ACLS - UBC Wiki

ACLS
1 Keep up to date with advanced cardiac life support (ACLS) recommendations (i.e., maintain your knowledge base). – PLEASE SEE LINK for 2010 Guidelines: http://circ.ahajournals.org/content/122/18_suppl_3.toc
2 Promptly defibrillate a patient with ventricular fibrillation (V fib), or pulseless or symptomatic ventricular tachycardia (V tach).
ACLS Cardiac Arrest Algorithm:
ACLS Cardiac Arrest Circular Algorithm.
3 Diagnose serious arrhythmias (V tach, V fib, supraventricular tachycardia, atrial fibrillation, or second- or third-degree heart block), and treat according to ACLS protocols.
Ventricular tachycardia occurs when electrical impulses originating from the ventricles cause rapid ventricular depolarization (140-250 beats per minute) – tx - see algorithm above
Ventricular fibrillation occurs when parts of the ventricles depolarize repeatedly in an erratic, uncoordinated manner. The EKG in ventricular fibrillation shows random, apparently unrelated waves.
Usually, there is no recognizable QRS complex . tx see algorithm above
Supraventricular tachycardia - A narrow QRS complex (<120 msec) reflects rapid activation of the ventricles via the normal His-Purkinje system, which in turn suggests that the arrhythmia originates above or within the atrioventricular (AV) node (ie, a supraventricular tachycardia). The site of origin may be in the sinus node, the atria, the atrioventricular node, the His bundle, or some combination of these sites. The
Ddx: atrial fib, atrial flutter, and a variety of paroxysmal SVTs, most commonly atrial tachycardias,
AVNRT, and AVRT Tx- see ACLS adult tachycardia algorithm below
Atrial Fibrillation: - Tx- see ACLS A fib algorithm below
2 nd degree Heart Block:
Type 1 ( Wenckebach ) -progressively increasing PR interval culminating in a dropped beat
Tx: if asymptomatic- no tx, if symptomatic –ie bradycardia- tx= permanent pacemaker (reversible causes should be excluded- MI, increased vagal tone, and meds)
Type 2 (Mobitz): PR interval remains unchanged prior to a P wave that suddenly fails to conduct to the ventricles.
Tx: permanent pacemaker-(reversible causes should be excluded- MI, increased vagal tone, and meds)\
3 rd degree HB : There is complete dissociation of atria and ventricles.
Tx: permanent pacemaker-(reversible causes should be excluded- MI, increased vagal tone, and meds)
Atropine- may be effective by reversing the decrease in AV nodal conduction induced by vagal tone in the emergent setting
Bradycardia Algorithm.
4 Suspect and promptly treat reversible causes of arrhythmias (e.g., hyperkalemia, digoxin toxicity, cocaine intoxication) before confirmation of the diagnosis.
Hyperkalemia - clinically weak and ECG shows tall peaked T waves, increased PR interval, and wide
QRS, progressing to sine wave pattern and PEA
Tx: r/o pseudohyperkalemia (hemolysis)
Acute management: calcium gluconate 2 amps IV, reg. insulin 10U with 1-2 amps D50W, Salbutamol 10 to
20 mg by neb over 10mins
Tx to eliminate total body K+: Kayexalate 30-90gms PO/PR, diuretics e.g. furosemide 40mg IV, or hemodialysis
Hypokalemia - clinically nausea, vomiting, weakness, muscle cramps, ST depression, flattened T, prominent U wave, prolonged QT ( Tx with KCL 10-20meq/hr IV if urgent or 40meq PO 4-6 hrs for non urgent)
Digoxin toxicity - ST scooped-like depression, mild PR prolongation if clinically significant manifestations (ventricular tach; ventricular fib; asystole; complete heart block;
Mobitz II heart block; symptomatic bradycardia) OR Evidence of end-organ dysfunction (eg, renal failure, altered mental status) OR Hyperkalemia (serum potassium >5 to 5.5 meq/L . Tx : digoxin-specific antibody
(Fab) fragments aka ‘Digibind’ - if Fab fragments are not immediately available, tx: bradycardia with atropine (0.5 mg IV in adults; 0.02 mg/kg IV in children, minimum dose 0.1 mg) and hypotension with IV boluses
HYPERcalcemia - bones (pain), stones (renal/biliary) , groans (abd pain/nausea/vomiting), psychic moans
(dep/anxiety) , thrones (sit on the throne – polyuria), dehydration, change in mental status, vomiting, pancreatitis, decreased reflexes, short QT TX : IVNS 4-6L/day, furosemide IV q6hrs, pamidronate 60-80mg
IV x 1 dose, ( calcitonin and glucocorticoids= questionable evidence)
HYPOcalcemia - perioral paresthesias, depression, psychosis, seizures, chvostek’s sign (tap facial nerve and contraction of facial muscles on ipsilatarel side), trousseau’s (inflate BP cuff and get carpal spasm), prolonged QT TX: symptomatic: calcium gluconate 1-2gIV over 20mins + calcitriol +/-Mg 50-
100mEq.day, asymptomatic oral calcium 1-3g/d (calcium gluconate 500-1000mg PO bid-qid and vit. D ergocalciferol 50000IUpo/wkx6-8wks, in chronic hyoparathryoid need to give calcitriol)
Cocaine intoxication mydriasis, euphoria, agitation, elevated HR and BP, sweating, tremors, confusion, seizure, HTN, arterial vasoconstriction (eg, coronary arteries), thrombus formation, psychomotor agitation
(neurologic effects can range from agitation to seizures to intracranial hemorrhage), severe hyperthermia, dyspnea (from pneumothorax, pulmonary infarction or other pulmonary injury), and ischemic bowel.
TX: stabilize vitals (ABC),
Airway management- Succinylcholine relatively contraindicated in rapid sequence intubation; consider rocuronium (1 mg/kg IV) or other nondepolarizing agent as alternative
Psychomotor agitation -diazepam 5 to 10 mg IV every 3 to 5 min
Severe or symptomatic hypertension -diazepam (5 mg IV) or lorazepam (1 mg IV); may repeat q 5 minutes until sedated, Phentolamine (1 to 5 mg IV); repeat as necessary, DO NOT ADMINISTER BETA-
BLOCKERS, INCLUDING LABETALOL
Cocaine-associated myocardial ischemia - EKG, diazepam (5 mg IV) or lorazepam (1 mg IV) for agitation or hypertension, Aspirin 325 mg PO, Nitroglycerin 0.4 mg SL with or without continuous infusion, Phentolamine 1 to 5 mg IV, repeat as necessary; hold for SBP <100, DO NOT ADMINISTER
BETA-BLOCKERS, INCLUDING LABETALOL. Beta-blockade is contraindicated in acute cocaine toxicity.
QRS widening on ECG (rare; suggests profound toxicity) - sodium bicarbonate, 1 to 2 mEq/kg IV push hyperthermia - initiate cooling, if elevated CK (rabdomyolosis) IV fluids.
5 Ensure adequate ventilation (i.e., with a bag valve mask), and secure the airway in a timely manner.
Bag-Mask Ventilation
All healthcare providers should be familiar with the use of the bag-mask device for support of oxygenation and ventilation. Bag-mask ventilation is particularly helpful during the first few minutes of resuscitation or when placement of an advanced airway is delayed or unsuccessful. Effective bagmask ventilation requires adequate training and frequent practice. When using a bagmask device (ie, no advanced airway is in place), the rescuer should deliver a tidal volume sufficient to produce chest rise (approximately 6 to 7 mL/kg or
500 to 600 mL) over 1 second. This volume of ventilation minimizes the risk of gastric inflation. The rescuer should be sure to open the airway adequately with a chin lift, lifting the jaw against the mask and holding the mask against the face, creating a tight seal. During CPR, give 2 breaths during a brief (about 3 to 4 seconds) pause after every 30 chest compressions. When an advanced airway (eg, endotracheal tube, esophageal-tracheal combitube [Combitube], or laryngeal mask airway [LMA]) replaces the face mask, rescuers should deliver 8 to 10 breaths per minute during CPR. Deliver each breath over about 1 second while chest compressions are delivered at a rate of 100 per minute, and do not attempt to synchronize the compressions with the ventilations .
6 In patients requiring resuscitation, assess their circumstances (e.g., asystole, long code times, poor precode prognosis, living wills) to help you decide when to stop. (Avoid inappropriate resuscitation.)
BLS- Termination of resuscitation rule for adult out of hospital cardiac arrest
ALS- Termination of resuscitation rule for adult out of hospital cardiac arrest
Terminating Cardiac Arrest Resuscitative Efforts in Adult In Hospital Cardiac Arrest
In the hospital the decision to terminate resuscitative efforts rests with the treating physician and is based on consideration of many factors, including witnessed versus unwitnessed arrest, time to CPR, initial arrest rhythm, time to defibrillation, comor- bid disease, prearrest state, and whether there is ROSC at some point during the resuscitative efforts. Clinical decision rules for in-hospital termination of resuscitation may be helpful in reduc- ing variability in decision making; however, the evidence for their reliability is limited, and rules should be prospectively validated before adoption.
7 In patients with serious medical problems or end-stage disease, discuss code status and end-of-life decisions (e.g., resuscitation, feeding tubes, levels of treatment), and readdress these issues periodically.
What is an advance directive ? An advance directive is a mechanism whereby competent people give instructions about what is to be done if they should subsequently lose the capacity to decide or to communicate. It covers decisions about medical treatment, particularly the treatment which might be provided as the patient approaches death. Also states legally appointed decision makers who would make decisions according to patient’s wishes outlined in advance directive. Only used if patient becomes incapable of making decisions. Drafting an advance statement is recommended be done with medical advice and counseling as part of a continuing doctor-patient dialogue.
A living will may be referred to as a “medical directive” or “declaration” or “directive to physicians,” and it provides written direction to healthcare providers about the care that the individual approves should he or she become terminally ill and be unable to make decisions. A living will constitutes evidence of the individual’s wishes, and in most areas it can be legally enforced.
A durable power of attorney for health care is a legal document that appoints an authorized person to make healthcare decisions (not limited to end-of-life decisions). Simply put, a living will affects the care received, and a durable power of attorney accounts for unforeseen circumstances. The latter decisions may be in conflict with the living will or advance directive; at the time of the unforeseen circumstances they are considered to be valid expressions of the patient’s best interests.
Levels of treatment : comfort care, limited care (e.g. antibiotics/IV fluids/O2 for pneumonia), surgical care, intensive care
Feeding - basic feeding, supplemental feeding (e.g. vitamins, supplements), intravenous feeding, tube feeding
DNR vs. CPR
-can make changes to advance directive while competent
8 Attend to family members (e.g., with counseling, presence in the code room) during and after resuscitating a patient . offering select family members the opportunity to be present during a resuscitation is reasonable and desirable (assuming that the patient, if an adult, has not raised a prior objection) . Parents and other family members seldom ask if they can be present unless they are encouraged to do so by healthcare providers. Resuscitation team members should be sensitive to the presence of family members during resuscitative efforts, assigning a team member to remain with the family to answer questions, clarify information, and otherwise offer comfort.
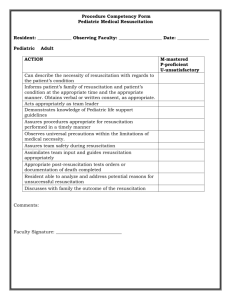
9 In a pediatric resuscitation, use appropriate resources ( e.g., Braeslow tape, the patient’s weight) to determine the correct drug doses and tube sizes.
In compensated shock, blood pressure remains normal; it is low in decompensated shock. Hypotension is a systolic blood pressure less than the 5th percentile of normal for age, namely:
● <60 mm Hg in term neonates (0 to 28 days)
● <70 mm Hg in infants (1 month to 12 months)
● <70mmHg+(2 x age in years) in children 1 to 10 years
● <90 mm Hg in children ≥10 years of age
Uncuffed endotracheal tube size (mmID)= (age/4) + 4
Cuffed endotracheal tube size (mmID)= (age/4) + 3
(Endotracheal tube size is more reliably based on a child’s body length.)
(Adult women- 7.5-8.0 cuffed, Adult males- 8-8.5 cuffed )
Braeslow tape - which is used during pediatric emergencies to quickly estimate a child's weight, determine weight-based drug doses, and select the correct size emergency or resuscitation equipment.