Risk factors of bovine tuberculosis in cattle in rural area in kaloubia
advertisement

Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
Risk Factors of Bovine Tuberculosis in Cattle in Rural Area in Egypt
BY
* El-Newishy,A,A. ** Sylvia, O. Ahmed
* Zoonoses Department, Faculty of Veterinary Medicine, Benha University
** Dept. of Animal Hyg. and Zoonoses, Faculty of Veterinary Medicine, Assiut University
Abstract
This study shows a representative stratified cluster samples survey of the
prevalence of comparative intradermal tuberculin test in cattle from two rural
regions in Kalyobia province in project which held by Benha University from 1 to
26 March 2009 (National Project for Tuberculosis Protection) to assess possible
risk factors for tuberculin-positive reaction in cattle. Two villages located in North
Benha city the capital of Kalyobia province , (Kafr saad- Meet rady) in where 200
cattle were randomly selected, and tested. In addition, 200 of these cattle owners
were tested and interviewed for risk factor assessment. Hundred percent of the
tested cattle in this study were traditional species (native). The individual overall
highest prevalence of cattle bovine tuberculosis (BTB) was 3 cases (1.5 %), in Kafr
saad, and the lowest in Meet rady 1 cases (0.5 %).
A total of 6 cases tuberculosis complex identified as M.bovis, 4 of them
were isolated from cattle and two isolates were obtained from human in the same
locality of those cattle. M.bovis were isolated from two (12.5 %) of 16 animals in
group A {(Tuberculin +ve with signs of tuberculosis (having clinical signs such as
debilitated condition, cough, decreasing milk production, etc)}, two (6 %) of 33
animals in group B (Tuberculin +ve and apparently healthy), (0%) of 87animals in
group C (Tuberculin -ve with clinical signs of tuberculosis), (0%) of 64 animals in
group D (Tuberculin -ve and apparently healthy animal). There was no positive
M.bovis samples isolated from cattle blood, or pharyngeal swabs, (total n =200
each), while positive isolates from milk samples were (1.5 %), (n=200), but from
1
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
fecal samples were (0.5 %), (n=200). As well as two positive cases from 200
human samples were obtained only from pharyngeal swabs.
The assessed potential risk factors of disease transmission between cattle
and human (food consumption, livestock husbandry and presence of positive
cattle) were statistically significant.
Introduction
Mycobacterium bovis has the broadest host range of the members of the
Mycobacterium tuberculosis complex and is well established as a zoonotic disease
causing disease in a wide range of mammals. Historically, milk-borne transmission
has been responsible for most human M. bovis infections [1]. In developed
countries, this route of transmission was virtually eliminated following the
widespread adoption of milk pasteurization [2]. The wide diversity of infected
species suggests several potential new routes of transmission for M. bovis from
animals to humans. However, the extent of M. bovis involvement in the global TB
burden in Africa is still largely unknown. This can be partly explained by the fact
that in humans, TB due to M. bovis is indistinguishable from that due to M.
tuberculosis in terms of clinical signs, radiological and pathological features [3].
Although cattle are considered to be the main hosts of M. bovis, the disease
has been reported in many other species, including humans, other domesticated
animals and wildlife. Infected animals shed M. bovis via milk, saliva, faeces, urine
and discharging lesions [4]. It is generally accepted that human beings get infected
either by inhalation of bacteria-containing dust-particles and aerosols shed by
infected animals or by ingestion of contaminated animal products (e.g., raw milk)
[5]. The main route of infection in cattle is through aerosol exposure, facilitated by
close contact between animals [6]. In cattle, ingestion of contaminated products
(e.g., pasture and water) is generally considered to be a secondary, less important
route of transmission [7]. A high prevalence of M. bovis was isolated from faeces
and from milking cattle. This indicates that transmission to young animals by milk
2
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
should not be neglected. Recent publications from Africa also suggest that
ingestion of M. bovis might be an important mode of disease transmission in cattle,
since mesenteric lymph nodes were shown to be more affected than mediastinal
lymph nodes [8]. In this article, we attempt mainly to assess possible risk factors
for bovine TB in cattle and humans in rural areas in Kalyobia province.
Materials and methods
A-Materials:
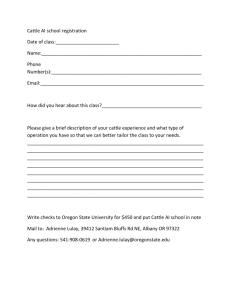
1. Study sites: This study was carried out in two regions in Kalyobia province
during project which held by Benha University (National Project for Tuberculosis
Protection from 1 to 26 March 2009). Although belonging to different ethnic
groups with different culture and religion, all farmers were sedentary small holders
with similar mixed livestock-crop farming system.
2. collection of the samples:2.1. Sampling of cattle: Cattle herds were selected by a stratified cluster sampling
proportional to the size of the cattle population, in which the unit village was
considered as a cluster. Sample size was calculated using the formula described by
[9]. A total of 200 specimens each from two regions in Kalyobia province, the
cattle were grouped to: group A (Tuberculin +ve and showing signs of
tuberculosis), (mastitis, enteritis, and pyrexia of unknown origin, group B
(Tuberculin +ve and apparently healthy animals), group C (Tuberculin -ve and
showing clinical signs of tuberculosis), D (Tuberculin -ve and apparently healthy
animals). Sample analyzed were heparinized as well as EDTA containing blood
(n=200), milk (n=200), pharyngeal swab (n=200) and faecal sample (n=200) [10].
2.1. Sampling of human: A total of 200 pharyngeal swabs were obtained from
human in the same locality of tested cattle.
3
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
3. Tuberculin testing of cattle:
The same person conducted the entire process of tuberculin testing and
reading of the result to avoid bias related to injection and reading technique. The
comparative intradermal tuberculin test was conducted in all cattle using bovine
purified protein derivatives (PPDs) supplied by the Public Veterinary Service
Agency in Egypt. Intradermal injections of 0.1 ml (2500 IU) bovine (PPD) were
administered in shaved site in the middle neck region, after having recorded skin
thickness with a caliper. Skin thickness was measured again at injection site after
72 h. The reaction at the site of injection was derived by measuring the skin
thickness before and 72 h after the injection. An animal was considered positive if
the thickness of the skin in the reaction site was greater than 10 mm [11].
4. Interview of cattle owners
Cattle owners were interviewed conducted on the two random selected sites
by a trained interviewer. Questionnaires included closed and open questions on
livestock husbandry/management and household characteristics, such as herd size
and structure, presence of other livestock, vaccination/de-worming of cattle,
mixing of cattle and other livestock at night, cattle housing at night, watering and
grazing system and reproduction. Furthermore, questions related to human
consumption habits, contact between humans and cattle, knowledge of TB and
known TB status in the household were also asked.
B- Methods:
The cattle samples obtained from (blood, pharyngeal swab, milk and feces)
were processed for isolation of mycobacteria. As well as human samples were
obtained only from pharyngeal swab, were mixed with equal volume of 4 %
sodium hydroxide and processed by modified Petroff’s method of washing with
water rather than neutralization recommended in the original method. A few drops
(about 5 ml) of processed sample were inoculated on Lowenstein-Jensen (L-J)
4
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
media then incubated at 37ºC in incubator for culture for a maximum period up to
8 wk [12].
C- Identification:
Species level identification of growth of acid fast bacilli (AFB) positive
mycobacterial isolates was done by standard biochemical tests [niacin production,
nitrate reduction, catalase activity at 68°C and at room temperature, tween
hydrolysis, arylsulphatase and thiophen-2 carboxylic acid hydrazide (TCH)
sensitivity, etc.]. A combination of positive activity for niacin, nitrate reduction,
TCH and negative activity for catalase at 68°C and arylsulphatase were considered
as characteristics of M. tuberculosis while negative activity for niacin, nitrate
reduction, catalase at 68°C, tween hydrolysis, arylsulphatase and TCH were
considered as characteristics of M. bovis as per CDC Manual [13].
D- Statistical analysis:
Data were analyzed by using statistical package STATA-7 State
Corporation. Chi square at 5 per cent level of significance was used to assess
statistical significance.
Results
Table1: Identification profile of M. bovis isolates from different clinical groups
of cattle:
Number of Tested
Cattle
M. bovis isolated
from
200 each tested
cattle samples
No. & category of cattle
Group A
No.16
Group B
No.33
Group C
No.87
Group D
No.64
2cases (12½ %)
Tuberculin +ve
2cases (6 %)
Tuberculin +ve
with signs of
and apparently
Zero case (0 %)
Tuberculin
-ve with clinical
Zero case (0 %)
Tuberculin -ve
and apparently
healthy animals
tuberculosis
healthy
signs of
tuberculosis
(having clinical
signs)
5
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
Table2: Identification profile of M. bovis isolated samples from cattle:
Number of Tested Cattle
Type of sample
M. bovis isolated
from
200 each tested
cattle samples
Milk
(n=200)
(3) 1.5 %
Fecal
(n=200)
(1) 0.5 %
Blood
(n=200)
(0) 0 %
Pharyngeal
(n=200)
(0) 0 %
Table 3: PPD prevalence in cattle in 2 different rural areas in Kalyobia
province :
Location
Tested animal
PPD-positive reactors
Percentage of reactor
animals (prevalence)
Kafr saad
Meet rady
Total
100
100
200
3
1
4
1½ %
½%
2%
Table 4: Identification profile of M. bovis isolated samples from cattle:
Number of Tested human
M. bovis isolated from
200 tested human samples
No. of individuals positive to
M. bovis
% of individuals positive
to M. bovis isolate
2
1%
6
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
Table 5: Analysis of risk factors for positive TB cases in humans as random
effect:
Risk factor
Cattle housing
Raw milk
consumption
Meat
consumption
Keeping other
livestock
Cattle herd size
Shepherding
Proportion%
(Nb/Total)
OR
95% CI for OR
p-value
Outside shed
Indoor with
people
1 (24/200)
1.7
0.7; 3.9
0.4
3 (176/200)
1
0.4; 2.6
0.2
-
3 (57/100)
0.3
0.5; 1.8
0.7
-
4 (83/100)
1.1
0.6; 2
0.6
-
70 (183/100)
1
0.6; 1.8
0.8
54 (164/200)
-
-
0.2
33 (25/200)
13 (11/200)
36 (144/200)
64 (56/200)
1.4
1.5
0.7
1.7
0.8; 2.5
0.7; 3.3
0.3; 1.7
0.6; 4.4
0.4
0.3
Base: <5
animals
<10 animals
<20 animals
Youth
Adult
Discussion
From (table1) a total of 4 cases tuberculosis complex identified as M.bovis,
M.bovis were isolated from two of 16 (12½ %) animals in group A {(Tuberculin
+ve with signs of tuberculosis (having clinical signs such as debilitated condition,
cough, decreasing milk production, etc)}, two of 33(6 %) animals in group B
(Tuberculin +ve and apparently healthy), zero, (0%) of 87animals in group C
(Tuberculin -ve with clinical signs of tuberculosis), zero, (0%) of 64 animals in
group D ( Tuberculin -ve and apparently healthy animals). Our study reports a
representative estimate of BTB prevalence in rural areas. The overall prevalence
found in our study is consistent with the results found in some African countries
[14, 15].
This suggests that BTB epidemiology in rural extensive systems very likely
differs from peri-urban livestock-production systems in our country. This could be
explained by different husbandry practices and a higher number of cross-breeds
7
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
and exotic breeds (considered to be more susceptible to BTB) found in peri-urban
settings. Bovine TB seems to be endemic and widespread in rural areas, with 2%
of the tested randomly selected village herds [16, 17]. Although the situation in the
sampled villages is favorable for BTB transmission among animals (very close
contact throughout the year in poor ventilated houses, communal
grazing/ploughing/threshing/watering, overcrowded pastures), only a few animals
per herd were found positive, with an overall individual prevalence of 2%. This
indicates a low transmission in the investigated livestock systems which are
characterized by small herd size; mostly communal grazing with some crop residue
supplementation [18].
From (Table2) the positive M.bovis samples isolated from cattle were (0 %)
(n=200) from blood, and pharyngeal swabs, while positive isolates from milk
samples were (1.5%) (n=200), but from fecal samples (0.5%), (n=200) were
positive. Maximum numbers of M.bovis were isolated from milk [(1.5%) (n=200)],
followed by feces [(0.5%), (n=200)] and as well as there was no M.bovis (0 %)
(n=200 of each samples) isolated from blood, or pharyngeal swabs of cattle. There
was significant difference in percentage of M. bovis isolates among the different
groups (faecal samples, pharyngeal swabs, milk and blood). Thus milk samples
and pharyngeal swabs were the most reliable sample which was significantly
different than others in terms of isolation rates and can thus be considered as
appropriate types of samples for diagnosis of tuberculosis from cattle.
Our study showed that milk samples were the most appropriate specimens
for isolation of M.bovis from infected cattle. Swollen udder lymph node and
discharging lymph node abscesses were important clinical signs of tuberculosis
infection in animals. Thus swollen of the udder lymph glands could be
recommended as a preferred specimen for confirmation of diagnosis of bovine
tuberculosis [19, 23, 24, 25]. Faeces and milk are considered as important media
for transmission of bovine tuberculosis [20, 22]. As is also evident from the data
8
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
published by others blood could be used as specimen for detection of tuberculosis
in cattle [26, 28].
From (table 3) representative survey of the prevalence of comparative
intradermal tuberculin test in cattle from two regions in Kalyobia province which
randomly selected to assess possible risk factors for tuberculin-positive reaction in
cattle. The two villages (Kafr saad- Meet rady) (altitude range are same) in North
Benha city the capital of Kalyobia province was randomly selected, from which
200 cattle were tested. In addition hundred percent of the tested cattle in this rural
livestock were traditional species (native), varied significantly between the overall
prevalence of cattle bovine tuberculosis (BTB) was highest (1½ %), in Kafr saad,
(3 cases) and low in Meet rady (½ %) (1cases), of the two village herds had tested
at least one positive tuberculin reactor, giving an overall herd prevalence of 2% in
all. In general, not all animals per owner were tested since as many owners as
possible per village were included in the study, either randomly from a list of all
owners.
From (Table 4) out of 200 swabs isolated from human in the same locality of
tested cattle, 2 cases tuberculosis complex identified as positive M.bovis. Similar
approaches have been also reported to be useful for diagnosis of mycobacterial
infection from pharyngeal swabs in humans [21, 29, 30]. Isolation of M. bovis
from pharyngeal swabs of human in the same locality would be important to watch
animal handlers, who would be the most probable category of suspects to have
transmitted these infections to animals. Transmission could have been by aerosols
or contamination of fodder due to indiscriminate spitting [31, 32, 33].
Suggested that the possible route of human to cattle transmission is by
inhalation of bacilli from grass contaminated with infected human urine, faeces, or
sputum [34]. There may be a small risk for transmission of tuberculosis carried by
M. bovis from cattle to human, making continued vigilance particularly necessary
[35]. Approximately 1 per cent of human tuberculosis cases could be attributed to
9
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
M. bovis. Milk and meat are one of the most important links between bovine
tuberculosis and human beings especially children [7, 24, 36]. Zoonotic
tuberculosis due to M. bovis in developing countries and estimated that the
proportion of human cases due to M. bovis accounted for 3.1 per cent of all forms
of tuberculosis. Accurate information about tuberculosis in animals particularly its
transmission to humans is speculative and studies using classical epidemiological
as well as molecular typing should be conducted to determine the exact magnitude
and also mode as well as chain of transmission. The isolation of M. bovis from
apparently healthy animals shows active transmission in the infected herds and
such findings have also been reported earlier [7, 24, 37].
Conventionally, tuberculin reactivity has been used to identify animal
infected with tuberculosis. Our data and also an earlier report show that tuberculin
reactivity is not a reliable indicator of active disease and/or tuberculosis infection
in cattle. Half of isolates of M. bovis and M. tuberculosis were obtained from
animals that were tuberculin positive. Thus our study showed wider circulation of
M. bovis in this herd, which did not correlate with clinical findings and/or
tuberculin activity. It would thus not be realistic to rely on this marker for control
of tuberculosis in animals [27, 28].
From Table (5) show the Analysis of risk factors for positive TB cases in
humans as random effect, although the situation in the sampled villages is
favorable for BTB transmission among animals (very close contact throughout the
year in poor ventilated houses, communal grazing/threshing/watering,
overcrowded pastures), only a few animals per herd were found positive, with an
overall individual prevalence of 2%. This indicates a low transmission in the
investigated livestock systems which are characterized by small herd size; mostly
communal grazing with some crop residue supplementation; if housing, then only
at night but not during the day and cattle that are often kept together with small
ruminants [1,2, 8].
10
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
The reported human TB in our study comprised all forms of the disease and
no differentiation was made between M. tuberculosis and M. bovis. It is plausible
that M. bovis might play a role. Farmer consumption habits (raw milk, raw meat)
did not show any statistical significance, as against previous findings in Kalyobia
province. However, statements on the zoonotic potential of BTB require confirmed
M. bovis cases to address their risk factors specifically. Vice versa, having
confirmed TB cases in a household was not associated with cattle reactors.
However, considering the very low prevalence of the disease in the country,
the power of the study should be further increased in future research. Because of
the clustered distribution of livestock, random effects models are more appropriate
and risk factor assessments more conservative.
Further studies on risk factors of BTB in humans require case–control
studies with confirmed M. bovis infection. ‘Classical’ risk factors have been
investigated to a certain extent in small studies in the Kalyobia province
Highlands, sometimes showing divergent results [37].
It appears that the epidemiology of BTB varies not only between different
African countries but also between different regions in Egypt depending on
livestock systems (extensive, intensive), breeds (local, exotic, and cross-breed) but
also ecological and geographic factors. Further research is needed to better
understand BTB transmission in extensive livestock systems of Kalyobia province
as well as the true potential of zoonotic risk of transmission and finally to address
the potential of control options [38].
Acknowledgements
We are very grateful to the Welcome Trust to all physicians, veterinarian,
and workers which did the work which held by Benha University Kalyobia
province from 1 to 26 March 2009 (National Project for Tuberculosis Protection).
11
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
References
1. O'Reilly LM, Daborn CJ. The epidemiology of Mycobacterium bovis infections
in animals and man: a review. Tuberculosis and Lung Disease. 1995;76:1–46.
(Suppl. 1).
2. Michigan Department of Natural Resources, Wildlife Disease Laboratory 1999. .
Summary of Michigan Wildlife Bovine Tuberculosis Surveillance, Report no. IC
2390-6.
3. Ayele W.Y., Neill S.D., Zinsstag J., Weiss M.G., Pavlik I. Bovine tuberculosis:
an old disease but a new threat to Africa. Int. J. Tuberc. Lung Dis. 2004;8:924–
937.
4. Phillips C.J.C., Foster C.R.W., Morris P.A., Teverson R. Genetic and
management factors that influence the susceptibility of cattle to Mycobacterium
bovis infection. Anim. Health Res. Rev. 2002;3(1):3–13.
5. Cosivi O., Grange J.M., Daborn C.J., Raviglione M.C., Fujikura T., Cousins D.,
Robinson R.A., Huchzermeyer H.F., de Kantor I., Meslin F.X. Zoonotic
tuberculosis due to Mycobacterium bovis in developing countries. Emerg. Infect.
Dis. 1998;4(1):59–70.
6. Neill S.D., Skuce R.A., Pollock J.M. Tuberculosis-new light from an old
window. J. Appl. Microbiol. 2005;98(6):1261–1269
7. Menzies F.D., Neill S.D. Cattle-to-cattle transmission of bovine tuberculosis.
Vet. J. 2000;160(2):92–106.
8. Cleaveland S., Shaw D.J., Mfinanga S.G., Shirima G., Kazwala R.R., Eblate E.,
Sharp M. Mycobacterium bovis in rural Tanzania: risk factors for infection in
human and cattle populations. Tuberculosis. 2007;87(1):30–43.
9. Bennett S., Woods T., Liyanage W.M., Smith D.L. A simplified general method
for cluster-sample surveys of health in developing countries. Rapp. Trimest.
Statist. Sanit. Mond. 1991;(44):98–106.
12
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
10. Vestal AL. In: Procedures for isolation and identification of Mycobacteria,
U.S. Department of Health, Education and Welfare, CDC Atlanta, Georgia,
Publication No CDC-77 - 8230. 1977: p15-9.
11. Ameni G., Erkihun A. Bovine tuberculosis on small-scale dairy farms in
Adama town, central Ethiopia, and farmer awareness of the disease. Rev. Sci.
Tech. Off. Int. Epiz. 2007;26(3):711–719.
12. Vestal AL. In: Procedures for isolation and identification of Mycobacteria,
U.S. Department of Health, Education and Welfare, CDC Atlanta, Georgia,
Publication No CDC-77 - 8230. 1977: p15-9.
13. Vestal AL. In: Procedures for isolation and identification of Mycobacteria,
U.S. Department of Health, Education and Welfare, CDC Atlanta, Georgia,
Publication No CDC-77 - 8230. 1977: p15-9.
14. Shirima G.M., Kazwala R.R., Kambarage D.M. Prevalence of bovine
tuberculosis in cattle in different farming systems in the Eastern zone of Tanzania.
Prev. Vet. Med. 2003;57(3):167–172.
15. Cleaveland S., Shaw D.J., Mfinanga S.G., Shirima G., Kazwala R.R., Eblate
E., Sharp M. Mycobacterium bovis in rural Tanzania: risk factors for infection in
human and cattle populations. Tuberculosis. 2007;87(1):30–43.
16.Saito M., Pan W.K., Gilman R.H., Bautista C.T., Bamrah S., Martin C.A.,
Tsiouris S.J., Argüello D.F., Martinez-Carrasco G. Comparison of altitude effect
on Mycobacterium tuberculosis infection between rural and urban communities in
Peru. Am. J. Trop. Med. Hyg. 2006;75(1):49–54.
17. Vargas M.H., Furuya M.E., Oérez-Guzman C. Effect of altitude on the
frequency of pulmonary tuberculosis. Int. J. Tuberc. Lung Dis. 2004;8(11):1321–
1324.
18. Lall JM. Tuberculosis among animals in India. Vet Bull 1969; 39 : 385-90.
13
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
19. Sulieman MS, Hamid ME. Identification of acid fast bacteria from caseous
lesions in cattle in Sudan. J Vet Med S B Infect Dis Vet Public Health 2002; 49 :
415-8.
20. Leite CQ, Anno IS, Leite SR, Roxo E, Morlock GP, Cooksey RC. Isolation and
identification of mycobacterium from livestock specimens and milk obtained in
Brazil. Mem Inst Oswaldo Cruz 2003; 98 : 319-23.
21. de Lisle GW, Bengis RG, Schmitt SM, O’Brien DJ. Tuberculosis in freeranging wildlife: detection, diagnosis and management. Rev Sci Tech 2002; 21 :
317-34.
22. Whelan AO, Coad M, Peck ZA, Clifford D, Hewinson R G, Vordermeier HM.
Influence of skin testing and overnight sample storage on blood-based diagnosis of
bovine tuberculosis. Vet Rec 2004; 155 : 204-6.
23. Buddle BM, Ryan TJ, Pollock JM, Andersen P, de Lisle GW. Use of ESAT-6
in the interferon-gamma test for diagnosis of bovine tuberculosis following skin
testing. Vet Microbiol 2001; 80 : 37-46.
24. Wood PR, Corner LA, Rothel JS, Baldock C, Jones SL, Cousins DB, et al.
Field comparisons of the interferon-gamma assay and the intradermal tuberculin
test for the diagnosis of bovine tuberculosis. Aust Vet J 1991; 68 : 286-90.
25. Hanna BA, Walters SB, Bonk BJ, Tick LJ. Recovery of mycobacteria from
blood in mycobacteria growth indicator tube and Lowenstein-Jensen slant after
lysis - centrifugation. J Clin Microbiol 1995; 33 : 3315-6.
26. Fandinho FC, Grinsztejn B, Veloso VG, Lourenço MC, Werneck-Barroso E,
João E, et al. Diagnosis of disseminated mycobacterial infection: testing a simple
and inexpensive method for use in developing countries: Pan Am J Public Health,
1998; 4 : 43-7.
27. Esteban J, Molleja A, Fernandez Roblas R, Soriano F. Number of days
required for recovery of mycobacteria from blood and other samples. J Clin
Microbiol 1998; 36 : 1456-7.
14
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
28. Pacios E, Alcalá L, Ruiz-Serrano M J, de Viedma DG, Rodríguez-Créixems M,
Marín-Arriaza M, et al. Evaluation of bone marrow and blood cultures for the
recovery of mycobacteria in the diagnosis of disseminated mycobacterial
infections. Clin Microbiol Infect 2004; 10 : 734-7.
29. Hutchings MR,Harris S. Effects of farm management practices on cattle
grazing behaviour and the potential for transmission of bovine tuberculosis from
badgers to cattle. Vet J 1997; 153 : 142-62.
30. Smith RM, Drobniewski F, Gibson A, Montague JD, Logan MN, Hunt D, et al.
Mycobacterium bovis infection, United Kingdom. Emerg Infect Dis 2004; 10 :
539-41.
31. Hardie RM, Watson JM. Mycobacterium bovis in England and Wales: past,
present and future. Epidemiol Infect 1992; 109 : 23-33.
32. Cosivi O, Grange JM, Daborn CJ, Ravijglione MC, Fujikura T,
Cousins D, et al. Zoonotic tuberculosis due to Mycobacterium bovis in developing
countries. Emerg Infect Dise 1998; 4 :59-70.
33. Kazwala RR, Dabron CJ, Kusiluka LJ, Jiwa SF, Sharp JM, Kambarage DM.
Isolation of Mycobacterium species from raw milk of pastoral cattle of the
Southern high lands of Tanzania. Trop Anim Health Prod 1998; 30 : 233-9.
34. Neill SD, Hanna J, Mackie DP, Bryson TG. Isolation of Mycobacterium bovis
from the respiratory tracts of skin test negative cattle. Vet Rec 1992; 131 : 45-7.
35. Hardie RM, Watson JM. Mycobacterium bovis in England and Wales: past,
present and future. Epidemiol Infect 1992; 109 : 23-33.
36. Cosivi O, Grange JM, Daborn CJ, Ravijglione MC, Fujikura T, Cousins D, et
al. Zoonotic tuberculosis due to Mycobacterium bovis in developing countries.
Emerg Infect Dise 1998; 4 : 59-70.
37. Kazwala RR, Dabron CJ, Kusiluka LJ, Jiwa SF, Sharp JM, Kambarage DM.
Isolation of Mycobacterium species from raw milk of pastoral cattle of the
Southern high lands of Tanzania. Trop Anim Health Prod 1998; 30 : 233-9.
15
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
38. Neill SD, Hanna J, Mackie DP, Bryson TG. Isolation of Mycobacterium bovis
from the respiratory tracts of skin testnegative cattle. Vet Rec 1992; 131 : 45-7.
عوامل الخطر للدرن البقرى فى الماشية فى المناطق الريفية فى مصر
سيلفيا أسامة أحمد/ عادل محمد عبد العزيز **د/*د
16
Benha Vet. Med. J., Vol. 20, No.1, Jun. 2010
قسم األمراض المشتركة كلية الطب البيطرى جامعة بنها
قسم صحة الحيوان واألمراض المشتركة كلية الطب البيطرى جامعة أسيوط
الملخص العربى
أجريت دراسة لمسح للعينات العشوائية لمعدل إنتشارمرض الدرن البقرى بأستخدام إختبار التيبركلين الجلدى
للمقارنة بين الماشية فى منطقتين ريفيتين في محافظة القليوبية من خالل المشروع الذي أقامتة جامعة بنها م ْن
1إلى 26مارس ( 2009المشروع الوطني للحماية من الدرن) لتقييم عوامل الخطر المحتملة للماشية
األيجابية أختبار التيبركلين الجلدى .قريتان واقعة في شمال مدينة بنها وهى عاصمة محافظة القليوبية( ،كفر
ْ
إختبرت 200ماشية باإلضافة ألى 200م ْن مالكي
سعد -ميت راضى) و التى إختيرت بشكل عشوائي،
جربة في هذه الدراسة ك ْ
انت
الماشية و الذى إختبروا وقوبلوا لتقييم عوامل الخطر .مائة بالمائة م ْن الماشية ال ُم ّ
من النوع التقليدي (متوطن) .اإلنتشار األعلى العا ّم لدرن الماشية كان 3حاالت ( ،)% 1,5في كفر سعد,
واألقل كان في حاالت ميت راضى و حالة واحدة ( .)% ,5من 6الحاالت المعزولة المنصنف درن بقرى ،
عزل و صنف الدرن البقري
عزل م ْن الماشية وإثنتان عْزال م ْن اإلنسان و على نفس المنوال ُ
4حاالت منهم ُ
من الماشية م ْن حالتان بنسبة أصابة ( )%12,5وم ْن 16حيوان في المجموعة أية {(أيجابية أختبار التيبركلين
قص إنتاج الحليب ،الخ)}،
الجلدى مع أعراض ال ُ
س ّل (أعراض سريريةُ مثل أعراض ضعف عام ،سعال ،ن ُ
إثنان ( )% 6م ْن 33حيوان في المجموعة بي (أيجابية أختبار التيبركلين الجلدى ال يبدو عليها أعراض
الدرن) )% 0( ،م ْن 87حيوان في المجموعة سي (سلبية أختبار,التيبركلين الجلدى يبدو عليها أعراض
الدرن) )% 0( ،م ْن 64حيوان في المجموعة دي (سلبية أختبار التيبركلين الجلدى ال يبدو عليها أعراض
الدرن) .اليوجد هناك عينات إيجابية للدرن المصنف بقري ع ْ
زلت م ْن د ّم الماشية ،أومن مسحات بلعومية لها،
(المجموع 200ل ُك ّل نوع عينة) ،بينما عْزلتُ عينات إيجابية م ْن الحليب بنسبة (( )% 1,5العدد الكلي
200عينة) ،بينما كانت أيجابية العينات البرازية بنسبة (( ،)%,5العدد الكلى 200عينة) .باإلضافة إلى إثنان
م ْن 200عينة إيجابية من اإلنسان عْزلتُ فقط م ْن المسحات البلعومية .عوامل الخطر المحتملة ال ُمقيَّمة
للمرض بين الماشية واإلنسان (إستهالك الغذاء وفالحة للماشية ووجود ماشية إيجابية) كانا ها ّم بشكل
إحصائي.
17