Technical Goals and Objectives
advertisement

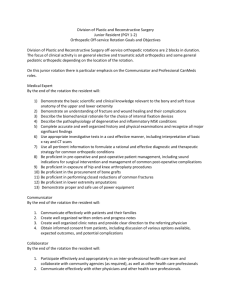
POSTGRADUATE YEAR III Ambulatory - Two Months The ambulatory rotation is designed for the more senior resident to refine his/her skills in management of abnormal cervical/vaginal/vulvar cytology and pathology, reproductive endocrinology and infertility, family planning, and office urogynecology. Learning objectives are both didactic (self-study, rounds and lectures, and patient evaluation) and technical (procedural skills). At the completion of the rotation, the resident is to have read and have an understanding of the didactic objectives outlined below. Technical objectives will be evaluated on an ongoing basis by more senior residents and faculty. Didactic and Management Goals and Objectives The resident should make extensive use of the current literature to apply evidence-based techniques for the rational management of medical and surgical obstetric conditions. All residents have access to online literature (i.e. Up to Date, Medscape, etc) and there are numerous Obstetrics Books (most recent editions) available in the Resident Call Rooms, and the Resident Clinic. In addition, all of the clinical sites have full service medical libraries with the more recent OB/GYN journals available. Technical Goals and Objectives Technical and procedure experience is an evolutionary process through the four years of training. Residents will be exposed to various procedures commensurate with their level of training. Some procedures will require continued exposure to achieve competence while others will be mastered after minimal exposure Following completion of the rotation, the resident is expected to have, under supervision, experience in: 1. Colposcopy with cervical/vaginal/vulvar biopsy 2. LEEP 3. Cryotherapy 4. Paracervical block 5. Ultrasound for evaluation of infertility/response to treatment 6. IVF 7. ICSI 8. Gamete donation 9. Preimplantation genetic diagnosis 10. Hysterosalpingography 11. Hysterosonography 12. Hysteroscopic submucosal fibroid/polyp resection 13. Hysteroscopic resection of uterine septum 14. Diagnostic laparoscopy 15. Laparoscopic chromopertubation, lysis of adhesions, fulguration/excision of endometriosis, fimbrioplasty, salpingostomy/salpingectomy 16. Metroplasty 17. Tubal anastamoses 18. Vaginal construction/reconstruction 19. Laminaria placement 20. First trimester surgical termination of pregnancy 21. First trimester medical termination of pregnancy 22. Second trimester surgical termination of pregnancy 23. Performance of POP-Q exam 24. Office cystoscopy 25. Bladder instillation 26. Pessary fitting and removal Following completion of the rotation, the resident is expected to have competence in: 1. Colposcopy with cervical/vaginal/vulvar biopsy 2. LEEP 3. Cryotherapy 4. Paracervical block 5. Ultrasound for evaluation of infertility/response to treatment 6. Hysterosonography 7. Hysteroscopic submucosal fibroid/polyp resection 8. Diagnostic laparoscopy 9. Laparoscopic chromopertubation, lysis of adhesions, fulguration/excision of endometriosis, salpingostomy/salpingectomy 10. Laminaria placement 11. First trimester surgical termination of pregnancy 12. First trimester medical termination of pregnancy 13. Early/uncomplicated second trimester surgical termination of pregnancy 14. POP-Q exam 15. Office cystoscopy 16. Bladder instillation 17. Uncomplicated pessary fitting and removal Medical Knowledge A. Colposcopy 1. The resident will understand guidelines for the management of abnormal cervical/vulvar/vaginal cytology and pathology including the role of colposcopy, biopsy, LEEP, cryotherapy, medical management, laser, and excision. B. Reproductive Endocrinology and Infertility 1. The resident will be able to describe the normal embryology of Mullerian and ovarian development, the pathogenesis of abnormal Mullerian development, and the pathogenesis of disorders of sexual differentiation. 2. The resident will be able to describe major developmental anomalies, there implications for sexual function, menstruation, fertility, and reproductive outcome, including: hymenal abnormalities, vaginal agenesis, vaginal septum, uterine septum, and unicornuate or bicornuate uterus. 3. The resident will be able to describe the pharmacology of medications used to: induce ovulation, inhibit ovulation (GNRH agonists and antagonists, steroid contraceptives), inhibit the effects of progesterones (mifepristone), treat hyperprolactinemia, serve as hormonal therapy, and serve as estrogen and progesterone receptor modulators. 4. The resident will be able to describe the clinical features and diagnostic criteria for PCOS, as well as perform an appropriate physical exam. In addition, the resident will understand how to interpret selected tests to determine the diagnosis and to describe appropriate initial management for patients who do and do not desire pregnancy. 5. The resident will be able to describe the causes of galactorrhea/hyperprolactinemia, perform appropriate history and physical exam, order and interpret diagnostic studies (prolactin, TSH, pituitary imaging), initiate treatment, describe long-term follow-up, outline indications for neurosurgical referral, and describe the management of pituitary adenoma in pregnancy. 6. The resident will be able to describe the principal causes of primary and secondary infertility, to elicit a pertinent history and perform a pertinent physical exam, and to interpret diagnostic tests such as basal body temperature, luteal phase progesterone, thyroid function, and prolactin. In addition, the resident will have an understanding of the roles and interpretation of imaging studies and semen analysis. 7. The resident will be able to define precocious puberty, outline principal causes, interpret results of tests such as ultrasonography, gonadotropin assays, and x-ray studies for bone age, and describe treatments and long-term prognosis for these patients. 8. The resident will be understand the principal causes of delayed puberty, perform an appropriate physical exam, interpret related diagnostic tests, and outline indications for referral. 9. The resident will be able to describe common causes of recurrent pregnancy loss, elicit a pertinent history, perform an appropriate physical exam, perform and interpret appropriate diagnostic tests, and provide counseling and treatment as appropriate. 10. The resident will be able to describe the indications, basic procedures, and potential complications of: IVF, GIFT, ZIFT, ICSI, gamete donation,and preimplantation genetic diagnosis. C. Family Planning 1. Discuss available methods of contraception, their relative efficacies, advantages, limitations, non-contraceptive benefits, relative and absolute medical contraindications, and appropriately counsel patients on their proper use. 2. Discuss available methods of emergency contraception and their use. 3. Understand the public health context of safe, elective abortion and describe the various surgical abortion procedures and the gestations for which they are appropriate. 4. Understand options for pain management in surgical abortion. 5. Understand the complications of first and second trimester abortions and their management. 6. Discuss the protocols used for medical abortion and their relative efficacies. 7. Describe side effects and complications associated with medical abortion and their appropriate treatments. 8. Explain the methods of cervical preparation for second trimester abortion including the process of laminaria insertion. 9. Discuss the use of misoprostol and other agents for induction termination in the second trimester and be able to provide appropriate counseling regarding the benefits and disadvantages of induction versus surgical evacuation for elective abortion, IUFD, and fetal anomalies. 10. Explain the process of examining uterine aspirate. 11. Explore ethical questions surrounding abortion and clarify personal feelings about the role of abortion in the resident’s future practice. D. Urogynecology 1. Obtain an appropriate history related to: involuntary los of urine, painful urination, incomplete bladder emptying, frequency, urgency, nocturia, and associated factors such as medications and past medical history. 2. Perform an appropriate physical exam for: involuntary loss of urine, alterations in bladder and urethral support, neurologic disorders, and evidence of infection. 3. Understand the role of diagnostic studies including: urinalysis and culture, post-void residual, physical function tests (valsalva, urethral angle, perineal muscle testing), cystometry, cystourethrography, cystoscopy, and uroflowmetry. 4. Be able to diagnose: disorders of support, structural or traumatic disorders, infection, and incontinence (including stress, urge, overflow, and mixed). 5. Have an understanding of possible interventions including medical, surgical, and behavioral. 6. Understand factors influencing intervention including age, severity of dysfunction, previous therapy, and medical comorbidities. Interpersonal and Communication Skills Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate leadership skills with the junior residents and medical students 2. Promote the team approach of patient care with nursing staff, social workers and all ancillary staff to ensure comprehensive care of the clinic patient 3. Communicate effectively with all patients and their family members both in person and on the phone Professionalism Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate respectfulness and compassion to all patients 2. Demonstrate respectfulness to all staff and allied health workers 3. Demonstrate respectfulness to all other residents and faculty members 4. Complete and fulfill responsibilities and respond promptly when paged 5. Demonstrate honesty and integrity when interacting with patients and staff 6. Accept responsibility for patient care and management plans 7. Accept the teaching responsibilities of all junior residents and medical student Systems Based Practice Following completion of this rotation, the resident is expected to be able to: 1. Be familiar with billing codes for common outpatient conditions and procedures 2. Identify system issues that contribute to poor patient care 3. Be familiar with home health care systems and community agencies that can improve patient care 4. Effectively utilize systematic approaches to reduce errors and improve patient care 5. Effectively utilize hospital resources and outside resources to improve patient care Practice Based Learning Following completion of this rotation, the resident is expected to be able to: 1. Effectively utilize technology to manage information for patient care and self improvement 2. Know the essential books associated with the management of the outpatient 3. Know how the access ACOG Bulletins, Committee Opinions regarding the standards of practice 4. Know how to access all online services to obtain pertinent up to date information regarding outpatient issues Evaluations The PG III resident rotating on the Ambulatory service is evaluated using 360 evaluations. They are evaluated by their faculty, their patients, the ancillary staff, the junior residents and themselves. The Ambulatory faculty completes the summative evaluations at the end of the rotation. The evaluations are done based on the core competencies as outlined in the Goals and Objectives that are listed above for this rotation. Self evaluations are used to determine whether or not a resident achieved competency with the management of specific outpatient conditions. Reading Assingments: Comprehensive Gynecology: Morton A. Stenchever, MD (Author), William Droegemueller, MD (Author), Arthur L. Herbst, MD (Author), Daniel Mishell Jr. MD (Author) Clinical Urogynecology -Mickey M. Karram, MD and Mark D.Walters, MD Clinical Gynecologic Endocrinology and Infertility: Leon Speroff (Author), Marc A. Fritz (Author) ACOG Compendium and Committee Opinions Hormonal Contraception in Women with Co-existing Medical Conditions Management of Infertility Caused by Ovulatory Dysfunction Emergency Contraception Medical Management of Abortion Intrauterine Device Additional reading assignments will be given by ambulatory instructors POSTGRADUATE YEAR THREE Continuity Clinic - Weekly The goals and objectives of the weekly continuity clinic at the PG-III level are to foster a continuum of care across primary care, obstetrical, and gynecologic practice. The PG-III resident should be able to counsel and screen patients for all primary care conditions across all age groups. The resident will further have a thorough understanding of preoperative management for all gynecologic surgery. By the completion of the third year the resident should be able to manage all antepartum high risk conditions with minimal supervision from faculty. Learning objectives are both didactic (self reading, rounds and lectures, and patient evaluation) and technical (procedural skills). At the completion of the rotation, the resident is to have read and have an understanding of the didactic objectives outlined below. These objectives, whether covered during lecture, rounds, conference, or resident self learning are to be considered a minimum for resident learning during the rotation. Technical objectives will be evaluated on an ongoing basis by more senior residents and faculty. Didactic and Management Goals and Objectives No specific didactic and management goals and objectives are set for this rotation with the exception of continued learning in the area of geriatric and adolescent medicine. Residents are expected to read from appropriate sources regarding their continuity patients. All residents have access to online literature (i.e. Up to Date, Medscape, etc) and there are numerous books in the resident clinic for use at all times. Technical Goals and Objectives The resident may enhance or complete the technical goals and objectives outlined for the Family Health Center rotation at the completion of the PG-III continuity experience. 1. Vulvar biopsy. 2. Ultrasonography, vaginal and abdominal. 3. Cautery and cryotherapy. 4. IUD insertion. 5. Fitting of pessary. 6. Implanon insertion and removal. Medical Knowledge A. The resident will have a thorough understanding of preconceptual care including: 1. History and assessment of risk factors to including genetic abnormalities by pedigree analysis, effects of pregnancy on chronic medical conditions, effects of chronic medical conditions on pregnancy, potential teratogenicity of prescribed and illicit substances, and alternatives to traditional pregnancy 2. Possible interventions in high risk pregnancy such as modification of lifestyle, infertility or genetic counseling, and appropriate medical and preventive interventions 3. Risk-benefit implications of various interventions or non-interventions including alterations in cardiovascular health, carbohydrate metabolism, risk of prematurity, disorders of intrauterine growth, late pregnancy bleeding abnormalities, and risk of operative delivery B. The resident will have a thorough understanding of the concepts of genetic counseling including: 1. Pedigree analysis, advanced maternal/paternal age, teratogen exposure, ethnic and racial background, recessive disorders including X-linked and autosomal, dominant disorders including X-linked and autosomal, balanced translocations, recurrent spontaneous abortion, multi-factorial disorders, and disorders of metabolism. 2. The resident will have a thorough knowledge of common genetic disorders including Trisomy-21, Trisomy-18, Trisomy-13, 47 XXY, 45 X, congenital adrenal hyperplasia, fragile X syndrome, cystic fibrosis, sickle cell disease, and Tay-Sachs disease 3. Physical characteristics that may indicate genetic disorder including IUGR, oligohydramnios, and polyhydramnios 4. Diagnostic studies including serum screening and nuchal translucency measurement and targeted screening based on family history and maternal age 5. Amniocentesis, chorionic villus sampling, and PUBS 6. Diagnosis and work-up for fetal death including post-mortem exam, photographs, genetic studies, amniocentesis, maternal laboratory testing, post-mortem imaging, and autopsy. 7. Possible interventions including medical, surgical, and preconception counseling 8. Follow-up including management plan for specific diagnosis and education and counseling. C. The resident should be able to evaluate the geriatric patient for preoperative and postoperative care including: 1. Returning the patient to maximum functional capacity following surgery. 2. Evaluating the effectiveness of diminished physiologic reserve and the potential effects of anesthesia, surgery, and medical comorbidities. D. The resident will have a thorough understanding of preoperative evaluation and management including: 1. Assessment of functional reserve 2. Assessment of cognitive, nutritional, and functional status 3. Assessment of host and hospital risk factors for delirium 4. Assessment of medical comorbidities 5. Assessment of socioeconomic status and resources including availability of necessary postoperative family and household aid services. 6. Patient education, informed consent, and advanced directives. 7. Complete medication review including preoperative medications for medical optimization and risk reduction E. The resident will have a thorough understanding of operative management and anesthesia including: 1. Choice of anesthesia selection and age-associated alterations in morbidity and mortality with general and regional techniques 2. Appropriate patient positioning and padding to avoid injury 3. Prevention of intraoperative hypothermia 4. Thromboembolic prophylaxis F. The resident will have a thorough understanding of postoperative management including: 1. The concept of early mobilization 2. Appropriate fluid and electrolyte management in the elderly 3. Pain management and its alterations in the geriatric patient 4. Understanding, recognition, prevention, and treatment of behavioral and mental changes 5. Initiation of rehabilitation and fall prevention 6. Appropriate consultation with physical therapy, occupational therapy, pain management, and nutrition services 7. Initiation of discharge planning including caregiver education, household assistance, home health consultation, and skilled nursing care. G. The resident will have an understanding of the impact on aging and communication skills and interpersonal interactions including: 1. The effect of nihilist and ageist attitudes of physicians, caregivers, and family members 2. Identification of pitfalls specific to communication with older patients including visual and hearing defects 3. Quality of life concerns including independence and autonomy issues 4. Techniques to improve patient comprehension and task performance. H. The resident will have an understanding of the common diseases, disorders, and health concerns of the aging woman including: 1. Cardiovascular disease 2. Nutrition and malnutrition 3. Cognitive impairment including Alzheimer’s and vascular dementia 4. Delirium 5. Depression, anxiety, grieving, and bereavement 6. Urinary incontinence 7. Bowel dysfunction 8. Sleep disorders. 9. Mobility issues 10. Hearing and visual problems 11. Sexuality Interpersonal and Communication Skills Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate leadership skills with the junior residents and medical students 2. Promote the team approach of patient care with nursing staff, social workers and all ancillary staff to ensure comprehensive care of the clinic patient 4. Supervise the care of all patients at clinic 5. Communicate effectively with all patients and their family members both in person and on the phone Professionalism Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate respectfulness and compassion to all patients 2. Demonstrate respectfulness to all staff and allied health workers 2. Demonstrate respectfulness to all other residents and faculty members 3. Demonstrate honesty and integrity when interacting with patients and staff 4. Accept responsibility for patient care and management plans 5. Accept the teaching responsibilities of all medical students working with RIII Systems Based Practice Following completion of this rotation, the resident is expected to be able to: 1. Be familiar with billing codes for common outpatient conditions and procedures 2. Identify system issues that contribute to poor patient care 3. Be familiar with home health care systems and community agencies that can improve patient care 4. Effectively utilize systematic approaches to reduce errors and improve patient care 5. Effectively utilize hospital resources and outside resources to improve patient care Practice Based Learning Following completion of this rotation, the resident is expected to be able to: 1. Effectively utilize technology to manage information for patient care and self improvement 2. Know the essential books associated with the management of the outpatient 4. Know how the access ACOG Bulletins, Committee Opinions regarding the standards of practice 5. Know how to access all online services to obtain pertinent up to date information regarding outpatient issues Evaluations The PG III resident charts are reviewed to ensure appropriate questions are asked at each type of visit including New OB, Gynecology visits and Annual Well Women exams. Reading Assingments: Comprehensive Gynecology: Morton A. Stenchever, MD (Author), William Droegemueller, MD (Author), Arthur L. Herbst, MD (Author), Daniel Mishell Jr. MD (Author) Clinical Urogynecology -Mickey M. Karram, MD and Mark D.Walters, MD Clinical Gynecologic Endocrinology and Infertility: Leon Speroff (Author), Marc A. Fritz (Author) ACOG Compendium and Committee Opinions Any topic pertinent to patients seen during continuity clinic POSTGRADUATE YEAR THREE Elective– One Month The goal of the PG-III elective rotation is to allow the resident to create a personalized educational and training experience in order to: expand upon the competencies achieved through established rotations, gain exposure to related fields, further research interests, participate in international medicine, and/or to work with mentors in other institutions in preparation for fellowship application. In preparation for the rotation, the resident will establish specific goals and objectives. Progress toward these individualized goals will be evaluated at the end of the rotation. Evaluation The resident will be evaluated by their mentors during their elective rotation POSTGRADUATE YEAR THREE Gynecology UCI – One Month The goals and objectives for the PG-III resident assigned to the UCI gynecology rotation are to enhance skills in operative gynecology with emphasis on abdominal and vaginal hysterectomy, laparoscopy, operative hysteroscopy, and urogynecologic procedures. Following the completion of this rotation, the resident, using the previous gynecologic rotations as a foundation for surgical technique, will develop skills to allow performance of these procedures under minimal faculty supervision in preparation for the fourth year. Learning objectives are both didactic (self-study, rounds and lectures, and patient evaluation) and technical (procedural skills). At the completion of the rotation, the resident is to have read and have an understanding of the didactic objectives outlined below. These objectives, whether covered during lecture, rounds, conference, or resident self learning, are to be considered a minimum for resident learning during the rotation. Technical objectives will be evaluated on an ongoing basis by more senior residents and faculty. Didactic and Management Goals and Objectives The resident should make extensive use of the current literature to apply evidence-based techniques for the rational management of medical and surgical obstetric conditions. All residents have access to online literature (i.e. Up to Date, Medscape, etc) and there are numerous Obstetrics Books (most recent editions) available in the Resident Call Rooms, and the Resident Clinic. In addition, all of the clinical sites have full service medical libraries with the more recent OB/GYN journals available. Technical Goals and Objectives Technical and procedure experience is an evolutionary process through the four years of training. Residents will be exposed to various procedures commensurate with their level of training. Some procedures will require continued exposure to achieve competence while others will be mastered after minimal exposure. Following completion of the rotation, the resident is expected to have had, under supervision, experience in: 1. Abdominal hysterectomy with and without adnexal removal 2. Vaginal hysterectomy with and without adnexal removal 3. Laparoscopic assisted vaginal hysterectomy 4. Total laparoscopic hysterectomy 5. Burch/MMK procedures 6. Operative laparoscopy 7. Abdominal, laparoscopic, and vaginal myomectomy 8. Diagnostic and operative hysteroscopy 9. Non-hysteroscopic endometrial ablation procedures 10. Anterior and posterior colporrhaphy 11. Pelvic floor suspension procedures 12. Vesicovaginal fistula repair 13. Rectovaginal fistula repair 14. Robotic surgery 15. Interstim procedures 16. Second trimester surgical termination of pregnancy Following completion of this rotation, the resident is expected to have begun establishing competency in the following procedures: 1. Abdominal hysterectomy with and without adnexal removal 2. Vaginal hysterectomy with and without adnexal removal 3. Laparoscopic assisted vaginal hysterectomy 4. Total laparoscopic hysterectomy 5. Operative laparoscopy 6. Abdominal, laparoscopic, and vaginal myomectomy 7. Diagnostic and operative hysteroscopy 8. Non-hysteroscopic endometrial ablation procedures 9. Anterior and posterior colporrhaphy 10. Pelvic floor suspension procedures 11. Second trimester surgical termination of pregnancy Medical Knowledge A. The resident will have a thorough understanding of operative techniques and complications of total abdominal hysterectomy including: 1. Preservation or removal of adnexa 2. Techniques for management of the cuff 3. Exposure of the ureters 4. Repair of incidental bowel injury 5. Repair of incidental cystotomy B. The resident will have a thorough understanding of operative techniques and complications of vaginal hysterectomy including: 1. Removal of adnexa 2. Cuff closure 3. Repair of enterocoele 4. Morcellation techniques C. The resident will have a thorough understanding of operative techniques and complications of laparoscopic assisted vaginal hysterectomy and total laparoscopic hysterectomy D. The resident will have a thorough understanding of operative techniques and complications of abdominal incontinence procedures including: 1. Anatomy of the space of retzious 2. Burch/MMK procedures 3. Sling procedures 4. Complications of the above techniques E. The resident will have a thorough understanding of operative techniques and complications of laparoscopic adnexal surgery including: 1. Oophorectomy 2. Cystectomy and ectopic pregnancy F. The resident will have a thorough understanding of operative techniques and complications of open, laparoscopic, and vaginal myomectomy G. The resident will have a thorough understanding of operative techniques and complications of diagnostic and operative hysteroscopy, as well as non-hysteroscopic endometrial ablation techniques H. The resident will have a thorough understanding of operative techniques and complications of cystocele and rectocele repair I. The resident will have a thorough understanding of operative techniques and complications of uterine and pelvic floor suspension procedures J. The resident will have a thorough understanding of operative techniques and complications of repair of vesicovaginal and rectovaginal fistulas K. The resident will have a thorough understanding of the diagnosis and management of pelvic support defects including: 1. Historical factors of pelvic pressure, difficulty in voiding or defecating, pain or discomfort, and bulge in the vagina 2. Physical examination findings of partial or complete procidentia, herniation of bladder, urethra or rectum, herniation of abdominal contents in the rectovaginal space, gaping vaginal introitus, and loss of muscular perineal support 3. Diagnostic studies including valsalva maneuver, erect anatomic assessment, and tenaculum traction on the cervix 4. Diagnosis of uterine procidentia, cystocele, cystourethrocele, enterocele, rectocele, and healed vaginal and perineal lacerations 5. Possible management interventions including lifestyle, hormonal, exercise, pessary, and surgical treatment 6. Factors influencing decisions regarding intervention including patient preference, age, desire for future fertility, severity of symptoms, degree of disability, and presence of medical comorbidities 7. Potential complications of intervention including bleeding, injury to adjacent tissue, prolapse, urinary or fecal incontinence, and fistula formation 8. Potential complications of non-intervention including progression of symptoms and disability, sexual and social dysfunction, and inability to void or defecate without splinting 9. Follow-up including post-op and non-operative assessment, patient education and counseling L. The resident will have a thorough understanding of second trimester surgical termination of pregnancy including patient counseling, preoperative preparation, surgical technique, and management of complications. M. The resident will be introduced to robotic surgery and begin to develop an understanding of its technique, indications, complications, and limitations. INTERPERSONAL AND COMMUNICATION SKILLS Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate leadership skills with the junior residents and medical students 2. Promote the team approach of patient care with nursing staff, social workers and all ancillary staff to ensure comprehensive care of the gynecologic patient 3. Communicate effectively with other services and the ER regarding consultations 4. Coordinate the care of all patients on the Gynecology service 5. Communicate effectively with all patients—in particular difficult patients PROFESSIONALISM Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate respectfulness and compassion to all patients 2. Demonstrate respectfulness to all staff and allied health workers 3. Demonstrate respectfulness to all other residents and faculty members 4. Complete and fulfill responsibilities and respond promptly when on call or paged 5. Demonstrate honesty and integrity when interacting with patients and staff 6. Accept responsibility for patient care and management plans 7. Accept the teaching responsibilities of all junior residents and medical students 8. Communicate effectively with other services and the ER regarding consultations 9. Coordinate the care of all patients on the Gynecology service along with the Attending SYSTEMS BASED PRACTICE Following completion of this rotation, the resident is expected to be able to: 1. Be familiar with billing codes for common gynecologic procedures 2. Identify system issues that contribute to poor patient care 3. Be familiar with home health care systems and agencies that can assist patients at home 4. Effectively utilize systematic approaches to reduce errors and improve patient care 5. Effectively utilize hospital resources and outside resources to improve patient care PRACTICE BASED LEARNING Following completion of this rotation, the resident is expected to be able to: 1. Effectively utilize technology to manage information for patient care and self improvement 2. Know the essential books associated with the management of Gynecologic surgeries and Management of Gynecologic Issues 3. Prepare cases for stats presentations 4. Know how the access ACOG Bulletins, Committee Opinions regarding the standards of practice 5. Know how to access all online services to obtain pertinent up to date information regarding Gynecologic issues and management Evaluations The PG III resident rotating on the Gynecology service is evaluated using 360 evaluations. They are evaluated by their faculty, their patients, the ancillary staff, the junior residents and themselves. The Gynecology and the Urogynecology faculty complete the summative evaluations at the end of the rotation. The evaluations are done based on the core competencies as outlined in the Goals and Objectives that are listed above for this rotation. Self evaluations are used to determine whether or not a resident achieved competency with the management of a specific gynecologic disorder or had only exposure to a specific disorder or procedure. Reading Assignments: TeLinde's Operative Gynecology: John A. Rock (Editor), Howard W Jones (Editor) Comprehensive Gynecology: Morton A. Stenchever, MD, William Droegemueller, MD, Arthur L. Herbst, MD, Daniel Mishell Jr. MD (Authors) Normal Pelvic Floor Anatomy- K. Strohbehn, MD Clinical Urogynecology -Mickey M. Karram, MD and Mark D.Walters, MD Willaims Gynecology Clinical Gynecologic Endocrinology and Infertility: Leon Speroff (Author), Marc A. Fritz (Author) ACOG Compendium and Committee Opinions Chronic Pelvic Pain Urinary Incontinence Antibiotic Propylaxis for GYN procedures Pelvic Organ Prolapse Medical and Surgical Management of Tubal Pregnancy Surgical Alternatives to Hysterectomy in the management of leiomyomas Management of Adnexal Masses Management of Anovulaory Bleeding POSTGRADUATE YEAR THREE-Kaiser Irvine Gynecology Kaiser – Two Months The goals and objectives for the PG-III resident assigned to the Kaiser gynecology rotation are to further enhance skills in operative gynecology with emphasis on abdominal and vaginal hysterectomy, laparoscopy, operative hysteroscopy, and urogynecologic procedures. In addition, the rotation is designed to further exposure in the area of gynecologic oncology. Following the completion of this rotation, the resident, using the previous gynecology rotations as a foundation for surgical technique, will develop skills to allow performance of these procedures under minimal faculty supervision in preparation for the fourth year. Learning objectives are both didactic (self-study, rounds and lectures, and patient evaluation), and technical (procedural skills). At the completion of the rotation, the resident is to have read and have an understanding of the didactic objectives outlined below. These objectives, whether covered during lecture, rounds, conference, or resident self learning, are to be considered a minimum for resident learning during the rotation. Technical objectives will be evaluated on an ongoing basis by more senior residents and faculty. Didactic and Management Goals and Objectives The resident should make extensive use of the current literature to apply evidence-based techniques for the rational management of clinic patients and conditions. All residents have access to online literature (i.e. Up to date, Medscape, etc) and there are numerous Obstetric and Gynecologic books available in call rooms. In addition, there is a full service medical library with the most recent Ob/Gyn articles available. Technical Goals and Objectives Technical and procedure experience is an evolutionary process through the four years of training. Residents will be exposed to various procedures commensurate with their level of training. Some procedures will require continued exposure to achieve competence while others will be mastered after minimal exposure. Following completion of the rotation, the resident is expected to have had, under supervision, experience in: 1. Abdominal hysterectomy with and without adnexal removal 2. Vaginal hysterectomy with and without adnexal removal 3. Laparoscopic assisted vaginal hysterectomy 4. Total laparoscopic hysterectomy 5. Burch/MMK procedures 6. Operative laparoscopy 7. Abdominal, laparoscopic, and vaginal myomectomy 8. Diagnostic and operative hysteroscopy 9. Non-hysteroscopic endometrial ablation procedures 10. Anterior and posterior colporrhaphy 11. Pelvic floor suspension procedures 12. Vesicovaginal fistula repair 13. Rectovaginal fistula repair 14. Cystoscopy 15. Radical hysterectomy 16. Staging and debulking procedures for ovarian/peritoneal malignancy 17. Lymph node dissection 18. Vulvectomy 19. Laser procedures of the vulva/vagina 20. Cervical conization Following completion of this rotation, the resident is expected to have begun establishing competency in the following procedures: 1. Abdominal hysterectomy with and without adnexal removal 2. Vaginal hysterectomy with and without adnexal removal 3. Laparoscopic assisted vaginal hysterectomy 4. Total laparoscopic hysterectomy 5. Operative laparoscopy 6. Abdominal, laparoscopic, and vaginal myomectomy 7. Diagnostic and operative hysteroscopy 8. Non-hysteroscopic endometrial ablation procedures 9. Anterior and posterior colporrhaphy 10. Pelvic floor suspension procedures 11. Cystoscopy 12. Cervical conization Medical Knowledge A. The resident will have a thorough understanding of operative techniques and complications of total abdominal hysterectomy including: 1. Preservation or removal of adnexa 2. Techniques for management of the cuff 1. Exposure of the ureters 2. Repair of incidental bowel injury 3. Repair of incidental cystotomy B. The resident will have a thorough understanding of operative techniques and complications of vaginal hysterectomy including: 1. Removal of adnexa 2. Cuff closure 3. Repair of enterocele 4. Morcellation techniques C. The resident will have a thorough understanding of operative techniques and complications of laparoscopic assisted vaginal hysterectomy and total laparoscopic hysterectomy D. The resident will have a thorough understanding of operative techniques and complications of abdominal incontinence procedures including: 1. Anatomy of the space of retzius 2. Burch/MMK procedures 3. Sling procedures 4. Complications of the above techniques E. The resident will have a thorough understanding of operative techniques and complications of laparoscopic adnexal surgery including: 1. Oophorectomy 2. Cystectomy and ectopic pregnancy F. The resident will have a thorough understanding of operative techniques and complications of open, laparoscopic, and vaginal myomectomy G. The resident will have a thorough understanding of operative techniques and complications of diagnostic and operative hysteroscopy, as well as non-hysteroscopic endometrial ablation techniques H. The resident will have a thorough understanding of operative techniques and complications of cystocele and rectocele repair I. The resident will have a thorough understanding of operative techniques and complications of uterine and pelvic floor suspension procedures J. The resident will have a thorough understanding of operative techniques and complications of repair of vesicovaginal and rectovaginal fistulas K. The resident will have a thorough understanding of the diagnosis and management of pelvic support defects including: 1. Historical factors of pelvic pressure, difficulty in voiding or defecating, pain or discomfort, and bulge in the vagina 2. Physical examination findings of partial or complete procidentia, herniation of bladder, urethra or rectum, herniation of abdominal contents in the rectovaginal space, gaping vaginal introitus, and loss of muscular perineal support 3. Diagnostic studies including valsalva maneuver, erect anatomic assessment, and tenaculum traction on the cervix 4. Diagnosis of uterine procidentia, cystocele, cystourethrocele, enterocele, rectocele, and healed vaginal and perineal lacerations 5. Possible management interventions including lifestyle, hormonal, exercise, pessary, and surgical treatment 6. Factors influencing decisions regarding intervention including patient preference, age, desire for future fertility, severity of symptoms, degree of disability, and presence of medical comorbidities 7. Potential complications of intervention including bleeding, injury to adjacent tissue, prolapse, urinary or fecal incontinence, and fistula formation 8. Potential complications of non-intervention including progression of symptoms and disability, sexual and social dysfunction, and inability to void or defecate without splinting 9. Follow-up including post-op and non-operative assessment, and patient education and counseling L. The resident will review the Didactic and Management Goals & Objectives of the R-1 and R-2 gynecologic oncology rotations. Interpersonal and Communication skills Following completion of this rotation, the resident is expected to be able to: 1. Promote the team approach of patient care with nursing staff, social workers and all ancillary staff to ensure comprehensive care of the obstetric and gynecology patient 2. Communicate effectively with other services including ER physicians and staff 3. Communicate effectively with all patients and families—in particular difficult situations Professionalism Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate respectfulness and compassion to all patients 2. Demonstrate respectfulness to all staff and allied health workers 3. Demonstrate respectfulness to all other residents and faculty members 4. Complete and fulfill responsibilities and respond promptly when on call or paged 5. Demonstrate honesty and integrity when interacting with patients and staff 6. Accept responsibility for patient care and management plans 7. Communicate effectively with other services Systems Based Practice Following completion of this rotation, the resident is expected to be able to: 1. Be familiar with billing codes for common obstetric and gynecologic procedures 2. Identify system issues that contribute to poor patient care 3. Effectively utilize systematic approaches to reduce errors and improve patient care 4. Effectively utilize hospital resources and outside resources to improve patient care Practice Based Learning Following completion of this rotation, the resident is expected to be able to: 1. Effectively utilize technology to manage information for patient care and self improvement 2. Know the essential books associated with the management of Obstetrics and Gynecology 3. Know how the access ACOG Bulletins, Committee Opinions regarding the standards of practice 4. Know how to access all online services to obtain pertinent up to date information regarding Obstetric and Gynecologic issues and management Evaluations The PG III resident rotating on the Kaiser service is evaluated using 360 evaluations. They are evaluated by their faculty, their patients, the ancillary staff, and themselves. The Kaiser faculty completes the summative evaluations at the end of the rotation. The evaluations are done based on the core competencies as outlined in the Goals and Objectives that are listed above for this rotation. Self evaluations are used to determine whether or not a resident achieved competency with the management of a specific obstetric and gynecologic cases. Reading Assignments Williams Obstetrics: Cunningham (Author) Obstetrics: Gabbe (Author) TeLinde’s Operative Gynecology: John A. Rock (Editor), Howard W Jones (Editor) Comprehensive Gynecology: Morton A. Stenchever, MD, William Droegemueller, MD, Arthur Herbst, MD, Daniel Mishell Jr. MD (Authors) Clinical Gynecologic Oncology: Disaia and Creasman (Authors) ACOG Compendium and Committee Opinions Surgical Alternatives to Hysterectomy Urinary Incontinence Pelvic Organ Prolapse Antibiotic Prophylaxis for GYN procedures Chronic Pelvic Pain Human Papillomavirus Management of Abnormal Cervical Cytology and Histology Management of the Adnexal Mass POSTGRADUATE YEAR THREE Gynecology Long Beach Memorial – Two Months Gynecology/Ultrasound Long Beach Memorial – Two Months The goals and objectives for the PG-III resident assigned to the Long Beach gynecology rotation are to further enhance skills in operative gynecology with emphasis on abdominal and vaginal hysterectomy, laparoscopy, operative hysteroscopy, and urogynecologic procedures. Following the completion of this rotation, the resident, using the previous gynecology rotations as a foundation for surgical technique, will develop skills to allow performance of these procedures under minimal faculty supervision in preparation for the fourth year. In addition, while on the ultrasound component of the rotation, the resident is expected to further the objectives of the R-1 ambulatory rotation in ultrasound. Learning objectives are both didactic (self-study, rounds and lectures, and patient evaluation) and technical (procedural skills). At the completion of the rotation, the resident is to have read and have an understanding of the didactic objectives outlined below. These objectives, whether covered during lecture, rounds, conference, or resident self learning, are to be considered a minimum for resident learning during the rotation. Technical objectives will be evaluated on an ongoing basis by more senior residents and faculty. Didactic and Management Goals and Objectives The resident should make extensive use of the current literature to apply evidence-based techniques for the rational management of medical and surgical obstetric conditions. All residents have access to online literature (i.e. Up to Date, Medscape, etc) and there are numerous Obstetrics Books (most recent editions) available in the Resident Call Rooms, and the Resident Clinic. In addition, all of the clinical sites have full service medical libraries with the more recent OB/GYN journals available. Technical Goals and Objectives Technical and procedure experience is an evolutionary process through the four years of training. Residents will be exposed to various procedures commensurate with their level of training. Some procedures will require continued exposure to achieve competence while others will be mastered after minimal exposure. Following completion of the rotation, the resident is expected to have had, under supervision, experience in: 1. Abdominal hysterectomy with and without adnexal removal 2. Vaginal hysterectomy with and without adnexal removal 3. Laparoscopic assisted vaginal hysterectomy 4. Total laparoscopic hysterectomy 5. Burch/MMK procedures 6. Operative laparoscopy 7. Abdominal, laparoscopic, and vaginal myomectomy 8. Diagnostic and operative hysteroscopy 9. Non-hysteroscopic endometrial ablation procedures 10. Anterior and posterior colporrhaphy 11. Pelvic floor suspension procedures 12. Vesicovaginal fistula repair 13. Rectovaginal fistula repair Ultrasound component: 1. Detailed fetal anatomic evaluation 2. First trimester fetal ultrasound including nuchal translucency measurement 3. Cervical length measurement 4. Umbilical artery doppler studies 5. MCA doppler studies Following completion of this rotation, the resident is expected to have begun establishing competency in the following procedures: 1. Abdominal hysterectomy with and without adnexal removal 2. Vaginal hysterectomy with and without adnexal removal 3. Laparoscopic assisted vaginal hysterectomy 4. Total laparoscopic hysterectomy 1. Operative laparoscopy 2. Abdominal, laparoscopic, and vaginal myomectomy 3. Diagnostic and operative hysteroscopy 4. Non-hysteroscopic endometrial ablation procedures 5. Anterior and posterior colporrhaphy 6. Pelvic floor suspension procedures Ultrasound component: 1. Detailed fetal anatomic evaluation 2. First trimester fetal ultrasound 3. Cervical length measurement Medical Knowledge A. The resident will have a thorough understanding of operative techniques and complications of total abdominal hysterectomy including: 1. Preservation or removal of adnexa 2. Techniques for management of the cuff 3. Exposure of the ureters 4. Repair of incidental bowel injury 5. Repair of incidental cystotomy B. The resident will have a thorough understanding of operative techniques and complications of vaginal hysterectomy including: 7. Removal of adnexa 8. Cuff closure 9. Repair of enterocele 10. Morcellation techniques C. The resident will have a thorough understanding of operative techniques and complications of laparoscopic assisted vaginal hysterectomy and total laparoscopic hysterectomy. D. The resident will have a thorough understanding of operative techniques and complications of abdominal incontinence procedures including: 1. Anatomy of the space of retzius 2. Burch/MMK procedures 3. Sling procedures 4. Complications of the above techniques E. The resident will have a thorough understanding of operative techniques and complications of laparoscopic adnexal surgery including: 1. Oophorectomy 2. Cystectomy and ectopic pregnancy F. The resident will have a thorough understanding of operative techniques and complications of open, laparoscopic, and vaginal myomectomy. G. The resident will have a thorough understanding of operative techniques and complications of diagnostic and operative hysteroscopy, as well as non-hysteroscopic endometrial ablation techniques. H. The resident will have a thorough understanding of operative techniques and complications of cystocele and rectocele repair. I. The resident will have a thorough understanding of operative techniques and complications of uterine and pelvic floor suspension procedures. J. The resident will have a thorough understanding of operative techniques and complications of repair of vesicovaginal and rectovaginal fistulas. K. The resident will have a thorough understanding of the diagnosis and management of pelvic support defects including: 1. Historical factors of pelvic pressure, difficulty in voiding or defecating, pain or discomfort, and bulge in the vagina 2. Physical examination findings of partial or complete procidentia, herniation of bladder, urethra or rectum, herniation of abdominal contents in the rectovaginal space, gaping vaginal introitus, and loss of muscular perineal support 3. Diagnostic studies including valsalva maneuver, erect anatomic assessment, and tenaculum traction on the cervix 4. Diagnosis of uterine procidentia, cystocele, cystourethrocele, enterocele, rectocele, and healed vaginal and perineal lacerations 5. Possible management interventions including lifestyle, hormonal, exercise, pessary, and surgical treatment 6. Factors influencing decisions regarding intervention including patient preference, age, desire for future fertility, severity of symptoms, degree of disability, and presence of medical comorbidities 7. Potential complications of intervention including bleeding, injury to adjacent tissue, prolapse, urinary or fecal incontinence, and fistula formation 8. Potential complications of non-intervention including progression of symptoms and disability, sexual and social dysfunction, and inability to void or defecate without splinting 9. Follow-up including post-op and non-operative assessment, and patient education and counseling L. While on the ultrasound component of the rotation, the resident will expand understanding of and competency in: fetal anatomic ultrasound including cardiac outflow tracts, first trimester ultrasound, cervical length measurement, umbilical artery doppler studies, and MCA doppler studies. INTERPERSONAL AND COMMUNICATION SKILLS Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate leadership skills with the junior residents and medical students 2. Promote the team approach of patient care with nursing staff, social workers and all ancillary staff to ensure comprehensive care of the gynecologic patient 3. Communicate effectively with other services and the ER regarding consultations 4. Coordinate the care of all patients on the Gynecology service 5. Communicate effectively with all patients—in particular difficult patients PROFESSIONALISM Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate respectfulness and compassion to all patients 2. Demonstrate respectfulness to all staff and allied health workers 3. Demonstrate respectfulness to all other residents and faculty members 4. Complete and fulfill responsibilities and respond promptly when on call or paged 5. Demonstrate honesty and integrity when interacting with patients and staff 6. Accept responsibility for patient care and management plans 7. Accept the teaching responsibilities of all junior residents and medical students 8. Communicate effectively with other services and the ER regarding consultations 9. Coordinate the care of all patients on the Gynecology service along with the Attending SYSTEMS BASED PRACTICE Following completion of this rotation, the resident is expected to be able to: 1. Be familiar with billing codes for common gynecologic procedures 2. Identify system issues that contribute to poor patient care 3. Be familiar with home health care systems and agencies that can assist patients at home 4. Effectively utilize systematic approaches to reduce errors and improve patient care 5. Effectively utilize hospital resources and outside resources to improve patient care PRACTICE BASED LEARNING Following completion of this rotation, the resident is expected to be able to: 1. Effectively utilize technology to manage information for patient care and self improvement 2. Know the essential books associated with the management of Gynecologic surgeries and Management of Gynecologic Issues 3. Know how the access ACOG Bulletins, Committee Opinions regarding the standards of practice 4. Know how to access all online services to obtain pertinent up to date information regarding Gynecologic issues and management Evaluations The PG III resident rotating on the Gynecology service is evaluated using 360 evaluations. They are evaluated by their faculty, their patients, the ancillary staff, the junior residents and themselves. The Gynecology faculty completes the summative evaluations at the end of the rotation. The evaluations are done based on the core competencies as outlined in the Goals and Objectives that are listed above for this rotation. Self evaluations are used to determine whether or not a resident achieved competency with the management of a specific gynecologic disorder or had only exposure to a specific disorder or procedure. Reading Assignments: TeLinde's Operative Gynecology: John A. Rock (Editor), Howard W Jones (Editor) Comprehensive Gynecology: Morton A. Stenchever, MD, William Droegemueller, MD, Arthur L. Herbst, MD, Daniel Mishell Jr. MD (Authors) Normal Pelvic Floor Anatomy- K. Strohbehn, MD Clinical Urogynecology -Mickey M. Karram, MD and Mark D.Walters, MD Willaims Gynecology Clinical Gynecologic Endocrinology and Infertility: Leon Speroff (Author), Marc A. Fritz (Author) ACOG Compendium and Committee Opinions Chronic Pelvic Pain Urinary Incontinence Antibiotic Propylaxis for GYN procedures Pelvic Organ Prolapse Medical and Surgical Management of Tubal Pregnancy Surgical Alternatives to Hysterectomy in the management of leiomyomas Management of Adnexal Masses Management of Anovulaory Bleeding Ultrasonography in Pregnancy Cervical Insufficiency POSTGRADUATE YEAR THREE UCI Nights High Risk Obstetrics – Two Months The goals and objectives for this PG-III rotation are to refine and enhance the skills obtained on the PG-II high risk obstetrical rotations. These skills include medical and surgical management of pregnancy complications, prenatal diagnosis and genetic counseling, and basic obstetrical ultrasound skills. In addition, the resident will further their ultrasound skills under the guidance of perinatal faculty. Learning objectives are both didactic (self-study, rounds and lectures, and patient evaluation) and technical (procedural skills). At the completion of the rotation, the resident is to have read and have an understanding of the didactic objectives outlined below. These objectives, whether covered during lecture, rounds, conference, or resident self learning are to be considered a minimum for resident learning during the rotation. Technical objectives will be evaluated on an ongoing basis by more senior residents and faculty. Didactic and Management Goals and Objectives The resident should make extensive use of the current literature to apply evidence-based techniques for the rational management of medical and surgical obstetric conditions. All residents have access to online literature (i.e. Up to Date, Medscape, etc) and there are numerous Obstetrics Books (most recent editions) available in the Resident Call Rooms, and the Resident Clinic. In addition, all of the clinical sites have full service medical libraries with the more recent OB/GYN journals available. Technical Goals and Objectives Technical and procedure experience is an evolutionary process through the four years of training. Residents will be exposed to various procedures commensurate with their level of training. Some procedures will require continued exposure to achieve competence while others will be mastered after minimal exposure. Following completion of the rotation, the resident is expected to have had, under supervision, experience in: 1. Amniocentesis for prenatal diagnosis and fetal lung maturity 2. External cephalic version 3. Interpretation of NST and CST 4. Biophysical profile 5. Ultrasound for biometry and fetal anatomy 6. Surgical procedures in the pregnant patient 7. Cervical cerclage placement and removal Following completion of this rotation, the resident is expected to be competent in the following procedures: 1. Amniocentesis for prenatal diagnosis and fetal lung maturity 2. Outlet and low operative vaginal delivery 3. Repair of perineal, cervical, vaginal, and rectal lacerations 4. Low transverse, low vertical, and classical cesarean section Medical Knowledge A. The resident will have a thorough understanding of the diagnosis and management of multiple gestation and its complications including: 1. Historical aspects of advanced maternal age, family history, ovulation induction, and ART 2. Physical examination including excessive increase in fundal height and maternal weight gain 3. Diagnostic studies including ultrasound, fetal heart rate testing, amniocentesis for FLM, and genetic studies 4. The impact of multiple gestation on maternal complications such as anemia, early onset hypertensive disorders of pregnancy, PPROM, and preterm labor 5. Diagnostic significance of multiple fetuses, zygocity, fetal anomalies and malpresentation, discordant fetal growth, twin-twin transfusion syndrome, and hydramnios 6. Possible interventions including bed rest, tocolytic therapy, fetal reduction procedures, treatment of twin-twin transfusion syndrome, route of delivery, and delivery of second twin 7. Factors influencing intervention including gestational age, number and presentation of fetuses, zygocity, and preterm labor 8. Potential complications of intervention including prematurity and complications of tocolysis, amniocentesis, and operative delivery 9. Potential complications of non-intervention including prematurity and perinatal morbidity and mortality 10. Follow-up including patient education and counseling, risk factors, and prevention of preterm delivery B. The resident will have experience in external cephalic version including: 1. Timing of procedure 2. Complications including need for immediate cesarean section 3. Prognostic factors for success/failure C. The resident will have experience in isoimmunization in pregnancy including: 1. Historical features of past obstetrical history, blood transfusion, change in consort, isoimmunization risk with regular and irregular antibiotics 2. Diagnostic studies to include antibody identification and titer, paternal antigen status, amniocentesis , ultrasonography, and PUBS 3. Diagnosis including antigen type and severity 4. Management interventions including intrauterine transfusion and timing of delivery 5. Factors influencing intervention including antibody type and titer, optical density, fetal hematocrit, fetal hydrops, and fetal lung maturity 6. Complications of intervention including transfusion complications and prematurity 7. Complications of non-intervention including perinatal morbidity, mortality, and long-term neurologic sequelae 8. Follow-up including patient education and counseling regarding subsequent pregnancies D. The resident will have an understanding of the diagnosis and management of post-term pregnancy including: 1. Determination of gestational age 2. Physical examination based on historical uterine size, fundal height, and estimation of fetal size by abdominal exam 3. Diagnostic studies to include ultrasound confirmation at various gestational ages, amniocentesis, and biophysical profile 4. Diagnosis including prolonged pregnancy, macrosomia, meconium, fetal hypoxia, and placental insufficiency 5. Management interventions including identification of Bishop’s score and fetal compromise 6. Factors influencing decisions for intervention including condition of the cervix, fetal condition, and gestational age 7. Potential complications of intervention including prematurity, fetal hypoxia, and risk for operative delivery 8. Potential complications of non-intervention including perinatal morbidity and mortality and longterm neurologic sequelae 9. Follow-up including patient education, antepartum surveillance, and timing and route of delivery E. The resident is expected to have a thorough understanding of collagen vascular disorders as they impact on pregnancy including: 1. Historical symptoms of arthralgias/myalgias, fatigue, hypertension, renal involvement, evidence of chronic pregnancy loss, and peripheral vascular insufficiency 2. Physical examination for signs of skin, connective tissue, joint, vascular, and cardiac manifestations 3. Diagnostic studies including anti-DNA, ANA, VDRL false positivity, rheumatoid factor, CBC, 24-hour urine for total protein and creatinine clearance, serum creatinine, chest x-ray, and EKG 4. Diagnosis of SLE, rheumatoid arthritis, and other collagen vascular diseases 5. Possible management interventions including medical therapy and mode of delivery 6. Factors influencing intervention including visceral involvement, fetal condition, and acute and chronic hypertension 7. Potential complications of intervention including prematurity and adverse drug reactions 8. Potential complications of non-intervention including fetal compromise, stillbirth, and progression of maternal disease 9. Follow-up maternal and fetal surveillance for progression of disease, hypertensive disorders of pregnancy, mode of delivery, and puerperal evaluation and counseling F. The resident will have a thorough understanding of the impact of psychiatric disorders preceding, during, and following pregnancy including: 1. Symptoms of affective disorders, past and current medications, substance abuse history, and family history 2. Physical examination including inappropriate affect, impaired mental status, thyroid disease, signs of substance abuse, and nutritional deficiency 3. Diagnostic studies including evaluation of mental status and studies to exclude organic disease 4. The diagnosis of affective and anxiety disorders, psychosis, somatization, and eating disorders 5. Management of possible interventions including psychiatric consultation and referral 6. Factors influencing decisions regarding intervention including risk of patient’s behavior to self or others, social and family support, gestational age, and duration and severity of symptoms 7. Potential complications of intervention including maternal and fetal adverse reactions to therapy 8. Potential complications of non-intervention including deterioration of work, family, social status, physical health, and physical harm to the patient or others 9. Follow-up including psychiatric counseling and referral, hospitalization, and family counseling and support G. The resident will have an understanding of the diagnosis and treatment of malignancies in pregnancy including: 1. Historical symptoms of bleeding or discharge, cough or hoarseness, change in bowel or bladder habits, non-healing lesions, changes in skin lesions and pigmentation, and impact of previous malignancy 2. Physical examination including signs of primary and metastatic disease 3. Diagnostic studies to evaluate severity and extent of maternal malignancy 4. Diagnosis of leukemia, Hodgkin’s disease, breast cancer, melanoma, and bowel cancer 5. Management interventions including surgery, chemotherapy, radiation, induced abortion, delivery, and fetal surveillance 6. Factors influencing intervention including type and extent of malignancy and fetal condition 7. Potential complications of intervention including side effects of maternal therapy and prematurity 8. Potential complications of non-intervention including progression of malignancy, fetal compromise or death, and maternal death 9. Follow-up including maternal and fetal surveillance H. The resident will have a thorough understanding of antepartum tests of fetal well-being including: 1. Indications for antepartum fetal monitoring 2. Physical examination to include maternal cardiovascular status, size/dates discrepancy, amniotic fluid volume, presentation and lie 3. Diagnostic studies including NST, CST, acoustic stimulation, and BPP 4. Diagnosis of abnormal fetal heart rate patterns including influence of disease and medications and false-negative and false-positive rates of normal and abnormal tests 5. Management interventions including further testing, expectant management, induction of labor, and cesarean delivery 6. Factors influencing decisions regarding intervention including confirmatory diagnostic studies, fetal condition, severity of underlying maternal disease, medications, and fetal presentation 7. Potential complications of intervention including prematurity, neonatal death, and complications of induction and delivery 8. Follow-up documentation of findings and continued surveillance I. The resident will have a thorough understanding of the basic physical principles and indications for medical ultrasonography including: 1. Relevant principles of acoustics, effects on human tissues, basic operating principles, Doppler instrumentation, signal processing, artifact, measuring systems, and image recording, storage and analysis 2. Investigation of early pregnancy including number of fetuses, amnionicity and chorionicity, CRL, early pregnancy failure, molar pregnancy, cervical length measurement, and evaluation of the adnexa 3. Normal fetal anatomy at 18 to 20 weeks including skull, nuchal fold, face, brain and posterior fossa, spine, heart at the 4-chamber view, abdomen, genitalia, and limbs 4. Fetal biometry including biparietal diameter, head circumference, abdominal circumference, humerus length, femur length, and cerebellar diameter 5. Estimation of gestational age 6. Assessment of fetal growth 7. Assessment of biophysical profile Interpersonal and Communication skills Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate leadership skills with the junior residents and medical students 2. Promote the team approach of patient care with nursing staff, social workers and all ancillary staff to ensure comprehensive care of the obstetric patient 3. Communicate effectively with other services 4. Coordinate the care of all patients on the Obstetric service 5. Communicate effectively with all patients—in particular difficult patients Professionalism Following completion of this rotation, the resident is expected to be able to: 1. Demonstrate respectfulness and compassion to all patients 2. Demonstrate respectfulness to all staff and allied health workers 3. Demonstrate respectfulness to all other residents and faculty members 4. Complete and fulfill responsibilities and respond promptly when on call or paged 5. Demonstrate honesty and integrity when interacting with patients and staff 6. Accept responsibility for patient care and management plans 7. Accept the teaching responsibilities of all junior residents and medical students 8. Communicate effectively with other services 9. Coordinate the care of all patients on the Obstetric service along with the Attending Systems Based Practice Following completion of this rotation, the resident is expected to be able to: 1. Be familiar with billing codes for common obstetric procedures 2. Identify system issues that contribute to poor patient care 3. Effectively utilize systematic approaches to reduce errors and improve patient care 4. Effectively utilize hospital resources and outside resources to improve patient care Practice Based Learning Following completion of this rotation, the resident is expected to be able to: 1. Effectively utilize technology to manage information for patient care and self improvement 2. Know the essential books associated with the management of Obstetrics 3. Know how the access ACOG Bulletins, Committee Opinions regarding the standards of practice 4. Know how to access all online services to obtain pertinent up to date information regarding Obstetric issues and management Evaluations The PG III resident rotating on the Obstetrics service is evaluated using 360 evaluations. They are evaluated by their faculty, their patients, the ancillary staff, the junior residents and themselves. The Obstetrics faculty completes the summative evaluations at the end of the rotation. The evaluations are done based on the core competencies as outlined in the Goals and Objectives that are listed above for this rotation. Self evaluations are used to determine whether or not a resident achieved competency with the management of a specific obstetric cases. Reading Assignments Williams Obstetrics: Cunningham Obstetrics: Gabbe ACOG Compendium and Committee Opinions Rubella Vaccination Asthma in Pregnancy Fetal Macrosomia Shoulder Dystocia Use of Progesterone to reduce Preterm Birth HIV in Pregnancy Hepatitis in Pregnancy Prevention of Rh D Alloimmunization