Human Life Cycle 7 – Puberty, Adolescence and
advertisement

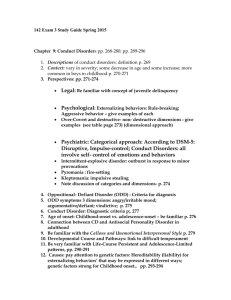
Human Life Cycle 7 - Puberty, Adolescence and Psychopathology Anil Chopra 1. To know the main endocrine factors associated with the onset of pubertal development. 2. To know the range of adolescent attitudes (males/females, ethnic variation) to pubertal development 3. To demonstrate that that these attitudes and associated behaviours in the context of other aetiological factors, may contribute to the onset of anorexia nervosa. 4. Describe the main features of anorexia nervosa. 5. To know selected features of treatment that may ameliorate the outcome of the disorder. 6. Understand the principles of adolescent development of self concept and identity in relation to biological, psychological, social and environmental changes during adolescence. 7. Know the range of disorders of mood accompanying adolescent development (dysthymia, depressive disorder, psychotic depression and bipolar disorder). 8. Know the main causes of depressive disorder in adolescence, encompassing biological psychological, social and environmental factors. 9. To know the main features of antisocial behaviour, conduct disorder, and offending. 10.To know some important aetiological and maintaining factors. 11.To know what interventions may ameliorate the problems. Puberty, Adolescence and Psychopathology There are a number of dynamic changes that occur in the brain as a result of adolescence: • White matter increases • Relative reduction in grey matter • Dorsal lateral prefrontal cortex (important in controlling impulses) matures until 20’s • The differences in gender become apparent as females develop more than males in the mesial temporal cortex, caudate thalamus. This results in a number of psychological changes that involve the cognition, understanding (e.g. morality), identity and personality. There are also a number of social changes that occur: • Family - parental surveillance, confiding • Peers - increased importance • Social role – education, occupation, etc • Psychosexual developmental These are thought to be influenced by school, work, culture, environment, social class, housing neighbourhood etc as well as genes. The psychology associated with adolescence mean that it is a time of: • Increased risk of disorders related to neurodevelopmental processes eg schizophrenia • Improvement in some other e.g. hyperkinetic disorders (improved impulse control) • Increased risk of eating disorders eg AN • Increased risk of depression (Females) or conduct problems/ delinquency (Males) Puberty, Body Shape and Anorexia Anorexia Nervosa is defined as having a body weight of at least 15% below that which is expected or a BMI of less than 17.5. It is characterised by the avoidance of the patient from “fattening” foods and to have a desired body weight that is lower than premorbid or healthy. Patients often have a dread of fatness and this often leads to a number of endocrine problems. The male : female ration is 1:10. Bulimia Nervosa is defined as a persistent preoccupation with eating, and an irresistible craving for food. Patients often succumb to episodes of eating large amounts of food in short periods of time and then go without food for long periods of time. They often have other weight losing behaviours such as force-vomiting. Male Pubertal Development - increase in height and musculature - often, slower maturing boys are dissatisfied with their height and musculature - early maturing boys feel more attractive, popular, relaxed and superior to their peers (better at sports); these feelings may persist - studies show that boys often wanted to gain weight associated with built musculature Female Pubertal Development - increase in height and body fat - insecurity about menarche (first period) - girls are often dissatisfied with their weight gain and fat proportion - may lead to lower self-esteem - being slim is perceived as desirable - studies show that many girls perceive themselves as fat and many are dieting Girls who are prone to having eating problems are often have early pubertal maturity and subsequent higher body fat, usually accompanied by some psychological disorders e.g. depression. They attribute slimmer body shapes as being attractive. It is thought that: - 20% of girls are obese - 30-50% of girls are dieting or dislike their body shape - 10% are severely dieting and using weight loss techniques e.g. vomiting, laxatives - 1% have anorexia nervosa or bulimia nervosa Ethnic variation – white English girls are more negative about body shape and weight than African Caribbean girls. Negative attitudes increase as weight and BMI increase Severe dieting is the main symptom of anorexia nervosa and studies have shown that it can increase the risk by 16 times. Twin studies show that there is a 50% inheritance and the disease is evident in personalities which are perfectionist and obsession. Negative attitudes to body shape from parents also increases the risk of anorexia development, along with maternal dieting. Experiences such as sexual abuse and other adverse life events can also influence the risk of anorexia nervosa. There is also the heavy influence of peers and the media. Presentation of Anorexia Nervosa - weight loss - abnormally slow growth from self starvation - nausea - abdominal distension - fainting and dizziness - deliberate self harm (especially in bulimia) - selective eating – fat avoidance - vomiting, and laxatives - low mood, irritability - poor concentration - sleep disturbance Assessment of Anorexia Nervosa • • • • • Family interview Individual interview with child/adolescent Physical examination Data on growth Physical examination & investigations Differential diagnosis: Physical o Gastro-intestinal disorder eg. crohns disease o Metabolic eg diabetes o Pituitary Psychiatric o Bulimia nervosa o Depression o Psychosis o Obsessive compulsive disorder Treatment of Anorexia Nervosa • Nutrition counselling • Family therapy - parents supervise eating, ensure weight gain - discussion of family relationships - family life-cycle issues - most adolescents are significantly helped by family treatments • Initially weight gain, then improvement in eating attitudes and mood • Family conflict reduces and warmth between parents increases, relationships become more harmonious • Important problems in treatment are drop-out, depression/DSH, poor treatment progress, low weight • Separation of parents from Adolescent associated with better outcome in critical families • Cognitive Behavioural therapy to reduce weight preoccupations, challenge faulty cognition Self Concept, Mood and Depression Self concept: what sort of person you are. This is a result of biologically based behavioural propensities e.g. autonomic reactivity, thinking and feeling patterns are a substrate for personality. The brain undergoes developmental programming following severe experiences which lead to changes in the neuroendocrine structure and function. - Attachment theory: it is thought that negative relations in childhood lead to negative thoughts about oneself and negative relationships in adulthood - concepts of the world are influenced by the development of our standards and values - Abstract Thinking – Piaget described a change from concrete operational thinking to the stage of formal operations. - Negative cognitive sets – cause persistence of adverse effect of experiences. Self efficacy is the ability to cope with different life challenges, depending on expectations of how other people are likely to respond to you. Environmental Factors o Poverty and deprivation o Disadvantaged schools and neighbourhoods with bullying o Disasters and wars Depressive Disorder: characterised by depression of mood, easy irritability plus any 2 or more of: Depressed mood, with sadness and tearfulness, misery and hopelessness Loss of energy and interest Self blame and feelings of unworthiness and guilt Change in sleep pattern – insomnia, early morning wakening, or sleepiness Changes in appetite, with diminished appetite/sometimes increased appetite Weight changes associated with the appetite changes Slowing of thought processes and bodily movements School problems academic and social problems, withdrawal or outbursts Suicidal thoughts or behaviour All of which result in impaired functioning. Psychotic Depression: patient may experience hallucinations with depressing content e.g. thoughts of suicide, voices of evil, worthlessness Bipolar Affective Disorder: characterised by alternating feelings of depression (dysthymia) and mania (elation, overactivity, grandeur). Epidemiology - 0.2% of children aged 10 and under experience depression o Male: female ratio is 1:1 - 3-5% of adolescents experience depression o Females more so than males There is also a high rate of comorbidity with 50% of children having at least one more disorder. Biological Factors The risk of depression is higher in those families with other major defective disorders. Twin studies also show a concordance for depression with monozygotic twins having a 76% risk of development of the other having it. It is thought that biochemically, depression is caused by lack of monoamine production in the brain and hence lack of activity of reward systems. Hormonally, it is thought that the rise in depression in adolescent females is due to androgens and oestrogen production. These also indirectly affect the secretion of hormones such as cortisol, thyroid hormone and growth hormone. Depression may also complicate physical illness, such as Cushing’s Disease, glandular fever, diabetes, asthma, rheumatoid arthritis, Crohn’s etc. Social and Environmental Causes Adolescent Depression may be a consequence of: • acute life events • chronic adversity • vulnerability factors, such as early loss – bereavement, especially loss of a parent leads to development of depression • change of cognition: from operant thinking to a stage in of formal operations involving abstract concepts, which may be depressive in nature • another disease (secondary depression) e.g. conduct disorder, adjustment disorder, separation anxiety, attention deficit, eating disorders and psychosomatic conditions • drug abuse and alcoholism • physical, sexual or emotional abuse at home or at school resulting in “learned helplessness” • disturbed parents • Bereavement, especially loss of a parent may lead to prolonged grief and depression • The manner with which the bereavement is coped with by the surviving family affects the outcome of depression • Change from concrete operational thinking to the stage of formal operations involving abstract concepts, which may be depressive in nature. • Depressed individuals have a negative cognitive set in which they blame themselves and develop negative attributions. • ”Learned helplessness” may result when adolescents’ security and self-esteem are impaired by chronic adverse circumstance such as discord or abuse at home or bullying at school. • domestic violence • marital conflict between parents – family divorce is seen in a number of cases often leading to secondary consequences such as financial instability, stress, arrival of step parent • loss of friendship or relationship with peers (especially boyfriend/ girlfriend) • difficulty with classwork at school • exam failure • social disadvantage and poverty • Depression may appear as a secondary condition accompanying and related to conduct disorder, adjustment disorder, separation anxiety, attention deficit, eating disorders and psychosomatic conditions. • Substance misuse or early alcoholism may also be associated with depression. Scarring: individuals are often affected by a primary episode of depression and hence are more likely to have subsequent episodes. This is caused by long-lasting changes in the biology and responsivity to stressors. Sensitisation: a first depressive episode may sensitise people to more episodes. This is caused by biochemical and microstructural changes in the brain. Treatment Depression is usually self limiting but can be decreased by treatment. Recurrence may occur if depressive disorder is severe, these may be Unipolar or bipolar and result in an increased risk of self harm. Psychotherapy – support and counselling, self-help, – cognitive behaviour therapy (CBT) changes cognitive distortions – interpersonal psychotherapy (IPT) modifies current relationships Psychopharmacological • Anti depressant medication - Fluoxetine (Prozac) a selective serotonin reuptake inhibitor useful in moderate to severe depression. • Lithium and anticonvulsants may be useful in Bipolar Affective Disorder. Family Approaches • Parental course for problem solving and communication • Family therapy may lessen intra-family conflict • Benefit risks associated with depression Environment • Improve the environment at home or school (eg bullying) • Admission to an adolescent unit may be necessary if there is suicidality, psychosis or refusal to eat or drink. Group Therapy • Supportive group therapy produces improved peer-relationships and social skills. Conduct Disorder, Antisocial Behaviour and Offending Conduct disorders are characterised by a repetitive and consistent pattern of offensive, antisocial, aggressive or defiant conduct. Features of Conduct Disorder • Disobedience/Defiance • Spitefulness and Bullying • Fighting and use or carrying of weapons • Stealing and mugging • Cruelty to people and animals • Destruction of property • Truancy and running away from home • Arson • Major violations of age-appropriate social expectations Types of conduct disorder: Conduct Disorder confined to the family context Unsocialized Conduct Disorder Socialized Conduct disorder Oppositional Defiant disorder Depressive Conduct Disorder Other mixed disorders of conduct and emotions Hyperkinetic conduct disorder Delinquency: failure to abide by the law. Epidemiology Child delinquency is the most common psychotic childhood condition: o 5% 5 – 15 years o 4% 5 - 10 o 6% 10 – 15 The boy: girl ratio is 2: 1. Causes of Delinquency • • • • • • • • • • • • • • • • Genetic e.g. through difficult / impulsive temperament Hyperactivity Physical health problems Developmental problems e.g. delayed language development Association with deviant peer groups e.g. gangs Poor parent supervision Erratic, harsh discipline from parents Parental rejection Lack of positive reinforcement of prosocial behaviour from parents Parental criminality Family violence Parental substance misuse Large family size Poor schooling e.g. inadequate law enforcement, or poorly defined laws Poverty Inner city crime and unemployment Consequences of Conduct Disorder For individual - expulsion from school - imprisonment - suicide - homicide - alcoholism and drug dependence - antisocial personality - increased risk of unemployment - difficulty in relationships There are also a number of effects on the innocent victims and a huge financial cost to society. Treatment Targeted at modifiable risk factors: - parenting programmes o play and positive parent-child interactions o praise and reward for good behaviour o clearly expressed rules and expectations o consistent and calm consequences for misbehaviour - cognitive problem solving skills o Adolescents with conduct disorder sometimes have distorted attributions of aggressive intentions in other people o Techniques used to develop more accurate perceptions o Teaching of problem-solving skills, including range of options and their consequences. - school intervention o teaching teachers about how to deal with disruptive behaviour o increasing school acheivment - hyperactivity management o medications used - multi-systemic therapy o intensive package of measures including parent management, social and educational measures and family work - mentoring There is not a good prognosis if the prevention fails. Psychological Changes in Adolescence Hormonal Changes: - it is risky to attribute all mood change to hormonal change during adolescence. - activation of the hypothalamic-pituitary gonadal axis. Tasks of Adolescence identity independence intimate relationships secure sexual identity employment leaving home Cognitive and social Changes Achievement of independent identity is important in adolescence. In becoming independent, autonomy is keen. Adolescents want to make boundaries themselves. Abstract thinking. Become more concerned with hypothetical & the future. Adolescents become increasingly self conscious. Need privacy. Quite egocentric – preoccupied with themselves. Worries about immediate issues rather than long term. Generally have an ideological mode of moral reasoning which addresses wider social issues rather than just personal and interpersonal situations. Peer and Family Relationships Peer relationship increasingly important Some risk taking ‘normal’. Self Concept: a view of what sort of person you are. Influences thoughts, feelings and actions. Develops throughout childhood but becomes more sophisticated in adolescence with the development of abstract thinking. Components of self concept include physical, psychological and social attributes. Development of self concept occurs through experiences, e.g. o Biological factors o Severe/traumatic experiences e.g. physical abuse o Psychological factors. o Social factors: self efficacy – ability to cope with life challenges. o Environmental factors: bullying, war, Challenges of Adolescence Stressful Social acceptances Friendships External pressures: school exams Vulnerable to mental health problems. Adolescents who have not learned adaptive ways of dealing with challenges. can lead to depressive disorder. Features of Depressive Disorder Depressed mood lasting at least 2 weeks. Depressive thinking. Hopelessness, suicidal thinking, negative about future. Biological symptoms – sleep disturbance, appetite disturbance. Associated functional impairment. Irritable mood. Social withdrawal. Psychotic symptoms are rare before mid-adolescence (hearing voices) Distinguish between mild, moderate and severe. Epidemiology - Prepubertal 0.2% prevalence o Boys same as girls - Postpubertal 6% prevalence o Females more prevalent than males. - 50% have more than 1 disorder. - 20% of adolescent GP attendees have suffered a recent depressive episode. - Increase in prevalence from pre to post pubertal due to o Direct effect of hormones o Cognitive changes o The social impact of puberty e.g. o Changes in life stress. Causes of Depression There is no one single cause, it is multifactorial. Predisposing factors: Genetic Family environment o Children of disturbed parents prone to depression o This finding mat be via an association with social advantage/family adversity. Early exposures Temperament & personality o Children who are slow to adapt to new experiences are prone to depression. o Cognitive style: e.g. tendency to blame self for problems rather than others. o Chronic causes e.g. bullying e.t.c. can lead to “learned helplessness”. Stressful events Acute, stressful life events often precede onset o Family separation o Loss of influential figure o Bereavement o Peer problems Wide variation in response to such events e.g. the timing, consequence, context of death of parent Maintaining factors Sub-syndromal symptoms Direct persistence Scarring of sensitisation Persisting biological or cognitive vulnerability Persisting adversity e.g. family dysfunction. Prognosis o Average length of mental health services = 9 months o High risk of recurrence o High risk of persistence into adulthood Treatment Individual Psychotherapy Biological treatments Family approaches Parental courses to improve problem solving skills and communication. Family therapy may lessen