Proposed Guidelines for the Research Use of Gadolinium at
advertisement

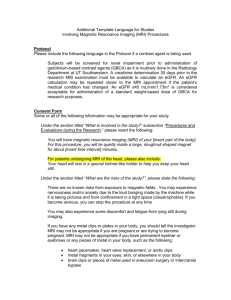
Proposed Guidelines for the Research Use of Gadolinium at Northwestern University. Darren Gitelman, MD On May 8th a meeting took place between Don Workman and several members of the CAMRI (Center for Advanced Magnetic Resonance Imaging) steering committee including James Carr, Darren Gitelman and Daniel Lee in order to develop consistent guidelines for the use of gadolinium based contrast agents (GBCA) in research studies at Northwestern University. Background Beginning in 1997 a series of cases, now up to several hundred, began to be identified of a condition termed nephrogenic systemic fibrosis (NSF) (originally nephrogenic fibrosing dermopathy). NSF is a systemic disorder associated with fibrosis of multiple organ systems and increased morbidity and mortality. It has been seen almost exclusively in patients with severe renal dysfunction (stage 4 and 5 chronic kidney disease (CKD)) and appears to be strongly associated with the administration of GBCAs [1]. The clinical presentation of NSF includes skin lesions with pruritis and pain over the affected areas. The skin lesions are described as indurated and hyperpigmented with a peau d’orange appearance. Swelling of the arms and legs has also been seen. In areas where the skin lesions extend across joints, they can lead to restriction of joint movements and contractions. In addition to skin involvement, the fibrotic process can affect other tissues including renal tubules, skeletal muscles, diaphragm, esophagus, stomach, heart, lungs, serous membranes and sclera [1, 2]. Mortality is significantly increased in chronic kidney disease patients with NSF vs. those without the disorder, 48% vs. 20%, respectively, over 24 months [3], and the time until death is also shortened [4]. All patients who have developed NSF to date have had stage 4 or 5 chronic kidney disease and a glomerular filtration rate of < 30 ml/min/1.73 m2 [1, 2]. It has occurred in patients both on and off dialysis. The FDA has summarized the major at risk patient populations as those with: acute or chronic severe renal insufficiency (glomerular filtration rate <30 mL/min/1.73m 2) acute renal dysfunction due to the hepatorenal syndrome or in the perioperative liver transplantation period [5]. NSF is equally common in men and women, and there is no association with race or age. Additional risk factors for NSF may include the use of erythropoesis-stimulating medications, thrombophilia (increased platelet count) and thrombosis, vascular surgical procedures, chronic liver disease, hepatorenal syndrome, and liver transplantation in the peritransplant period [1]. Many of these potential risk factors appear to be associated with activation of fibroblasts or release of inflammatory mediators. Within the last 3 years, gadolinium-based contrast agents have been identified as the inciting factor most strongly associated with the development of NSF in vulnerable patient populations, although very rare reports have documented NSF after organ transplantation (heart and kidney) without prior GBCA exposure [6]. NSF has been reported with all 5 FDA approved GBCAs, as well as with other GBCAs in use in Europe. The greatest risk appears to be with gadodiamide (Omniscan) with over 340 cases reported. This is followed by gadoversetamide (OptiMARK), gadopentetate dimeglumine (Magnevist) and less commonly gadoteridol (ProHance) and gadobenate dimeglumine (MultiHance). Northwestern uses Magnevist and MultiHance. Note that despite differences in the incidence of NSF with these agents, the FDA does not consider any of the GBCAs safe, and for the purposes of IRB policy all gadolinium based agents should be considered to confer a risk for NSF in a vulnerable subject. Repeated GBCA Version: June 3, 2009 1 exposure increases the risk of NSF 5 to 10 times vs. a single dose [1]. Symptom onset after GBCA exposure can range from 3 weeks to 18 months [7]. The median time is around 12 weeks [4]. The overall incidence of NSF is quite rare. Since 2000, approximately 200 million patients worldwide have been exposed to gadolinium, but less than 500 cases of NSF have been reported, for a prevalence of 1 in 400,000 [8]. In a study that included 4 U.S. medical centers the incidence was between 1 in 2,131 and 1 in 65,000 [9]. In patients with renal disease the risk of NSF after gadolinium exposure is significantly increased and is between 1% and 7% [1, 10]. At this time there no clearly effective therapy for the disorder, although case reports have documented improvement after successful renal transplantation and extracorporeal photophoresis [1]. Recommendations for Research Gadolinium Use at Northwestern The following guidelines were proposed based on the above background, and consideration of the FDA and American College of Radiology guidelines [5, 10]. All subjects will have a determination of their estimated glomerular filtration rate (eGFR) within 24 hours of undergoing any study where gadolinium based contrast agents will be administered. Subjects should not have a known history of recent onset acute renal dysfunction. Subjects with a history of stable chronic renal dysfunction may participate in studies using GBCA based on their eGFR, as outlined below. Subjects should not have severe liver dysfunction, particularly when associated with kidney disease. Subjects should receive GBCAs in the perioperative period (i.e. within 4 weeks) after renal or liver transplantation. Since the occurrence of NSF is very strongly linked to renal function, the proposed guidelines are stratified by the eGFR. 1) eGFR > 60 ml/min/1.73 m2 : Normal subjects or patients with stage 1 or 2 chronic kidney disease a. There is no evidence that these subjects are at an increased risk of developing NSF [10]. b. Gadolinium usage should be within FDA dosing guidelines. 2) eGFR 30 - 59 ml/min/1.73 m2 : Patients with stage 3 chronic kidney disease, history of renal or liver transplant beyond the perioperative period (even if eGFR > 60 ml/min/1.73 m2) a. If renal function has been stable the risk of NSF is estimated to be extremely low [10]. b. The protocol should use only single doses of gadolinium ( ≤ 0.1 mmol/kg) c. Subjects must not have received any other gadolinium within 1 week of the study. 3) eGFR < 30 ml/min/1.73 m2 : Patients with recent renal or liver transplant (within 4 weeks even if their eGFR is good) a. These subjects are at the highest risk of developing NSF. b. These subjects should not receive gadolinium based contrast agents in research studies. Consent Form Guidance The consent form should state that during the MRI scan subjects will be given a contrast dye containing gadolinium. Contrast dyes containing gadolinium have recently been linked to the development of Nephrogenic Systemic Fibrosis (NSF), a rare systemic disease that causes fibrosis Version: June 3, 2009 2 (scarring) of the skin, muscles and internal organs and can be fatal. NSF has been only reported to occur in patients with severe kidney disease. The risk of NSF is approximately 4% in patients with severe kidney disease. NSF has not been reported in patients with either normal kidney function or mild to moderate kidney impairment. In order to minimize the risk of NSF subjects will have their kidney function assessed by a blood test within 24 hours of an MRI scan in which they will be given a contrast dye containing gadolinium. If the result of the blood test shows there is kidney dysfunction the study doctor will discuss with the subject whether adjustments are needed to the gadolinium contrast dose. Note: Some studies may have patients with severe kidney dysfunction who receive a gadolinium based contrast dye undergo dialysis immediately after the MRI scan and again the next day. However, it is unknown if this will prevent the occurrence of NSF. Version: June 3, 2009 3 REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Kribben, A., et al., Nephrogenic systemic fibrosis: pathogenesis, diagnosis, and therapy. J Am Coll Cardiol, 2009. 53(18): p. 1621-8. Galan, A., S.E. Cowper, and R. Bucala, Nephrogenic systemic fibrosis (nephrogenic fibrosing dermopathy). Curr Opin Rheumatol, 2006. 18(6): p. 614-7. Todd, D.J., et al., Cutaneous changes of nephrogenic systemic fibrosis: Predictor of early mortality and association with gadolinium exposure. Arthritis and Rheumatism, 2007. 56(10): p. 3433-3441. Swaminathan, S., et al., Cardiac and vascular metal deposition with high mortality in nephrogenic systemic fibrosis. Kidney Int, 2008. 73(12): p. 1413-8. FDA. Information for Healthcare Professionals: Gadolinium-Based Contrast Agents for Magnetic Resonance Imaging. 2008 June 4, 2008 [cited 2009 May 27, 2009]; Available from: http://www.fda.gov/cder/drug/InfoSheets/HCP/gcca_200705.htm. Wahba, I.M., E.L. Simpson, and K. White, Gadolinium is not the only trigger for nephrogenic systemic fibrosis: insights from two cases and review of the recent literature. Am J Transplant, 2007. 7(10): p. 2425-32. Wiginton, C.D., et al., Gadolinium-based contrast exposure, nephrogenic systemic fibrosis, and gadolinium detection in tissue. AJR Am J Roentgenol, 2008. 190(4): p. 1060-8. Penfield, J.G. and R.F. Reilly, Jr., What nephrologists need to know about gadolinium. Nat Clin Pract Nephrol, 2007. 3(12): p. 654-68. Wertman, R., et al., Risk of nephrogenic systemic fibrosis: evaluation of gadolinium chelate contrast agents at four American universities. Radiology, 2008. 248(3): p. 799-806. American College of Radiology (2008) Manual on Contrast Media. 2009, 53-57. Version: June 3, 2009 4