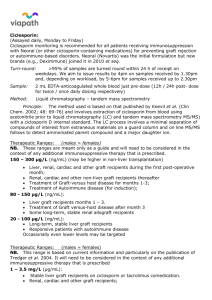
Ciclosporin
advertisement

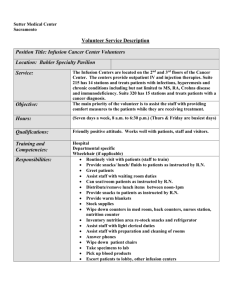
Dr A. G. Lim, Updated 2004-06-13 Epsom & St Helier’s University Healthcare Trust Guidelines for Ciclosporin in Severe Ulcerative Colitis (Dr A. G. Lim, Consultant Gastroenterology) Contents 1. Protocol for ciclosporin in severe ulcerative colitis 2. Background 3. Truelove and Witt criteria 4. Informed consent 5. Baseline studies 6. Contraindications 7. Drug interactions 8. Anaphylaxis 9. Patient monitoring 10. Clinical activity index 11. Drug monitoring 12. Side effects 13. Switching to oral ciclosporin 14. Concurrent treatment 15. Outpatient monitoring References Appendices i. Patient Information Leaflet ii. Nurse’s Guide for Ciclosporin Infusion iii. Checklist for during Inpatient Ciclosporin infusion 1 Dr A. G. Lim, Updated 2004-06-13 1. Protocol for Ciclosporin in severe Ulcerative Colitis (UC) refractory to Corticosteroid and opposed to surgery Confirmed diagnosis of UC 3 or more Truelove & Witt criteria No response to IV Methyprednisolone after 5 – 7 days Initiating ciclosporin use Informed consent Baseline studies Check for contraindications Check for drug interactions Ciclosporin therapy as continuous infusion Dose = 2 mg/kg/day. [Extra caution with elderly or patient with mild impaired creatinine clearance] Monitor of signs of allergy or anaphylaxis every 15 minutes in the first hour Discontinue and treat if signs of allergy develop If tolerating ciclosporin, continue infusion for 7 days Strict patient and drug monitoring Treatment failure Refer for surgery Contact Stoma Nurse Treatment success Switch to oral ciclosporin Outpatient monitoring Wean off ciclosporin Concurrent Treatment Continue with IV Steroid, switch to oral if ciclosporin treatment successful If on Azathioprine or 6-mercaptopurine, to stop and restart 2-3 months in outpatient if ciclosporin treatment successful Maintain aminosalicylates but not added to regime 2 Dr A. G. Lim, Updated 2004-06-13 2. Background Standard treatment of severe exacerbation of ulcerative colitis (UC) consists of high dose intravenous corticosteroid and aminosalicylates (5-ASA) compounds. Azathioprine is of limited use in the acute setting because of its slow onset of action. Approximately 15% of patients with acute UC will require hospital admissions for control of symptoms and up to 40% of these patients will need colectomy. Ciclosporin is a potent inhibitor of cell-mediated immunity. It acts mainly by reversibly inhibiting T-lymphocyte function by inhibiting interleukin-2 production. It does not interfere with stem cell activity. Ciclosporin is extracted from the fungus Tolypocladium inflatum There is evidence from controlled and uncontrolled studies that ciclosporin is efficacious for UC. In a multicentre, double-blind, placebo-controlled trial of intravenous and oral ciclosporin for the treatment of severe, steroid refractory UC, achieving success in 80% of patients in the short term and maintaining success in about two thirds of patients in the longer term. The short term outcome of ciclosporin with a mean follow up period of 39 months was 91%. More than half were found to avoid colectomy in the longer term. Based on current evidence, ciclosporin appears to be a viable alternative to emergency colectomy in severe UC in the short term. 3 Dr A. G. Lim, Updated 2004-06-13 3. Truelove and Witt criteria Passage of 6 or more stools per day Temperature of > 37 degrees centigrade Pulse rate > 90 bpm Anaemia < 75% of normal HB ESR > 30mm/hr after failing to respond to 5 – 10 days of IV Steroid 4. Informed consent Inform patient that this treatment is unlicensed for inflammatory bowel disease. It is offered as an alternative to surgery Patients are also informed of the risks and benefits of colectomy by surgical colleagues 5. Basline studies History: Detailed drug history Seizure history Cancer history Menstrual history Compliance Physical examination Blood pressure Infection Abdominal examination Laboratory data FBC U&E plus creatinine creatinine is borderline clearance if serum difficile toxin, Magnesium Cholesterol ESR/CRP Pregnancy test Stool- MC&S, Clostridium parasites and ova AXR 4 Dr A. G. Lim, Updated 2004-06-13 6. Contraindications Septicaemia Bowel perforation Megacolon Positive stool to MC&S/ Chlostridium difficile toxin/ parasites/ova Uncontrolled hypertension Creatinine > 33% above upper normal limit Elevated LFT (>3times normal) Uncorrected hypomagnesiumia (associated with an increased risk of seizures) Serum cholesterol <3.1 mmol/l (associated with an increased risk of seizures) Pregnancy / breast feeding Maglinancy of any kind Known hypersensitivity to ciclosporin / polyethoxylated castor oils (in injection) 7. Drug interactions Drugs that increase ciclosporin levels Diltiazem Nicardipine Verapamil Bromocriptine Metoclopramide Danazol Ketoconazole Fluconazole Itraconazole Erythromycin Methylprednisolone Oral Contraceptives 5 Dr A. G. Lim, Updated 2004-06-13 Drugs that decrease ciclosporin levels Rifampicin Phenobarbital Phenytoin Carbamazipine Other interactions Grapefruit juice increases the blood levels of ciclosporin and increases the risk of toxicity. Should not be consumed less than one hour before or after and oral dose 8. Anaphylaxis Monitor every 15 minutes for the first hour Signs include hypotension, hives, wheezing, laryngeal spasm Immediate discontinuation if such signs develop Treat with chlorpheniramine/ adrenaline, as necessary, as with any allergic reaction The first infusion should not be started at night due to the risk of anaphylaxis 9. Patient monitoring – Joint management with surgeons Vital signs – pulse, blood pressure, temperature 4 times a day or more often if deterioration Daily physical examination for abdominal tenderness and distension Daily review for adverse effects Stool chart for bowel frequency, stool consistency, presence or absence of blood Blood tests – FBC, U&E, LFT, Mg, Cholesterol, ESR, CRP every 2nd day (daily if abnormal) Daily AXR if colonic atony or dilatation are detected; worrisome findings include small bowel ileus and a continuous column of colonic gas which may precede megacolon Objective measure of clinical activity score (see table 1) *Maximal score = 21 **Score of less than 10 on 2 consecutive days = indicate a clinical response 6 Dr A. G. Lim, Updated 2004-06-13 10. Table 1: Clinical activity index Symptom Diarrhoea (no of daily stools) 0-2 3 or 4 5 or 6 7-9 10 Nocturnal diarrhoea No Yes Visible blood in stools (% of movement) 0 <50 >50 100 Faecal incontinence No Yes Abdominal pain or cramping None Mild Moderate Severe General well-being Perfect Very good Good Average Poor Terrible Abdominal tenderness None Mild and localized Mild to moderate and diffuse Severe or rebound Need for antidiarrhoeal drugs No Yes Score 0 1 2 3 4 0 1 0 1 2 3 0 1 0 1 2 3 4 0 1 2 3 4 5 0 1 2 3 0 1 7 Dr A. G. Lim, Updated 2004-06-13 11. Drug monitoring and administration Continuous infusion at dose of 2 mg/kg/day over 24 hours [ Caution with elderly or in mild impaired creatinine clearance (ie 20-30% reduction of estimated creatinine clearance)] Drug only stable for 6 hours after mixing, therefore the infusion is split into 4x 6 hours infusion pump. E.g. 60kgs patient needs 120mg/24hours. Therefore, ciclosporin is delivered at 30mgs/48ml N/Saline: 8ml/hr Ciclosporin needs to be administered in the syringes and giving sets that do not come in PVC. Giving sets used for heparin/GTN are polyethylene based and can be used. Trough ciclosporin levels every 2 days To achieve levels of 300-400 ng/ml Dose of ciclosporin reduced if – levels >500 ng/ml for 2 consecutive days serum creatinine increases by 30% over baseline serum liver enzymes double diastolic blood pressure exceeds 90mmHg or systolic blood pressure exceeds 150 mmHg despite antihypertensive treatment Ciclosporin doses can be reduced by 25% at least Discuss ciclosporin monitoring with renal physicians (contact at Renal Unit, St Helier Hospital) 12. Side effects Seizures Hypertension – treat with calcium channel blocker but this can lead to a rise in ciclosporin level Renal toxicity Liver toxicity Hyperkalaemia Increased susceptibility to infection Hyperlipidaemia Anaphylaxis Irritation at cannula injection site – care of cannula site essential 8 Dr A. G. Lim, Updated 2004-06-13 Flushing Tremor Fatigue Headaches Gastrointestinal disturbances Paraethesia (burning sensation in hands and feet) Gingival hyperplasia (long term treatment only) Hypertricosis (long term treatment only) 13. Switching to oral ciclosporin If patient has demonstrated a decisive clinical improvement Intravenous ciclosporin is discontinued at 8pm on that evening Ciclosporin level is checked at 8am the following morning, immediately preceding the first oral dose Oral dose = 4-5 mg/kg/day ciclosporin (Neoral) given in 2 divided doses To achieve trough level of 150 – 300ng/ml 14. Concurrent treatment Tail-off IV steroid (IV methylprednisolone) 60mg/24hrs to zero during the 1st 3 days of ciclosporin use On switching to oral ciclosporin, IV steroid can be discontinued and switched to oral prednisolone 60mg. 5-ASA drug can be continued Consider Septrin during time when patient on both IV steroid and ciclosporin 9 Dr A. G. Lim, Updated 2004-06-13 15. Outpatient monitoring Clinic visit and review for adverse effects Weekly x 4 then, biweekly x 2 then, every 3-4 weeks Ciclosporin levels, FBC, ESR, CRP, U&E, LFT, Mg, Cholesterol With each visit as above and within 1 week after any dose change Hypomagnesium Often require parenteral supplementation as oral supplementation can exacerbate diarrhoea Prednisolone Reduce by 10mg each week until 30mg is reached and then by 5 mg weekly or every other week as tolerated At 15-20 mg of daily prednisolone, smaller reductions may be required Patients who cannot be maintained on 20mg of prednisolone daily are considered ciclosporin failure and should be referred for surgery All patients should be weaned off within 6 months of hospital discharge Ciclosporin Once weaned off prednisolone, ciclosporin dose is reduced by 50% for 2 weeks, followed by complete ciclosporin withdrawal Azathioprine or 6-mercaptopurine Initiate at about 2-3 months after discharge to allow onset of action before ciclosporin is stopped 5-ASA Maintenance dose Endoscopy Flexible sigmoidoscopy after 6-8 weeks Rx Colonoscopy at 4-6 months Pregnancy Ensure that contraception is used during the period of ciclosporin treatment. Safety of ciclosporin in human pregnancy has not been fully established Breastfeeding Ciclosporin passes into breast milk and mothers receiving treatment should not breast feed their infants 10 Dr A. G. Lim, Updated 2004-06-13 Appendix 1 CICLOSPORIN – in treatment for severe ulcerative colitis PATIENT INFORMATION LEAFLET Background Ciclosporin is an immune suppressing medication. It is used in patients with severe exacerbation of ulcerative colitis (UC), who have not responded to high dose intravenous steroids after 5-10 days. It is a relatively new in the treatment for UC. However, it has been used for many years in preventing organ transplant rejection. It has been shown that approximately 15% of patients with acute UC will require hospital admissions for control of symptoms and up to 40% of these patients will need surgery e.g. bowel resection. There is preliminary research evidence shown that ciclosporin is effective for treating severe UC. It has shown to achieve success in 80% - 91% of patients in the short term and maintaining success in about two thirds of patients in the longer term as in avoiding surgery. Based on current evidence, ciclosporin appears to be a viable alternative to emergency surgery in severe UC in the short term. How is Ciclosporin given? Ciclosporin is administered as a continuous infusion over 24hours via a pump. The medication dose is split into 4 infusion bags or syringes. Intravenous steroid is continued while you are having intravenous ciclosporin. The steroid infusion is gradually tailed off and eventually discontinued. You will be monitored closely when you are having the ciclosporin infusion. A nurse will be caring out observation on blood pressure and pulse and any sign of allergic reaction every 15 minutes during the first hour of the infusion. Observation on blood pressure, pulse and temperature is gradually decreased to 4 hourly. If you are already on Azathioprine or 6-mercaptopurine, this medication is stopped temporarily to avoid excessive suppression of immune system. 11 Dr A. G. Lim, Updated 2004-06-13 How long do I have the infusion? The ciclosporin infusion is administered for 5 – 10 days. If your condition improved after 5 – 10 days, then you will be prescribed oral ciclosporin twice daily. (Please note: Grapefruit juice interact with ciclosporin, so it should only be consumed less than one hour before and after an ORAL dose.) Azathioprine or 6-mercaptopurine may be restarted once you are on oral ciclosporin medication. What are the side effects? Ciclosporin is generally well tolerated. Side-effects from ciclosporin are: headaches, flushing, tremor, fatigue, gastrointestinal disturbances, burning sensation in hands and feet, seizures, kidney impairment, liver toxicity, susceptibility to infections, irritation to cannula’s site and anaphylaxis. Regular blood tests will be carried to monitor your kidney and liver function. Do I take ciclosporin for life? No. You will be slowly weaned off ciclosporin until complete withdrawal. You will be seen in the clinic weekly on the first month after you leave the hospital, then every 2 weeks for 4 weeks, then every 3 – 4 weeks. We will continue to monitor the ciclosporin level to prevent toxicity and your liver and kidney function closely. I hope this information has been helpful. Please do not hesitate to ask your doctor if you need more information. Dr A. G. Lim Consultant Gastroenterology Epsom and St Helier University Healthcare Trust 12 Dr A. G. Lim, Updated 2004-06-13 Appendix ii NURSE’S GUIDE FOR CICLOSPORIN INFUSION PRE INFUSION 1. Baseline vital sign of temperature, blood pressure and pulse HOW TO ADMINISTER 1. DO NOT start the first infusion at night due to risk of anaphylaxis 2. Use polyethylene based giving sets and NOT PVC e.g. use the giving sets that used for heparin/ GTN infusion 3. Administer infusion in N/Saline 4. Ciclosporin is given as continuous infusion. However, the infusion is only stable for 6 hrs, therefore infusion is split into 4 pumps/ 24 hours 5. For example: -> A 60kgs patient – needs 120mg/24hrs -> Dilute 30mgs Ciclosporin in 48mls N/Saline -> Run the pump rate at 8mls/hour (48mls in 6hrs) DURING INFUSION 1. Monitor BP & P every 15 minutes for the first hour. Then 30 minutes for 2 hours. Observations gradually decreased to 4 hourly or QDS daily 2. Observe for sign of anaphylactic shock – stop the infusion immediately and treat appropriately and inform doctor 3. Other side-effects - see Guidelines pg 8-9 4. Monitor temperature 4 hourly 5. Monitor stool chart – note frequency, stool consistency, presence or absence of blood 13 Dr A. G. Lim, Updated 2004-06-13 Appendix iii CHECKLIST FOR DURING INPATIENT CICLOSPORIN INFUSION See Protocol pre-infusion Daily review of adverse effects Daily physical examination Daily AXR Blood test : FBC, U&E, LFT, Mg, Cholesterol, ESR, CRP every 2nd day (daily if abnormal) Ciclosporin levels every 2 days (to achieve levels of 300 – 400ng/l) Alert EGH pathlab to send blood sample to St Helier (St Helier lab tel no for result: 721 2662/ 3421) Objective measure of clinical activity score (see table 1) Wean off IV methyprednisolone to zero during 1st 3 days of Ciclosporin Consider Septrin during time when patient is having both IV Steroids and Ciclosporin 14