Therapeutic recommendations for the management of
advertisement

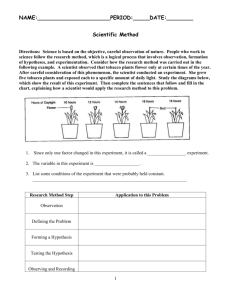
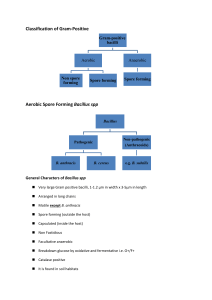
THERAPEUTIC RECOMMENDATIONS FOR THE MANAGEMENT OF PATIENTS EXPOSED TO BACILLUS ANTHRACIS IN NATURAL SETTINGS L. Pirotha,i, J. Leroyb,i, O. Rogeauxc,i, JP Stahld,i, M. Mocke, B. Garin-Bastujif, N. Madanif, C. Brezillone, A. Maillesg,i, Th Mayh,i,* a Department of Infectious and Tropical Diseases, Dijon Teaching Hospital, France Department of Infectious and Tropical Diseases, Besançon Teaching Hospital, France c Department of Infectious and Tropical Diseases – Internal medicine, Chambéry Hospital, France d Department of Infectious and Tropical Diseases, Grenoble Teaching Hospital, France e Anthrax National Reference Center, Institut Pasteur, Paris, France f Anthrax National Reference Laboratory, ANSES Maisons-Alfort, France g National Institute for Public Health Surveillance InVS, Saint Maurice, France h Department of Infectious and Tropical Diseases, Nancy Teaching Hospital, France i French Infectious Diseases Society (SPILF) b * Corresponding author: t.may@chu-nancy.fr INTRODUCTION Except in the context of bioterrorism, human anthrax infection is acquired after exposure to a sick animal or to a contaminated animal product (wool, leather, etc.). The sporulating bacterium Bacillus anthracis is considered as one of the most lethal potential biological weapons. Since 2001, the risk of inhalation after a possible intentional dissemination has led to numerous recommendations for a preemptive treatment both immediately after exposure and after onset of symptoms [1-5]. But in the context of exposure to a natural source of the anthrax bacillus (mainly farm animals), the management of potentially exposed individuals has never been the object of therapeutic recommendations and there is very little published on the issue. In 2005, the InVS had published a multidisciplinary report on the surveillance and prevention of animal and human anthrax (or “anthrax fever”), but this document did not deal with the management of individuals exposed to an animal infected or suspected to be infected by anthrax. It specifically mentioned that “in case of exposure to a risk identified by the enquiry, individual chemoprophylaxis could be suggested”, without any indication for the evaluation of the contamination risk, or any indications for treatment, or any suggestions for a specific therapeutic regimen. Nevertheless, every year foci of animal anthrax are reported in various French regions, and for each focus individuals potentially exposed to the anthrax bacillus. The objective of this document was to determine therapeutic recommendations for the evaluation and management of patients potentially exposed to the anthrax bacillus, in “natural” settings. I – METHOD The SPILF initiated a work group including infectiologists having been consulted during various episodes of human exposure to infected animals or to their product (Côte d’Or, Doubs, Moselle, Savoie), a microbiologist from the Pasteur Institute Anthrax National Reference Center in Paris, two veterinarians specialized in microbiology from the ANSES Anthrax National Reference Laboratory in Maisons Alfort, one veterinarian specialized in epidemiology from the Department of Infectious Diseases at the InVS. This group drafted recommendations according to the following method: 1 i) ii) iii) iv) from recommendations on the surveillance and prevention of animal and human anthrax issued by the InVS in 2005 [6] by using published data when available (infecting inoculum, food borne epidemics, etc). Searching on the Pub Med database using «post-exposure; anthrax; treatment» as keywords brought up 26 articles 8 of which were related to antibiotherapy, 2 of which concerned bioterrorism, 7 of which concerned vaccination or immunologic treatments, 4 of which were general reviews. Using «human anthrax and antibiotic treatment» brought up 341 references, 68 of which published since 2006. 9 of these 68 references were non-redundant with a «Post-exposure» search. when there was no published data, recommendations were made according to experience acquired by the various experts during previous episodes of animal anthrax. after visiting a knackering and rendering facility and better understanding procedures and potential occupational risks of various workstations in these settings. Most evaluated settings with a weak level of proof were analyzed and drafted collectively by the expert group, so that the resulting recommendation was a consensus between members of the work group. II - BACILLUS ANTHRACIS DATA B. anthracis is a sporulating Gram-positive bacterium, of the Bacillus cereus family. During its biological cycle, B. anthracis presents in spore and vegetative form. The spore form is the one which resists and persists in the environment. Sporulation is triggered in conditions of nutritional deficiency with air oxygen (central position non deforming endospore) [7]. In its natural cycle, sporulation occurs when the animal dies, after liberation of bacilli in the air, and the dissemination into the ground (via body fluids or open carcasses). Spores also form in waste or by products of infected animals (bones, skin, wool, etc). The ground, when contaminated by spores, is the true reservoir of B. anthracis. The persistence of spores in the ground for several decades, is responsible for the recurrent infection of animals on some sites, «the cursed fields», known for ages. The vegetative form, found inside the infected host’s organism, is a thick bacillus, with square ends, immobile and capsulated. The virulence of B. anthracis is due to the presence of two plasmids, pXO1 and pXO2, coding respectively for the synthesis of two toxins and a capsule. The loss of one plasmid or the other strongly decreases the strain’s virulence. This is the case for the Sterne vaccinal strain, non capsulated by loss of pXO2, used in veterinarian medicine. B. anthracis is aero-anaerobic and develops in 18 to 24 hours on common agarose, incubated at 37°C in normal atmosphere, yielding large white to gray colonies, with a "jelly fish head" aspect, on a serum enriched medium and in the presence of 5% CO2. The colonies are smooth because of the capsule synthesis. Flakes can be observed in the broth, they sediment leaving a clear broth. In direct microscopic examination, the bacillus appears isolated, in short chains or long bamboo stalk-like associations. B. anthracis does not induce hemolysis on blood agarose and most strains are susceptible to phage and penicillin. The absence of mobility may be investigated with complementary tests. Multiplex PCR, using specific markers of plasmids pXO1 and pXO2 and a chromosome marker, allows confirming the bacteriologic identification of B. anthracis [8,9]. 2 III - ANIMAL ANTHRAX (OR ANTHRAX FEVER) Anthrax fever (AF) due to B. anthracis usually occurs in the spring and summer, in animals grazing on contaminated ground, after long periods of drought followed by episodes of rain. It mainly affects herbivorous animals, more rarely omnivores or carnivores, domestic or wild animals. It usually presents as an acute septicemic disease, evolving rapidly to death, with general digestive, respiratory, and meningeal symptoms. The incubation usually lasts from 1 day in ovines to 3 up to 7 days, in bovines (table 1). Several forms de AF have been described in ruminants. The hyper acute form presents with a short lasting tipsy gait, dyspnea, and convulsions. Death is sudden. In the acute form the onset of symptoms is brutal, with fever, interruption of milk production, then respiratory disorders, and tachycardia, digestive disorders (diarrhea, bloody diarrhea), and urinary disorders (hematuria). Death comes in very rapidly (1 to 3 days). Most of the time, AF occurring in grazing animals presents as «sudden death» and the discovery of the cadaver in the pasture without observing any symptom. In small ruminants, the hyper acute form is the most frequent. In horses, digestive disorders are more severe (diarrhea) and death occurs within 3 to 6 days. In Suidae (pigs, boars), the edematous form or anthrax laryngitis is common: throat edema, fever, respiratory and circulatory disorders, diarrhea sometimes hemorrhagic, sometimes congestive or hemorrhagic cutaneous lesions. Death may occur in 2 to 4 days but cure is possible in this species. In carnivores, symptoms are similar: hemorrhagic septicemia and throat edema. In wild animals, symptoms would seem to be analogue to those of domestic animals. In birds, there are very rare cases. Sporadic cases have been reported in ostriches and Barbary ducks. The microbiologic diagnosis is made by culture and/or PCR. The most efficient samples are blood and the spleen, as well as milk. Autopsy is forbidden if AF is suspected because of the great exposure risks for the veterinarian and farm personnel, and risk of contaminating the environment. In France, since 2002, 15 confirmed anthrax fever foci have been reported in 13 French subdivisions. These cases are described in chapter 4.2.2 Table 1: clinical presentation of anthrax fever in bovines Clinical description - Incubation period from 1 to 5 days, usually - Specific clinical signs Acute form: septicemic anthrax - After ingestion of B. anthracis, onset of acute febrile respiratory and circulatory disorders with bleeding from natural orifices, petechia, and edema before death Sub-acute form: external anthrax or «anthrax tumor» - Edematous reaction often in the throat or in the upper respiratory tract before symptoms appear as in the previous form 3 IV - ANTHRAX IN HUMANS 4.1 Modes of transmission to man and risk factors In “natural” transmission settings, a man can be contaminated by exposure to sick animals or to contaminated animal products. There are 3 presentations of the human disease: cutaneous, inhalation, or gastro-intestinal. Transmission occurs: • by skin or mucosal contact with spores on contaminated material, animals or animal products. • by inhalation of spore aerosol penetrating in pulmonary alveoli and transported by lymph to mediastinal lymph nodes. The germination of spores at this level frees toxins which trigger hemorrhage, edema, and tissue necrosis; • by ingestion of contaminated products. The germination of spores and then the multiplication of bacilli free toxins at various levels of the digestive tract: mouth, esophagus; or intestine. 4.2 Epidemiological data: human cases and animal foci in France since 2002 [54]. 4.2.1 Notified anthrax cases in France since 2002 Since 2002, 4 cases of human B. anthracis infection were reported. In 2003, a case of cutaneous anthrax was diagnosed in a contaminated patient who had handled sheep wool in Algeria. In 2008, 3 cases of cutaneous anthrax were reported in Moselle; they concerned men who had cut-up and gutted the same anthrax infected cow [10]. The diagnosis was made by PCR on skin biopsies made next to the lesions [11]. The strain was isolated from a human case and from the infected bovine. The 3 cases had a favorable outcome without complications. 4.2.2 Animal anthrax foci and management of exposed persons Since 2002, 61 confirmed foci of animal anthrax1 were reported in 12 French subdivisions (Aveyron, Cantal, Côte d’Or, Doubs, Isère, Jura, Meurthe-and-Moselle, Moselle, Puy de Dôme, Saône et Loire, and Savoie). Three other foci were reported but without bacteriological confirmation in 3 other subdivisions (Aube, Loire Atlantique and Vienne) (figure 1). In all, data on the number of exposed individuals is documented for 11 foci. During these episodes, 150 patients received post-exposure prophylactic treatment to (PEPT), average 14 per animal anthrax focus [0 to 108] (table 2). Individuals considered as exposed to the bacterium or to its spores were most often farmers and owners of the anthrax infected animals and people working on these farms, the veterinarian having examined the animal or animals, and knackering and rendering facility personnel having processed the animal cadavers. Less frequently, they were subdivision veterinarian laboratory personnel (SVL), members of the farmer’s family, or relatives having helped to move the anthrax infected animal cadavers. The reported types of exposure were direct contact with cadavers, or exposure to aerosols possibly generated by moving the cadaver or processing it at the knackering and rendering facility. More rarely, consumption of raw milk, meat, or offal from anthrax-infected animals, was responsible for contamination. Finally, for SVL personnel, unprotected contact with diagnostic samples of animals suspected to be infected by anthrax, and in one cases, the spattering of samples during the accidentally brutal opening of a package were considered to be the source of exposure. 4 Table 2: foci of animal anthrax and management of exposed patients in France since 2003 Date Subdivision Animal(s) involved Bovine (milk) (Comte cheese with raw milk) Bovine (meat) Bovine (meat) (Charolais) Management of exposed individuals Veterinarian and farmer: doxycycline 8 d SVL technicians: ciprofloxacin 60 d Veterinarian intern: no treatment, anthrax blood test Veterinarian and 2 farmers: amoxicillin 10 d One of the 2 farmers consulted, management not documented Farmer, 8 close relatives, 4 DDSV(veterinarian subdivision agency) agents, 8 SVL agents: amoxicillin 12 d Farmer and veterinarian: no treatment June 2003 Doubs June 2003 Côte d’Or 2004 Saône and Loire August 2005 Aube Bovine (milk) August 2006 Vienne August 2006 Cantal August 2006 Sept. 2006 Cantal Savoie 5 bovines 5 bovines (meat) 1 horse 3 bovines (Salers) 1 bovine (Montbeliard) June 2007 Lozere 3 bovine herds (Aubrac) August 2007 Jura 1 bovine (Montbeliard) August 2007 Meurthe and Moselle Bovines October 2007 Cantal 2 bovines (Aubrac) August 2008 Doubs 37 bovines (milk and meat) (21 herds in 10 towns) Dec. 2008 Moselle 1 bovine (meat) July 2009 Puy de Dôme 5 bovines (milk) (Saint-Nectaire AOC) 5 non treated exposed individuals (refusal) July 2009 Côte d’Or 3 bovines (meat) Farmer + 5 family members, a veterinarian and an SVL agent: fluoroquinolone then doxycycline after antibiogram, Comments Consumption of raw milk non considered at risk Clinical diagnosis only, not confirmed in bovines Clinical diagnosis without biological confirmation for bovines Badly documented episode Not documented No individual considered as potentially contaminated 3 individuals: fluoroquinolone 10 d 5 SVL agents: amoxicillin 10 d Farmer and 2 neighbors having helped him to move the bovine cadavers: prescription not documented Not documented Farmer: fluoroquinolone (length of treatment not documented) 3 knackering and rendering facility personnel: amoxicillin (length of treatment not documented) Veterinarian: no treatment No individual considered as potentially contaminated 108 known patients assessed at the Besançon teaching hospital and treated most frequently for cutaneous and digestive exposure (consumption of anthrax infected cow milk) 10 individuals treated with fluoroquinolone and 1 with amoxicillin because of a contra-indication for fluoroquinolones Nature of exposure not documented Episode having occurred after earthworks in a pasture Possibly community practice prescribed treatments, but not documented 7 other non treated exposed individuals because of the delay between latest risk exposure and consultation 5 total length 2 months Farmer + 4 close relatives, a veterinarian, a milk, collection technician, knackering and rendering facility personnel: prescription made but not documented July 2009 Aveyron 5 bovines (meat) and 15 dairy goats July 2009 Savoie/Isere Around 20 bovines belonging to 12 herds 38 individuals: fluoroquinolone 15 or 21 d Sept. 2009 Loire Atlantique 8 bovines (meat) Veterinarian: antibiotic self prescription Farmer and a neighbor: no treatment A second veterinarian wearing gloves and a mask during his intervention did not receive any treatment Fluoroquinolone was chosen because a penicillin resistant strain was isolated from an anthrax infected bovine in 1997 in the same town Anthrax without biological confirmation but episode having occurred on a previously “cursed” field No human case occurred after discovering these animal anthrax foci. In the Moselle 2008 episode, the 3 human cases led to discovering the animal focus and occurred before implementing any preemptive treatment. 6 Figure 1: geographical distribution of animal anthrax foci identified in France from 2003 to 2010 Legend Number of animal anthrax foci 0, 87.5, 175, 250 kilometers 7 Table 3: clinical presentation of human anthrax Clinical description - Incubation period from an average of 1 to 10 days (after cutaneous-mucosal contact or ingestion) up to 60 days (after inhalation) - Non-specific clinical signs Inhalation anthrax - After inhalation of B. anthracis and a short prodrome, acute febrile respiratory distress, complicated by hypoxia, dyspnea, and radiological observation of mediastinal enlargement associated to septicemia Cutaneous anthrax - After contact with a sick animal or infected products of animal origin, skin lesion with first a papula, then a vesicle, and finally a black sore surrounded by edema. The lesion is usually painless but it may be complicated by fever and malaise, which can be associated to septicemia Gastro-intestinal anthrax - After consuming a contaminated raw product, syndrome with sharp abdominal pain, diarrhea, fever, and septicemia 4.3 Clinical course 4.3.1 Length of incubation The length of incubation (between exposure and onset of symptoms) after cutaneous and/or mucosal contact or ingestion is 1 to 10 days, rarely more. Nevertheless, after inhalation of spores, incubation has been reported to last up to 60 days (table 3). 4.3.2 Cutaneous anthrax The exposed cutaneous zones (arms, hands, face, and neck) are the most frequently affected (figure 2). The disease begins with a macula or pruritic papula which develops into a circular shaped ulcer on the second day. Small vesicles from 1 to 3 mm may appear, discharging a clear or bloody fluid containing numerous bacilli. The lesion then changes to a black sore, often associated to local and severe edema. The sore dries and disappears in 1 to 2 weeks without leaving any scar. Lymphangitis, painful lymph nodes, and severe edema may develop and the disease may be complicated by bacteremia. An adapted antibiotic oral treatment is effective. Without treatment, the death rate may reach 20% (in case of sepsis). With an early treatment, it is inferior to 1%. 8 Figure 2: cutaneous anthrax (picture courtesy of Bacillus anthracis NRC, Institut Pasteur) 4.3.3 Gastro-intestinal anthrax It begins with acute gastroenteritis which can evolve rapidly to bacteremia with bloody diarrhea. Death may occur within a few hours (estimated death rate between 25% and 60%). Oropharyngeal presentations with lymph node involvement and sub-lingual edema have been described. 4.3.4 Inhalation anthrax It is improperly called “pulmonary” form: it is not really pneumonia but a first involvement of mediastinal lymph nodes. According to available data, the disease could includes two stages: 1) an initial pseudo-influenza syndrome with catarrhal rhinitis which may last from a few hours to a few days; 2) a secondary and fulminant respiratory failure associated to bacteremia. Thoracic X-ray reveals mediastinal enlargement often related to lymph node involvement very often associated to pleural and parenchymal involvement. In half of the cases, patients develop a hemorrhagic meningeal form. If very early antibiotic treatment is not initiated (in the early phase of the disease), the death rate ranges between 80% and 100%. The mean delay between onset of des symptoms and death is 3 days. 4.3.5 Meningeal anthrax It may be a complication of all the other presentations. The initial site may also be directly ethmoidal after spore inhalation. This severe hemorrhagic meningitis rapidly evolves to coma and death [12]. 4.4 Microbiologic diagnosis The microbiologic diagnosis is performed by: isolation and identification of Bacillus anthracis from clinical samples (hemocultures, skin swabs, CSF, lymph node biopsies, etc.) which should be collected before any antibiotherapy; specific PCR (Polymerase Chain Reaction) ; blood tests (ELISA). Serodiagnosis is useful only for a retrospective diagnosis in case of antibiotic treatment before sampling. 9 The following are available in all laboratories - direct examination: non-mobile Gram positive bacilli; - culture: positive in 6 to 24 h, identification in 24 to 48 h (non hemolytic, depending on culture medium either in short chains of 2 to 3 consecutive elements, or in very dense reticulation of long mycelium-like chains); - antibiogram: to be required systematically (penicillin, doxycycline, ciprofloxacin). Samples must be managed by a P3 laboratory if anthrax is suspected. Nevertheless, incidental identification of the bacillus in culture by a non-P3 laboratory may be possible. Laboratories in the biotox-piratox network (reference laboratories in defense zones) may perform culture and antibiogram, as well as PCR. The Paris Institut Pasteur Anthrax National Reference Center and the Anthrax National Reference Laboratory (Anses, Maisons Alfort) will perform PCR for confirmation (results in 24 h after receiving samples), the antibiogram of strains, and blood tests. V - EVALUATION OF RISK DEPENDING ON THE CONTACT The risk of developing human anthrax depends on the contact with a sick animal, living or dead. The risk of person-to-person transmission, if it has sometimes been suggested, is not significant. The risk of developing human anthrax after contact with a sick animal depends of the source bacterial inoculum and of the contact type. 5.1 Estimation of the source inoculum The vegetative form is present at very high concentrations in all tissues of the living animal or in the non open carcass during the first days (cf. infra) [13]. It may be a source of infection for man only in case of direct contact direct with a sick animal, during care giving for example, or with bacterial culture in the laboratory [5]. The spore form is most often responsible for human contamination. Spores develop only in the presence of oxygen. This condition explains why sporulation develops only once the animal is dead and the carcass opened. Thus, if the carcass is not opened, anaerobic breakdown and ambient acidity will kill vegetative forms en 4 days without allowing spore formation. Sporulation is a process the length of which depends on temperature and humidity conditions [14] and which ranges from several hours to several days. For example, in laboratory conditions, the sporulation rate of bacilli reaches 100% in 12 hours at 37°C if relative humidity is 100%, but if it is only at 50%, this rate only reaches 35% after 34 hours. Sporulation is less important if the temperature does not exceed 15 to 21°C. There is none below 9°C [15]. Thus, only contact with an anthrax infected carcass which was opened or soiled by biological fluids exposes to spores. The source spore inoculum to which is exposed an individual in contact with this carcass is thus variable and dependant on environmental conditions (humidity, temperature, oxygen) and on the delay after the animal’s death. 5.2 Estimation of the transmission risk depending on the type of contact 5.2.1 Respiratory The available data comes almost exclusively from preparation of response plans to bioterrorism and of the experience of malevolent exposure in the USA in 2001. It allows estimating that the 50% lethal 10 dose (LD50) ranges from 8,000 to 10,000 inhaled spores [16]. Experimental studies in primates have nevertheless reported lower LD50s [17]. This estimated LD50 is probably much more important than the inoculum potentially inhaled after opening an animal carcass. Indeed, circumstances in which spores are aerosolized from a carcass are rare [18]. Furthermore, if an aerosol is created from a carcass, the density of spores would certainly be inferior to that of aerosols from envelopes of powder de malevolently distributed during the 2001 American episode. Indeed, no human case of “respiratory” anthrax has ever been reported after exposure to anthraxinfected animals. This risk could be under estimated, either because the diagnosis of such cases is not made in countries with weak medical means, or because the prescription of preemptive treatment in developed countries prevented such cases. These hypotheses remain weakly probable because of the rarity of settings leading to aerosol formation. The only cases of reported non malevolent respiratory anthrax are cases of occupational anthrax in the wool industry [19, 20] and anecdotal cases in bongo manufacturers or African drum players [20]. Nevertheless, an old study made in several New Hampshire goat wool processing manufactures (United States) proved that workers exposed daily to several hundreds of spores did not develop respiratory anthrax [21]. Thus it may be said that the contamination risk via the respiratory tract on contact with an anthraxinfected animal is null to negligible, except for a few very specific circumstances generating an aerosol (using a high pressure cleaner or compressed air in a confined atmosphere to clean a building or strip the skin of a sick animal). In these cases, upstream prevention measures must be observed by using individual protection equipment (including wearing a mask, gown, and gloves) and banning the use of high pressure cleaner when possible [18]. 5.2.2 Digestive Cases of digestive anthrax are rare, and due to the ingestion of raw or sometimes cooked meat [22-26]. This meat may come from animals dead or infected before being slaughtered. The infecting dose after ingestion is unclear but probably more important than the one for the respiratory tract. A study performed in Kazakhstan in 2004 showed that the risk of developing anthrax was more important if meat was consumed raw or grilled and less if it was boiled [27]. In this study, cooking the meat was not itself a risk factor to develop non-cutaneous anthrax. In France, in individuals exposed both cutaneously and by ingestion of meat coming from an anthrax infected animal, the cutaneous form only was observed [11]. The probability to consume meat from an anthrax-infected animal is very weak in France because of the rapid evolution of the disease in an animal, and because of veterinarian surveillance in knackering and rendering facilities. But the consumption of non-controlled meat (illegal butchering or importation) or that of wild animals infected or found dead is not without risks. Finally, if the bacillus or des may be found in the milk of infected animals, no case of digestive anthrax has ever been documented after the exclusive consumption of milk, even if a risk remains possible. 5.2.3 Cutaneous Cutaneous anthrax is by far the most frequent form of «farm» human anthrax [27-30]. Incubation is always inferior to 12 days and no case of cutaneous anthrax has ever been reported after a prolonged latency period, contrary to respiratory anthrax [11]. If any direct handling of an anthrax infected animal may involve a risk of cutaneous anthrax (a fortiori in case of hand wounds), cutting up the cadaver or the carcass is the greatest risk [27,31]. Some very rare cases of human-to-human transmission by direct contact direct with skin lesions have been reported but never any digestive or respiratory forms. Usual hygiene precautions should be respected [5,32,33,34]. 11 The risk of vectorial transmission sometimes suggested is highly improbable [31]. VI – RECOMMENDATIONS CONCERNING PREVENTION MEASURES 6.1 Reminders on investigation and management of an animal focus As soon as an anthrax animal focus is suspected, the ARS (regional heath agency) identifies potentially exposed individuals, along with the Subdivision Direction of population protection (DDPP previously Subdivision Direction of Veterinarian Services) and InVS/CIRE. Exposure to screen for includes: direct contacts with the sick animal(s), and products from these animals, among individuals living and working on the farm, and among outside individuals such as the farm veterinarian, knackering and rendering facility personnel, etc. Once the contact is proved, these individuals will be referred to a physician who will determine if antibiotic treatment is necessary, and eventually prescribed. If the animal focus is proved or suspected, a July 2010 ANSES recommendation specifies that animals sharing the infected animal’s pasture should not be moved so as to prevent spore displacement and not opening the cadaver to limit human exposure [18]. Clinical samplings of the suspicious animal or animals are sent to the national reference laboratory or to the subdivision veterinarian laboratory (if it is a P3 level) to confirm the animal diagnosis. If the focus is confirmed, vaccination or antibioprophylactic measures are implemented for animals by the ministry of agriculture and its local services to prevent other animal cases. 6.2 Preemptive treatment regimen and indications 6.2.1 Preemptive treatment objective The aim of this treatment is to prevent evolution to disease after a potentially contaminating exposure [32,35]. The work group recommends initiating the treatment as soon as possible after exposure. It is not possible to use preventive vaccination in man because there is no available vaccine in France. [5] Human cases of anthrax after contact with an sick animal are rare. The indications for preemptive treatment must be specific and restricted [36]. 6.2.2 Recommended antibiotics In vitro, the bacterium is susceptible to several molecules: penicillins, fluoroquinolones, cyclines, phenicoles, aminosides, macrolides, penemes, rifampicin, and vancomycin [35-40]. B. anthracis is resistant to cephalosporins, trimethoprim, and sulfonamide [37,38,41]. Because of a possible inducible beta-lactam secretion, penicillin or amoxicillin monotherapy is not recommended without a prior antibiogram [32,40]. There is no natural resistance to ciprofloxacin or la doxycycline but the selection of resistant strains under treatment remains possible [32,37,39,43]. Determining the susceptibility of the isolated strains is always necessary [34,39]. Ciprofloxacin or doxycycline are the two first-line molecules to initiate treatment before performing an antibiogram [4,12,32,36,42,44,45,46]. 6.2.3 Length of preemptive treatment There is no human study on this issue, comparing molecules together or against placebo [32,35,41]. The length of preemptive treatment thus takes into account the disease’s physiopathology, animal experimental studies (primate), and modelization [32,47,48,49]. The length of preemptive treatment 12 should be twice the average incubation time of the disease, that is 10 days for cutaneous or digestive exposure. For airborne exposure, incubation may be longer. In case of bioterrorism, the recommendation is to treat for 60 days, but in case of “natural” or non-malevolent contamination, 35 days seem enough. Indeed, in a macaque receiving a respiratory inoculum, 10 days of prophylaxis are enough to prevent the onset of the disease [48]. But in a primate model exposed to a respiratory inoculum, the germination of spores into pathogenic bacilli may occur up to 60 days after exposure to [36]. Finally, in a Monte Carlo simulation, Drusano et al showed that 30 days would be enough to prevent the onset of the disease, always in case of significant respiratory exposure [49]. Furthermore, a long term treatment prescription exposes to observance problems as demonstrated in mailmen exposed to envelopes of powder potentially containing spores, malevolently distributed in the USA in 2001 [50,51]. Clinical surveillance remains recommend during preemptive treatment [39]. 6.2.4 Treatment indications and modalities Precise indications were established for each type of exposure, they are specified in figure 3 and table 4. Ciprofloxacin or doxycycline are recommended in first line. If the antibiogram of the B. anthracis focus strain is documented and if the susceptibility to beta-lactams is demonstrated, amoxicillin may be used. Cyclines cannot be used in pregnant women or in children under 8 years of age, except when no other antibiotic can be prescribed and should be defined case by case [52,53]. Preemptive treatment is not recommended for healthcare personnel or for morgue personnel if standard precautions are observed, when dealing with patients infected by anthrax [3]. 13 Figure 3: management for human exposure after contact with an animal with suspected or confirmed anthrax Any animal with suspected or confirmed infection, dead or alive Cutaneous or mucosal exposure by handling or spattering on the skin or mucosa 1, 2 Cadaver not opened, no biological fluid discharge Food-borne exposure Respiratory exposure Cadaver opened, or biological fluid discharge (animal dead or alive) no individual protective equipment (IPE) Workstation with risk of aerosol exposure In knackering and rendering facilities 4 Using a high pressure cleaner in confined settings (truck, livestock van, stable, etc.) Cleaning stable area without IPE, 5 milk Meat (even cooked) Exposure within 72h before signs or animal death and consultation in the 10 days following the latest exposure Treatment 10 days Other cases Animal infected or dead Treatment 35 days No treatment Mixed milk or milked 72h before signs or animal death Individual milk or slightly mixed milk (<5 animals) within 72h before signs or animal death Other animal in the herd or from another herd 3 No treatment No gloves Gloves worn No treatment. Clinical surveillance and updating the family physician Exposure within 72h before signs or animal death and consultation in the 10 days following the latest exposure Treatment 10 days Other cases Exposure dating back to more than 10 days at consultation No treatment Exposure dating back to 10 days or less at consultation Treatment 10 days Exposure dating back to more than 10 days at consultation No treatment Exposure dating back to 10 days or less at consultation 14 Treatment 10 days The settings listed in the flowchart were considered by the workgroup as being the only ones with a risk for human contamination. Settings and/or activities not mentioned are thus considered as not being at risk. If the diagnosis of anthrax on one or several suspected animals is refuted, treatment must be stopped. 1 - Handling and spattering to skin or mucosa were considered as risk for a local form of anthrax (especially cutaneous). These activities are not considered as potentially aerosol generating. Handling pieces of animal meat and offal, surfaces, material or documents strongly soiled by blood or other biological fluids from the animal with suspected or confirmed infection is considered at risk as well as handling the whole animal. Contact with work wear or boots having been in contact with the animal is not considered at risk except if work wear is soiled by blood or biological fluids from the animal with suspected or confirmed infection. 2 - Accidental exposure to blood of animal with suspected or confirmed infection, within 72h before the onset of signs or death of the animal, during care giving for example, is considered as risk exposure, on the same level as handling, and is an indication for treatment. 3 – There is a negligible risk of B. anthracis transmission when ingesting products from animals which may have been gutted and cut up with the same instruments as those used for an animal(s) with suspected or confirmed infection, or products which may have been in direct contact with products from an animal with suspected or confirmed infection, as in a refrigerator fro example. Treatment is not recommended for individuals having ingested these products but clinical surveillance is. 4 – Knackering and rendering facility specificities. Visiting and analyzing the various works stations in knackering and rendering facility enabled determining risk exposure taking into account the type of exposure and wearing or not protective equipment (cf. Addendum 1). Globally, individual protective measures (gloves, protective hood) should be implemented permanently on risk works stations, and should be reinforced as soon as the first case of animal anthrax is reported so as to prevent recurrent exposure in case of a growing focus. - Collecting animals: direct handling of the cadaver without gloves is a risk for cutaneous requiring treatment. Pulling out a cadaver from inside a truck if the truck is equipped with a winch (driver at the back of the truck pulling out a cadaver from inside) is a risk for respiratory exposure except if a mask or protective hood is worn. Cleaning the truck without protective equipment (mask or protective hood) is a risk for respiratory exposure requiring treatment. - Administration: individuals who may have handled documents strongly soiled by blood or other biological fluids are considered as cutaneous exposure cases by handling, requiring treatment. These documents should be placed rapidly under a plastic protection, using disposable gloves. - Triage of animals to retrieve hides and BSE decapitation: cutaneous contamination is possible, treatment is required if gloves were not worn, there is no risk of respiratory contamination a priori. - Decapitation with a knife to screen for BSE: no treatment is needed a priori unless protective equipment was not worn (hood, gloves) and there were spattering of biological fluid toward the face or direct skin contact. 15 - Cutting up cadavers: treatment for a possible cutaneous contamination if no compressed air was used, and gloves were not worn, treatment for a possible respiratory contamination if no compressed air was used to dissect sub-cutaneous conjunctive tissue (if no mask or hood was used). - Cleaning the decapitation, cutting up, and triage area with a high pressure cleaner: cleaning up the area without adequate protection (mask or hood) is a respiratory exposure requiring treatment. - Chopping cadavers and cooking: no treatment. Nevertheless, cleaning the chopper with a high pressure cleaner, in case of diagnosed anthrax, is not necessary because the permanent forward motion prevents a long-lasting contamination of the chopper and this type of cleaning would probably not ensure an effective decontamination of the cadaver-processing device if it were required. Furthermore, this type of cleaning presents a non-negligible risk for the operator (accident, spattering of decaying organic matter, etc.) to be compared with the expected benefit. 5 – An animal infected or dead in a farm building (stable), will probably contaminate the floor by dejections and biologic fluid discharge. In these settings, the risk to have airborne spores when cleaning the floor cannot be excluded (removing the straw and dejections packed on the floor requiring «scraping» the animal position area in the building). This scraping should be performed wearing individual protective equipment if an animal was diagnosed with anthrax. Airborne contamination cannot be excluded if individual protective equipment is not worn. 16 Table 4: suggested antibiotic regimen after risk exposure to anthrax Cutaneous or food exposure: 10 days per os Individuals Antibiotic susceptibility Respiratory exposure: 35 days per os (2) - Doxycycline 100 mg x 2/day Adults Before antibiogram or - Ciprofloxacin 500mg x 2/ day If the strain is susceptible to penicillin (1) Before antibiogram Pregnant women If the strain is susceptible to penicillin (1) Amoxicillin 500 mg x 3/ day Ciprofloxacin 500 mg x 2/day Amoxicillin 500 mg x 3/ day Ciprofloxacin 10-15mg/kg x 2/ day not exceeding 1 g/ day or - Doxycycline Child >8 years of age and >45 kg: Children Before antibiogram 100mg x 2/ day Child >8 years of age and < 45kg: 2.2 mg/kg x 2/ day not exceeding 200 mg/day Child <8 years of age: avoid using doxycycline (1) In case of extended focus on several herds, the susceptibility of isolated strains should be checked during the episode to detect the emergence of possible resistance to penicillins as soon as possible. At least one antibiogram should be performed for each new infected herd. (2) For long-term treatments (35 days), the prescription should be modified and switched to amoxicillin if the strain is susceptible, if there is no allergy or contraindication. The referent infectious diseases department or ARS should be contacted to document antibiogram results for the animal strain. For short-term treatments, the prescription should not be modified. 17 References 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Bossi P, Tegnell A, Baka A and al. Recommendations Bichat sur la management clinique des patients présentant une maladie du Charbon liée or non à un acte bioterrorisme. Euro Surveill. 2004;9(12):E3-4. Inglesby T, O’Toole T, Henderson D and al. Anthrax as a biological weapon-2002: updated recommendations for management. JAMA. 2002;287(17):2236-52. Erratum in: JAMA 2002;288(15):1849. Brook I. The prophylaxis and treatment of anthrax. Int J Antimicrob Agents. 2002;20(5):320-5. Stern EJ, Uhde KB, Shadomy SV, Messonier N. Conference report on public health and clinical guidelines for anthrax. Emerg. Inf. Dis. 2008;14(4), pii: 07-0969. Schmid G, Kaufmann A. Anthrax in Europe: its epidemiology, clinical characteristics, and role in bioterrorism. Clin Microbiol Infect 2002;8(8):479-488. InVS. Recommendations pour la surveillance and la lutte contre le charbon animal and humain. Guide méthodologique. Saint Maurice, June 2005:35pp. http://www.invs.sante.fr/publications/2005/guide_charbon/guide_charbon.pdf Accédé le 10/08/2010. Mock M, Fouet A. Anthrax. Annu Rev Microbiol. 2001;55:647-71. Ramisse V, Patra G, Garrigue H, Guesdon JL, Mock M. Identification and characterization of Bacillus anthracis by multiplex PCR analysis of sequences on plasmids pXO1 and pXO2 and chromosomal DNA. FEMS Microbiol Lett. 1996;145(1):9-16. WHO/OIE/FAO (2008) Anthrax in humans and animals. 4ème édition. OMS, Genève, Suisse, 208 p InVS. Cas groupés de charbon cutané humain en Moselle – Décembre 2008. Saint-Maurice, février 2010 : 4 pp. http://www.invs.sante.fr/publications/2010/charbon_cutane_moselle/plaquette_charbon_cutane _moselle.pdf. Accédé le 10/08/2010. Cinquetti G, Banal F, Dupuy AL and al. Three related cases of cutaneous anthrax in France: clinical and laboratory aspects. Medicine (Baltimore). 2009;88(6):371-5. Swartz M. Current concepts: recognition and management of anthrax – an update. N Engl J Med. 2001;345(22):1621-6. Erratum in: N Engl J Med 2002 Feb 21;346(8):634. Koehler TM. Bacillus anthracis physiology and genetics. Mol Aspects Med 2009;30:386-96. Driks A. The Bacillus anthracis spore. Mol Aspects Med 2009;30:368-73. Beyer W, Turnbull PC. Anthrax in animals. Mol Aspects Med 2009;30:481-9. Fennelly KP, Davidow AL, Miller SL, Connell N, Ellner JJ. Airborne infection with Bacillus anthracis--from mills to mail. Emerg Infect Dis 2004;10:996-1002. Peters CJ, Hartley DM. Anthrax inhalation and lethal human infection. Lancet 2002;359:710711. ANSES. Avis de l’Agence nationale de sécurité sanitaire de l’alimentation, de l’environnement and du travail relatif à une demande d'avis sur les mesures de gestion en santé animale and en sécurité sanitaire des aliments lors de suspicions and de confirmations de cas de fièvre charbonneuse. Maisons-Alfort, 13 juillet 2010. http://www.afssa.fr/Documents/SANT2010sa0007.pdf. Accédé le 10/08/2010 Carter T. The dissemination of anthrax from imported wool: Kidderminster 1900-14. Occup Environ Med 2004;61:103-7. 18 20 Centers for Disease Control and Prevention (CDC).Inhalation anthrax associated with dried animal hides--Pennsylvania and New York City, 2006.MMWR Morb Mortal Wkly Rep. 2006 Mar 17;55(10):280-2. 21 Dahlgren CM, Buchanan LM, Decker HM, Freed SW, Phillips CR, Brachman PS. Bacillus anthracis aerosols in goat hair processing mills. Am J Hyg 1960;72:24-31. 22 Doganay M, Almac A, Hanagasi R. Primary throat anthrax. A report of six cases. Scand J Infect Dis 1986;18:415-9. 23 Sirisanthana T, Brown AE. Anthrax of the gastrointestinal tract. Emerg Infect Dis 2002;8:649651. 24 Sirisanthana T, Navachareon N, Tharavichitkul P, Sirisanthana V, Brown AE. Outbreak of oraloropharyngeal anthrax: an unusual manifestation of human infection with Bacillus anthracis. Am J Trop Med Hyg 1984;33:144-50. 25 Anonymous. From the Centers for Disease Control and Prevention. Human ingestion of Bacillus anthracis-contaminated meat--Minnesota, August 2000. Jama 2000;284:1644-6. 26 Hugh-Jones M. 1996-97 Global Anthrax Report. J Appl Microbiol 1999;87:189-91. 27 Woods CW, Ospanov K, Myrzabekov A, Favorov M, Plikaytis B, Ashford DA. Risk factors for human anthrax among contacts of anthrax-infected livestock in Kazakhstan. Am J Trop Med Hyg 2004;71:48-52. 28 Ozcan H, Kayabas U, Bayindir Y, Bayraktar MR, Ay S. Evaluation of 23 cutaneous anthrax patients in eastern Anatolia, Turkey: diagnosis and risk factors. Int J Dermatol 2008;47:1033-7. 29 Davies JC. A major epidemic of anthrax in Zimbabwe. The experience at the Beatrice Road Infectious Diseases Hospital, Harare. Cent Afr J Med 1985;31:176-80. 30 Doganay M, Metan G. Human anthrax in Turkey from 1990 to 2007. Vector Borne Zoonotic Dis 2009;9:131-40. 31 Doganay M. Anthrax. In: Cohen J, Powderly WG, Eds., Infectious diseases. 2nd ed. Edinburg Mosby Elsevier; 2004. 1685-1689. 32 Brook I. The prophylaxis and treatment of anthrax. Intern J Antimicrob Agents 2002;20:320-5. 33 Yakupogullari Y, Koroglu M. Nosocomial spread of Bacillus anthracis. J Hospit Infect 2007;66:401-2. 34 Weber DJ, Rutala WA. Risks and prevention of nosocomial transmission of rare zoonotic diseases. Clin Infect Dis 2001; 32: 446-56. 35 Kyriacou DN, Adamski A, Khardori N. Anthrax: from antiquity and obscurity to a front-runner in bioterrorism. Infect Dis Clin N Am 2006;20:227-51. 36 Spencer RC. Bacillus anthracis. J Clin Pathol 2003; 56: 182-7. 37 Bryskier A. Bacillus anthracis and antibacterial agents. Clin Microbiol Infect. 2002;8:467-78. 38 Luna V, King DS, Gulledge J, and al. Susceptibility of Bacillus anthracis, Bacillus cereus, Bacillus mycoides, Bacillus pseudomycoides and Bacillus thuringiensis to 24 antimicrobials using Sensititre® automated microbroth dilution and Etest® agar gradient diffusion methods. J antimicrob Chemother 2007;60: 555-67. 39 IDSA. Anthrax: current, comprehensive information on pathogenesis, microbiology, epidemiology, diagnosis, treatment, and prophylaxis. Last updated July 2010; http://www.cidrap.umn.edu/idsa/bt/anthrax/biofacts/anthraxfactsheet.html. Accédé le 10/08/2010 40 Turnbull PCB, Sirianni NM, LeBron CI, and al. MICs of selected antibiotics for Bacillus anthracis, Bacillus cereus, Bacillus thuringiensis, and bacillus mycoides from a range of clinical and environmental sources as determined by Etest. J Clin Microbiol 2004; 42:3626-34. 41 Centers for Disease Control and Prevention (CDC).Update: Investigation of bioterrorismrelated anthrax and interim guidelines for exposure management and antimicrobial therapy, 19 42 43 44 45 46 47 48 49 50 51 52 53 54 October 2001.MMWR Morb Mortal Wkly Rep. 2001;50(42):909-19.Erratum in: MMWR Morb Mortal Wkly Rep 2001;50(43):962. Bartlett JG., Inglesky TV., Borio L. Management of anthrax. Clin Infect Dis 2002; 35: 851-848 Athamna A, Athamna M, Abu-Rashed N, and al. Selection of Bacillus anthracis isolates resistant to antibiotics. J Antimicrob Chemother 2004; 54: 424-8. Ministère de la Santé and des Sports. Agents de la menace biologique. Stratégies de réponse face a une menace d’agression par les agents de la peste, du charbon or de la tularémie. http://www.sante-sports.gouv.fr/IMG/pdf/Guide_Peste_-_Charbon_-_Tularemie_PCT.pdf. Accédé le 10/08/2010. Centers for Disease Control and Prevention (CDC).Update: Interim recommendations for antimicrobial prophylaxis for children and breastfeeding mothers and treatment of children with anthrax.MMWR Morb Mortal Wkly Rep. 2001 Nov 16;50(45):1014-6. ACOG Committee on obstetric practice. ACOG Committee Opinion number 268, February 2002. Management of asymptomatic pregnant or lactating women exposed to anthrax. Obset Gynecol 2002; 99: 366-8. Deziel MR, Heine H, Louie A, and al. Effective antimicrobial regimens for use in humans for therapy of Bacillus anthracis infections and postexposure prophylaxis. Antimicrob Agents Chemother. 2005 ;49(12):5099-106. Vietri NJ, Purcell BK, Tobery SA, and al. A short course of antibiotics treatment is effective in preventing death from experimental inhalational anthrax after discontinuing antibiotics. J. Infect. Dis. 2009;199:336-41. Drusano GL, Okusanya OO, Okusanya A, and al. Is 60 days of ciprofloxacin administration necessary for postexposure prophylaxis for Bacillus anthracis. Antimicrob. Agents Chemother 2008;52:3973-9. Williams JL, Noviello SS, Griffith KS, and al. Anthrax postexposure prophylaxis in postal workers, Connecticut, 2001. Emerg Infect Dis 2002; 8: 1133-7. Shepard CW, Soriano-Gabarro M, Zell ER, and al.Antimicrobial postexposure prophylaxis for anthrax: adverse events and adherence.Emerg Infect Dis. 2002 Oct;8(10):1124-32. Kadanali A, Taysyaran MA, Kadanali S. Anthrax during pregnancy: case report and review. Clin Infect Dis 2003; 36: 1343-6. Centers for Disease Control and Prevention (CDC).Updated recommendations for antimicrobial prophylaxis among asymptomatic pregnant women after exposure to Bacillus anthracis.MMWR Morb Mortal Wkly Rep. 2001;50(43):960. Madani N, Mendy C, Moutou F, Garin-Bastuji B, 2010. La fièvre charbonneuse en France. Épisodes de l’été 2009 and foyers enregistrés sur la dernière décennie (1999-2009). BEH Horssérie / 14 septembre 2010, 15-17. 20 Work group The SPILF drafted these recommendations from the evaluations of a multidisciplinary group of experts chaired by Th. MAY, infectiologist (Nancy) including: - C. BREZILLON, microbiologist (Institut Pasteur) B. GARIN-BASTUJI, veterinarian microbiologist (Anses - Maisons Alfort) J. LEROY, infectious diseases physician (Besançon) N. MADANI, veterinarian microbiologist (Anses - Maisons Alfort) A. MAILLES, epidemiologist (InVS) M. MOCK, microbiologist (Institut Pasteur) L. PIROTH, infectious diseases physician (Dijon) O. ROGEAUX, infectious diseases physician (Chambéry) JP. STAHL, infectious diseases physician (Grenoble) 21 Addendum 1 - Knackering and rendering organization All the knackering and rendering facilities in France treat around 2.5 million tons of biomass per year. 40% of this mass is made up of animal cadavers. The cadavers that are processed come from farm animals dead after disease accident unfit for consumption, as well as from wild animals (pigeons, rats, etc.), or pets dead or killed by veterinarians, marine mammals run aground, cadavers from research laboratories, etc. Knackering and rendering facilities also process waste from agri-food industries, milk unfit for consumption, etc. Usually, if the facility is warned that anthrax fever was suspected (AF) before collecting a cadaver, the protective measures which are implemented should be sufficient to prevent exposure. There is a risk for the facility personnel only if the facility was not warned, or warned too late after having already processed several cadavers (in case the diagnosis of AF was late). 1 Collecting cadavers According to the current legislation, knackering and rendering facilities may collect only closed cadavers (not having undergone autopsy) or sutured. Nevertheless, this law may be overruled in some cases, and this increases the risks of exposure to infected biological fluids. The collecting trucks are not allowed to enter pastures and must remain on the road (including in city streets), thus limiting contamination of truck wheels and the role of trucks in spreading spores and bacteria. Two types of trucks may perform picking up cadavers at the pasture side. - Trucks with an articulated arm and a remote controlled «clamp», with a roof opening: no handling of the cadaver by the par personnel, no leak of fluids from the cadaver. - Trucks with a winch and opening at the rear: handling of the cadaver by the truck driver is needed to attach the cadaver before pulling it inside the truck and biological fluids may leak during traction. Furthermore, this type of equipment requires the driver’s coming inside the truck to detach the animal (confined space). In case of prior information on the suspicion of anthrax and request from the competent authority (Local veterinarian health authorities for the protection of populations), a specific collection may be organized directly from the facility. Protective kits including gloves and hoods are given to drivers in this case protection. If no prior information is available, cadavers are collected during routine rounds at various distances from the facility. If the distance is great, the round may start from another collecting spot other than the facility with change of truck and driver, thus with potentially more handling of the cadaver. In this case, sub-contractors may be used for knackering. 2 Processing cadavers of bovines Bovines, killed or dead by accident, more than 24 months of age, are systematically screened for Bovine Spongiform Encephalopathy (BSE) during knackering. They are triaged on arrival and decapitated with knives. The worker in charge of cutting-up the cadaver wears steel mesh gloves, but not systematically a mask or hood. But, the veterinarian mandated to perform the sampling for ESB (who is not affiliated as facility personnel but with the DDPP) wears gloves, protective glasses and hood most often but not systematically. Bovines under 24 months of age, the skin of which is in a satisfactory state, are also table-cut. Before table cutting, the hide may be detached from the sub-cutaneous conjunctiva by using compressed air and then traction. Hides are the sent to a tanning facility after a stabilizing pre-treatment brine curing. 22 All the cadavers are put in a grinder hopper (or a crusher) around 10 by 5 meters, featuring a feed screw which performs a first course crushing. The grinder is never completely emptied and it is the permanent forward motion which plays the role of a prophylactic device (year round function). The crushed meat is then transferred to closed tanks, without risk of exposure, and is submitted to transformation (grinding into a given granulometry then sanitized by heat treatment) as defined in paragraph III of addendum V of the 1774/2002 European Regulations. The room in which triage, sampling for SBE, and table cutting are performed is cleaned superficially with a high pressure cleaner daily at the end of the workday. 3 Cleaning trucks Trucks are cleaned with a high pressure cleaner (open or confined space), and soiled water is collected and sent to a wastewater treatment station. The person responsible for cleaning up is usually the truck driver who may use a hood protecting him from spattering. 4 Protective measures for workers Boot and hand washers are installed on the site for disinfection outside of work zones and previously mentioned individual protective equipment is issued to the personnel (gloves, goggles, hoods). Workers are given occupational wear and must shower and change on the work before going home. Passive spreading of spores outside of facilities is thus theoretically impossible. 23