THE KINGSTON HOSPITAL
advertisement

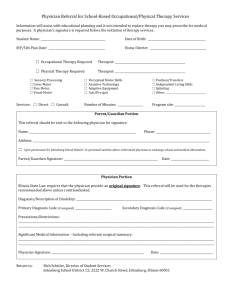
RECORD OF PHYSICAL EXAMINATION NAME: ___________________________________________________________________________++++___________ ADDRESS: _______________________________________________________________________________________ Height __________________Weight _____________Blood Pressure __________________ Pulse______________ Are there any signs of illness/abnormalities of the following: (If “yes” please provide description in space provided) Skin ___NO ___Yes ___________________________________ Lungs ___NO ___Yes ___________________________________ Heart ___NO ___Yes ___________________________________ Ears/Nose/Throat ___NO ___Yes ___________________________________ Abdomen ___NO ___Yes ___________________________________ Lymph Nodes ___NO ___Yes ___________________________________ Extremities ___NO ___Yes ___________________________________ Neurological System ___NO ___Yes ___________________________________ Is there are pertinent history or condition that is being treated: ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ ________________________________________________________________________________________ Examining Physician _________________________________________Phone: _____________________ PLEASE PRINT Examining Physician’s Signature ________________________________________________Date: ______________ ANNUAL TB SCREENING TEST FORM Name: REQUIRED: ANNUAL PPD – MANTOUX TEST This test can be done at the Employee Health Office of HealthAlliance Hospital: Broadway Campus. Please call 334-2769 for hours. If you have had the test elsewhere, you must submit a certified copy of your test results to the Medical Staff Office of HealthAlliance Hospital: Broadway Campus. The test must be certified by a NYS Licensed Practitioner OTHER THAN THE APPLICANT/MEMBER. Date Administered: Injection Site: Brand and Lot Number: Date Read: Results: Certified by: Signature: PLEASE PRINT NAME BE CERTAIN TO HAVE TEST READ WITHIN 48 HOURS Chest X-ray indicated? Yes No If indicated, test date: (Attach copy of report) TB POSITIVE OR BCG VACCINATION NOTE: If it has been longer than 10 years since you received the BCG vaccine, you must be retested. Please submit the results along with this application. If you are TB Positive, please complete this questionnaire. Please check any of the following symptoms that you may be experiencing: ______ Loss of appetite ______ Fatigue ______ Fever ______ Weight loss ______ Chronic cough ______ Blood tinged sputum ______ None of the above ______Night sweats Signature: _________________________________________________________________ Print Name: ___________________________________________________ PHYSICAL AND MENTAL CAPACITY STATEMENT TO: Credentials Committee In my observations of ________________________________I have not received credible information nor have I seen evidence of impairment of physical or emotional health, including habituation or addiction to any substance that could interfere with the performance of the privileges requested. DO NOT SIGN THIS FORM It must be signed by your Personal Physician or another physician who can attest to your physical and mental capacity. Physician (Print name) Physician signature Phone: ____________________________ Date NOTE: Initial applicants may have their health status confirmed by the director of a training program, the chief of services, or chief of staff at another hospital at which the applicant holds privileges, or a currently licensed physician.. PERSONAL INITIAL HEALTH ASSESSMENT Name Answer all of the following questions. If your response to any question is “yes,” please provide a written explanation on a separate sheet. 1. Present health status: Good Fair Poor (if fair or poor, please state reasons on a separate sheet) 2. Have you consulted a physician or sought medical treatment for any reason in the last year? Yes_____ No _____ 3. Have you been hospitalized for any reason in the last year? Yes_____ No _____ 4. Have you been habituated to drugs or alcohol in the last year? Yes_____ No _____ 5. Have you been denied or have you had any limitations on your health, life, or disability insurance in the last year? Yes_____ No _____ Are you currently taking any medication that may affect your clinical judgment or motor skills? Yes_____ No _____ 7. Are you currently under any limitations in terms of activity or work load? Yes_____ No _____ 8. Are you currently under the care of a physician? Yes_____ No _____ 6. 10. Rubella (German Measles): Titre: Date done: Results: Submit serologic proof (copy of lab slip) Negative titre requires immunization consistent with good medical practice. 11. Rubeola (Measles): Only required for those born on or after 01/01/1957 12. Hepatitis B Vaccine: Date: _________________ 12. Varicella (Chicken Pox): Titre: Date done: _________________ Results: _____________________ Show proof of: TWO measles or MMR vaccinations given after 1st birthday and at least one month apart; OR Physician-diagnosed disease; OR Serologic proof of immunity (attach copy of lab slip) Immunization dates: #1 Disease Date: APPLICANT’S SIGNATURE: #2 Titre Date: DATE: