENNONITE COLLEGE OF NURSING AT ILLINOIS STATE UNIVERSITY NUR 431 Diagnostic Reasoning for Advanced Nursing Practice Abdominal Assessment Abdominal complaints are a frequent chief complaint of patients evaluated by NPs. Remember... • • Be consistent with technique Thorough history & physical examination (see lab module) may avoid unnecessary diagnostic tests. Abdomen: General Overview • Gastrointestinal System – Stomach – Small intestine – Liver – Gall bladder – Pancreas – Large intestine – Appendix • Urinary System – Kidneys – Ureters – Bladder – Urethra • Reproductive System – Prostate – Uterus – Ovaries – Fallopian tubes – Cervix • Other – Aorta/Vasculature – Spleen Types of Abdominal Pain • Obstruction • Peritoneal irritation • Vascular disorders • Mucosal ulceration or irritation • Altered bowel motility • Capsular expansion • Metabolic disturbances • Nerve injury Abdominal assessment 2 • • • Muscle wall diseases Referred pain Psychopathology Abdominal Pain: Differential Diagnosis • Appendicitis • Cholecystitis • Pancreatitis • Perforated ulcer • Diverticulitis • Intestinal obstruction • Volvulus • Leaking abdominal aneurysm • Biliary stones, colic • Salpingitis • Ectopic pregnancy – LMP? • Pelvic inflammatory disease (PID) • Ruptured ovarian cyst Common Symptoms of Abdominal Disease: Pain • • Origin of abdominal pain – pain due to tension – pain due to ischemia – pain due to peritoneal irritation Onset Onset of Pain: Immediate Onset • Perforated ulcer • Cholecystitis • Pancreatitis • Mesenteric infarction • Intestinal obstruction • Ruptured aneurysm • Ureteral stone • Diverticulitis • Perforated colon • Appendicitis • Incarcerated hernia • Ruptured ectopic pregnancy Onset of Pain: Gradual Onset • Urinary tract infection Abdominal assessment 3 • • • Appendicitis Low mechanical obstruction Hernia Abdominal Disease: Nature of the Pain • • • • • • Burning (peptic ulcer) Cramping (biliary colic, gastroenteritis) Aching (appendiceal irritation) Knife-like (pancreatitis) Gradual onset (infection) Sudden onset (duodenal ulcer, acute pancreatitis, obstruction, perforation) Common Symptoms of Abdominal Disease: Pain • • Location (referred pain) Associated symptoms – Observation of the patient – Presence of vomiting – Signs of impending vascular collapse – Pelvic and/or rectal exam Other Common Symptoms of Abdominal Disease • • • • • • • • Nausea/vomiting Changes in bowel movements Rectal bleeding Jaundice Abdominal distention Mass Pruritis (elevated bilirubin?) Fever Other History Components • • • Past medical history – If surgical history, think adhesions – Check meds/OTC (NSAIDS - epigastric pain) Family history Psychosocial history – money – support systems – alcohol/caffeine intake Review of Systems Abdominal assessment 4 • Don’t forget….Date of LMP (include with ALL females of childbearing age) Objective Assessment of the Client: Examination Components • • • • • • Complete set of vital signs (including wt.) 1st Inspection 2nd Auscultation 3rd Percussion 4th Palpation – light (“scouting mission”) – then deep Note: Stay on right side of patient, comfort/relaxation measures important Inspection • • • Landmarks Skin – Scars – Striae (purple with Cushing’s) Size/shape of abdomen (flat) – If not flat, then one of the “Seven F’s” is the cause The 7 F’s • • • • • • • Fat Fibroids Flatus Fluid Fetus Feces Fatal (tumors) Inspection • • • • Symmetry – masses – scoliosis Check for masses, pulsations, musculature, hernias Engorged vessels Visible peristalsis Auscultation • Where? – 4 quadrants and epigastric Abdominal assessment 5 • • • Bowel sounds – Normal (5-34X/minute) – Hyperactive – Borborygmi – Sluggish – Absent Bruits – abdominal aorta – renal arteries – iliac arteries – femoral arteries Friction rubs – with liver tumor, enlargement Percussion • • Why and where? Percussion sounds – Tympanic (gastric air bubble, gas in bowels) – Hyperresonant (base of left lung) – Resonant (normal lung) – Dull (liver, spleen) – Flat (thigh) Palpation • • • • Warm hands appreciated! Watch the patient’s face for signs of pain or discomfort. Think of the underlying organs. Light Deep – tenderness, voluntary guarding, rigidity – rebound – liver, spleen, kidneys, aorta, hernia Special Tests • • • Iliopsoas test – Pain elicited when supine patient attempts to flex thigh against resistance of examiner’s hand Obturator test – Supine patient, flex thigh to 60 degrees – Pain on internal rotation indicates inflamed obturator internus muscle due to perforated intrapelvic appendix Others; Murphy’s sign (GB) and Rovsing’s sign (appendix) Other Examination Considerations Abdominal assessment 6 • • • Rectal exam – every year after age 50 with 10-year life expectancy (ACS; USPSTF-insufficient evidence) – fecal occult blood - yearly after age 50 (ACS); discontinue at 76+ if no indications and 85+ regardless (USPSTF) – sigmoidoscopy - every 5 years after 50 (ACS); discontinue as above (USPSTF) – colonoscopy – every 10 years after age 50 (ACS); discontinue as above (USPSTF) – with poorly differentiated abdominal pain, may find retrocecal appendix Pelvic exam - with pain below the umbilicus (STD, PID) Prostate exam Labs • • • • • Urinalysis Urine HCG CBC Chemistries Amylase Radiographs (x-rays) • • Flat plate Upright chest x-ray How does the NP sort out all of this stuff? If not normal, then... • • Acute Etiologies – Surgically emergent • appendicitis • ectopic pregnancy • intestinal obstruction • acute cholecystitis – Medically emergent • acute pancreatitis – Self-limiting (gastroenteritis) Chronic etiologies – Cancer of stomach or pancreas – Irritable bowel syndrome – Hepatitis – What to keep and what to REFER? • Refer anything not sure of