CDAR2L3_IG_NEONATALRPT_R1_D1_2010JAN_PUBDRAFT
Neonatal Care Report (NCR)
Implementation Guide for CDA Release 2
(US Realm)
Based on HL7 CDA Release 2.0
Draft Standard for Trial use
First Ballot
January 2010
© 2010 Health Level Seven, Inc.
Ann Arbor, MI
All rights reserved.
Co-Chair/Co-Editor:
Robert H. Dolin, MD
Semantically Yours, LLC
bobdolin@gmail.com
Co-Chair/Co-Editor
Liora Alschuler
Alschuler Associates, LLC
liora@alschulerassociates.com
Co-Chair
Calvin Beebe
Mayo Clinic
cbeebe@mayo.edu
Co-Chair
Keith W. Boone
GE Healthcare
keith.boone@ge.com
Primary Editor:
Gay Giannone, MSN RN
Alschuler Associates, LLC
gay@alschulerassociates.com
Co-Editor:
Joy Kuhl, MBA, CPF
Principal | Optimal Accords, LLC
joy@optimalaccords.com
Co-Editor:
Michael A. Padula, MD
Neonatologist, Clinical Informaticist
The Children's Hospital of Philadelphia
padula@email.chop.edu
Co-Editor:
Feliciano Yu, M.D.
Information Technology Division
Pediatrics Professor
University of Alabama at Birmingham School of Medicine
fyu@peds.uab.edu
Co-Editor:
Karna Murthy, MD
Neonatologist, Children's Memorial Hospital
Assistant Professor of Pediatrics, Northwestern University
k-murthy@northwestern.edu
Co-Editor
David J. Durand, MD
Director, Division of Neonatology
Children's Hospital and Research Center Oakland
ddurand@mail.cho.org
Jacqueline Kueser
Vice President, Strategy/R&D
Children’s Hospitals Corporation of America
jacqueline.kueser@chca.com
Co-Editor
Co-Editor
Kirk Elrod
CHCA IT Liaison/Business Analyst
Children’s Hospitals Corporation of America
kirk.elrod@chca.com
Current Working Group also
includes:
Kate Conrad, Bobby George, Andy Spooner, David Muraco,
Diane Ward, Celeste Milton, Jean Millar, Ann Watt, Shaun
Shakib, Sandy Stuart, Brett Marquard, Jingdong (JD) Li,
Anneke Goossen, William Goossen, Teresa Finitzo
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 2
January 2010
Acknowledgments
This guide was produced and developed through the efforts of the Neonatal Care Report
(NCR) Project supported by the Children’s Hospitals Neonatal Consortium (CHNC), a
group of over 25 children’s hospital Neonatal Intensive Care Units, in collaboration with
the Child Health Corporation of America (CHCA), a business alliance of 43 leading
children’s hospitals in North America.
CHNC and CHCA thank the Health Level Seven (HL7) Structured Documents Work
Group for its support and sponsorship of this project within HL7, the Child Health
Work Group for its participation, and the other volunteers throughout HL7 who
contributed time and input into the effort.
Finally, we acknowledge the foundational work on HL7 Version 3 and the Reference
Information Model (RIM), the HL7 domain committees, especially Patient Care, and the
work done on Clinical Document Architecture (CDA) itself.
All these efforts were critical ingredients to the development of this Draft Standard for
Trial Use (DSTU), and the degree to which the DSTU reflects these efforts will foster
interoperability across the spectrum of health care.
SNOMED CT is the registered trademark of the International Health Terminology
Standard Development Organisation (IHTSDO). LOINC is a registered United States
trademark of Regenstrief Institute, Inc.
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 3
January 2010
Revision History
Rev
Date
By Whom
Changes
Final
DSTU for
ballot
12/11/2009
Et al
Final draft for ballot submitted to HL7
Headquarters.
Draft with
tracked
changes
3/17/2010
Et al
Draft for publication with tracked
changes posted for review prior to
submission to HQ for publication
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 4
January 2010
Table of Contents
1
INTRODUCTION ............................................................................................................ 10
1.1
Purpose................................................................................................................... 10
1.2
Approach ................................................................................................................ 10
1.3
Scope ...................................................................................................................... 10
1.3.1
Inheritance of Constraints ................................................................................ 11
1.3.2
Future Work .................................................................................................... 11
1.4
Audience ................................................................................................................. 11
1.5
Organization of This Guide ...................................................................................... 11
1.5.1
Templates ........................................................................................................ 11
1.5.2
Vocabularies and Value Sets............................................................................. 12
1.6
1.6.1
Originator Responsibilities: General Case .......................................................... 12
1.6.2
Recipient Responsibilities: General Case ........................................................... 12
1.7
2
Conventions Used in This Guide .............................................................................. 12
1.7.1
Conformance Requirements .............................................................................. 12
1.7.2
Keywords ......................................................................................................... 14
1.7.3
XML Examples ................................................................................................. 14
1.8
Contents of the DSTU Package................................................................................. 15
1.9
Templates by Containment ...................................................................................... 15
DOCUMENT TEMPLATE ................................................................................................ 17
2.1
3
Use of Templates ..................................................................................................... 12
Neonatal Care Report .............................................................................................. 17
SECTION TEMPLATES .................................................................................................. 22
3.1
CCD Encounters section .......................................................................................... 22
3.1.1
4
Encounters section – NCR ................................................................................ 22
3.2
Acuity score data section ......................................................................................... 23
3.3
Patient data section ................................................................................................. 24
3.4
Patient data section – NCR....................................................................................... 25
3.5
Reporting parameters section .................................................................................. 27
CLINICAL STATEMENT TEMPLATES ............................................................................. 29
4.1
Acuity indicator data generic organizer .................................................................... 29
4.2
Acuity data time organizer - admission to 12 hours .................................................. 32
4.3
Acuity data time organizer - day 3............................................................................ 33
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 5
January 2010
4.4
Acuity data time organizer - day 7............................................................................ 33
4.5
Admission activity – neonatal................................................................................... 34
4.6
CCD Encounter activity ........................................................................................... 35
4.6.1
4.7
Neonatal ICU encounter activity ........................................................................ 35
CCD Medication activity .......................................................................................... 37
4.7.1
Nitric oxide administration ............................................................................... 38
4.7.2
Oxygen administration ..................................................................................... 39
4.8
CCD Result observation ........................................................................................... 41
4.8.1
CDA XML patterns conforming to CCD Result observation ................................ 42
4.8.2
Activated partial thromboplastin time ............................................................... 43
4.8.3
Alanine aminotransferase (ALT) ........................................................................ 43
4.8.4
Albumin observation ........................................................................................ 44
4.8.5
Apgar at 1 minute ............................................................................................ 44
4.8.6
Apgar at 5 minutes ........................................................................................... 45
4.8.7
Apgar score prolonged ...................................................................................... 45
4.8.8
Arterial PaO2 Observation ................................................................................ 46
4.8.9
Aspartate aminotransferase (AST) ..................................................................... 46
4.8.10
Bicarbonate serum ........................................................................................... 47
4.8.11
Bilirubin, conjugated ........................................................................................ 47
4.8.12
Bilirubin, total .................................................................................................. 48
4.8.13
Birth head circumference ................................................................................. 48
4.8.14
Birth weight ..................................................................................................... 48
4.8.15
Blood gas base deficit ....................................................................................... 49
4.8.16
Blood gas base excess ...................................................................................... 50
4.8.17
Blood pH .......................................................................................................... 50
4.8.18
Blood urea nitrogen (BUN) ................................................................................ 51
4.8.19
Body temperature ............................................................................................. 51
4.8.20
Body weight ..................................................................................................... 52
4.8.21
Calcium ionized ................................................................................................ 52
4.8.22
Calcium total serum ......................................................................................... 53
4.8.23
Creatinine observation...................................................................................... 53
4.8.24
Diastolic blood pressure ................................................................................... 53
4.8.25
Fibrinogen level ................................................................................................ 54
4.8.26
Gestational age ................................................................................................ 54
4.8.27
Glucose serum ................................................................................................. 55
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 6
January 2010
4.8.28
Head circumference .......................................................................................... 55
4.8.29
Heart rate ........................................................................................................ 56
4.8.30
Hemoglobin ...................................................................................................... 56
4.8.31
International normalized ratio (INR) .................................................................. 57
4.8.32
Lactic acid from serum/plasma ........................................................................ 57
4.8.33
Mean airway pressure ...................................................................................... 57
4.8.34
Mean blood pressure ........................................................................................ 58
4.8.35
PaCO2 Observation .......................................................................................... 58
4.8.36
Platelets ........................................................................................................... 59
4.8.37
Potassium serum ............................................................................................. 60
4.8.38
Prothrombin time (PT) ...................................................................................... 60
4.8.39
Respiratory rate ............................................................................................... 60
4.8.40
Seizures ........................................................................................................... 61
4.8.41
Sodium serum .................................................................................................. 61
4.8.42
Systolic blood pressure ..................................................................................... 62
4.8.43
Urine output .................................................................................................... 62
4.8.44
White blood cell (leukocyte) count ..................................................................... 63
4.9
Discharge activity – Neonatal ................................................................................... 63
4.10 Inborn/outborn ....................................................................................................... 64
4.11 Nothing by mouth (NPO) .......................................................................................... 65
4.12 Oxygenation index ................................................................................................... 65
4.13 PaO2/FIO2 ratio ..................................................................................................... 66
4.14 Renal dialysis (renal replacement therapy) ............................................................... 66
4.15 Reporting parameters act ........................................................................................ 67
4.16 Respiratory or ventilatory support ............................................................................ 68
4.17 Respiratory severity score ........................................................................................ 69
4.18 Steroid treatment (systemic) .................................................................................... 70
4.19 CCD Location participation ...................................................................................... 71
4.19.1
5
Neonatal ICU location ....................................................................................... 71
REFERENCES .............................................................................................................. 73
APPENDIX A —
ACRONYMNS AND ABBREVIATIONS ......................................................... 74
APPENDIX B —
TEMPLATES USED IN THIS GUIDE ........................................................... 76
APPENDIX C —
SUMMARY OF VALUE SETS ...................................................................... 79
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 7
January 2010
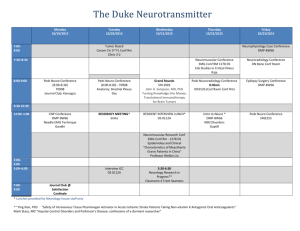
Table of Figures
Figure 1: Template name and "conforms to" appearance ....................................................... 13
Figure 2: Template-based conformance statements example ................................................. 13
Figure 3: CCD conformance statements example .................................................................. 14
Figure 4: ClinicalDocument example .................................................................................... 14
Figure 5: NCR document template example .......................................................................... 20
Figure 6: NCR encounters section example ........................................................................... 23
Figure 7: Acuity score data section example.......................................................................... 24
Figure 8: NCR patient data section example .......................................................................... 27
Figure 9: Reporting parameters section example ................................................................... 28
Figure 10: Admission activity act example ............................................................................ 34
Figure 11: Neonatal ICU encounter example ......................................................................... 37
Figure 12: Nitric oxide administration example ..................................................................... 39
Figure 13: Oxygen administration example ........................................................................... 41
Figure 14: Typical laboratory pattern for CCD-result observation conforming templates ........ 42
Figure 15: Typical non-laboratory pattern for CCD-result observation conforming templates . 42
Figure 16: Specimen type pattern for CCD-result observation conforming templates .............. 43
Figure 17: Neonatal discharge activity example ..................................................................... 64
Figure 18: Inborn/outborn example ..................................................................................... 64
Figure 19: Nothing by mouth (NPO) example ......................................................................... 65
Figure 20: Oxygenation index example ................................................................................. 66
Figure 21: PaO2/FIO2 example ............................................................................................ 66
Figure 22: Renal dialysis example (did not occur) .................................................................. 67
Figure 23: Reporting parameters act example ....................................................................... 68
Figure 24: Respiratory or ventilatory support example .......................................................... 69
Figure 25: Respiratory severity score example ....................................................................... 69
Figure 26: Steroid treatment example ................................................................................... 70
Figure 27: Neonatal ICU location example ............................................................................ 72
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 8
January 2010
Table of Tables
Table 1: Contents of the DSTU Package ................................................................................ 15
Table 2: Templates by Containment ...................................................................................... 16
Table 3: Templates Organized Hierarchically ......................................................................... 76
Table 4: Summary of Value Sets ........................................................................................... 79
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 9
January 2010
1 INTRODUCTION
1.1 Purpose
Over the previous few years, the Children’s Hospitals Neonatal Consortium (CHNC), a
group of over 25 children’s hospital Neonatal Intensive Care Units (NICUs), developed a
core data set of common data elements important to children’s hospital NICUs. CHNC
is committed to developing tools to evaluate the effectiveness of tertiary neonatal
intensive care in their unique patient population. Through the systematic collection
and analyses of clinical data on infants admitted to children’s hospital NICUs, CHNC
expects to spearhead benchmarking, quality improvement, and research initiatives that
have not previously been possible in their patient population. In 2008, CHNC
approached CHCA, a business alliance of 43 leading children’s hospitals in North
America, to assist in creation of the database for this effort.
This project is intended to facilitate electronic extraction of a subset of the CHNC data
set using a standard reporting specification in the form of a Neonatal Care Report (NCR)
to support performance improvement and research. CHNC and CHCA envision this
effort as a building block for more widespread use of the electronic medical record in
place of manual data abstraction.
1.2 Approach
The CHNC core data set contains around 700 data elements; a subset of approximately
60 data elements are addressed in this Draft Standard, including 37 physiologic and
laboratory elements for assessment of illness severity (4.1 Acuity indicator data generic
organizer) and 21 base data elements (found throughout the header and body of the
NCR, e.g. name, medical record number, birth weight and discharge head
circumference). Some of the data elements included in the NCR are known to
correspond to Vermont Oxford Network (VON); others correspond to data collection sets
mapped to national standards such as the Continuity of Care Document (CCD) and the
Quality Reporting Document Architecture (QRDA). Working with an initial portion of
the data provides the opportunity to work with the data from the perspective of the
underlying model and electronic format and to explore many design issues thoroughly.
Taking this as an initial step ensures that the data set developers and standards
community can reach consensus prior to the larger commitment of time that would be
required to bring the full data set into standard format.
This project supports reusability and ease of data collection through a standard data
representation harmonized with work developed through Health Information Technology
Expert Panel (HITEP), balloted through Health Level Seven (HL7) and/or recognized by
the Health Information Technology Standards Panel (HITSP).
This implementation guide (IG) specifies a standard for electronic submission of NCRs
in a Clinical Document Architecture (CDA), Release 2 format.
1.3 Scope
This implementation guide is a conformance profile, as described in the Refinement and
Localization section of the HL7 Version 3 standards. The base standard for this
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 10
January 2010
implementation guide is the HL7 Clinical Document Architecture, Release 2.0. As
defined in that document, this implementation guide is both an annotation profile and a
localization profile. It does not describe every aspect of CDA.
1.3.1 Inheritance of Constraints
As an annotation profile, portions of this implementation guide summarize or explain
the base standard; therefore, not all requirements stated here are original to the
implementation guide. Some originate in the base specification. Those requirements
that do not add further constraints to the base standard and that can be validated
through CDA.xsd may not have corresponding conformance statements.
Where no constraints are stated in this guide, NCR CDA instances are subject to and
are to be created in accordance with the base CDA R2 specification. Where, for
instance, the CDA R2 specification declares an attribute to be optional and the NCR
specification contains no additional constraints, that attribute remains optional for use
in an NCR CDA instance.
1.3.2 Future Work
The standard data submission format supported through this project represents a key,
initial step in the move toward automation of data collection for quality monitoring and
improvement in children’s hospitals NICUs. A natural follow-on to this work is a pilot
project integrating the reporting into current workflow and information technology
infrastructures. Other possible future work includes expansion of the NCR to include
additional data elements.
1.4 Audience
The audience for this document includes software developers and implementers who
wish to develop reporting capabilities within their electronic health record (EHR and
Pediatric EHR systems), and developers and analysts in receiving institutions who wish
to process CDA NCR documents created according to this specification. The intended
audience also includes neonatal experts and other children’s hospital providers.
1.5 Organization of This Guide
The requirements as laid out in the body of this document are subject to change per the
policy on implementation guides (see section 13.02 “Draft Standard for Trial Use
Documents” within the HL7 Governance and Operations Manual,
http://www.hl7.org/documentcenter/public/membership/HL7_Governance_and_Oper
ations_Manual.pdf).
1.5.1 Templates
Templates are organized by document (see Document Template), by section (see Section
Templates), and by clinical statements (see Clinical Statement Templates). Within a
section, templates are arranged hierarchically, where a more specific template is nested
under the more generic template that it conforms to. See Templates by Containment for
a listing of the higher level templates by containment; the appendix Templates Used in
This Guide includes a table of all of the templates Organized Hierarchically.
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 11
January 2010
1.5.2 Vocabularies and Value Sets
Vocabularies recommended in this guide are from standard vocabularies. When
SNOMED codes are used, rules defined in Using SNOMED CT in HL7 Version 3 are
adhered to. In many cases, these vocabularies are further constrained into value sets
for use within this guide. Value set names and OIDs are summarized in the table
Summary of Value Sets. Each named value set in this summary table is stored in a
template database that will be maintained by CHCA.
1.6 Use of Templates
When valued in an instance, the template identifier (templateId) signals the imposition
of a set of template-defined constraints. The value of this attribute provides a unique
identifier for the templates in question.
1.6.1 Originator Responsibilities: General Case
An originator can apply a templateId to assert conformance with a particular
template.
In the most general forms of CDA exchange, an originator need not apply a templateId
for every template that an object in an instance document conforms to. This
implementation guide asserts when templateIds are required for conformance.
1.6.2 Recipient Responsibilities: General Case
A recipient may reject an instance that does not contain a particular templateId (e.g.,
a recipient looking to receive only CCD documents can reject an instance without the
appropriate templateId).
A recipient may process objects in an instance document that do not contain a
templateId (e.g., a recipient can process entries that contain Observation acts within
a Problems section, even if the entries do not have templateIds).
1.7 Conventions Used in This Guide
1.7.1 Conformance Requirements
Conformance statements are grouped and identified by the name of the template, along
with the templateId and the context of the template (e.g., ClinicalDocument, section,
observation), which specifies the element under constraint. If a template is a
specialization of another template, its first constraint indicates the more general
template. In all cases where a more specific template conforms to a more general
template, asserting the more specific template also implies conformance to the more
general template. An example is shown below.
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 12
January 2010
Figure 1: Template name and "conforms to" appearance
Template name
[<type of template>: templateId <XXXX.XX.XXX.XXX>]
Description of the template will be here .....
1. Conforms to <The template name> Template (templateId: XXXX<XX>XXX>YYY).
2. SHALL contain [1..1] @classCode = <AAA> <code display name> (CodeSystem:
123.456.789 <XXX> Class) STATIC (CONF:<number>).
.......
The conformance verb keyword at the start of a constraint ( SHALL, SHOULD, MAY, etc.)
indicates business conformance, whereas the cardinality indicator (0..1, 1..1, 1..*, etc.)
specifies the allowable occurrences within an instance. Thus, " MAY contain 0..1" and
"SHOULD contain 0..1" both allow for a document to omit the particular component, but
the latter is a stronger recommendation that the component be included if it is known.
The following cardinality indicators may be interpreted as follows:
0..1 as zero to one present
1..1 as one and only one present
2..2 as two must be present
1..* as one or more present
0..* as zero to many present
Value set bindings adhere to HL7 Vocabulary Working Group best practices, and
include both a conformance verb (SHALL, SHOULD, MAY, etc.) and an indication of
DYNAMIC vs. STATIC binding. The use of SHALL requires that the component be valued
with a member from the cited value set; however, in every case any HL7 "null" value
such as other (OTH) or unknown (UNK) may be used.
Each constraint is uniquely identified (e.g., "CONF:605") by an identifier placed at or
near the end of the constraint. These identifiers are not sequential as they are based on
the order of creation of the constraint.
Figure 2: Template-based conformance statements example
1.
contain [1..1] component/structuredBody (CONF:4082).
a. This component/structuredBody SHOULD contain [0..1] component
(CONF:4130) such that it
i.
SHALL contain [1..1] Reporting Parameters section
(templateId:2.16.840.1.113883.10.20.17.2.1) (CONF:4131).
b. This component/structuredBody SHALL contain [1..1] component
(CONF:4132) such that it
i.
SHALL contain [1..1] Patient data section - NCR
(templateId:2.16.840.1.113883.10.20.17.2.5) (CONF:4133).
SHALL
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 13
January 2010
CCD templates are included within this implementation guide for ease of reference.
CCD templates contained within this implementation guide are formatted WITHOUT
typical KEYWORD and XML element styles. A WIKI site is available if you would like to
make a comment to be considered for the next release of CCD:
http://wiki.hl7.org/index.php?title=CCD_Suggested_Enhancements. The user name
and password are: wiki/wikiwiki. You will need to create an account to edit the page
and add your suggestion.
Figure 3: CCD conformance statements example
1. The value for “Observation / @moodCode” in a problem observation SHALL be
“EVN” 2.16.840.1.113883.5.1001 ActMood STATIC. (CONF: 814).
2. A problem observation SHALL include exactly one Observation / statusCode.
(CONF: 815).
3. The value for “Observation / statusCode” in a problem observation SHALL be
“completed” 2.16.840.1.113883.5.14 ActStatus STATIC. (CONF: 816).
4. A problem observation SHOULD contain exactly one Observation / effectiveTime, to
indicate the biological timing of condition (e.g. the time the condition started, the
onset of the illness or symptom, the duration of a condition). (CONF: 817).
1.7.2 Keywords
The keywords SHALL, SHALL NOT, SHOULD, SHOULD NOT, MAY, and NEED NOT in this
document are to be interpreted as described in the HL7 Version 3 Publishing
Facilitator's Guide:
SHALL:
an absolute requirement
SHALL NOT:
an absolute prohibition against inclusion
SHOULD/SHOULD NOT:
valid reasons to include or ignore a particular item, but
must be understood and carefully weighed
MAY/NEED NOT:
truly optional; can be included or omitted as the author decides
with no implications
1.7.3 XML Examples
XML samples appear in various figures in this document in a fixed-width font.
Portions of the XML content may be omitted from the content for brevity, marked by an
ellipsis (…) as shown in the example below.
Figure 4: ClinicalDocument example
<ClinicalDocument mins=’urn:h17-org:v3’>
...
</ClinicalDocument>
XPath expressions are used in the narrative and conformance requirements to identify
elements because they are familiar to many XML implementers.
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 14
January 2010
1.8 Contents of the DSTU Package
Table 1: Contents of the DSTU Package
Filename
Description
CDAR2L3_IG_NEONATALRPT_
R1_D1_2010JAN_PUBDRAFT
This guide
NeonatalCareReport.xml
The Neonatal Care Report sample
cda.xsl
A generic stylesheet for displaying the content of the
sample document in HTML
1.9 Templates by Containment
The table below shows the Neonatal Case Report (NCR) templates organized by the
document template and the section templates the document contains. In turn, it shows
the sections and many of the clinical statement entry templates the sections contain.
The 44 clinical statement templates contained in the Acuity indicator data generic
organizer templates are not included for ease of reading. This Table 2: Templates by
Containment table is placed before the template descriptions and conformance
statements to provide an understanding of various groupings and organization of the
templates as they would exist in an NCR CDA instance. To view all of the templates
contained in the guide in hierarchical order, see the Templates Organized Hierarchically
table.
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 15
January 2010
Table 2: Templates by Containment
Template OID
Type
2.16.840.1.113883.10.20.17.1.1
document Neonatal Care Report
2.16.840.1.113883.10.20.17.2.1
2.16.840.1.113883.10.20.17.3.8
2.16.840.1.113883.10.20.17.2.5
section
entry
section
Template Title
Reporting parameters section
Reporting parameters act
Patient data section - NCR
2.16.840.1.113883.10.20.17.3.4
entry
Apgar at 1 minute
2.16.840.1.113883.10.20.17.3.5
entry
Apgar at 5 minute
2.16.840.1.113883.10.20.17.3.6
entry
Apgar score prolonged
2.16.840.1.113883.10.20.17.3.2
entry
Birth head circumference
2.16.840.1.113883.10.20.17.3.1
entry
Birth weight
2.16.840.1.113883.10.20.17.3.3
entry
Gestational age
2.16.840.1.113883.10.20.17.3.7
entry
Inborn/outborn
2.16.840.1.113883.10.20.17.2.2
section
Encounters section NCR
2.16.840.1.113883.10.20.17.3.15
entry
Neonatal ICU encounter activity
2.16.840.1.113883.10.20.17.3.14
subentry
Neonatal ICU location
2.16.840.1.113883.10.20.17.3.12
entry
Admission activity - neonatal
2.16.840.1.113883.10.20.17.3.10 entry
Body temperature
2.16.840.1.113883.10.20.17.3.11 entry
Body weight
2.16.840.1.113883.10.20.17.3.13
entry
Discharge activity - Neonatal
2.16.840.1.113883.10.20.17.3.11 entry
Body weight
2.16.840.1.113883.10.20.17.3.9
Head circumference
2.16.840.1.113883.10.20.17.2.3
entry
section
Acuity score data section
entry
Acuity indicator data generic
organizer1
2.16.840.1.113883.10.20.17.3.60
entry
Acuity data time organizer admission to 12 hours
2.16.840.1.113883.10.20.17.3.61
entry
Acuity data time organizer - day 3
2.16.840.1.113883.10.20.17.3.62
entry
Acuity data time organizer - day 7
2.16.840.1.113883.10.20.17.3.59
The 44 clinical statement templates contained in the Acuity indicator data generic organizer
template are not included in this chart for ease of reading. Please see the template itself.
1
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 16
January 2010
2
DOCUMENT TEMPLATE
2.1 Neonatal Care Report
[ClinicalDocument: templateId 2.16.840.1.113883.10.20.17.1.1]
The Neonatal Care Report (NCR) constrains CDA to express the data elements identified
by CHNC. This NCR CDA R2 document template defines the data elements that belong
in the header of the NCR CDA document and prescribes the sections that belong in the
NCR. The NCR document contains an initial segment of data elements from the CHNC
Neonatal Intensive Care Unit (NICU) Core Data Set (CDS). This NCR CDA will send
these data elements from neonatal intensive care providers to the CHNC database in
standardized CDA format for analysis and performance improvement work.
A complete NCR is created and sent after an infant is discharged. An initial NCR may be
created and sent shortly after the infant is born. Many data elements in this initial NCR
will have null values for the values that are unknown or not applicable at this point.
The complete NCR sent after discharge will replace the initial document.
Implementers should note that constraints 6, 7, and 9.b. below duplicate the CDA R2
base standard and are called out for emphasis; this NCR implementation requires no
further constraints on them unless further constrained by a child constraint.
1. SHALL contain [1..1] realmCode="US" (CodeSystem: 2.16.840.1.113883.5.147 HL7
RealmOfUse) STATIC (CONF:4066).
2. SHALL contain [1..1] templateId/@root="2.16.840.1.113883.10.20.17.1.1"
(CONF:4067).
3. SHALL contain [1..1] code/@code="NCR-X" Neonatal Care Report (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:4068).
4. SHALL contain [1..1] title (CONF:4069).
a. This title SHALL be valued with a case-insensitive, text string containing
"Neonatal Care Report" (CONF:4083).
5. SHALL contain [1..1] recordTarget (CONF:4070).
a. This recordTarget SHALL contain [1..1] patientRole (CONF:4071).
i.
This patientRole SHALL contain [1..*] id (CONF:4175).
1. Such ids SHALL have one id that is the infant's medical record
number (CONF:4203).
ii.
This patientRole SHALL contain [1..1] patient (CONF:4183).
1. This patient SHALL contain [1..*] name (CONF:4184) such that it
a. SHALL contain [1..1] given (CONF:4185).
b. SHALL contain [1..1] family (CONF:4186).
c. SHALL contain [1..1] validTime/low (CONF:4187).
d. At least one name SHALL not have a valid/time/high
indicating this was the name at the time of discharge.
(CONF:4202).
2. This patient SHALL contain [1..1]
administrativeGenderCode/@code, which SHALL be selected
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 17
January 2010
from ValueSet 2.16.840.1.113883.11.20.5.24 NCR gender
DYNAMIC (CONF:4191).
3. This patient SHALL contain [1..1] birthTime (CONF:4195).
a. This birthTime SHALL be precise at least to the day.
(CONF:4240).
6. SHALL contain [1..*] author (CONF:4072).
7. SHALL contain [1..1] custodian (CONF:4075).
a. This custodian SHALL be the reporting hospital. (CONF:4177).
8. SHALL contain [1..1] participant (CONF:4084) such that it
a. SHALL contain [1..1] @typeCode="IND" (CodeSystem: 2.16.840.1.113883.5.90
HL7ParticipationType) STATIC (CONF:4085).
b. SHALL contain [1..1] associatedEntity (CONF:4088).
i.
ii.
iii.
This associatedEntity SHALL contain [1..1] @classcode="PRS"
(CodeSystem: 2.16.840.1.113883.5.6 HL7ActClass) STATIC
(CONF:4089).
This associatedEntity SHALL contain [1..1] code="MTH" (CodeSystem:
2.16.840.1.113883.5.111 HL7RoleCode) STATIC (CONF:4090).
This associatedEntity SHALL contain [1..1] addr (CONF:4091).
1. This addr SHALL contain [1..1] postalCode (CONF:4095).
2. This addr SHALL contain [1..1] useablePeriod (CONF:4086).
a. This useablePeriod SHALL contain the discharge date of the
infant within its interval. (CONF:4087).
iv.
This associatedEntity SHALL contain [1..1] associatedPerson
(CONF:4092).
1. This associatedPerson SHALL contain [1..1] name (CONF:4093).
a. This name SHALL contain [1..1] family (CONF:4094).
9. MAY contain [0..1] relatedDocument (CONF:4096) such that it
a. SHALL contain [1..1] @typeCode="RPLC" (CodeSystem: 2.16.840.1.113883.5.90
HL7ParticipationType) STATIC (CONF:4097).
b. SHALL contain [1..1] parentDocument (CONF:4098).
i.
ii.
iii.
This parentDocument SHALL contain [1..1] @classCode="DOCCLIN"
(CodeSystem: 2.16.840.1.113883.5.6 HL7ActClass) STATIC
(CONF:4099).
This parentDocument SHALL contain [1..1] @moodCode="EVN"
(CodeSystem: 2.16.840.1.113883.5.1001 HL7ActMood) STATIC
(CONF:4100).
This parentDocument SHALL contain [1..1] id (CONF:4101).
10. SHALL contain [1..1] componentOf (CONF:4104).
a. This componentOf SHALL contain [1..1] encompassingEncounter (CONF:4105).
i.
ii.
iii.
This encompassingEncounter SHALL contain [1..1] id (CONF:4106).
This encompassingEncounter SHALL contain [1..1] effectiveTime/low
(CONF:4108).
This encompassingEncounter SHALL contain [1..1] effectiveTime/high
(CONF:4109).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 18
January 2010
iv.
This encompassingEncounter SHALL contain [1..1] location
(CONF:4234).
1. This location SHALL contain [1..1] healthCareFacility
(CONF:4235).
a. This healthCareFacility SHALL contain [1..*] id
(CONF:4236).
i.
At least one id SHALL contain
@root="2.16.840.1.113883.3.375" and SHALL
contain @extension composed of a unique number
assigned by CHNC (CONF:4237).
11. SHALL contain [1..1] component/structuredBody (CONF:4082).
a. This component/structuredBody MAY contain [0..1] component (CONF:4130)
such that it
i.
contain [1..1] Reporting parameters section
(templateId:2.16.840.1.113883.10.20.17.2.1) (CONF:4131).
SHALL
b. This component/structuredBody SHALL contain [1..1] component (CONF:4132)
such that it
i.
contain [1..1] Patient data section - NCR
(templateId:2.16.840.1.113883.10.20.17.2.5) (CONF:4133).
SHALL
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 19
January 2010
Figure 5: NCR document template example
<realmCode code="US" />
<typeId root="2.16.840.1.113883.1.3" extension="POCD_HD000040" />
<templateId root="2.16.840.1.113883.10.20.17.1.1" />
<!-- Fake document id -->
<id root="cf18e3e1-aea7-4553-a087-b42a004dd27d" />
<code code="NCR-X" codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC"
displayName="Neonatal Care Report" />
<title>Neonatal Care Report</title>
<effectiveTime value="200906261100" />
<confidentialityCode codeSystem="2.16.840.1.113883.5.25" code="N" />
<languageCode code="en-US" />
<recordTarget>
<patientRole>
...
<patient>
<name use="L">
<!-- "official" name -->
<given>Kari</given>
<family>Kidd</family>
<validTime>
<low value="20090325" />
<!-- low value without a high value, indicates this was the name in
place at the time of discharge) -->
</validTime>
</name>
<name use="ASGN">
<given>Baby Girl</given>
<family>Mumm</family>
<validTime>
<high value="20090325" />
<!-- High value indicating when name was no longer valid -->
</validTime>
</name>
<administrativeGenderCode code="1086007"
codeSystem="2.16.840.1.113883.6.96" displayName="Female" />
<birthTime value="200903031537" />
</patient>
</patientRole>
</recordTarget>
<author>
...
</author>
<!-- The CHCA hospital responsible for the data (the sending org. is serving as
custodian. -->
<custodian>
...
</custodian>
<legalAuthenticator>
...
</legalAuthenticator>
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 20
January 2010
<!-- Mother's name (and address, note: CDS only requires zipcode) with time –
at the discharge from infant's first admission. -->
<participant typeCode="IND">
<associatedEntity classCode="PRS">
<code code="MTH" codeSystem="2.16.840.1.113883.5.111" />
addr>
<postalCode>99999</postalCode>
<useablePeriod value="20090625"/>
<!-- discharge date -->
</addr>
<associatedPerson>
<name>
<!--Biological mother's name -->
<given>Martha</given>
<family>Mum</family>
</name>
</associatedPerson>
</associatedEntity>
</participant>
<!-- This represents how to show that a CDA NCR created after discharge
replaces the initial CDA NCR that was created and sent at the time of
delivery -->
<relatedDocument typeCode="RPLC">
<parentDocument classCode="DOCCLIN" moodCode="EVN">
<!-- Below is a fake id representing the id of the intial document -->
<id root="d619e9c0-d168-11de-8a39-0800200c9a66" />
<code codeSystem="2.16.840.1.113883.6.1" codeSystemName="LOINC"
code="NCR-X" displayName="Neonatal Care Report" />
</parentDocument>
</relatedDocument>
<componentOf>
<encompassingEncounter>
<id extension="IN302902" root="1.1.2" />
<!-- encompassingEncounterID shall be the "Data Processing (DP)
Account number"(example), a number unique to the visit -->
<effectiveTime>
<low value="200903031600" />
<high value="20090625" />
</effectiveTime>
</encompassingEncounter>
</componentOf>
...
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 21
January 2010
3 SECTION TEMPLATES
3.1 CCD Encounters section
[section: templateId 2.16.840.1.113883.10.20.1.3]
The CCD encounters section is used to list and describe any healthcare encounters
pertinent to the patient's current health status or historical health history. An
encounter is an interaction, regardless of the setting, between a patient and a
practitioner who is vested with primary responsibility for diagnosing, evaluating, or
treating the patient's condition. It may include visits, appointments, as well as non faceto-face interactions. It is also a contact between a patient and a practitioner who has
primary responsibility for assessing and treating the patient at a given contact,
exercising independent judgment. This section may contain all encounters for the time
period being summarized, but should include notable encounters.
1. The encounters section SHALL contain Section / code. (CONF:593).
2. The value for "Section / code" SHALL be "46240-8" "History of encounters"
2.16.840.1.113883.6.1 LOINC STATIC. (CONF:594).
3. The encounters section SHALL contain Section / title. (CONF:595).
4. Section / title SHOULD be valued with a case-insensitive language-insensitive text
string containing "encounters". (CONF:596).
3.1.1 Encounters section – NCR
[section: templateId 2.16.840.1.113883.10.20.17.2.2]
This section contains administrative encounter information and selected data specific to
each admission and discharge in an encounter. This section contains data for the
current encounter being reported and may contain information about historical
encounters.
1. Conforms to CCD Encounters section Template (templateId:
2.16.840.1.113883.10.20.1.3).
2. SHALL contain [1..1] templateId/@root="2.16.840.1.113883.10.20.17.2.2"
(CONF:3337).
3. SHALL contain [1..1] title="Encounters" (CONF:3338).
4. SHALL contain [1..1] text (CONF:3339).
5. SHALL contain [1..*] entry (CONF:3340) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3341).
b. SHALL contain [1..1] Neonatal ICU encounter activity
(templateId:2.16.840.1.113883.10.20.17.3.15) (CONF:3342).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 22
January 2010
Figure 6: NCR encounters section example
<section>
<templateId root="2.16.840.1.113883.10.20.1.3" />
<templateId root="2.16.840.1.113883.10.20.17.2.2" />
<code code="46240-8" codeSystem="2.16.840.1.113883.6.1"
displayName="Encounters" />
<title>Encounters</title>
<text>
...
</text>
<entry typeCode="DRIV">
<encounter classCode="ENC" moodCode="EVN">
<!-- CCD Encounter activity template -->
<templateId root="2.16.840.1.113883.10.20.1.21" />
<!-- Neonatal ICU encounter activity -->
<templateId root="2.16.840.1.113883.10.20.17.3.15" />
<id extension="IN302902" root="1.1.2" />
<!-- same as encompassing encounterID -->
...
</encounter>
</entry>
</section>
3.2 Acuity score data section
[section: templateId 2.16.840.1.113883.10.20.17.2.3]
This section contains the templates that represent data elements whose variants are
thought to be significant indicators of the severity of illness and of subsequent infant
outcomes. Using organizers the data is grouped into three clinically significant periods
of time: the first 12 hours of an admission, and the third and seventh days of an
admission.
1. SHALL contain [1..1] code/@code=" 11283-9" Acuity Assessment (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:4205).
2. SHALL contain [1..1] title="ACUITY SCORE DATA" (CONF:4206).
3. SHALL contain [1..1] text (CONF:4207).
4. SHALL contain [1..1] templateId/@root="2.16.840.1.113883.10.20.17.2.3"
(CONF:4165).
5. SHALL contain [1..1] entry (CONF:4172) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4167).
b. SHALL contain [1..1] Acuity data time organizer - admission to 12
hours (templateId:2.16.840.1.113883.10.20.17.3.60) (CONF:4168).
6. SHALL contain [1..1] entry (CONF:4169) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4170).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 23
January 2010
b. SHALL contain [1..1] Acuity data time organizer - day 3
(templateId:2.16.840.1.113883.10.20.17.3.61) (CONF:4171).
7. SHALL contain [1..1] entry (CONF:4166) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4173).
b. SHALL contain [1..1] Acuity data time organizer - day 7
(templateId:2.16.840.1.113883.10.20.17.3.62) (CONF:4174).
Figure 7: Acuity score data section example
<section>
<templateId root="2.16.840.1.113883.10.20.17.2.3" />
<code code="11283-9" codeSystem="2.16.840.1.113883.6.1"
displayName="Acuity assessment" />
<title>Acuity score data</title>
<organizer moodCode="EVN" classCode="CLUSTER">
<!-- This is the first acuity data organizer = Admit -> 1st 12 hr
...
<effectiveTime>
<low value="200903031600" />
<high value="200903040400" />
</effectiveTime>
...
<organizer moodCode="EVN" classCode="CLUSTER">
<!-- This is the second data organizer = Day 3 of admission -->
...
<effectiveTime>
<low value="200903050001" />
<high value="200903052359" />
</effectiveTime>
...
<organizer moodCode="EVN" classCode="CLUSTER">
<!-- This is the third acuity data organizer = Day 7 of admission
...
<effectiveTime>
<low value="200903100001" />
<high value="200903102359" />
</effectiveTime>
...
</section>
-->
-->
3.3 Patient data section
[section: templateId 2.16.840.1.113883.10.20.17.2.4]
The patient data section contains clinically significant patient data and may contain
patient data elements and measure-specific grouping data elements as defined by
particular measure(s).
1. SHALL contain [1..1] code/@code="55188-7" Patient data (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3865).
2. SHALL contain [1..1] title="PATIENT DATA" (CONF:3866).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 24
January 2010
3. SHALL contain [1..1] text (CONF:3867).
3.4 Patient data section – NCR
[section: templateId 2.16.840.1.113883.10.20.17.2.5]
The patient data section in the NCR contains data collected during a neonatal intensive
care unit (NICU) inpatient stay. This section contains data that could be used in
endorsed quality measures, and it may inform the creation of NICU quality measures. It
contains significant basic data about the infant's birth and two subsections: an
encounter section and an acuity assessment section.
1. Conforms to Patient data section Template (templateId:
2.16.840.1.113883.10.20.17.2.4).
2. SHALL contain [1..1] templateId/@root="2.16.840.1.113883.10.20.17.2.5"
(CONF:4134).
3. SHALL contain [1..1] entry (CONF:4135) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4136).
b. SHALL contain [1..1] Encounters section - NCR
(templateId:2.16.840.1.113883.10.20.17.2.2) (CONF:4137).
4. SHALL contain [1..1] entry (CONF:4138) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4139).
b. SHALL contain [1..1] Acuity score data section
(templateId:2.16.840.1.113883.10.20.17.2.3) (CONF:4140).
5. SHALL contain [1..1] entry (CONF:4144) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4145).
b. SHALL contain [1..1] Birth weight
(templateId:2.16.840.1.113883.10.20.17.3.1) (CONF:4146).
6. SHALL contain [1..1] entry (CONF:4147) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4148).
b. SHALL contain [1..1] Birth head circumference
(templateId:2.16.840.1.113883.10.20.17.3.2) (CONF:4149).
7. SHALL contain [1..1] entry (CONF:4150) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4151).
b. SHALL contain [1..1] Gestational age
(templateId:2.16.840.1.113883.10.20.17.3.3) (CONF:4152).
8. SHALL contain [1..1] entry (CONF:4153) such that it
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 25
January 2010
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4154).
b. SHALL contain [1..1] Apgar at 1 minute
(templateId:2.16.840.1.113883.10.20.17.3.4) (CONF:4155).
9. SHALL contain [1..1] entry (CONF:4156) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4157).
b. SHALL contain [1..1] Apgar at 5 minute
(templateId:2.16.840.1.113883.10.20.17.3.5) (CONF:4158).
10. MAY contain [0..*] entry (CONF:4159) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4160).
b. SHALL contain [1..1] Apgar score prolonged
(templateId:2.16.840.1.113883.10.20.17.3.6) (CONF:4161).
11. SHALL contain [1..1] entry (CONF:4162) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:4163).
b. SHALL contain [1..1] Inborn/outborn
(templateId:2.16.840.1.113883.10.20.17.3.7) (CONF:4164).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 26
January 2010
Figure 8: NCR patient data section example
<component>
<section>
<templateId root="2.16.840.1.113883.10.20.17.2.4" />
<templateId root="2.16.840.1.113883.10.20.17.2.5" />
<code code="55188-7" codeSystem="2.16.840.1.113883.6.1" />
<title>Patient Data</title>
<text>
...
</text>
<entry typeCode="DRIV">
<observation ...
<templateId root="2.16.840.1.113883.10.20.17.3.1" />
<code code="47340003" codeSystem="2.16.840.1.113883.6.96"
displayName="Birth weight" />
...
<entry typeCode="DRIV">
<observation ...
<templateId root="2.16.840.1.113883.10.20.17.3.3" />
<code code="268477000" codeSystem="2.16.840.1.113883.6.96"
displayName="Gestational age at birth" />
...
<component>
<section>
...
<title>Encounters</title>
...
<component>
<section>
...
<title>Patient Data</title>
...
</section>
</component>
</section>
</component>
3.5 Reporting parameters section
[section: templateId 2.16.840.1.113883.10.20.17.2.1]
The reporting parameters section provides information about the reporting time
interval, and may contain other information that provides context for the patient data
being reported. The receiving organization may tell the reporting hospitals what
information they want in this section.
1. SHALL contain [1..1] code/@code="55187-9" Reporting Parameters (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:4141).
2. SHALL contain [1..1] title="Reporting Parameters" (CONF:4142).
3. SHALL contain [1..1] text (CONF:4143).
4. SHALL contain [1..1] templateId/@root="2.16.840.1.113883.10.20.17.2.1"
(CONF:3276).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 27
January 2010
5. SHALL contain [1..1] entry (CONF:3277) such that it
a. SHALL contain [1..1] @typeCode="DRIV" Is derived from (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3278).
b. SHALL contain [1..1] Reporting parameters act
(templateId:2.16.840.1.113883.10.20.17.3.8) (CONF:3279).
Figure 9: Reporting parameters section example
<section>
<templateId root="2.16.840.1.113883.10.20.17.2.1" />
<code code="55187-9" codeSystem="2.16.840.1.113883.6.1" />
<title>Reporting Parameters</title>
<text>
...
</text>
<entry typeCode="DRIV">
<act classCode="ACT" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.17.3.8" />
...
</act>
</entry>
</section>
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 28
January 2010
4 CLINICAL STATEMENT TEMPLATES
4.1 Acuity indicator data generic organizer
[organizer: templateId 2.16.840.1.113883.10.20.17.3.59]
This template contains a collection of templates representing data elements whose
variants are thought to be significant indicators of the severity of illness and of
subsequent infant outcomes. Please navigate to the contained template to see its
complete definition. For example, go to Oxygen administration
(2.16.840.1.113883.10.20.17.3.17) to see the oxygen administration template
representation including the recommended codes and terms. The use of SHALL requires
that the component be valued with a member from the cited value set; however, in every
case any HL7 "null" value such as other (OTH) or unknown (UNK) may be used.
1. SHALL contain [1..1] @classCode="CLUSTER" Cluster (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:4113).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:4114).
3. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:4115).
4. SHALL contain [2..2] component (CONF:3964) such that it
a. SHALL contain [1..1] Arterial PaO2 Observation
(templateId:2.16.840.1.113883.10.20.17.3.16) (CONF:3965).
5. SHALL contain [2..2] component (CONF:3966) such that it
a. SHALL contain [1..1] Oxygen Administration
(templateId:2.16.840.1.113883.10.20.17.3.17) (CONF:3967).
6. SHALL contain [1..1] component (CONF:3968) such that it
a. SHALL contain [1..1] PaO2/FIO2 ratio
(templateId:2.16.840.1.113883.10.20.17.3.18) (CONF:3969).
7. SHALL contain [2..2] component (CONF:3975) such that it
a. SHALL contain [1..1] Mean airway pressure
(templateId:2.16.840.1.113883.10.20.17.3.19) (CONF:3976).
8. SHALL contain [2..2] component (CONF:3977) such that it
a. SHALL contain [1..1] PaCO2 Observation
(templateId:2.16.840.1.113883.10.20.17.3.20) (CONF:3978).
9. SHALL contain [2..2] component (CONF:3979) such that it
a. SHALL contain [1..1] Respiratory rate
(templateId:2.16.840.1.113883.10.20.17.3.21) (CONF:3980).
10. SHALL contain [1..1] component (CONF:3981) such that it
a. SHALL contain [1..1] Oxygenation index
(templateId:2.16.840.1.113883.10.20.17.3.22) (CONF:3982).
11. SHALL contain [1..1] component (CONF:3983) such that it
a. SHALL contain [1..1] Respiratory Severity Score
(templateId:2.16.840.1.113883.10.20.17.3.23) (CONF:3984).
12. SHALL contain [1..1] component (CONF:3985) such that it
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 29
January 2010
a. SHALL contain [1..1] Nitric oxide administration
(templateId:2.16.840.1.113883.10.20.17.3.24) (CONF:3986).
13. SHALL contain [1..1] component (CONF:3987) such that it
a. SHALL contain [1..1] Respiratory or ventilatory support
(templateId:2.16.840.1.113883.10.20.17.3.25) (CONF:3988).
14. SHALL contain [2..2] component (CONF:3989) such that it
a. SHALL contain [1..1] Body temperature
(templateId:2.16.840.1.113883.10.20.17.3.10) (CONF:3990).
15. SHALL contain [2..2] component (CONF:3991) such that it
a. SHALL contain [1..1] Mean blood pressure
(templateId:2.16.840.1.113883.10.20.17.3.26) (CONF:3992).
16. SHALL contain [2..2] component (CONF:3993) such that it
a. SHALL contain [1..1] Systolic blood pressure
(templateId:2.16.840.1.113883.10.20.17.3.27) (CONF:3994).
17. SHALL contain [2..2] component (CONF:3995) such that it
a. SHALL contain [1..1] Diastolic blood pressure
(templateId:2.16.840.1.113883.10.20.17.3.28) (CONF:3996).
18. SHALL contain [2..2] component (CONF:3997) such that it
a. SHALL contain [1..1] Heart rate
(templateId:2.16.840.1.113883.10.20.17.3.29) (CONF:3998).
19. SHALL contain [2..2] component (CONF:3999) such that it
a. SHALL contain [1..1] Blood pH
(templateId:2.16.840.1.113883.10.20.17.3.30) (CONF:4000).
20. SHOULD contain [0..2] component (CONF:4001) such that it
a. SHALL contain [1..1] Blood gas base excess
(templateId:2.16.840.1.113883.10.20.17.3.31) (CONF:4002).
21. SHOULD contain [0..2] component (CONF:4003) such that it
a. SHALL contain [1..1] Blood gas base deficit
(templateId:2.16.840.1.113883.10.20.17.3.32) (CONF:4004).
22. There SHALL only be 2 total results from base excess
(templateId:2.16.840.1.113883.10.20.17.3.31) or base deficit
(templateId:2.16.840.1.113883.10.20.17.3.32) (CONF:4005).
23. SHALL contain [1..1] component (CONF:4006) such that it
a. SHALL contain [1..1] Lactic acid from serum/plasma
(templateId:2.16.840.1.113883.10.20.17.3.33) (CONF:4007).
24. SHALL contain [1..1] component (CONF:4008) such that it
a. SHALL contain [1..1] Calcium ionized
(templateId:2.16.840.1.113883.10.20.17.3.34) (CONF:4009).
25. SHALL contain [1..1] component (CONF:4010) such that it
a. SHALL contain [1..1] Calcium total serum
(templateId:2.16.840.1.113883.10.20.17.3.35) (CONF:4011).
26. SHALL contain [2..2] component (CONF:4012) such that it
a. SHALL contain [1..1] Sodium serum
(templateId:2.16.840.1.113883.10.20.17.3.36) (CONF:4013).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 30
January 2010
27. SHALL contain [1..1] component (CONF:4049) such that it
a. SHALL contain [1..1] Seizures
(templateId:2.16.840.1.113883.10.20.17.3.54) (CONF:4050).
28. SHALL contain [2..2] component (CONF:4033) such that it
a. SHALL contain [1..1] Hemoglobin
(templateId:2.16.840.1.113883.10.20.17.3.46) (CONF:4034).
29. SHALL contain [2..2] component (CONF:4035) such that it
a. SHALL contain [1..1] Blood urea nitrogen (BUN)
(templateId:2.16.840.1.113883.10.20.17.3.47) (CONF:4036).
30. SHALL contain [1..1] component (CONF:4037) such that it
a. SHALL contain [1..1] Creatinine observation
(templateId:2.16.840.1.113883.10.20.17.3.48) (CONF:4038).
31. SHALL contain [1..1] component (CONF:4039) such that it
a. SHALL contain [1..1] Aspartate aminotransferase (AST)
(templateId:2.16.840.1.113883.10.20.17.3.49) (CONF:4040).
32. SHALL contain [1..1] component (CONF:4041) such that it
a. SHALL contain [1..1] Alanine aminotransferase (ALT)
(templateId:2.16.840.1.113883.10.20.17.3.50) (CONF:4042).
33. SHALL contain [1..1] component (CONF:4043) such that it
a. SHALL contain [1..1] Bilirubin, total
(templateId:2.16.840.1.113883.10.20.17.3.51) (CONF:4044).
34. SHALL contain [1..1] component (CONF:4031) such that it
a. SHALL contain [1..1] International normalized ratio (INR)
(templateId:2.16.840.1.113883.10.20.17.3.45) (CONF:4032).
35. SHALL contain [1..1] component (CONF:4047) such that it
a. SHALL contain [1..1] Albumin observation
(templateId:2.16.840.1.113883.10.20.17.3.53) (CONF:4048).
36. SHALL contain [1..1] component (CONF:4029) such that it
a. SHALL contain [1..1] Activated partial thromboplastin time
(templateId:2.16.840.1.113883.10.20.17.3.44) (CONF:4030).
37. SHALL contain [1..1] component (CONF:4051) such that it
a. SHALL contain [1..1] Urine output
(templateId:2.16.840.1.113883.10.20.17.3.55) (CONF:4052).
38. SHALL contain [1..1] component (CONF:4045) such that it
a. SHALL contain [1..1] Bilirubin, conjugated
(templateId:2.16.840.1.113883.10.20.17.3.52) (CONF:4046).
39. SHALL contain [2..2] component (CONF:4021) such that it
a. SHALL contain [1..1] White blood cell (leukocytes)
(templateId:2.16.840.1.113883.10.20.17.3.40) (CONF:4022).
40. SHALL contain [2..2] component (CONF:4015) such that it
a. SHALL contain [1..1] Potassium serum
(templateId:2.16.840.1.113883.10.20.17.3.37) (CONF:4016).
41. SHALL contain [2..2] component (CONF:4017) such that it
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 31
January 2010
a. SHALL contain [1..1] Bicarbonate serum
(templateId:2.16.840.1.113883.10.20.17.3.38) (CONF:4018).
42. SHALL contain [1..1] component (CONF:4025) such that it
a. SHALL contain [1..1] Fibrinogen level
(templateId:2.16.840.1.113883.10.20.17.3.42) (CONF:4026).
43. SHALL contain [2..2] component (CONF:4019) such that it
a. SHALL contain [1..1] Glucose serum
(templateId:2.16.840.1.113883.10.20.17.3.39) (CONF:4020).
44. SHALL contain [1..1] component (CONF:4023) such that it
a. SHALL contain [1..1] Platelets
(templateId:2.16.840.1.113883.10.20.17.3.41) (CONF:4024).
45. SHALL contain [1..1] component (CONF:4027) such that it
a. SHALL contain [1..1] Prothrombin time (PT)
(templateId:2.16.840.1.113883.10.20.17.3.43) (CONF:4028).
46. SHALL contain [1..1] component (CONF:4053) such that it
a. SHALL contain [1..1] Nothing by mouth (NPO)
(templateId:2.16.840.1.113883.10.20.17.3.56) (CONF:4054).
47. SHALL contain [1..1] component (CONF:4055) such that it
a. SHALL contain [1..1] Renal dialysis (renal replacement therapy)
(templateId:2.16.840.1.113883.10.20.17.3.57) (CONF:4056).
48. SHALL contain [1..1] component (CONF:4057) such that it
a. SHALL contain [1..1] Steroid treatment (systemic)
(templateId:2.16.840.1.113883.10.20.17.3.58) (CONF:4058).
4.2 Acuity data time organizer - admission to 12 hours
[organizer: templateId 2.16.840.1.113883.10.20.17.3.60]
This organizer template groups the observations, findings, or values in the Acuity
indicator data generic organizer (templateId 2.16.840.1.113883.10.20.17.3.59)
into the time period from the admission through the first 12 hours of the admission.
1. Conforms to Acuity indicator data generic organizer Template (templateId:
2.16.840.1.113883.10.20.17.3.59).
2. SHALL contain [1..1] @classCode="CLUSTER" Cluster (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:4059).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:4060).
4. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:4061).
5. SHALL contain [1..1] effectiveTime/low (CONF:4062).
a. This effectiveTime/low SHALL be equal to the admission time and SHALL be
accurate at least to the hour (CONF:4064).
6. SHALL contain [1..1] effectiveTime/high (CONF:4063).
a. This effectiveTime/high SHALL be equal to the admission time plus 12 hours
and SHALL be accurate at least to the hour (CONF:4065).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 32
January 2010
4.3 Acuity data time organizer - day 3
[organizer: templateId 2.16.840.1.113883.10.20.17.3.61]
This organizer template groups the observations, findings, or values in the Acuity
indicator data generic organizer (templateId 2.16.840.1.113883.10.20.17.3.59)
into the time period of the third day of the admission.
1. Conforms to Acuity indicator data generic organizer Template (templateId:
2.16.840.1.113883.10.20.17.3.59).
2. SHALL contain [1..1] @classCode="CLUSTER" Cluster (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:4116).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:4117).
4. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:4118).
5. SHALL contain [1..1] effectiveTime/low (CONF:4119).
a. This effectiveTime/low day SHALL equal the third day after the day of
admission and the minute SHALL equal 0001 (CONF:4120).
6. SHALL contain [1..1] effectiveTime/high (CONF:4121).
a. This effectiveTime/high day SHALL equal the third day after the day of
admission and the minute SHALL equal to 2359 (CONF:4122).
4.4 Acuity data time organizer - day 7
[organizer: templateId 2.16.840.1.113883.10.20.17.3.62]
This organizer template groups the observations, findings, or values in the Acuity
indicator data generic organizer (templateId 2.16.840.1.113883.10.20.17.3.59)
into the time period of the seventh day of the admission.
1. Conforms to Acuity indicator data generic organizer Template (templateId:
2.16.840.1.113883.10.20.17.3.59).
2. SHALL contain [1..1] @classCode="CLUSTER" Cluster (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:4123).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:4124).
4. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:4125).
5. SHALL contain [1..1] effectiveTime/low (CONF:4126).
a. This effectiveTime/low day SHALL equal the seventh day after the day of
admission and the minute SHALL equal to 0001 (CONF:4127).
6. SHALL contain [1..1] effectiveTime/high (CONF:4128).
a. This effectiveTime/high day SHALL equal the seventh day after the day of
admission and the minute SHALL equal to 2359 (CONF:4129).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 33
January 2010
4.5 Admission activity – neonatal
[act: templateId 2.16.840.1.113883.10.20.17.3.12]
This admission act contains admission-related observation templates for body
temperature and body weight.
1. SHALL contain [1..1] @classCode="ACT" (CodeSystem: 2.16.840.1.113883.5.6
HL7ActClass) STATIC (CONF:3298).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3299).
3. SHALL contain [1..1] code/@code="305056002" Admission procedure (CodeSystem:
2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3301).
4. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3302).
5. SHALL contain [1..1] entryRelationship (CONF:3306) such that it
a. SHALL contain [1..1] @typeCode="COMP" Refers to (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3304).
b. SHALL contain [1..1] Body temperature
(templateId:2.16.840.1.113883.10.20.17.3.10) (CONF:3305).
6. SHALL contain [1..1] entryRelationship (CONF:3303) such that it
a. SHALL contain [1..1] @typeCode="COMP" Refers to (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3307).
b. SHALL contain [1..1] Body weight
(templateId:2.16.840.1.113883.10.20.17.3.11) (CONF:3308).
Figure 10: Admission activity act example
<!-- Admission Act -->
<act classCode="ACT" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.17.3.12" />
<code code="305056002" codeSystem="2.16.840.1.113883.6.96"
displayName="Admission procedure" />
<statusCode code="completed" />
<entryRelationship typeCode="COMP">
<observation classCode="OBS" moodCode="EVN">
...
</observation>
</entryRelationship>
<entryRelationship typeCode="COMP">
<observation classCode="OBS" moodCode="EVN">
...
</observation>
</entryRelationship>
</act>
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 34
January 2010
4.6 CCD Encounter activity
[encounter: templateId 2.16.840.1.113883.10.20.1.21]
This clinical statement represents the details of an encounter.
1. The value for "Encounter / @classCode" in an encounter activity SHALL be "ENC"
2.16.840.1.113883.5.6 ActClass STATIC. (CONF:577).
2. The value for "Encounter / @moodCode" in an encounter activity SHALL be "EVN"
2.16.840.1.113883.5.1001 ActMood STATIC. (CONF:578).
3. An encounter activity SHALL contain at least one Encounter / id. (CONF:579).
4. An encounter activity SHOULD contain exactly one Encounter / code. (CONF:580).
5. The value for "Encounter / code" in an encounter activity SHOULD be selected from
ValueSet 2.16.840.1.113883.1.11.13955 EncounterCode 2.16.840.1.113883.5.4
ActCode DYNAMIC. (CONF:581).
6. An encounter activity MAY contain exactly one Encounter / effectiveTime, to
indicate date, time, and/or duration of an encounter. (CONF:582).
7. An encounter activity MAY contain one or more Encounter / entryRelationship,
whose value for "entryRelationship / @typeCode" SHALL be "RSON" "Has reason"
2.16.840.1.113883.5.1002 ActRelationshipType STATIC, where the target of the
relationship represents the indication for the activity. (CONF:583).
8. An encounter activity MAY contain one or more Encounter / performer, used to
define the practioners involved in an encounter. (CONF:584).
9. Encounter / performer MAY contain exactly one Encounter / performer /
assignedEntity / code, to define the role of the practioner. (CONF:585).
10. An encounter activity MAY contain one or more patient instructions (templateId
2.16.840.1.113883.10.20.1.49). (CONF:586).
11. The value for "Encounter / entryRelationship / @typeCode" in an encounter activity
MAY be "SUBJ" "Subject" 2.16.840.1.113883.5.1002 ActRelationshipType STATIC to
reference an age observation (templateId 2.16.840.1.113883.10.20.1.38).
(CONF:587).
12. An encounter activity SHALL contain one or more sources of information, as defined
in section 5.2 Source. (CONF:588).
13. An encounter activity MAY contain one or more location participations (templateId
2.16.840.1.113883.10.20.1.45). (CONF:589).
4.6.1 Neonatal ICU encounter activity
[encounter: templateId 2.16.840.1.113883.10.20.17.3.15]
The neonatal ICU encounter contains selected data specific to each admission and
discharge in an encounter. This template captures data for the current encounter being
reported and may capture data from historical encounters.
1. Conforms to CCD Encounter activity Template (templateId:
2.16.840.1.113883.10.20.1.21).
2. SHALL contain [1..1] @classCode="ENC" Encounter (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3323).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3324).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 35
January 2010
4. SHALL contain [1..*] id (CONF:3325).
a. The encounter that is the same encounter as the encompassingEncounter
SHALL contain an encounter/id that equals the encompassingEncounter id
(CONF:3330).
5. SHALL contain [1..1] code/@code="IMP" Inpatient encounter (CodeSystem:
2.16.840.1.113883.5.4 HL7ActCode) STATIC (CONF:3327).
6. SHOULD contain [0..1] effectiveTime/low (CONF:3329).
7. SHOULD contain [0..1] effectiveTime/high (CONF:3328).
8. SHALL contain [1..1] participant (CONF:3775).
a. This participant SHALL contain [1..1] @typeCode="LOC" (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3776).
b. This participant SHALL contain [1..1] Neonatal ICU location
(templateId:2.16.840.1.113883.10.20.17.3.14) (CONF:3777).
9. SHALL contain [1..1] entryRelationship (CONF:3331) such that it
a. SHALL contain [1..1] @typeCode="COMP" Component (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3332).
b. SHALL contain [1..1] Admission activity - neonatal
(templateId:2.16.840.1.113883.10.20.17.3.12) (CONF:3333).
10. SHALL contain [1..1] entryRelationship (CONF:3334) such that it
a. SHALL contain [1..1] @typeCode="COMP" Component (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3335).
b. SHALL contain [1..1] Discharge activity - Neonatal
(templateId:2.16.840.1.113883.10.20.17.3.13) (CONF:3336).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 36
January 2010
Figure 11: Neonatal ICU encounter example
<encounter classCode="ENC" moodCode="EVN">
<!-- CCD Encounter activity template -->
<templateId root="2.16.840.1.113883.10.20.1.21" />
<!-- Neonatal ICU encounter activity -->
<templateId root="2.16.840.1.113883.10.20.17.3.15" />
<id extension="IN302902" root="1.1.2" />
<!-- same as encompassing encounterID -->
<code code="IMP" codeSystem="2.16.840.1.113883.5.4"
displayName="Inpatient encounter" />
<effectiveTime>
<low value="200903031600" />
<high value="20090625" />
</effectiveTime>
<!-- CCD Location participation template -->
<participant typeCode="LOC">
<templateId root="2.16.840.1.113883.10.20.1.45" />
<templateId root="2.16.840.1.113883.10.20.17.3.14" />
<participantRole classCode="SDLOC">
<code code="PEDNICU" codeSystem="2.16.840.1.113883.5.111"
displayName="Neonatal ICU" />
</participantRole>
</participant>
<entryRelationship typeCode="COMP">
...
</entryRelationship>
</encounter>
4.7 CCD Medication activity
[substanceAdministration: templateId 2.16.840.1.113883.10.20.1.24]
A medication activity is used to describe what is administered. Reconciliation of
conflicting medication information from various sources is enabled both by indicating
the source of information and by indicating whether the source is reporting intended or
actual medication use. For instance, a physician may intend for a patient to be on a
particular dose, but the patient may actually be taking a different dose; a pharmacy
may fill a prescription for a particular dose only to then have the patient's physician
lower the dose without notifying the pharmacy. Therefore, medication and supply
activities can be expressed in either the "EVN" (event) mood or the "INT" (intent) mood.
Medication activities in "INT" mood are not orders, but rather are reflections of what a
clinician intends a patient to be taking. Medication activities in "EVN" mood reflect
actual use. A pharmacy system will typically report what was actually filled, along with
intended use. A physician will often report intended use. A patient or family member
will typically report actual use.
1. The value for "SubstanceAdministration / @moodCode" in a medication activity
SHALL be "EVN" or "INT" 2.16.840.1.113883.5.1001 ActMood STATIC. (CONF:1013).
2. A medication activity SHALL contain at least one SubstanceAdministration / id.
(CONF:1014).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 37
January 2010
3. A medication activity SHOULD contain exactly one SubstanceAdministration /
statusCode. (CONF:1015).
4. A medication activity SHOULD contain one or more SubstanceAdministration /
effectiveTime elements, used to indicate the actual or intended start and stop date of
a medication, and the frequency of administration. (See section 5.4.1 Dates and
Times for additional details about time representation). (CONF:1016).
5. A medication activity SHOULD contain exactly one SubstanceAdministration /
routeCode. (CONF:1017).
6. The value for "SubstanceAdministration / routeCode" in a medication activity
SHOULD be selected from the HL7 RouteOfAdministration
(2.16.840.1.113883.5.112) code system. (CONF:1018).
7. A medication activity SHOULD contain exactly one SubstanceAdministration /
doseQuantity or SubstanceAdministration / rateQuantity. (CONF:1019).
8. A medication activity MAY contain exactly one SubstanceAdministration /
maxDoseQuantity, which represents a maximum dose limit. (CONF:1020).
9. A medication activity MAY contain one or more SubstanceAdministration /
performer, to indicate the person administering a substance. (CONF:1021).
10. A medication activity MAY have one or more associated consents, represented in the
CCD Header as ClinicalDocument / authorization / consent. (CONF:1022).
11. A medication activity SHALL contain one or more sources of information, as defined
in section 5.2 Source. (CONF:1023).
12. A medication activity MAY contain exactly one medication status observation.
(CONF:1024).
13. A medication activity SHALL contain exactly one SubstanceAdministration /
consumable, the target of which is a product template (CONF:1051).
14. A medication activity MAY contain exactly one medication series number
observation. (CONF:2019).
4.7.1 Nitric oxide administration
[substanceAdministration: templateId 2.16.840.1.113883.10.20.17.3.24]
This template represents inhaled nitric oxide administered to a patient in parts per
million. This guide uses route codes from the HITSP-endorsed Medication Route FDA
Value Set.
1. Conforms to CCD Medication activity Template (templateId:
2.16.840.1.113883.10.20.1.24).
2. SHALL contain [1..1] @classCode="SBADM" Substance administration
(CodeSystem: 2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3414).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3415).
4. SHALL contain [1..1] statusCode (CONF:3416).
5. SHOULD contain [0..1] effectiveTime (CONF:3417).
6. SHALL contain [1..1] routeCode/@code="C38216" RESPIRATORY (INHALATION)
(CodeSystem: 2.16.840.1.113883.3.26.1.1 FDA RouteOfAdministration)
STATIC (CONF:3418).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 38
January 2010
7. SHALL contain [1..1] doseQuantity (CONF:3419).
8. SHALL contain [1..1] value (CONF:3420).
a. This value SHALL contain [1..1] @unit="%" percent (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3421).
9. SHALL contain [1..1] consumable (CONF:3422).
a. This consumable SHALL contain [1..1] manufacturedProduct (CONF:3423).
i.
This manufacturedProduct SHALL contain [1..1]
manufacturedMaterial (CONF:3424).
1. This manufacturedMaterial SHALL contain [1..1]
code/@code="562851" Nitric Oxide / Nitrogen Gas for
Inhalation (CodeSystem: 2.16.840.1.113883.6.88
RxNorm) STATIC (CONF:3425).
a. This code SHOULD contain [0..1] originalText
(CONF:3426).
Figure 12: Nitric oxide administration example
<!-- Nitric Oxide Administration -->
<substanceAdministration classCode="SBADM" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.1.24" />
<!-- CCD Medication activity template -->
<templateId root="2.16.840.1.113883.10.20.17.3.24" />
<id root="cdbd5b05-6cde-11db-9fe1-0800200c9a66" />
<statusCode code="completed" />
<effectiveTime value="200903032300" />
<routeCode code="C38216" codeSystem="2.16.840.1.113883.3.26.1.1"
displayName="RESPIRATORY (INHALATION)"
codeSystemName="FDA RouteOfAdministration" />
<doseQuantity value="20" unit="ppm" />
<consumable>
<manufacturedProduct>
<templateId root="2.16.840.1.113883.10.20.1.53" />
<!-- CCD Product template -->
<manufacturedMaterial>
<code code="562851" codeSystem="2.16.840.1.113883.6.88"
displayName=" Nitric Oxide/Nitrogen Gas for Inhalation">
<originalText>Nitric Oxide</originalText>
</code>
</manufacturedMaterial>
</manufacturedProduct>
</consumable>
</substanceAdministration>
4.7.2 Oxygen administration
[substanceAdministration: templateId 2.16.840.1.113883.10.20.17.3.17]
This template represents the percent or fraction of inspired oxygen administered to a
patient. This guide uses route codes from the HITSP-endorsed Medication Route FDA
Value Set.
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 39
January 2010
1. Conforms to CCD Medication activity Template (templateId:
2.16.840.1.113883.10.20.1.24).
2. SHALL contain [1..1] @classCode="SBADM" Substance administration
(CodeSystem: 2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3357).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3358).
4. SHALL contain [1..1] statusCode (CONF:3360).
5. SHOULD contain [0..1] effectiveTime (CONF:3361).
6. SHALL contain [1..1] routeCode/@code="C38216" RESPIRATORY (INHALATION)
(CodeSystem: 2.16.840.1.113883.3.26.1.1 FDA RouteOfAdministration)
STATIC (CONF:3363).
7. SHALL contain [1..1] doseQuantity (CONF:3369).
8. SHALL contain [1..1] value (CONF:3370).
a. This value SHALL contain [1..1] @unit="%" percent (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3371).
9. SHALL contain [1..1] consumable (CONF:3364).
a. This consumable SHALL contain [1..1] manufacturedProduct (CONF:3365).
i.
This manufacturedProduct SHALL contain [1..1]
manufacturedMaterial (CONF:3366).
1. This manufacturedMaterial SHALL contain [1..1]
code/@code="7806" Oxygen (CodeSystem:
2.16.840.1.113883.6.88 RxNorm) STATIC (CONF:3367).
a. This code SHOULD contain [0..1] originalText
(CONF:3368).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 40
January 2010
Figure 13: Oxygen administration example
<substanceAdministration classCode="SBADM" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.1.24" />
<!-- CCD Medication activity template -->
<templateId root="2.16.840.1.113883.10.20.17.3.17" />
<id root="cdbd5b05-6cde-11db-9fe1-0800200c9a68" />
<statusCode code="completed" />
<effectiveTime value="200903031607" />
<routeCode code="C38216" codeSystem="2.16.840.1.113883.3.26.1.1"
displayName="RESPIRATORY (INHALATION)"
codeSystemName="FDA RouteOfAdministration" />
<doseQuantity value="80" unit="%" />
<consumable>
<manufacturedProduct>
<manufacturedMaterial>
<code code="7806" codeSystem="2.16.840.1.113883.6.88"
codeSystemName="RxNorm" displayName="Oxygen">
<originalText>Oxygen</originalText>
</code>
</manufacturedMaterial>
</manufacturedProduct>
</consumable>
</substanceAdministration>
4.8 CCD Result observation
[observation: templateId 2.16.840.1.113883.10.20.1.31]
This clinical statement represents details of a lab, radiology, or other study performed
on a patient.
1. The value for "Observation / @moodCode" in a result observation SHALL be "EVN"
2.16.840.1.113883.5.1001 ActMood STATIC. (CONF:800).
2. A result observation SHALL contain at least one Observation / id. (CONF:801).
3. A result observation SHALL contain exactly one Observation / statusCode.
(CONF:802).
4. A result observation SHOULD contain exactly one Observation / effectiveTime,
which represents the biologically relevant time (e.g. time the specimen was obtained
from the patient). (CONF:803).
5. A result observation SHALL contain exactly one Observation / code. (CONF:804).
6. The value for "Observation / code" in a result observation SHOULD be selected from
LOINC (codeSystem 2.16.840.1.113883.6.1) or SNOMED CT (codeSystem
2.16.840.1.113883.6.96), and MAY be selected from CPT-4 (codeSystem
2.16.840.1.113883.6.12). (CONF:805).
7. A result observation MAY contain exactly one Observation / methodCode if the
method isn't inherent in Observation / code or if there is a need to further specialize
the method in Observation / code. (CONF:806).
8. Observation / methodCode SHALL NOT conflict with the method inherent in
Observation / code. (CONF:807).
9. A result observation SHALL contain exactly one Observation / value. (CONF:808).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 41
January 2010
10. Where Observation / value is a physical quantity, the unit of measure SHALL be
expressed using a valid Unified Code for Units of Measure (UCUM) expression.
(CONF:809).
11. A result observation SHOULD contain exactly one Observation / interpretationCode,
which can be used to provide a rough qualitative interpretation of the observation,
such as "N" (normal), "L" (low), "S" (susceptible), etc. Interpretation is generally
provided for numeric results where an interpretation range has been defined, or for
antimicrobial susceptibility test interpretation. (CONF:810).
12. A result observation SHOULD contain one or more Observation / referenceRange to
show the normal range of values for the observation result. (CONF:811).
4.8.1 CDA XML patterns conforming to CCD Result observation
The subsections below describe additional constraints that conform to the CCD Result
observation template. Most of these result observations use the following pattern.
Figure 14: Typical laboratory pattern for CCD-result observation conforming templates
<observation classCode="OBS" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.1.31" />
<!-- CCD Result observation template -->
<templateId root="2.16.840.1.113883.10.20.17.3.44" />
<id nullFlavor="NI" />
<code code="14979-9" codeSystem="2.16.840.1.113883.6.1"
displayName="Coagulation surface induced Time PPP" />
<statusCode code="completed" />
<effectiveTime value="200903031800" />
<value xsi:type="PQ" value="33" unit="s" />
</observation>
Non-laboratory NCR templates such as Birth weight or Gestational age at birth that
conform to the CCD Result observation template do not include the effectiveTime
element that is usually present in a lab result.
Figure 15: Typical non-laboratory pattern for CCD-result observation conforming
templates
<observation classCode="OBS" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.1.31" />
<!-- CCD Result observation template -->
<templateId root="2.16.840.1.113883.10.20.17.3.3" />
<code code="268477000" codeSystem="2.16.840.1.113883.6.96"
displayName="Gestational age at birth" />
<statusCode code="completed" />
<value xsi:type="PQ" value="185" unit="d" />
</observation>
The Arterial PaO2 observation requires a specimen element to represent the specimen
type. The Blood gas base deficit, Blood gas base excess, and Blood gas pH observations
may optionally follow this pattern to show specimen type.
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 42
January 2010
Figure 16: Specimen type pattern for CCD-result observation conforming templates
<!-- Arterial PaO2 Observation -->
<observation classCode="OBS" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.1.31" />
<!-- CCD Result observation template -->
<templateId root="2.16.840.1.113883.10.20.17.3.16" />
<id nullFlavor="NI" />
<code code="11556-8" codeSystem="2.16.840.1.113883.6.1"
displayName="Oxygen PPres Bld" />
<statusCode code="completed" />
<effectiveTime value="200903031607" />
<value xsi:type="PQ" value="55" unit="mm[Hg]" />
<specimen>
<specimenRole>
<id root="d5a9ef50-d05e-11dd-ad8b-0800200c9a66" />
<specimenPlayingEntity>
<code code="122552005" codeSystem="2.16.840.1.113883.6.96"
displayName="Arterial blood specimen" />
<!-- Specimen type -->
</specimenPlayingEntity>
</specimenRole>
</specimen>
</observation>
4.8.2 Activated partial thromboplastin time
[observation: templateId 2.16.840.1.113883.10.20.17.3.44]
This observation represents an activated partial thromboplastin time result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3605).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3606).
4. SHALL contain [1..1] code/@code="14979-9" Coagulation surface induced Time
PPP (CodeSystem: 2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3607).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3608).
6. SHALL contain [1..1] value (CONF:3609).
a. This value SHALL contain [1..1] @unit="s" seconds (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3610).
4.8.3 Alanine aminotransferase (ALT)
[observation: templateId 2.16.840.1.113883.10.20.17.3.50]
This observation represents an alanine aminotransferase (ALT) result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 43
January 2010
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3653).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3654).
4. SHALL contain [1..1] code/@code="1742-6" Alanine aminotransferase Ser/Plas
(CodeSystem: 2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3655).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3656).
6. SHALL contain [1..1] value (CONF:3657).
a. This value SHALL contain [1..1] @unit="U/L" Units per liter (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3658).
4.8.4 Albumin observation
[observation: templateId 2.16.840.1.113883.10.20.17.3.53]
This observation represents an albumin result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3671).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3672).
4. SHALL contain [1..*] id (CONF:3673).
5. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.11 Albumin DYNAMIC (CONF:3674).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3675).
7. SHOULD contain [0..1] effectiveTime (CONF:3676).
8. SHALL contain [1..1] value (CONF:3677).
a. This value SHALL contain [1..1] @unit="mg/dL" Milligrams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3678).
4.8.5 Apgar at 1 minute
[observation: templateId 2.16.840.1.113883.10.20.17.3.4]
This observation represents the apgar score assigned to a neonate at 1 minute after
birth.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3244).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3245).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.16 Apgar 1 minute post birth DYNAMIC
(CONF:3246).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 44
January 2010
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3247).
6. MAY contain [0..1] effectiveTime (CONF:3255).
7. SHALL contain [1..1] value (CONF:3248).
4.8.6 Apgar at 5 minutes
[observation: templateId 2.16.840.1.113883.10.20.17.3.5]
This observation represents the apgar score assigned to a neonate at 5 minutes after
birth.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3249).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3250).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.17 Apgar 5 minutes post birth DYNAMIC
(CONF:3251).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3252).
6. MAY contain [0..1] effectiveTime (CONF:3254).
7. SHALL contain [1..1] value (CONF:3253).
4.8.7 Apgar score prolonged
[observation: templateId 2.16.840.1.113883.10.20.17.3.6]
This observation represents the apgar score assigned to a neonate after 5 minutes after
birth. Typically, neonates are assigned additional apgar scores at 10, 15, and 20
minutes until the total score is 7 or greater.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3256).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3257).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.1 Apgar Summary Score (prolonged) DYNAMIC
(CONF:3258).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3259).
6. MAY contain [0..1] effectiveTime (CONF:3260).
7. SHALL contain [1..1] value (CONF:3261).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 45
January 2010
4.8.8 Arterial PaO2 Observation
[observation: templateId 2.16.840.1.113883.10.20.17.3.16]
This observation represents a PaO2 (Arterial tension of oxygen) result from an arterial
blood sample.
NCR: The blood gas component values for a given time period are represented
independently of other blood gas component values in the acuity data element reporting
grouper. For example, the lowest or highest PaO2 value may or may not occur in the same
blood gas from which another highest or lowest blood gas component is reported.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3343).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3344).
4. SHALL contain [1..*] id (CONF:3345).
5. SHALL contain [1..1] code/@code="11556-8" Oxygen PPres Bld (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3346).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3347).
7. SHOULD contain [0..1] effectiveTime (CONF:3348).
8. SHALL contain [1..1] value (CONF:3355).
a. This value SHALL contain [1..1] @unit="mm[Hg]" millimeters of mercury
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3356).
9. SHALL contain [1..1] specimen (CONF:3350).
a. This specimen SHALL contain [1..1] specimenRole (CONF:3351).
i.
This specimenRole SHOULD contain [0..1] id (CONF:3352).
ii. This specimenRole SHALL contain [1..1] specimenPlayingEntity
(CONF:3353).
1. This specimenPlayingEntity SHALL contain [1..1]
code/@code="122552005" Arterial blood specimen
(CodeSystem: 2.16.840.1.113883.6.96 SNOMEDCT) STATIC
(CONF:3354).
4.8.9 Aspartate aminotransferase (AST)
[observation: templateId 2.16.840.1.113883.10.20.17.3.49]
This observation represents an aspartate aminotransferase (AST) result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3647).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3648).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 46
January 2010
4. SHALL contain [1..1] code/@code="1920-8" Aspartate aminotransferase
Ser/Plas (CodeSystem: 2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3649).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3650).
6. SHALL contain [1..1] value (CONF:3651).
a. This value SHALL contain [1..1] @unit="U/L" Units per liter (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3652).
4.8.10 Bicarbonate serum
[observation: templateId 2.16.840.1.113883.10.20.17.3.38]
This observation represents a serum bicarbonate result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3563).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3564).
4. SHALL contain [1..1] code/@code="1963-8" Bicarbonate Ser (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3565).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3566).
6. SHALL contain [1..1] value (CONF:3567).
a. This value SHALL contain [1..1] @unit="meq/L" Milliequivalents per
liter (CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3568).
4.8.11 Bilirubin, conjugated
[observation: templateId 2.16.840.1.113883.10.20.17.3.52]
This observation represents a conjugated bilirubin result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3665).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3666).
4. SHALL contain [1..1] code/@code="15152-2" Bilirubin.glucuronidated
Ser/Plas (CodeSystem: 2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3667).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3668).
6. SHALL contain [1..1] value (CONF:3669).
a. This value SHALL contain [1..1] @unit="mg/dL" Milligrams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3670).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 47
January 2010
4.8.12 Bilirubin, total
[observation: templateId 2.16.840.1.113883.10.20.17.3.51]
This observation represents a total bilirubin result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3659).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3660).
4. SHALL contain [1..1] code/@code="1975-2" Bilirubin Ser/Plas TBIL
(CodeSystem: 2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3661).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3662).
6. SHALL contain [1..1] value (CONF:3663).
a. This value SHALL contain [1..1] @unit="mg/dL" Milligrams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3664).
4.8.13 Birth head circumference
[observation: templateId 2.16.840.1.113883.10.20.17.3.2]
This observation represents a birth head circumference result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3232).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3233).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.19 Birth head circumference DYNAMIC
(CONF:3234).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3235).
6. SHALL contain [1..1] value (CONF:3236).
a. This value SHALL contain [1..1] @unit="cm" centimeter (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3237).
4.8.14 Birth weight
[observation: templateId 2.16.840.1.113883.10.20.17.3.1]
This observation represents a birth weight.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3226).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 48
January 2010
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3227).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.15 Birth weight DYNAMIC (CONF:3228).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3229).
6. SHALL contain [1..1] value (CONF:3230).
a. This value SHALL contain [1..1] @unit="g" gram (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3231).
4.8.15 Blood gas base deficit
[observation: templateId 2.16.840.1.113883.10.20.17.3.32]
This observation represents a blood gas base deficit result from any blood sample.
NCR: The blood gas component values for a given time period are represented
independently of other blood gas component values in the acuity data element reporting
grouper. For example, the lowest or highest base deficit value may or may not occur in the
same blood gas from which another highest or lowest blood gas component is reported.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3497).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3498).
4. SHALL contain [1..*] id (CONF:3499).
5. SHALL contain [1..1] code/@code="30318-0" Base deficit Bld (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3500).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3501).
7. SHOULD contain [0..1] effectiveTime (CONF:3502).
8. SHALL contain [1..1] value (CONF:3503).
a. This value SHALL contain [1..1] @unit="mmol/L" millimoles per liter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3504).
9. MAY contain [0..1] specimen (CONF:3505).
a. This specimen, if present, SHALL contain [1..1] specimenRole (CONF:3506).
i.
This specimenRole SHOULD contain [0..1] id (CONF:3507).
ii. This specimenRole SHALL contain [1..1] specimenPlayingEntity
(CONF:3508).
1. This specimenPlayingEntity SHALL contain [1..1] code
(CONF:3509).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 49
January 2010
4.8.16 Blood gas base excess
[observation: templateId 2.16.840.1.113883.10.20.17.3.31]
This observation represents a blood gas base excess result from any blood sample.
NCR: The blood gas component values for a given time period are represented
independently of other blood gas component values in the acuity data element reporting
grouper. For example, the lowest or highest base excess value may or may not occur in
the same blood gas from which another highest or lowest blood gas component is
reported.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3484).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3485).
4. SHALL contain [1..*] id (CONF:3486).
5. SHALL contain [1..1] code/@code="11555-0" Base excess Bld (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3487).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3488).
7. SHOULD contain [0..1] effectiveTime (CONF:3489).
8. SHALL contain [1..1] value (CONF:3490).
a. This value SHALL contain [1..1] @unit="mmol/L" Milli-osmoles per liter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3491).
9. MAY contain [0..1] specimen (CONF:3492).
a. This specimen, if present, SHALL contain [1..1] specimenRole (CONF:3493).
i.
This specimenRole SHOULD contain [0..1] id (CONF:3494).
ii. This specimenRole SHALL contain [1..1] specimenPlayingEntity
(CONF:3495).
iii. This specimenRole SHALL contain [1..1] code (CONF:3496).
4.8.17 Blood pH
[observation: templateId 2.16.840.1.113883.10.20.17.3.30]
This observation represents a measure of the acidity or alkalinity of blood from any
blood sample.
NCR: The blood gas component values for a given time period are represented
independently of other blood gas component values in the acuity data element reporting.
For example, the lowest or highest pH value may or may not occur in the same blood gas
from which another highest or lowest blood gas component is reported.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3471).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 50
January 2010
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3472).
4. SHALL contain [1..*] id (CONF:3473).
5. SHALL contain [1..1] code/@code="11558-4" pH Bld (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3474).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3475).
7. SHOULD contain [0..1] effectiveTime (CONF:3476).
8. SHALL contain [1..1] value (CONF:3477).
a. This value SHALL contain [1..1] @unit="[pH]" pH (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3478).
9. MAY contain [0..1] specimen (CONF:3479).
a. This specimen, if present, SHALL contain [1..1] specimenRole (CONF:3480).
b. This specimen, if present, SHOULD contain [0..1] id (CONF:3481).
c. This specimen, if present, SHALL contain [1..1] specimenPlayingEntity
(CONF:3482).
i.
This specimenPlayingEntity SHALL contain [1..1] code (CONF:3483).
4.8.18 Blood urea nitrogen (BUN)
[observation: templateId 2.16.840.1.113883.10.20.17.3.47]
This observation represents a blood urea nitrogen (BUN) result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3633).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3634).
4. SHALL contain [1..*] id (CONF:3635).
5. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.12 Blood Urea Nitrogen (BUN) DYNAMIC
(CONF:3636).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3637).
7. SHOULD contain [0..1] effectiveTime (CONF:3638).
8. SHALL contain [1..1] value (CONF:3639).
a. This value SHALL contain [1..1] @unit="mg/dL" Milligrams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3640).
4.8.19 Body temperature
[observation: templateId 2.16.840.1.113883.10.20.17.3.10]
This observation represents a body temperature.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 51
January 2010
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3286).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3287).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.2 Body temperature DYNAMIC (CONF:3288).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3289).
6. SHALL contain [1..1] value (CONF:3290).
a. This value SHALL contain [1..1] @unit="cel" celcius (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3291).
4.8.20 Body weight
[observation: templateId 2.16.840.1.113883.10.20.17.3.11]
This observation represents a body weight result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3292).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3293).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.18 Body weight DYNAMIC (CONF:3294).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3295).
6. SHALL contain [1..1] value (CONF:3296).
a. This value SHALL contain [1..1] @unit="g" gram (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3297).
4.8.21 Calcium ionized
[observation: templateId 2.16.840.1.113883.10.20.17.3.34]
This observation represents an ionized (unbound) calcium result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3518).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3519).
4. SHALL contain [1..*] id (CONF:3520).
5. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.5 Ionized Calcium DYNAMIC (CONF:3521).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3522).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 52
January 2010
7. SHOULD contain [0..1] effectiveTime (CONF:3523).
8. SHALL contain [1..1] value (CONF:3524).
a. This value SHALL contain [1..1] @unit="mg/dL" Milligrams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3525).
4.8.22 Calcium total serum
[observation: templateId 2.16.840.1.113883.10.20.17.3.35]
This observation represents a total serum calcium result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3539).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3540).
4. SHALL contain [1..1] code/@code="17861-6" Calcium Ser/Plas (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3541).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3542).
6. SHALL contain [1..1] value (CONF:3543).
a. This value SHALL contain [1..1] @unit="mg/dL" Milligrams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3544).
4.8.23 Creatinine observation
[observation: templateId 2.16.840.1.113883.10.20.17.3.48]
This observation represents a creatinine result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3641).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3642).
4. SHALL contain [1..1] code/@code="2160-0" Creatinine Ser/Plas (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3643).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3644).
6. SHALL contain [1..1] value (CONF:3645).
a. This value SHALL contain [1..1] @unit="mg/dL" Milligrams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3646).
4.8.24 Diastolic blood pressure
[observation: templateId 2.16.840.1.113883.10.20.17.3.28]
This observation represents a diastolic blood pressure.
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 53
January 2010
NCR: The highest and lowest blood pressure component values for a given time period are
represented independently of other blood pressure component values in the acuity data
element reporting grouper. For example, the lowest mean blood pressure may or may not
occur during the same reading where a lowest systolic or lowest diastolic reading
occurred.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3456).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3457).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.21 Diastolic blood pressure DYNAMIC
(CONF:3458).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3459).
6. SHALL contain [1..1] value (CONF:3460).
a. This value SHALL contain [1..1] @unit="mm[Hg]" Millimeter of mercury
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3461).
4.8.25 Fibrinogen level
[observation: templateId 2.16.840.1.113883.10.20.17.3.42]
This observation represents a fibrinogen level result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3591).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3592).
4. SHALL contain [1..*] id (CONF:3593).
5. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.8 Fibrinogen DYNAMIC (CONF:3594).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3595).
7. SHOULD contain [0..1] effectiveTime (CONF:3596).
8. SHALL contain [1..1] value (CONF:3597).
a. This value SHALL contain [1..1] @unit="mg/dL" Milligrams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3598).
4.8.26 Gestational age
[observation: templateId 2.16.840.1.113883.10.20.17.3.3]
This observation represents the gestational age of an infant at birth; it is not the
gestation of a pregnancy. Although gestational age of an infant is typically recorded in
weeks plus days (e.g., 27 weeks and 3 days), the xsi:type PQ does not allow for mixed
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 54
January 2010
units. The gestational age must be represented in days; in this case 27 weeks and 3
days would be represented with 192 days.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3238).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3239).
4. SHALL contain [1..1] code/@code="412726003" Gestational age at birth
(CodeSystem: 2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3240).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3241).
6. SHALL contain [1..1] value (CONF:3242).
a. This value SHALL contain [1..1] @unit="d" day (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3243).
4.8.27 Glucose serum
[observation: templateId 2.16.840.1.113883.10.20.17.3.39]
This observation represents a serum glucose result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3569).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3570).
4. SHALL contain [1..1] code/@code="2345-7" Glucose Ser/Plas (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3571).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3572).
6. SHALL contain [1..1] value (CONF:3573).
a. This value SHALL contain [1..1] @unit="mg/dL" Milligrams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3574).
4.8.28 Head circumference
[observation: templateId 2.16.840.1.113883.10.20.17.3.9]
This observation represents a head circumference.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3280).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3281).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 55
January 2010
4. SHALL contain [1..1] code/@code which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.25 Head circumference DYNAMIC (CONF:3282).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3283).
6. SHALL contain [1..1] value (CONF:3284).
a. This value SHALL contain [1..1] @unit="cm" centimeter (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3285).
4.8.29 Heart rate
[observation: templateId 2.16.840.1.113883.10.20.17.3.29]
This observation represents the beats per minute of the heart.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3465).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3466).
4. SHALL contain [1..1] code/@codewhich SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.25 Heart rate DYNAMIC (CONF:3467).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3468).
6. SHALL contain [1..1] value (CONF:3469).
a. This value SHALL contain [1..1] @unit="/min" Per minute (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3470).
4.8.30 Hemoglobin
[observation: templateId 2.16.840.1.113883.10.20.17.3.46]
This observation represents a hemoglobin result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3619).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3620).
4. SHALL contain [1..*] id (CONF:3621).
5. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.10 Hemoglobin DYNAMIC (CONF:3622).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3623).
7. SHOULD contain [0..1] effectiveTime (CONF:3624).
8. SHALL contain [1..1] value (CONF:3625).
a. This value SHALL contain [1..1] @unit="g/dL" Grams per deciliter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3626).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 56
January 2010
4.8.31 International normalized ratio (INR)
[observation: templateId 2.16.840.1.113883.10.20.17.3.45]
This observation represents an international normalized ratio (INR) result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3611).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3612).
4. SHALL contain [1..*] id (CONF:3613).
5. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.9 International Normalized Ratio (INR)
DYNAMIC (CONF:3614).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3615).
7. SHOULD contain [0..1] effectiveTime (CONF:3616).
8. SHALL contain [1..1] value (CONF:3617).
a. This value SHALL contain [1..1] @unit="s" seconds (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3618).
4.8.32 Lactic acid from serum/plasma
[observation: templateId 2.16.840.1.113883.10.20.17.3.33]
This observation represents a lactic acid measurement in serum or plasma.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3510).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3511).
4. SHALL contain [1..*] id (CONF:3512).
5. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.4 Lactic acid/lactate DYNAMIC (CONF:3513).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3514).
7. SHOULD contain [0..1] effectiveTime (CONF:3515).
8. SHALL contain [1..1] value (CONF:3516).
a. This value SHALL contain [1..1] @unit="mmol/L" millimoles per liter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3517).
4.8.33 Mean airway pressure
[observation: templateId 2.16.840.1.113883.10.20.17.3.19]
This observation represents the average pressure to which the lungs are exposed during
the respiratory cycle while receiving measurable positive pressure respiratory support.
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 57
January 2010
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3377).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3378).
4. SHALL contain [1..1] code/@code="20056-8" Mean Airway Pressure (MAP)
(CodeSystem: 2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3379).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3380).
6. SHALL contain [1..1] value (CONF:3381).
a. This value SHALL contain [1..1] @unit="cm[H2O]" Centimeters of water
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3382).
4.8.34 Mean blood pressure
[observation: templateId 2.16.840.1.113883.10.20.17.3.26]
This observation represents a mean blood pressure.
NCR: The highest and lowest blood pressure component values for a given time period are
represented independently of other blood pressure component values in the acuity data
element reporting grouper. For example, the lowest mean blood pressure may or may not
occur during the same reading where a lowest systolic or lowest diastolic reading
occurred.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3444).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3445).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.22 Mean blood pressure DYNAMIC (CONF:3446).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3447).
6. SHALL contain [1..1] value (CONF:3448).
a. This value SHALL contain [1..1] @unit="mm[Hg]" Millimeter of mercury
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3449).
4.8.35 PaCO2 Observation
[observation: templateId 2.16.840.1.113883.10.20.17.3.20]
This observation represents partial pressure of carbon dioxide in blood from any blood
sample.
NCR: The blood gas component values for a given time period are represented
independently of other blood gas component values in the acuity data element reporting
grouper. For example, the lowest or highest PaCO2 value may or may not occur in the
same blood gas from which another highest or lowest blood gas component is reported
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 58
January 2010
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3383).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3384).
4. SHALL contain [1..*] id (CONF:3385).
5. SHALL contain [1..1] code/@code="11557-6" Carbon dioxide PPres Bld
(CodeSystem: 2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3386).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3387).
7. SHOULD contain [0..1] effectiveTime (CONF:3388).
8. SHALL contain [1..1] value (CONF:3389).
a. This value SHALL contain [1..1] @unit="mm[Hg]" millimeters of mercury
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3390).
9. MAY contain [0..1] specimen (CONF:3391).
a. This specimen, if present, SHALL contain [1..1] specimenRole (CONF:3392).
i.
This specimenRole SHOULD contain [0..1] id (CONF:3393).
ii. This specimenRole SHALL contain [1..1] specimenPlayingEntity
(CONF:3394).
1. This specimenPlayingEntity SHALL contain [1..1] code
(CONF:3395).
4.8.36 Platelets
[observation: templateId 2.16.840.1.113883.10.20.17.3.41]
This observation represents a blood platelet result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3583).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3584).
4. SHALL contain [1..*] id (CONF:3585).
5. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.7 Platelet DYNAMIC (CONF:3586).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3587).
7. SHOULD contain [0..1] effectiveTime (CONF:3588).
8. SHALL contain [1..1] value (CONF:3589).
a. This value SHALL contain [1..1] @unit="10*3/uL" ThousandsPerMicroLiter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3590).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 59
January 2010
4.8.37 Potassium serum
[observation: templateId 2.16.840.1.113883.10.20.17.3.37]
This observation represents a serum potassium result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3557).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3558).
4. SHALL contain [1..1] code/@code="22760-3" Potassium Ser/Plas (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3559).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3560).
6. SHALL contain [1..1] value (CONF:3561).
a. This value SHALL contain [1..1] @unit="meq/L" Milliequivalents per
liter (CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3562).
4.8.38 Prothrombin time (PT)
[observation: templateId 2.16.840.1.113883.10.20.17.3.43]
This observation represents a prothrombin time (PT) result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3599).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3600).
4. SHALL contain [1..1] code/@code="5902-2" Coagulation tissue factor induced
time PPP (CodeSystem: 2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3601).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3602).
6. SHALL contain [1..1] value (CONF:3603).
a. This value SHALL contain [1..1] @unit="s" seconds (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3604).
4.8.39 Respiratory rate
[observation: templateId 2.16.840.1.113883.10.20.17.3.21]
This observation represents a patient's number of breaths per minute.
NCR: If patient is apneic or breathing at a rate below ventilatory rate, it is understood that
the value in documentation will likely be the ventilator rate.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 60
January 2010
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3396).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3397).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.23 Respiratory rate DYNAMIC (CONF:3398).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3399).
6. SHALL contain [1..1] value (CONF:3400).
a. This value SHALL contain [1..1] @unit="/min" per minute (CodeSystem:
2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3401).
4.8.40 Seizures
[observation: templateId 2.16.840.1.113883.10.20.17.3.54]
This observation represents presence of clinical or electroencephalographic (EEG)
seizures. The possible values are: none, single, or multiple.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3685).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3686).
4. SHALL contain [1..1] code/@code="170707004" Fit frequency (CodeSystem:
2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3687).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3688).
6. SHALL contain [1..1] value/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.13 Seizure frequency DYNAMIC (CONF:3689).
4.8.41 Sodium serum
[observation: templateId 2.16.840.1.113883.10.20.17.3.36]
This observation represents a serum sodium result.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3551).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3552).
4. SHALL contain [1..1] code/@code="42570-2" Sodium Ser/Plas (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3553).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3554).
6. SHALL contain [1..1] value (CONF:3555).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 61
January 2010
a. This value SHALL contain [1..1] @unit="meq/L" Milliequivalents per
liter (CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3556).
4.8.42 Systolic blood pressure
[observation: templateId 2.16.840.1.113883.10.20.17.3.27]
This observation represents a systolic blood pressure.
NCR: The highest and lowest blood pressure component values for a given time period are
represented independently of other blood pressure component values in the acuity data
element reporting grouper. For example, the lowest mean blood pressure may or may not
occur during the same reading where a lowest systolic or lowest diastolic reading
occurred.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3450).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3451).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.20 Systolic blood pressure DYNAMIC
(CONF:3452).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3453).
6. SHALL contain [1..1] value (CONF:3454).
a. This value SHALL contain [1..1] @unit="mm[Hg]" Millimeter of mercury
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3455).
4.8.43 Urine output
[observation: templateId 2.16.840.1.113883.10.20.17.3.55]
This observation represents the urine output in milliliters per kilogram per hour.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3699).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3700).
4. SHALL contain [1..1] code/@code="364202003" Measure of urine output
(CodeSystem: 2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3701).
5. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3702).
6. SHALL contain [1..1] value (CONF:3703).
a. This value SHALL contain [1..1] @unit="mL/kg/h" Milliliters per
kilogram per hour (CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC
(CONF:3704).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 62
January 2010
4.8.44 White blood cell (leukocyte) count
[observation: templateId 2.16.840.1.113883.10.20.17.3.40]
This observation represents the white blood cell (WBC) (leukocyte) count.
1. Conforms to CCD Result observation Template (templateId:
2.16.840.1.113883.10.20.1.31).
2. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3575).
3. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3576).
4. SHALL contain [1..*] id (CONF:3577).
5. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.6 White blood cell count DYNAMIC (CONF:3578).
6. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3579).
7. SHOULD contain [0..1] effectiveTime (CONF:3580).
8. SHALL contain [1..1] value (CONF:3581).
a. This value SHALL contain [1..1] @unit="10*3/uL" ThousandsPerMicroLiter
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3582).
4.9 Discharge activity – Neonatal
[act: templateId 2.16.840.1.113883.10.20.17.3.13]
This discharge act contains discharge-related observation templates for head
circumference and body weight.
1. SHALL contain [1..1] @classCode="ACT" (CodeSystem: 2.16.840.1.113883.5.6
HL7ActClass) STATIC (CONF:3309).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3310).
3. SHALL contain [1..1] code/@code="58000006" Discharge procedure (CodeSystem:
2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3311).
4. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3312).
5. SHALL contain [1..1] entryRelationship (CONF:3313) such that it
a. SHALL contain [1..1] @typeCode="COMP" Refers to (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3314).
b. SHALL contain [1..1] Head circumference
(templateId:2.16.840.1.113883.10.20.17.3.9) (CONF:3315).
6. SHALL contain [1..1] entryRelationship (CONF:3316) such that it
a. SHALL contain [1..1] @typeCode="COMP" Refers to (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3317).
b. SHALL contain [1..1] Body weight
(templateId:2.16.840.1.113883.10.20.17.3.11) (CONF:3318).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 63
January 2010
Figure 17: Neonatal discharge activity example
<!-- Discharge Act -->
<act classCode="ACT" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.17.3.13" />
<code code="58000006" codeSystem="2.16.840.1.113883.6.96"
displayName="Discharge procedure" />
<statusCode code="completed" />
<entryRelationship typeCode="COMP">
...
</entryRelationship>
<entryRelationship typeCode="COMP">
...
</entryRelationship>
</act>
4.10 Inborn/outborn
[observation: templateId 2.16.840.1.113883.10.20.17.3.7]
This observation represents whether an infant was born at the reporting hospital or
some other location. If the negation indicator is true the infant was outborn (born at
another location), if the negation indicator is false the infant was inborn (born at the
reporting hospital.
1. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3262).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3263).
3. SHALL contain @negationInd (CONF:3264).
4. SHALL contain [1..1] code/@code="ASSERTION" (CodeSystem:
2.16.840.1.113883.5.4 HL7ActCode) STATIC (CONF:3265).
5. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3266).
6. SHALL contain [1..1] value/@code="169818001" Born before arrival
(CodeSystem: 2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3268).
Figure 18: Inborn/outborn example
<observation classCode="OBS" moodCode="EVN" negationInd="false">
<templateId root="2.16.840.1.113883.10.20.17.3.7" />
<code code="ASSERTION" codeSystem="2.16.840.1.113883.5.4" />
<statusCode code="completed" />
<value xsi:type="CD" code="169818001" codeSystem="2.16.840.1.113883.6.96"
displayName="Born before arrival" />
</observation>
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 64
January 2010
4.11 Nothing by mouth (NPO)
[observation: templateId 2.16.840.1.113883.10.20.17.3.56]
This observation represents whether a patient was taking nothing by mouth (NPO). If
the patient was NPO the value of the negation indicator is set to "FALSE" and if the
patient was taking (nutritive) feeds the negation indicator is set to "TRUE".
NCR: NPO status in the NICU settings may include non-nutritive volumes for gastric
stimulation.
1. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3705).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3706).
3. SHALL contain @negationInd (CONF:3707).
4. SHALL contain [1..1] code/@code="ASSERTION" (CodeSystem:
2.16.840.1.113883.5.4 HL7ActCode) STATIC (CONF:3708).
5. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3709).
6. SHALL contain [1..1] value/@code="182923009" NPO - Nothing by mouth
(CodeSystem: 2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3710).
Figure 19: Nothing by mouth (NPO) example
<observation classCode="OBS" moodCode="EVN" negationInd="false">
<templateId root="2.16.840.1.113883.10.20.17.3.56" />
<code code="182923009" codeSystem="2.16.840.1.113883.6.96"
displayName="NPO - Nothing by mouth" />
</observation>
4.12 Oxygenation index
[observation: templateId 2.16.840.1.113883.10.20.17.3.22]
This observation represents the sum of the calculated value of (Mean Airway Pressure *
FIO2*100)/PaO2.
1. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3402).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3403).
3. SHALL contain [1..1] code/@code="313558004" Oxygenation index measurement
(CodeSystem: 2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3404).
4. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3405).
5. SHALL contain [1..1] value (CONF:3406).
a. This value SHALL contain [1..1] @unit="mm[Hg]" millimeters of mercury
(CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC (CONF:3407).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 65
January 2010
Figure 20: Oxygenation index example
<observation classCode="OBS" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.17.3.22" />
<code code="313558004" codeSystem="2.16.840.1.113883.6.96"
displayName="Oxygenation index measurement " />
<effectiveTime value="200903031620" />
<value xsi:type="PQ" value="11.6" unit="mm[Hg]" />
</observation>
4.13 PaO2/FIO2 ratio
[observation: templateId 2.16.840.1.113883.10.20.17.3.18]
This observation represents the ratio of PaO2 (Arterial tension of oxygen) to FIO2
(Fraction of inspired oxygen).
NCR: This is recorded when the lowest PaO2 is recorded during the specified time
interval.
1. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3372).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3373).
3. SHALL contain [1..1] code/@code="PaO2/FIO2-X" PaO2/FIO2 ratio (CodeSystem:
2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3374).
4. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3375).
5. SHALL contain [1..1] value (CONF:3376).
Figure 21: PaO2/FIO2 example
<observation classCode="OBS" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.17.3.18" />
<code code="PaO2/FIO2-X" codeSystem="2.16.840.1.113883.6.1"
displayName="PaO2/FIO2 ratio" />
<statusCode code="completed" />
<effectiveTime value="200903051607" />
<value xsi:type="REAL" value="257.1" />
</observation>
4.14 Renal dialysis (renal replacement therapy)
[observation: templateId 2.16.840.1.113883.10.20.17.3.57]
This observation represents whether or not a patient received any type of renal dialysis.
If the negation indicator is true, the patient did NOT receive renal dialysis therapy. If
the negation indicator is false, the patient did receive renal dialysis therapy.
1. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3711).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 66
January 2010
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3712).
3. SHALL contain @negationInd (CONF:3713).
4. SHALL contain [1..1] code/@code="ASSERTION" (CodeSystem:
2.16.840.1.113883.5.4 HL7ActCode) STATIC (CONF:3714).
5. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3715).
6. SHALL contain [1..1] value/@code="265764009" Renal dialysis (CodeSystem:
2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3716).
Figure 22: Renal dialysis example (did not occur)
<observation classCode="OBS" moodCode="EVN" negationInd="true">
<!-- "true" negationInd negates finding; dialysis did not occur -->
<templateId root="2.16.840.1.113883.10.20.17.3.57" />
<code code="265764009" codeSystem="2.16.840.1.113883.6.96"
displayName="Renal dialysis" />
</observation>
4.15 Reporting parameters act
[act: templateId 2.16.840.1.113883.10.20.17.3.8]
The reporting parameters act provides information about the reporting time interval,
and helps provide context for the patient data being reported to the receiving
organization. The receiving organization may tell the reporting hospitals what
information to include, such as dates representing the quarters of the year for which
patient data is desired.
1. SHALL contain [1..1] @classCode="ACT" (CodeSystem: 2.16.840.1.113883.5.6
HL7ActClass) STATIC (CONF:3269).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3270).
3. SHALL contain [1..1] code/@code="252116004" Observation Parameters
(CodeSystem: 2.16.840.1.113883.6.96 SNOMEDCT) STATIC (CONF:3272).
4. SHALL contain [1..1] effectiveTime (CONF:3273).
a. This effectiveTime SHALL contain [1..1] low (CONF:3274).
b. This effectiveTime SHALL contain [1..1] high (CONF:3275).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 67
January 2010
Figure 23: Reporting parameters act example
<act classCode="ACT" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.17.3.8" />
<code code="252116004" codeSystem="2.16.840.1.113883.6.96"
displayName="Observation Parameters" />
<effectiveTime>
<low value="20090601" />
<!-- The first day of the period reported. -->
<high value="20090831" />
<!-- The last day of the period reported. -->
</effectiveTime>
</act>
4.16 Respiratory or ventilatory support
[act: templateId 2.16.840.1.113883.10.20.17.3.25]
This act represents the type of respiratory or ventilatory support a patient is receiving.
The most general code 266700009 Ventilation assistance from the valueSet should
be used with the negation indicator to represent that the patient did not receive
ventilatory/respiratory assistance.
1. SHALL contain [1..1] @classCode="ACT" (CodeSystem: 2.16.840.1.113883.5.6
HL7ActClass) STATIC (CONF:3427).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3428).
3. SHALL contain @negationInd (CONF:3429).
4. SHALL contain [1..1] code/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.3 Respiratory/Ventilatory Support Modes
DYNAMIC (CONF:3430).
5. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3431).
6. MAY contain [0..1] entryRelationship (CONF:3432) such that it
a. SHALL contain [1..1] @typeCode="COMP" Component (CodeSystem:
2.16.840.1.113883.5.1002 HL7ActRelationshipType) STATIC
(CONF:3433).
b. SHALL contain [1..1] observation (CONF:3434).
i.
This observation SHALL contain [1..1] @classCode="OBS"
Observation (CodeSystem: 2.16.840.1.113883.5.6 HL7ActClass)
STATIC (CONF:3435).
ii. This observation SHALL contain [1..1] @moodCode="EVN" Event
(CodeSystem: 2.16.840.1.113883.5.1001 HL7ActMood) STATIC
(CONF:3436).
iii. This observation SHALL contain [1..1] code/@code="79063001" Gas
flow rate (v) (CodeSystem: 2.16.840.1.113883.6.96 SNOMEDCT)
STATIC (CONF:3437).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 68
January 2010
iv. This observation SHALL contain [1..1]
statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3438).
v. This observation SHALL contain [1..1] value (CONF:3440).
1. This value SHALL contain [1..1] @unit="L/min" Liters per
minute (CodeSystem: 2.16.840.1.113883.6.8 UCUM) STATIC
(CONF:3441).
7. This act SHALL contain the entryRelationship representing gas flow rate if the act is
representing nasal cannula support (CONF:4201).
Figure 24: Respiratory or ventilatory support example
<act classCode="ACT" moodCode="EVN" negationInd="false">
<templateId root="2.16.840.1.113883.10.20.17.3.25" />
<code code="59427005" codeSystem="2.16.840.1.113883.6.96"
displayName="synchronized intermittent mandatory ventilation" />
<statusCode code="completed" />
</act>
4.17 Respiratory severity score
[observation: templateId 2.16.840.1.113883.10.20.17.3.23]
This observation represents the sum of the calculated value of (Mean Airway Pressure *
FIO2).
1. SHALL contain [1..1] @classCode="OBS" Observation (CodeSystem:
2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3408).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3409).
3. SHALL contain [1..1] code/@code="RSS-X" Respiratory Severity Score
(CodeSystem: 2.16.840.1.113883.6.1 LOINC) STATIC (CONF:3410).
4. SHALL contain [1..1] statusCode/@code="completed" Completed (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3411).
5. SHALL contain [1..1] value (CONF:3412).
Figure 25: Respiratory severity score example
<observation classCode="OBS" moodCode="EVN">
<templateId root="2.16.840.1.113883.10.20.17.3.23" />
<code code="RSS-X" codeSystem="2.16.840.1.113883.6.1"
displayName="Respiratory Severity Score " />
<effectiveTime value="200903031620" />
<value xsi:type="REAL" value="5.12" />
</observation>
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 69
January 2010
4.18 Steroid treatment (systemic)
[substanceAdministration: templateId 2.16.840.1.113883.10.20.17.3.58]
This template represents whether or not systemic steroids have been administered. The
ingredient code N0000175576 Corticosteroid [EXT] from the NDF-RT code system
in the valueSet should be used with the negation indicator to represent that the patient
did not receive systemic steroids.
1. SHALL contain [1..1] @classCode="SBADM" Substance administration
(CodeSystem: 2.16.840.1.113883.5.6 HL7ActClass) STATIC (CONF:3717).
2. SHALL contain [1..1] @moodCode="EVN" Event (CodeSystem:
2.16.840.1.113883.5.1001 HL7ActMood) STATIC (CONF:3718).
3. MAY contain @negationInd (CONF:3719).
4. SHALL contain [1..1] statusCode/@code="completed" (CodeSystem:
2.16.840.1.113883.5.14 HL7ActStatus) STATIC (CONF:3720).
5. MAY contain [0..1] effectiveTime (CONF:3721).
6. MAY contain [0..1] routeCode/@code, which SHALL be selected from ValueSet
2.16.840.1.113883.3.88.12.3221.8.7 Medication Route FDA DYNAMIC
(CONF:3723).
7. SHALL contain [1..1] consumable (CONF:3724).
a. This consumable SHALL contain [1..1] manufacturedProduct (CONF:3725).
i.
This manufacturedProduct SHALL contain [1..1]
manufacturedMaterial (CONF:3726).
1. This manufacturedMaterial SHALL contain [1..1] code/@code,
which SHALL be selected from ValueSet
2.16.840.1.113883.11.20.5.14 Systemic steroids
DYNAMIC (CONF:3727).
Figure 26: Steroid treatment example
<!-- Steroid Treatment not given -->
<substanceAdministration classCode="SBADM" moodCode="EVN" negationInd="true">
<templateId root="2.16.840.1.113883.10.20.17.3.58" />
<statusCode code="completed" />
<consumable>
<manufacturedProduct>
<manufacturedMaterial>
<code code="N0000175576" codeSystem="2.16.840.1.113883.3.26.1.5"
displayName="Corticosteroid" codeSystemName="NDF-RT">
<originalText>Corticosteroid</originalText>
</code>
</manufacturedMaterial>
</manufacturedProduct>
</consumable>
</substanceAdministration>
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 70
January 2010
4.19 CCD Location participation
[participant: templateId 2.16.840.1.113883.10.20.1.45]
This clinical statement represents a location.
1. The value for "participant / @typeCode" in a location participation SHALL be "LOC"
2.16.840.1.113883.5.90 ParticipationType STATIC. (CONF:570).
2. A location participation SHALL contain exactly one participant / participantRole.
(CONF:571).
3. The value for "participant / participantRole / @classCode" in a location participation
SHALL be "SDLOC" "Service delivery location" 2.16.840.1.113883.5.110 RoleClass
STATIC. (CONF:572).
4. Participant / participantRole in a location participation MAY contain exactly one
participant / participantRole / code. (CONF:573).
5. The value for "participant / participantRole / code" in a location participation
SHOULD be selected from ValueSet 2.16.840.1.113883.1.11.17660
ServiceDeliveryLocationRoleType 2.16.840.1.113883.5.111 RoleCode DYNAMIC.
(CONF:574).
6. Participant / participantRole in a location participation MAY contain exactly one
participant / participantRole / playingEntity. (CONF:575).
7. The value for "participant / participantRole / playingEntity / @classCode" in a
location participation SHALL be "PLC" "Place" 2.16.840.1.113883.5.41 EntityClass
STATIC. (CONF:576).
4.19.1 Neonatal ICU location
[participant: templateId 2.16.840.1.113883.10.20.17.3.14]
This template restricts the CCD location participation template to a Neonatal ICU.
1. Conforms to CCD Location participation Template (templateId:
2.16.840.1.113883.10.20.1.45).
2. SHALL contain [1..1] @typeCode="LOC" Location (CodeSystem:
2.16.840.1.113883.5.90 HL7ParticipationType) STATIC (CONF:3319).
a. This @typeCode SHALL contain [1..1] participantRole (CONF:3320).
i.
This participantRole SHALL contain [1..1] @classCode="SDLOC"
Located entity (CodeSystem: 2.16.840.1.113883.5.110
HL7RoleClass) STATIC (CONF:3321).
ii. This participantRole SHALL contain [1..1] code/@code="1040-5"
Neonatal critical care unit (CodeSystem:
2.16.840.1.113883.6.259 HL7 HealthcareServiceLocation)
STATIC (CONF:3322).
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 71
January 2010
Figure 27: Neonatal ICU location example
<!-- CCD Location participation template -->
<participant typeCode="LOC">
<templateId root="2.16.840.1.113883.10.20.1.45" />
<templateId root="2.16.840.1.113883.10.20.17.3.14" />
<participantRole classCode="SDLOC">
<code code="PEDNICU" codeSystem="2.16.840.1.113883.5.111"
displayName="Neonatal ICU" />
</participantRole>
</participant>
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 72
January 2010
5 REFERENCES
1. HL7 Implementation Guide: CDA Release 2 – Continuity of Care Document (CCD) A
CDA implementation of ASTM E2369-05 Standard Specification for Continuity of
Care Record© (CCR) April 01, 2007 available through HL7.
2. HL7 Implementation Guide for CDA Release 2 Quality Reporting Document
Architecture (QRDA) Draft Standard for Trial Use March 2009. Available at: Quality
Reporting Document Architecture (QRDA)
3. HL7 Implementation Guide for CDA Release 2 CDA for Public Health Case Reports
(PHCR) Informative Standard October 2009. Available through HL7.
4. HL7 Implementation Guide for CDA Release 2: NHSN Healthcare Associated
Infection (HAI) Reports, Release 2 Draft Standard for Trial Use January 2009
Available at: NHSN Healthcare Associated Infection (HAI) Reports
5. Dolin RH, Alschuler L, Boyer S, Beebe C, Behlen FM, Biron PV, Shabo A, (Editors).
HL7 Clinical Document Architecture, Release 2.0. ANSI-approved HL7 Standard;
May 2005. Ann Arbor, Mich.: Health Level Seven, Inc. Available through HL7 or if an
HL7 member with the following link:
CDA Release 2 Normative Web Edition.
6. LOINC®: Logical Observation Identifiers Names and Codes, Regenstrief Institute.
7. SNOMED CT®: SNOMED Clinical Terms SNOMED International Organization.
8. Extensible Markup Language, www.w3.org/XML.
9. Dolin RH, Alschuler L, Boyer S, Beebe C, Behlen FM, Biron PV, Shabo A., HL7
Clinical Document Architecture, Release 2. J Am Med Inform Assoc. 2006;13:3039.
Available at: http://www.jamia.org/cgi/reprint/13/1/30.
10. Using SNOMED CT in HL7 Version 3; Implementation Guide, Release 1.5. Available
through HL7 or if an HL7 member with the following link: Using SNOMED CT in
HL7 Version 3
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 73
January 2010
APPENDIX A — ACRONYMNS AND ABBREV IATIONS
ALT
alanine aminotransferase
AST
aspartate aminotransferase
ANSI
American National Standards Institute
ASTM
American Society for Standards and Materials
BUN
blood urea nitrogen
CCD
Continuity of Care Document
CDA
Clinical Document Architecture
CDS
Core data set
CHCA
Child Health Corporation of America
CHNC
Children’s Hospitals Neonatal Consortium
CONF
Conformance
CPT-4
Current Procedural Terminology, 4th Edition
DRIV
Is derived from
DSTU
Draft Standard for Trial Use
EEG
electroencephalogram
EHR
electronic health record
ENC
encounter
EVN
event
FIO2
Fraction of inspired oxygen
HAI
Healthcare Associated Infection
HITEP
Health Information Technology Expert Panel
HITSP
Health Information Technology Standards Panel
HL7
Health Level 7
ICU
Intensive Care Unit
IG
Implementation Guide
IMP
Inpatient
INT
Intent
INR
International Normalized Ratio
LOC
location
LOINC
Logical Observation Identifiers Names and Codes
NCR
Neonatal Care Report
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 74
January 2010
NHSN
National Healthcare Safety Network
NICU
Neonatal Intensive Care Unit
NPO
nothing by mouth
OBS
observation
OID
object identifier
OTH
Other
PaO2
Arterial tension of oxygen
PaCO2
Arterial tension of carbon dioxide
pH
Acidity (or basicity) of a solution
PHCR
Public Health Case Report
PLC
place
PQ
physical quantity
PT
prothrombin time
QRDA
Quality Reporting Document Architecture
R2
Release 2
RIM
Reference Information Model
RSON
reason
SBADM
substance administration
SDLOC
service delivery location
SNOMED CT Systematized Nomenclature of Medicine--Clinical Terms
SUBJ
subject
UCUM
Unified Code for Units of Measure
UNK
Unknown
VON
Vermont Oxford Network
WBC
white blood cells
XML
Extensible Markup Language
XSL
Extensible Stylesheet Language
XSI
XML Schema Instance
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 75
January 2010
APPENDIX B — TEMPLATES USED IN THIS GUIDE
The following table lists template hierarchically as they appear in this document. See
the Templates by Containment table to see templates see the various groupings and
organization of the templates as they would exist in an NCR CDA instance.
Table 3: Templates Organized Hierarchically
Template Title
Template OID
Document Templates
Neonatal Care Report
2.16.840.1.113883.10.20.17.1.1
Section Templates
CCD Encounters section
NCR encounters section
2.16.840.1.113883.10.20.1.3
2.16.840.1.113883.10.20.17.2.2
Acuity score data section
2.16.840.1.113883.10.20.17.2.3
Patient data section
2.16.840.1.113883.10.20.17.2.4
Patient data section - NCR
2.16.840.1.113883.10.20.17.2.5
Reporting parameters section
2.16.840.1.113883.10.20.17.2.1
Clinical Statement Templates
Acuity indicator data generic organizer
2.16.840.1.113883.10.20.17.3.59
Acuity data time organizer - admission to 12 hours
2.16.840.1.113883.10.20.17.3.60
Acuity data time organizer - day 3
2.16.840.1.113883.10.20.17.3.61
Acuity data time organizer - day 7
2.16.840.1.113883.10.20.17.3.62
Admission activity - neonatal
2.16.840.1.113883.10.20.17.3.12
CCD Encounter activity
2.16.840.1.113883.10.20.1.21
Neonatal ICU encounter activity
CCD Medication activity
2.16.840.1.113883.10.20.17.3.15
2.16.840.1.113883.10.20.1.24
Nitric oxide administration
2.16.840.1.113883.10.20.17.3.24
Oxygen administration
2.16.840.1.113883.10.20.17.3.17
CCD Result observation
2.16.840.1.113883.10.20.1.31
Activated partial thromboplastin time
2.16.840.1.113883.10.20.17.3.44
Alanine aminotransferase (ALT)
2.16.840.1.113883.10.20.17.3.50
Albumin observation
2.16.840.1.113883.10.20.17.3.53
Apgar at 1 minute
2.16.840.1.113883.10.20.17.3.4
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 76
January 2010
Template Title
Template OID
Apgar at 5 minute
2.16.840.1.113883.10.20.17.3.5
Apgar score prolonged
2.16.840.1.113883.10.20.17.3.6
Arterial PaO2 Observation
2.16.840.1.113883.10.20.17.3.16
Aspartate aminotransferase (AST)
2.16.840.1.113883.10.20.17.3.49
Bicarbonate serum
2.16.840.1.113883.10.20.17.3.38
Bilirubin, conjugated
2.16.840.1.113883.10.20.17.3.52
Bilirubin, total
2.16.840.1.113883.10.20.17.3.51
Birth head circumference
2.16.840.1.113883.10.20.17.3.2
Birth weight
2.16.840.1.113883.10.20.17.3.1
Blood gas base deficit
2.16.840.1.113883.10.20.17.3.32
Blood gas base excess
2.16.840.1.113883.10.20.17.3.31
Blood pH
2.16.840.1.113883.10.20.17.3.30
Blood urea nitrogen (BUN)
2.16.840.1.113883.10.20.17.3.47
Body temperature
2.16.840.1.113883.10.20.17.3.10
Body weight
2.16.840.1.113883.10.20.17.3.11
Calcium ionized
2.16.840.1.113883.10.20.17.3.34
Calcium total serum
2.16.840.1.113883.10.20.17.3.35
Creatinine observation
2.16.840.1.113883.10.20.17.3.48
Diastolic blood pressure
2.16.840.1.113883.10.20.17.3.28
Fibrinogen level
2.16.840.1.113883.10.20.17.3.42
Gestational age
2.16.840.1.113883.10.20.17.3.3
Glucose serum
2.16.840.1.113883.10.20.17.3.39
Head circumference
2.16.840.1.113883.10.20.17.3.9
Heart rate
2.16.840.1.113883.10.20.17.3.29
Hemoglobin
2.16.840.1.113883.10.20.17.3.46
International normalized ratio (INR)
2.16.840.1.113883.10.20.17.3.45
Lactic acid from serum/plasma
2.16.840.1.113883.10.20.17.3.33
Mean airway pressure
2.16.840.1.113883.10.20.17.3.19
Mean blood pressure
2.16.840.1.113883.10.20.17.3.26
PaCO2 Observation
2.16.840.1.113883.10.20.17.3.20
Platelets
2.16.840.1.113883.10.20.17.3.41
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 77
January 2010
Template Title
Template OID
Potassium serum
2.16.840.1.113883.10.20.17.3.37
Prothrombin Time (PT)
2.16.840.1.113883.10.20.17.3.43
Respiratory rate
2.16.840.1.113883.10.20.17.3.21
Seizure frequency
2.16.840.1.113883.10.20.17.3.54
Sodium serum
2.16.840.1.113883.10.20.17.3.36
Systolic blood pressure
2.16.840.1.113883.10.20.17.3.27
Urine output
2.16.840.1.113883.10.20.17.3.55
White blood cell (leukocytes)
2.16.840.1.113883.10.20.17.3.40
Discharge activity - Neonatal
2.16.840.1.113883.10.20.17.3.13
Inborn/outborn
2.16.840.1.113883.10.20.17.3.7
Nothing by mouth (NPO)
2.16.840.1.113883.10.20.17.3.56
Oxygenation index
2.16.840.1.113883.10.20.17.3.22
PaO2/FIO2 ratio
2.16.840.1.113883.10.20.17.3.18
Renal dialysis (renal replacement therapy)
2.16.840.1.113883.10.20.17.3.57
Reporting parameters act
2.16.840.1.113883.10.20.17.3.8
Respiratory or ventilatory support
2.16.840.1.113883.10.20.17.3.25
Respiratory severity score
2.16.840.1.113883.10.20.17.3.23
Steroid treatment (systemic)
2.16.840.1.113883.10.20.17.3.58
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 78
January 2010
APPENDIX C — SUMM ARY OF V ALUE SET S
The following table summarizes the value sets used in this Neonatal Care Report Implementation Guide at the time of
publishing. (Note: changes in display name and NOT code reflect a request in the display name change ONLY)
Table 4: Summary of Value Sets
valueSetOID
Description
code
displayName
codeSystem
Code
System
Name
A valueSet of SNOMED
and LOINC codes for the
1 minute Apgar
169895004
Apgar at 1 minute
2.16.840.1.113883.6.96
SNOMED
48334-7
Apgar panel^1M post
birth
2.16.840.1.113883.6.1
LOINC
169909004
Apgar at 5 minute
2.16.840.1.113883.6.96
SNOMED
48333-9
Apgar panel^5M post
birth
2.16.840.1.113883.6.1
LOINC
169922007
Apgar at 10 minute
2.16.840.1.113883.6.96
SNOMED
48332-1
Apgar panel^10M post
birth
2.16.840.1.113883.6.1
LOINC
443848000
Apgar at 15 minute
2.16.840.1.113883.6.96
SNOMED
443849008
Apgar at 20 minute
2.16.840.1.113883.6.96
SNOMED
169876006
Birth head circumference
2.16.840.1.113883.6.96
SNOMED
8290-9
Circumference.occipitalfrontal^at birth
2.16.840.1.113883.6.1
LOINC
(localValueSetName)
2.16.840.1.113883.11.20.5.16
Apgar 1 minute post birth
2.16.840.1.113883.11.20.5.17
Apgar 5 minutes post birth
2.16.840.1.113883.11.20.5.1
(Apgar Summary Score
(prolonged))
2.16.840.1.113883.11.20.5.19
(Birth head circumference)
A valueSet of SNOMED
and LOINC codes for the
5 minute Apgar
A valueSet of SNOMED
codes for the 10, 15 and
20 minute summary
scores that are recorded
in an extended neonatal
resuscitation
A valueSet of SNOMED
and LOINC codes for
birth head circumference
valueSetOID
Description
code
displayName
codeSystem
Code
System
Name
A valueSet of SNOMED
and LOINC codes for
birth weight
47340003
Birth weight
2.16.840.1.113883.6.96
SNOMED
56056-5
Body weight^at birth
(reported)
2.16.840.1.113883.6.1
LOINC
8339-4
Body weight^at birth
(measured)
2.16.840.1.113883.6.1
LOINC
(localValueSetName)
2.16.840.1.113883.11.20.5.15
(Birth weight)
2.16.840.1.113883.11.20.5.18
(Body weight)
A valueSet of SNOMED
and LOINC codes for
measured body weight
27113001
Body weight
2.16.840.1.113883.6.96
SNOMED
3141-9
Body weight (measured)
2.16.840.1.113883.6.1
LOINC
2.16.840.1.113883.11.20.5.2
(Body temperature)
A valueSet of applicable
SNOMED body
temperature codes for
neonatal ICU
386725007
Body temperature
2.16.840.1.113883.6.96
SNOMED
8310-5
Body Temperature
2.16.840.1.113883.6.1
LOINC
276885007
Core body temperature
2.16.840.1.113883.6.96
SNOMED
415882003
Axillary temperature
2.16.840.1.113883.6.96
SNOMED
307047009
Rectal temperature
2.16.840.1.113883.6.96
SNOMED
364537001
Temperature of skin
2.16.840.1.113883.6.96
SNOMED
2.16.840.1.113883.11.20.5.21
(Diastolic blood pressure)
A valueSet of SNOMED
and LOINC codes for
diastolic blood pressure
271650006
Diastolic blood pressure
2.16.840.1.113883.6.96
SNOMED
8462-4
Intravascular
diastolic:Pres
2.16.840.1.113883.6.1
LOINC
2.16.840.1.113883.11.20.5.22
(Mean blood pressure)
A valueSet of SNOMED
and LOINC codes for
mean blood pressure
6797001
Mean blood pressure
2.16.840.1.113883.6.96
SNOMED
8478-0
Intravascular mean:Pres
2.16.840.1.113883.6.1
LOINC
2.16.840.1.113883.11.20.5.20
(Systolic blood pressure)
A valueSet of SNOMED
and LOINC codes for
systolic blood pressure
271649006
Systolic blood pressure
2.16.840.1.113883.6.96
SNOMED
8480-6
Intravascular systolic:Pres
2.16.840.1.113883.6.1
LOINC
2.16.840.1.113883.11.20.5.23
(Respiratory rate)
A valueSet of SNOMED
and LOINC codes for
respiratory rate
86290005
Respiratory rate
2.16.840.1.113883.6.96
SNOMED
9279-1
Breaths:Nrat
2.16.840.1.113883.6.1
LOINC
2.16.840.1.113883.11.20.5.3
(Respiratory/Ventilatory
Support Modes)
A valueSet of applicable
SNOMED procedure
codes relating to types of
ventilation
233573008
ECMO - Extracorporeal
membrane oxygenation
2.16.840.1.113883.6.96
SNOMED
243153009
High frequency positive
pressure ventilation
2.16.840.1.113883.6.96
SNOMED
243154003
High frequency jet
2.16.840.1.113883.6.96
SNOMED
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 80
January 2010
valueSetOID
Description
code
displayName
codeSystem
Code
System
Name
(localValueSetName)
ventilation
2.16.840.1.113883.11.20.5.4
(Lactic acid/lactate)
A valueSet of applicable
lab LOINC lactate codes
2.16.840.1.113883.11.20.5.5
(Ionized Calcium)
A valueSet of applicable
lab LOINC ionized
calcium codes
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
243155002
High frequency oscillatory
ventilation
2.16.840.1.113883.6.96
SNOMED
243147009
Controlled ventilation
2.16.840.1.113883.6.96
SNOMED
182687005
Intermittent positive
pressure ventilation
2.16.840.1.113883.6.96
SNOMED
286813003
Pressure controlled SIMV
2.16.840.1.113883.6.96
SNOMED
59427005
Synchronized intermittent
mandatory ventilation
2.16.840.1.113883.6.96
SNOMED
229312009
Nasal ventilation therapy
2.16.840.1.113883.6.96
SNOMED
47545007
CPAP - Continuous
positive airway pressure
therapy
2.16.840.1.113883.6.96
SNOMED
266700009
Ventilation assistance
2.16.840.1.113883.6.96
SNOMED
2524-7
Lactate Ser/Plas
2.16.840.1.113883.6.1
LOINC
32693-4
Lactate Bld
2.16.840.1.113883.6.1
LOINC
17863-2
Calcium.ionized
[Mass/volume] in Serum
or Plasma
17864-0
Calcium.ionized
[Mass/volume] in Serum
or Plasma by Ion-selective
membrane electrode (ISE)
2.16.840.1.113883.6.1
38230-9
Calcium.ionized
[Mass/volume] in Blood
2.16.840.1.113883.6.1
1994-3
Calcium.ionized
[Moles/volume] in Blood
2.16.840.1.113883.6.1
1995-0
Calcium.ionized
[Moles/volume] in Serum
or Plasma
2.16.840.1.113883.6.1
12180-6
Calcium.ionized
[Moles/volume] in Serum
2.16.840.1.113883.6.1
Page 81
January 2010
LOINC
2.16.840.1.113883.6.1
LOINC
LOINC
LOINC
LOINC
LOINC
valueSetOID
Description
code
displayName
codeSystem
(localValueSetName)
Code
System
Name
or Plasma by Ion-selective
membrane electrode (ISE)
2.16.840.1.113883.11.20.5.6
(White blood cell count)
2.16.840.1.113883.11.20.5.7
(Platelet)
2.16.840.1.113883.11.20.5.8
(Fibrinogen)
2.16.840.1.113883.11.20.5.9
(International Normalized
Ratio (INR))
A valueSet of applicable
lab LOINC white count
codes
A valueSet of applicable
lab LOINC platelet count
codes
A valueSet of applicable
lab LOINC fibrinogen
level codes
A valueSet of applicable
lab LOINC International
Normalized Ratio (INR)
codes
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
47596-2
Calcium.ionized
[Moles/volume] in Blood
by Ion-selective
membrane electrode (ISE)
LOINC
2.16.840.1.113883.6.1
26464-8
Leukocytes [#/volume] in
Blood
2.16.840.1.113883.6.1
6690-2
Leukocytes Bld Qn
Automated count
2.16.840.1.113883.6.1
26515-7
Platelets Bld
2.16.840.1.113883.6.1
LOINC
49497-1
Platelets Bld Estimate
2.16.840.1.113883.6.1
LOINC
777-3
Platelets [#/volume] in
Blood by Automated
count
LOINC
LOINC
LOINC
2.16.840.1.113883.6.1
30902-1
Fibrinogen [Mass/volume]
in Platelet poor plasma by
Heat denaturation
2.16.840.1.113883.6.1
LOINC
3255-7
Fibrinogen [Mass/volume]
in Platelet poor plasma by
Coagulation assay
2.16.840.1.113883.6.1
LOINC
55452-7
Fibrinogen in Platelet
poor plasma
2.16.840.1.113883.6.1
LOINC
34714-6
INR in Blood by
Coagulation assay
2.16.840.1.113883.6.1
LOINC
Page 82
January 2010
valueSetOID
Description
code
displayName
codeSystem
Code
System
Name
52129-4
INR in Platelet poor
plasma by Coagulation
assay --post heparin
2.16.840.1.113883.6.1
LOINC
6301-6
INR in Platelet poor
plasma by Coagulation
assay
2.16.840.1.113883.6.1
LOINC
46418-0
INR in Capillary blood by
Coagulation assay
2.16.840.1.113883.6.1
LOINC
A valueSet of applicable
lab LOINC hemoglobin
codes
718-7
Hemoglobin
[Mass/volume] in Blood
2.16.840.1.113883.6.1
LOINC
20509-6
Hemoglobin
[Mass/volume] in Blood
by calculation
2.16.840.1.113883.6.1
LOINC
A valueSet of applicable
lab LOINC albumin codes
1751-7
Albumin [Mass/volume]
in Serum or Plasma
2.16.840.1.113883.6.1
LOINC
2862-1
Albumin [Mass/volume]
in Serum or Plasma by
Electrophoresis
2.16.840.1.113883.6.1
LOINC
3094-0
Urea nitrogen
[Mass/volume] in Serum
or Plasma
2.16.840.1.113883.6.1
LOINC
6299-2
Urea nitrogen
[Mass/volume] in Blood
2.16.840.1.113883.6.1
LOINC
A valueSet of applicable
SNOMED frequency
qualifier codes
260413007
None
2.16.840.1.113883.6.96
SNOMED
50607009
Single
2.16.840.1.113883.6.96
SNOMED
255204007
Multiple
2.16.840.1.113883.6.96
SNOMED
A valueSet of applicable
systemic steroid
medication codes
N0000175576
Corticosteroid [EXT]
2.16.840.1.113883.3.26.1.5
ND FRT
3264
Dexamethasone
2.16.840.1.113883.6.88
RxNorm
5492
Hydrocortisone
2.16.840.1.113883.6.88
RxNorm
8640
Prednisone
2.16.840.1.113883.6.88
RxNorm
8638
Prednisolone
2.16.840.1.113883.6.88
RxNorm
(localValueSetName)
2.16.840.1.113883.11.20.5.10
(Hemoglobin)
2.16.840.1.113883.11.20.5.11
(Albumin)
2.16.840.1.113883.11.20.5.12
(Blood Urea Nitrogen (BUN))
2.16.840.1.113883.11.20.5.13
(Seizure frequency)
2.16.840.1.113883.11.20.5.14
(Systemic steroids)
A valueSet of applicable
lab LOINC BUN codes
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 83
January 2010
valueSetOID
Description
code
displayName
codeSystem
Code
System
Name
6902
methylprednisolone
2.16.840.1.113883.6.88
RxNorm
1086007
Female
2.16.840.1.113883.6.96
SNOMED
10052007
Male
2.16.840.1.113883.6.96
SNOMED
37791004
Indeterminate
2.16.840.1.113883.6.96
SNOMED
F
Female
2.16.840.1.113883.5.1
HL7
AdministrativeGender
M
Male
2.16.840.1.113883.5.1
HL7
AdministrativeGender
UN
Undifferentiated
2.16.840.1.113883.5.1
HL7
AdministrativeGender
(localValueSetName)
2.16.840.1.113883.11.20.5.24
(NCR gender)
A valueSet of both the
HL7
administrativeGender
codes valueSet and
HITSP foundations sex
structure codes valueSet
2.16.840.1.113883.11.20.5.25
(Heart rate)
A valueSet of SNOMED
and LOINC codes for
heart rate
364075005
Heart rate
2.16.840.1.113883.6.96
SNOMED
8867-4
Heart
beat:NRat:Pt:XXX:Qn:
2.16.840.1.113883.6.1
LOINC
2.16.840.1.113883.11.20.5.26
Head circumference
A valueSet of SNOMED
and LOINC codes for
heart rate
363812007
Head circumference
2.16.840.1.113883.6.96
SNOMED
8287-5
Circumference.occipitalfrontal
2.16.840.1.113883.6.1
LOINC
Implementation Guide for CDA R2
NCR- US Realm
Draft Standard for Trial Use
Release 1
© 2010 Health Level Seven, Inc. All rights reserved.
Page 84
January 2010