PPHSN Guidelines SARS 9th April 03
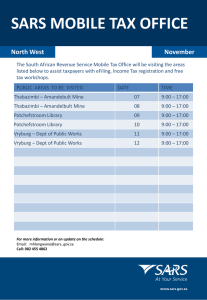
advertisement

PPHSN Guidelines
For The Preparedness, Surveillance And
Response To Severe Acute Respiratory
Syndrome (SARS) in Pacific Island Countries
And Territories
April 9th 2003
SARS is a new disease syndrome. Our knowledge about the best way to
prevent and treat it is constantly evolving. These guidelines will be
continuously updated. Please regularly check PPHSN website for the most up
to date guidance. These guidelines have also been ‘harmonised’ with the WHO
WPRO guidelines published on 4th April.
PPHSN. SARS Guidelines
09/04/2003
1
Table of Contents
BASIC DISEASE FACTS (updated 09.04.2003) .................................................................................... 4
Background ............................................................................................................................ 4
Description of disease ............................................................................................................ 4
Epidemiology ......................................................................................................................... 4
Agent and infectious dose ............................................................................................................................. 4
Source ........................................................................................................................................................... 4
Occurrence .................................................................................................................................................... 4
Mode of transmission .................................................................................................................................... 5
Period of communicability ............................................................................................................................ 5
Incubation period .......................................................................................................................................... 5
Vulnerable population sub-groups ................................................................................................................ 5
Risk in the Pacific ......................................................................................................................................... 5
SURVEILLANCE (updated 09.04.2003) ................................................................................................. 6
PPHSN Case Definitions for hospital based surveillance ..................................................... 6
Suspected case............................................................................................................................................... 6
Probable case ................................................................................................................................................ 6
Surveillance and reporting .................................................................................................... 6
Minimum dataset .................................................................................................................... 7
PREPAREDNESS – INITIAL ACTION AND RESPONSIBILITIES (updated 09.04.2003) ..................... 8
Staff responsibilities for the various actions .......................................................................... 8
Clinical assessment of suspected patients.............................................................................. 9
Enhanced surveillance ........................................................................................................... 9
Communications (between members of team and with outside bodies, media etc.) .............. 9
Laboratory diagnosis ............................................................................................................. 9
Initial community interventions ........................................................................................... 10
External (international) reporting, requests for support, & coordination among agencies10
CASE MANAGEMENT – the clinical response (updated 09.04.2003) ................................................. 11
Investigations ....................................................................................................................... 11
CXR ............................................................................................................................................................ 11
FBC ............................................................................................................................................................. 11
Other ........................................................................................................................................................... 11
Management of suspect cases .............................................................................................. 11
In-flight care of suspected case of SARS .................................................................................................... 11
General care of suspected case of SARS .................................................................................................... 11
Management of probable cases ........................................................................................... 12
Specific Treatment ............................................................................................................... 12
Hospital discharge and follow-up........................................................................................ 13
HOSPITAL INFECTION CONTROL (updated 09.04.2003) .................................................................. 14
Care for patients with probable SARS ................................................................................. 14
General Principles ....................................................................................................................................... 14
Principles of isolation.................................................................................................................................. 14
PPHSN. SARS Guidelines
09/04/2003
2
Principles of Personal Protective Equipment (PPE) .................................................................................... 15
Who should use PPE? ................................................................................................................................. 16
Minimum PPE to be worn ........................................................................................................................... 16
How should PPE be used?........................................................................................................................... 16
Masks................................................................................................................................................. 16
Goggles/Eye wear .............................................................................................................................. 16
Putting on PPE before entering isolation area (In order of dressing) ................................................ 16
Taking off PPE when leaving isolation area ...................................................................................... 17
Linen, cleaning and clinical waste .............................................................................................................. 17
MANAGEMENT OF CONTACTS OF SUSPECTED & PROBABLE CASES (updated 09.04.2003) ... 18
General ................................................................................................................................ 18
Contact tracing .................................................................................................................... 18
Contacts of probable cases .................................................................................................. 19
Contacts of suspected cases ................................................................................................. 19
Contacts of suspected cases on aircraft ............................................................................... 19
REDUCING THE RISK OF IMPORTING SARS THROUGH INTERNATIONAL TRAVEL (updated
09.04.2003) ........................................................................................................................................... 20
WHO recommendations to limit the spread of SARS by international travel ...................... 20
Travellers' Alert ................................................................................................................... 20
Advice to airline staff and national airport health authorities ............................................ 21
Disinfection of aircraft ......................................................................................................... 21
REFERENCES AND FURTHER SOURCES OF INFORMATION (updated 09.04.2003) .................... 22
ANNEXES (updated 09.04.2003) ......................................................................................................... 23
PPHSN. SARS Guidelines
09/04/2003
3
Severe Acute respiratory Syndrome (SARS)
BASIC DISEASE FACTS (updated 09.04.2003)
Background
As of 08 April 2003, reports of over 2671 cases, including 103 deaths, of Severe Acute Respiratory
Syndrome (SARS), an atypical pneumonia of unknown aetiology, have been received by the World
Health Organization (WHO) since 16 November 2002. WHO is coordinating the international
investigation of this outbreak and is working closely with health authorities in the affected countries to
provide epidemiological, clinical and logistical support as required.
SARS was first recognised on the 26 February 2003 in Hanoi, Viet Nam, but the epidemic started in
Guangdong in November 2002. Local transmission occurred in the following areas: Guangdong and
Shanxi provinces and the Special Administrative Region of Hong Kong in China, Taiwan in China,
Hanoi in Vietnam, Singapore and Toronto in Canada. Only imported cases were reported in 13 other
countries.
It is currently agreed that a new coronavirus (“SARS virus”) is the major
causative agent of SARS. The main symptoms and signs include high fever (>38 degrees Celsius),
cough, shortness of breath or breathing difficulties. Approximately 10 percent of patients with SARS
develop severe pneumonia; about half of these have needed ventilator support.
As of 09 April the majority of cases have occurred in people who have had very close contact with
other cases; for this reason, health care workers are at particular risk.
Description of disease
The syndrome begins with fever for 1-2 days, then a dry cough or dyspnea for 2-3 days. Atypical
pneumonia develops on day 4-5 in the majority of cases. It is initially unilateral but after a further 1-3
days it often becomes bilateral, progressing to extensive "white-out" on chest XRay.
The disease then takes 1 of 2 courses:
A) the patient improves (80-90% of cases) and recovers over the next 4-7 days; or
B) the patient deteriorates severely on day 6-7 with respiratory distress (10-20% of cases).
50% of patients in category B require mechanical ventilation. The mortality rate in this sub-group is
high. During the early phase of the outbreak, around 50% of type B cases have died, giving an overall
CFR of 5-10%. Risk factors for poor outcome are not clear, apart from the severity of illness and the
need for mechanical ventilation. So far SARS has affected predominantly adults aged 20-70 yrs. Very
few cases have occurred in children.
All modes of transmission have yet to be determined. Aerosol and/or droplet spread is likely as is
transmission from body fluids. Respiratory isolation, strict respiratory and mucosal barrier nursing are
recommended for cases. Cases should be treated as clinically indicated. (see below for further
details).
Epidemiology
Agent and infectious dose
The search has been progressively narrowed to members of the paramyxovirus and coronavirus
families, and it is currently agreed that a new coronavirus, “SARS virus”, is the major
causative agent of SARS. The infectious dose is unknown.
Source
From the knowledge available to date the source of an infection is another person who is ill with
SARS.
Occurrence
So far all cases reported from outside the affected areas have a history of travel in the previous 10
days through an affected area OR close contact with a case of SARS.
PPHSN. SARS Guidelines
09/04/2003
4
Mode of transmission
The agent is spread from person to person through respiratory droplets and contact (including
fomites). Airborne transmission appears uncommon if it occurs at all and transmission through
environmental factors is being investigated.
Period of communicability
Not known but particularly infectious once respiratory symptoms appear. A lower risk of transmission
is likely to be present during the prodromal phase (see figure 1).
Incubation period
The incubation period is thought to be 2-7 days exceptionally 10 days, most commonly 3-5 days
Vulnerable population sub-groups
Health care workers and immediate family members and friends of SARS cases are at extreme risk of
becoming a case.
Secondary cases from air travel are reported.
Insufficient information available at this stage about who is at risk to become severe ill and die. But
probably worse outcomes can be expected in individuals with underlying respiratory and cardiac
illnesses such as asthma, COPD and heart disease.
Risk in the Pacific
The main risk in the Pacific is the importation of cases from affected areas with subsequent local
transmission to close contacts including health workers.
Figure 1: Clinical picture in SARS patients
Exposure to SARS
Incubation period
~2 to 10 days
fever, myalgia, dry
cough, headache
(early symptoms)
non-productive cough
shortness of breath
Prodrome
Lower respiratory
phase
~1 to 2 days
From day 4 onwards
Recovery
80-90%
up to 13 days reported
Infectivity
None or very low
PPHSN. SARS Guidelines
09/04/2003
Low
Very high
5
Acute
respiratory
distress
syndrome
50% require
ventilation
SURVEILLANCE (updated 09.04.2003)
Please note that a SINGLE case of suspected/probable SARS is an outbreak.
PPHSN Case Definitions for hospital based surveillance
Suspected case
Clinicians should be alert for persons with onset of illness after November 1, 2002 with:
Fever (>38° C)
AND
One or more signs or symptoms of respiratory illness, including:
cough,
shortness of breath,
difficulty breathing,
AND
A history of either of the following:
close contact*, within 14 days of onset of symptoms, with a person who has been diagnosed
with SARS.
history of travel, within 14 days of onset of symptoms, to an area** (see table below) in which
there are reported foci of transmission of SARS.
* close contact means having cared for, having lived with, or having had direct contact
with respiratory secretions and body fluids of a person with SARS.
Affected Areas** - Severe Acute Respiratory Syndrome (SARS)
Country
Canada
Singapore
China
China
Viet Nam
Area
Toronto
Singapore
Guangdong Province, Hong Kong Special Administrative Region of China,
Shanxi Province
Taiwan
Hanoi
Last revised 09 April 2003
**An "Affected Area" is defined as a region at the first administrative level where the country is
reporting local transmission of SARS.
Note
In addition to fever and respiratory symptoms, SARS may be associated with other symptoms
including: headache, muscular stiffness, loss of appetite, malaise, confusion, rash, and diarrhea.
Probable case
A suspected case with chest X-ray findings of pneumonia or adult respiratory distress
syndrome.
OR
A person with an unexplained respiratory illness resulting in death, with an autopsy
examination demonstrating the pathology of Respiratory Distress Syndrome without an
identifiable cause.
Surveillance and reporting
If travel questionnaires are issued to arriving passengers or passengers from affected areas
are requested to identify themselves, record number of arrivals with a travel history that puts
them in the at risk group (travel to an affected area within the previous 14 days).
Report all suspected/probable cases immediately to National Public Health Authorities, using
the PPHSN reporting form (see ANNEX 2).
Report all suspected/probable cases immediately to PPHSN Coordinating Body (CB) Focal
point or WHO Suva (through local WHO Office if present) using the PPHSN reporting form (a
PPHSN. SARS Guidelines
09/04/2003
6
copy of the completed form used to report to the National Public Health Authorities) (see
contacts list in ANNEX 1)
Report to PacNet or PacNet-restricted.
Minimum dataset
Upon arrival:
o affected area visited in the last 10 days and presence of symptoms.
o identity of individuals and residence/contact in the next 14 days (purpose: active
surveillance/retrieving contacts of suspected or probable case on board a plane or boat).
o national health or port authorities may consider routinely collecting a copy of the passenger
seating list of every flight arriving from SARS affected areas.
Please see PPHSN reporting form for data items.
For PacNet or PacNet-restricted, same as on reporting form, EXCEPT reporter and patient details
(you can send the form on PacNet or PacNet-restricted, but delete the 2nd page).
PPHSN. SARS Guidelines
09/04/2003
7
PREPAREDNESS – INITIAL ACTION AND RESPONSIBILITIES (updated 09.04.2003)
Key points
Countries should set up a response structure at the national level as a matter of
urgency and develop a contingency plan for SARS.
A cornerstone of this plan is close collaboration between public health departments
(disease control unit), clinical departments treating patients and laboratories.
Staff responsibilities for the various actions
At the ministry of health level, a task force including the EpiNet team and with one national focal
point, an expert committee and a surveillance unit with a hotline must be set up.
For the purpose of proper SARS control in hospital environment, this task force and expert
committee should include a member experienced in hospital infection control, and who can advise
on isolation and barrier nursing issues.
Priority functions of the task force are to:
o identify the facility(ies) where suspected and probable cases of SARS can be nursed.
o perform an inventory of supplies required for nursing such patients (using WPRO SARS
Preparedness Kit contents list).
o plan how contacts of suspect/probable cases will be managed
o liaise with customs/immigration authorities on the best way to provide information to
arriving passengers, record travel details for surveillance and plan of action if an
individual arrives ill on a plane with suspected SARS.
The task force should be responsible for all the issues concerning SARS including establishing
good communications. The expert committee should be responsible for making a decision on the
public health response to reported cases.
An urgent task of this task force will be establishing a national surveillance system. The
surveillance system should also include private hospital and clinics. Information should be
provided for the media and general public.
Designate at least one hospital to isolate cases and one laboratory responsible for managing
clinical samples. Good communications should be established between the national focal point
and the designated hospital and the designated laboratory. (see Figure 2)
The tasks at national level includes development of inventory of barrier nursing supplies,
community infection control, quarantine at port of entry, and public awareness (avoiding panic).
Figure 2: Information Flows
WHO or PPHSNCB Focal Point
1 & 2 Information collected from government and private hospitals, the media and the general public
3 Reports should be verified by surveillance unit
4 The information should be shared with the designated hospital and laboratory focal point as well as the WHO focal point if
available, or PPHSN Coordinating Body focal point (SPC).
5 In principle, probable cases should be transferred to the designated isolation facility for further assessment, treatment and
infection control. This should be decided by the task force or expert committee on a case-by-case basis
6 Specimens should be collected under the supervision of the laboratory focal point following the guidelines and transferred to
an international laboratory if necessary
PPHSN. SARS Guidelines
09/04/2003
8
Clinical assessment of suspected patients
Clinicians must be aware of the symptoms and signs of SARS.
Patients with symptoms of SARS and a history of travel from an affected area or contact with
a case of SARS should be triaged immediately to designated examination rooms or wards to
minimize exposure to other patients and staff.
Where feasible, separate specific reception areas for triaging patients who may have SARS
should be established
Patients with suspected SARS should be issued with surgical masks.
Medical and nursing staff must take precautions when examining the patient ie barrier
nursing.
Where material resources for barrier nursing are scarce, available supplies should be used
sparingly in triage settings (such as by limiting the number of staff working in this area), so in
the event of a SARS admission supplies will not have been exhausted.
Obtain and record detailed clinical, travel and contact history including occurrence of acute
respiratory diseases in contact persons during the last 10 days.
Obtain chest X-ray (CXR) and full blood count (FBC).
(See example patient management flow chart in ANNEX 4)
Enhanced surveillance
Complete PPHSN reporting form and send immediately to National Health Authorities, with a
cc to PPHSN-CB Focal Point or WHO Suva (through local WHO Office if present). Also send
immediately the form WITHOUT reporter and patient details (i.e. page 2) to PacNet or
PacNet-restricted
Identify close contacts and give information to contacts. Screen any contacts with compatible
symptoms as for suspected cases.
Communications (between members of team and with outside bodies, media etc.)
Ensure that lines of communication are clear.
Identify spokesperson for the team who will be the focal point for media briefings and will
liaise with international agencies eg WHO/SPC (this could be the EpiNet team Focal Point or
another person).
Laboratory diagnosis
The agent causing SARS remains to be established. There are no specific diagnostic tests at
this stage.
For suspected cases where the diagnosis of SARS is by exclusion and the patient is not very
ill (ie no chest X-ray changes compatible with SARS). It is reasonable to take specimens for
diagnostic purposes. However health care workers must take full barrier nursing
precautions to protect themselves from aerosols or splashing/splattering of blood or
other body fluids.
For probable cases where the diagnosis of SARS is very likely and particularly if the patient
has significant respiratory symptoms. The clinicians must perform a risk/ benefit analysis.
There have been documented cases of transmission to HCWs during
diagnostic/therapeutic procedures, particularly those prone to the generation of
aerosols. Therefore the priority should be for tests likely to influence the clinical management
of the patient.
If specimens are collected for diagnostic testing (rather than clinical management), they
should be stored under appropriate conditions. At this stage, the three laboratories in our
region that have agreed to receive specimens are:
o Institute Pasteur, New Caledonia
o WHO Collaborating Centre for Reference and Research on Influenza, Australia
o Clinical Virology, Communicable Disease Programme, Institute of Environmental
Science and Research (ESR), New Zealand
(See Contact List in ANNEX 1 for addresses)
PPHSN. SARS Guidelines
09/04/2003
9
Initial community interventions
Provide suitable information to arriving passengers (particularly those who have traveled
through affected countries) about the risks of SARS and where they can go to for advice and
assistance (as example, see Advice to Arriving Travelers in ANNEX 5).
Simple health education messages should be communicated to the public via appropriate
media (see Health Advices from Hong Kong in ANNEXES 6 and 7 for examples).
WHO has introduced new travel advice on 4th April advising against travel to the worst
affected areas (Hong Kong and Guandong Province in China), unless essential. The PPHSN
SARS Task force has also produced a travel advisory that goes further than WHO (see
ANNEX 3). This careful attitude helps to avoid SARS long-distance spread through travel to
and from infected zones and prevents the importation of SARS "home" (lots of close
contacts...). This is particularly important in places where control measures may not be easy
to implement (and SARS importation may have serious public health consequences).
External (international) reporting, requests for support, & coordination among agencies
Report all suspect and probable cases to PPHSN/WHO using the PPHSN reporting form
Contact PPHSN-CB Focal Point or WHO South Pacific if additional information or assistance
is required (see contact list in ANNEX 1).
PPHSN. SARS Guidelines
09/04/2003
10
CASE MANAGEMENT – the clinical response (updated 09.04.2003)
Investigations
CXR
Chest radiographs might be normal during the febrile prodrome and throughout the course of
illness. However, in a substantial proportion of patients, the respiratory phase is characterized
by early focal infiltrates progressing to more generalized, patchy, interstitial infiltrates. Some
chest radiographs from patients in the late stages of SARS have also shown areas of
consolidation.
In typical severe cases, chest x-ray findings begin with a small unilateral patchy shadow, and
progress over 24 - 48 hours to become bilateral, generalized, interstitial/confluent infiltrates.
Patchy chest x-ray changes are sometimes noted in the absence of chest symptoms. Acute
respiratory distress syndrome might be observed in the end stage. Post-mortem lung tissue
shows generalized alveolar damage and lymphocytosis without obvious viral inclusion bodies.
FBC
Initially the blood picture is often normal. However, by day 3 - 4 of the illness, lymphopenia is
commonly observed (>50%), and less commonly, there might be thrombocytopenia. If SARS
is complicated by secondary bacterial infection, neutrophilia may occur.
Other
Elevated hepatic transaminases and creatine phosphokinase levels are seen early in the
respiratory phase of the disease.
Management of suspect cases
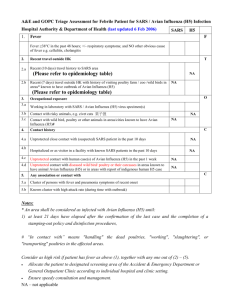
Figure 3: Algorithm For Triaging Potential SARS Cases
Within the
previous 14
days does the
patient have a
recent history
of travel to an
affected area
or close
contact with a
SARS patient?
Yes
Has fever
(>38°C)
developed
within 14 days
of leaving
affected area,
or contact with
known SARS
patient?
Yes
ISOLATE AND INVESTIGATE
Treat as possible SARS
case; isolate / barrier
nursing; implement local
SARS plan; notify local
health authorities and WHO
country representative about
possible SARS case
No
No
No
Is the patient still within known
incubation period for SARS (14
days) following travel/contact
with SARS case?
Yes
Give information about personal surveillance for fever during
incubation period (refer to figure 5 for risk assessment); treat
nonSARS medical illness
Provide information about SARS; treat nonSARS medical illness
In-flight care of suspected case of SARS
If a passenger on a flight from an affected area becomes noticeably ill with a fever and
respiratory symptoms, the following action is recommended for cabin crew:
o The passenger should be, as far as possible, isolated from other passengers and
crew
o The passenger should be asked to wear a protective mask and those caring for the ill
passenger should follow the infection control measures recommended for cases of
SARS
o A toilet should be identified and made available for the exclusive use of the ill
passenger
o The captain should radio ahead to alert the airport of destination so that quarantine or
health authorities are altered to the arrival of a suspect case of SARS
o On arrival, the ill passenger should be placed in isolation and assessed by port health
authorities
General care of suspected case of SARS
Patients with symptoms of SARS should be triaged immediately (see Figure 3) to designated
examination rooms or wards to minimize exposure to other patients and staff.
PPHSN. SARS Guidelines
09/04/2003
11
Patients with suspected SARS should be issued with surgical masks
obtain and record detailed clinical, travel and contact history including occurrence of acute
respiratory diseases in contact persons during the last 14 days
obtain chest X-ray (CXR) and full blood count (FBC)
if CXR is normal and:
Individual is a close contact of a case of SARS
(high risk of becoming a case of SARS):
Admit to hospital using full isolation and barrier nursing procedures
NURSE separately from probable cases of SARS
OR
Individual has a history of travel to an affected area
(Lower risk of becoming a case of SARS):
Provide advice on personal hygiene, avoidance of crowded areas and public
transportation, remain at home until well [consider “home isolation" until incubation
period over].
Discharge with CLEAR advice to seek medical care if respiratory symptoms worsen
if CXR demonstrates uni- or bi-lateral infiltrates with or without interstitial infiltration
SEE MANAGEMENT OF PROBABLE CASES
Management of probable cases
Hospitalise under isolation or cohorted with other SARS cases.
Cases need to be in the best isolation facility that can be arranged and MUST be nursed
using strict barrier techniques including gown or preferably overalls, gloves, boots or overshoes, HEPA or N95-100 mask (or at least a surgical mask if nothing else available) and
goggles. Avoid interventions which may cause aerolisation of respiratory secretions, such as
nebulisers, chest physiotherapy, bronchoscopy, and any intervention which may release
respiratory secretions.
Samples for laboratory investigation (if possible) and exclusion of known causes of atypical
pneumonia:
o throat and/or nasopharyngeal swabs 1
o blood for culture and serology (acute specimen and convalescent specimen taken
after 3 weeks)
o bronchoalveolar lavage
o post mortem examination as appropriate
Samples should be investigated in laboratories with proper containment facilities (BL3).
CXR as clinically indicated
treat as clinically indicated
Specific Treatment
1
Treatment regimens have included several antibiotics to presumptively treat known bacterial
agents of atypical pneumonia.
In several locations, therapy has included antiviral agents such as oseltamivir or ribavirin; the
effectiveness of these treatments is uncertain.
Steroids have also been administered orally or intravenously to patients in combination with
ribavirin and other antimicrobials. Intravenous steroids may be associated with improved
outcomes in severe cases.
At present, the most efficacious treatment regime, if any, is unknown.
At the time of admission WHO recommends antibiotic therapy that will cover the common
causative organisms in acquired pneumonia (including atypical pneumonia). Prophylactic
antibiotics should also be used to prevent secondary bacterial infection.
best specimen for (known) respiratory viruses is nasal swab
PPHSN. SARS Guidelines
09/04/2003
12
Hospital discharge and follow-up
The period of communicability of the agent that causes SARS is unknown at this time. WHO advises
that patients are fit for discharge if:
Clinical symptoms/findings:
Afebrile for 48 hours
Resolving cough
Laboratory tests: if done and previously abnormal
White cell (lymphocyte) count returning to normal
Platelet count returning to normal
Creatinine phosphokinase returning to normal
Liver function tests returning to normal
Plasma Sodium returning to normal
C reactive protein returning to normal
Radiological findings:
Improving chest x-ray changes
Follow-up for convalescent cases
Discharged convalescent patients should be asked to return to hospital If they have an
elevated temperature of 38 degrees and above on two consecutive occasions they should
report to the health care facility from which they were discharged.
Follow up is recommended at one week (or before if decided so by the clinician) at which time
they should have a repeat chest x-ray, full blood count and any other blood tests that were
previously abnormal.
The patient should be followed up by the health care facility from which they were discharged.
If possible they should not return to their home island.
Subsequent follow-ups are recommended until the chest x-ray and patient’s health returns to
normal.
As part of the follow-up convalescent serology should be taken is taken at 3 weeks (if an
acute serum specimen was taken) after the date of the presenting symptoms and provided to
the health care facility from which they were discharged.
Until more is known about the aetiological agent, and the potential for continued carriage (and
hence the risk of continuing transmission) a cautious approach is warranted.
WHO advises that following discharge from hospital convalescent cases should be advised to
wait for a minimum of 14 days, before considering returning to work/school/college. This is
twice the known maximum incubation period. During this period they should stay indoors,
keeping contact with others to a minimum. Clear instructions should be given to convalescent
cases to return to the health care facility from which they were discharged [see above] if their
condition deteriorates and any further symptoms develop.
PPHSN. SARS Guidelines
09/04/2003
13
HOSPITAL INFECTION CONTROL (updated 09.04.2003)
[See also NEW ZEALAND MOH Infection Control advice for the management of patients with
suspected Severe Acute Respiratory Syndrome (SARS) in ANNEX 8 for an example of measures that
can be adapted depending on the resources available. Alternatively see WHO publication Infection
Control for VHF in the African Health Care Setting for simple guidance. This is available on the
PPHSN website (http://www.spc.int/phs/PPHSN/Outbreak/SARS_Outbreak.htm).
Key points
WHO advises strict adherence with the barrier nursing of patients with
SARS using precautions for airborne, droplet and contact transmission.
Triage nurses should rapidly divert persons presenting to their health
care facility with flu-like symptoms to a separate assessment area to
minimise transmission to others in the waiting areas.
Suspect cases should wear N 95 masks (surgical masks if N 95 not
available) until SARS is excluded.
Staff involved in the triage process should wear a N 95 mask and wash
hands :
o before and after contact with any patient,
o after activities likely to cause contamination and
o after removing gloves
Probable and suspected cases MUST be nursed SEPARATELY, and
suspected/probable cases must NEVER be placed with other patients for
observation.
Care for patients with probable SARS
Patients with probable SARS should be isolated and accommodated as follows in descending
order of preference:
o Negative pressure rooms with the door closed
o Single rooms with their own bathroom facilities
o Cohort placement in an area with an independent air supply, exhaust system and
attached bathroom facilities.
Note Turning off air conditioning and opening windows for good ventilation is
recommended if an independent air supply is not possible. Please ensure that if
windows are opened they are away from public places
General Principles
WHO advises strict adherence with the barrier nursing of patients with SARS using precautions
for airborne, droplet and contact transmission
Isolation and avoidance of unnecessary contact. Minimise the number of HCWs that will
have contact with SARS patient(s). In addition WHO recommends that any specimens for
laboratory testing MUST be taken by the physician designated to care for the SARS
patient(s).
Use of personal protective equipment (PPE) for all in close proximity
Strict personal hygiene
Masking of patient to reduce respiratory spread
Principles of isolation
Isolation facilities should be identified beforehand. They should include the following (see
figure 4):
o Isolation room: patient care room, with no airflow to other rooms.
o Changing room. Separate areas in room for storage of outside clothes, and removal
of PPE.
o Outside the isolation room (in changing-room, where present) – direct access to a
biohazard waste bag (with foot-operated lid) and a handbasin is necessary
o General access area (ie rest of hospital)
Suspect SARS cases should be individually isolated
o HCWs should disinfect their hands and change PPE between patients
o Disinfect or use separate ward equipment (tourniquets etc).
PPHSN. SARS Guidelines
09/04/2003
14
Probable SARS patients may be treated in cohort isolation (>1 per room)
o Place a screen between patients.
o Staff must wash hands between patients
NEVER put suspect cases in the same room as probable cases Central air-conditioning
should be turned off unless the room can be isolated from the system.
Open external windows to areas with no public access.
Keep doors closed
Visits by family and non-essential staff should be avoided wherever possible
All patient care devices (e.g. tourniquets, tubing) must be restricted to the patient, and
disposed of or cleaned and disinfected by staff wearing PPE.
Transport of SARS patients should follow the same principles of isolation, including mask on
patient, full PPE at all times for all staff, minimal contact, strict hygiene /washing, and
complete disinfection of all transport and equipment.
Figure 4: General Principles of isolation unit
ISOLATION
WASH/TOILET
A
B
ISOLATION ROOM
Negative pressure/
(e.g. blow air out of
E
window with fan)
D
A
D
A
E
A.
B.
C.
D.
E.
GENERAL
ACCESS AREA
CHANGE
ROOM
C
Disinfection station
Storage for general ward clothes, new PPE.
Biohazard bag for used PPE disposal.
Wall-mounted alcohol hand-wash dispensers.
Windows…external only. Keep clear of public.
Principles of Personal Protective Equipment (PPE)
PPE reduces but does not completely eliminate the possibility of infection.
PPE is only effective if used correctly and at all times where contact may occur.
Any contact between contaminated (used) PPE and surfaces / clothing / people outside the
isolation area must be avoided.
Used PPE must be sealed in appropriate disposal bags and incinerated or decontaminated.
The use of PPE does not replace basic hygiene measures such as hand-washing, washing is still
essential to prevent transmission.
Exposure to the infected patient should be kept to an absolute minimum necessary for the level of
care required.
Visits by non-staff should be avoided where possible.
The patient should be as self-caring as possible, and the staff team assigned to care for the
patient should be kept to a minimum.
Staff should be strictly supervised and be experienced in infection control.
PPHSN. SARS Guidelines
09/04/2003
15
Who should use PPE?
PPE should be worn by:
o All HCWs who provide direct patient care to SARS cases (keep to minimum
necessary for patients' condition);
o All support staff including medical aides, cleaners, laundry staff (keep staff to the
minimum necessary, designate SARS laundry staff, etc.);
o All laboratory staff who handle patient specimens from suspect cases (keep to the
minimum necessary for laboratory procedures);
o Family members who care for SARS patients (visits should be avoided where
possible)
o The patient(s) should wear a surgical mask (N95 preferable) when other people
are in the isolation area.
Minimum PPE to be worn
N95 mask as a minimum
Single pair of gloves
Disposable gown
Apron
Goggles
Footwear that can be decontaminated
How should PPE be used?
Masks
o Disposable masks should be discarded after 4-6 hours use. (patient's mask may be
reused by patient).
o It is essential that the mask makes a complete seal on the face (see manufacturer's
fitting instructions) at all times. Ensure seal is complete before approaching patient
o Masks cannot be worn with beards / unshaven faces.
o If a mask is splashed, wet, it should be changed using strict hand-washing and
gloves.
o N95 masks are recommended for use in the isolation room where close contact with
the patient and direct contamination with saliva / sputum (cough, sneezing etc) is not
likely. Ideally, masks should be splash-proof (e.g. 3M 1860 model) if available
o The patient should wear an N95 mask at all times when staff / other people are in
room.
o HEPA (P100, N100) masks are recommended for use during procedures likely to
generate aerosols or splattering of body fluids
o Standard surgical masks can be used by patients if N95 masks are not tolerated or
unavailable
o Standard surgical masks are NOT adequate protection for staff or visitors
Goggles/Eye wear
o Goggles should be worn at all times during patient contact
o They should be cleaned thoroughly in alcohol-based disinfectant solution prior to reuse
o UVEX goggles may be worn with glasses
o Safety glasses are not a good substitute for goggles and should only be used if
extreme heat and humidity prevents goggles from being tolerated.
Putting on PPE before entering isolation area (In order of dressing)
o Wear scrub suit or old set of thin clothes before entering the designated changing
room or area
o Put on shoe covers or boots with trousers tucked inside
o Put on outer laboratory gown or coveralls
o Put on impermeable apron
o Put on gloves with gown sleeve cuff tucked into glove
o Put on the mask and goggles
o Boots should be used for heavily contaminated / wet flooring and floor cleaning
PPHSN. SARS Guidelines
09/04/2003
16
Taking off PPE when leaving isolation area
o Wash gloved hands in >60% alcohol handwash solution (eg Sterillium). Disinfect
boots with 1% bleach.
o Using gloved hands, remove aprons, gowns, and shoe covers without contaminating
clothing underneath. Touch only outside of clothing. Place in biohazard disposal bag
o Remove gloves (fingers under cuff of second glove to avoid contact between skin and
outside of gloves).
o Wash hands in >60% alcohol hand-cleaning solution.
o Remove goggles then boots and place in separate containers (receptacle) with close
fitting lids for soaking and cleaning.
o Remove head cover and mask, place in biohazard disposal bag.
o Wash hands to elbows thoroughly in >60% alcohol hand cleansing solution, followed
by soapy water.
o Change into street clothing and wash hands in soapy water before leaving facility.
o Never wear PPE in general ward area.
o Plan ahead when entering the isolation area (or laboratory), so that all necessary
equipment is available, and all necessary patient care activities are completed in one
visit.
o If staff must temporarily leave the isolation area, a complete change of PPE and
thorough hand washing (above) must be performed each time.
Linen, cleaning and clinical waste
Linen from the patients should be prepared on site for the laundry staff. Appropriate PPE should
be worn in this preparation and the linen should be put into biohazard bags.
The room should be cleaned by staff wearing PPE using a broad spectrum disinfectant of proven
antiviral activity.
Standard precautions should be applied when handling any clinical wastes. All waste should be
handled with care to avoid injuries from concealed sharps (which may not have been placed in
sharps containers). Gloves and protective clothing should be worn when handling clinical waste
bags and containers. Where possible, manual handling of waste should be avoided. Clinical
waste must be placed in appropriate leak-resistant biohazard bags or containers labelled and
disposed of safely.
PPHSN. SARS Guidelines
09/04/2003
17
MANAGEMENT OF CONTACTS OF SUSPECTED & PROBABLE CASES (updated 09.04.2003)
Key points
Close contacts of a probable or suspect case of SARS are at high risk of becoming a case,
and should be isolated in the community during their potential incubation period. Attack
rates in health care workers caring for the initial cases of SARS is >50%.
Travellers from affected areas should be given advice about whom to contact, and what to
do if they develop a fever within their potential incubation period.
Health departments should assign staff to undertake contact tracing and daily review of
contacts in the community. Ideally, this should be in conjunction with a 24-hour SARS
hotline.
General
Most cases of SARS have been attributable to transmission through close contact with other
cases. These include people living with or caring for cases at home or in hospital, who have
prolonged exposure to droplet spread and/or body fluids including respiratory secretions. The
incubation period is short, typically 2 to 7 days, but exceptionally up to 13 days (see figure 5).
Close contacts should be informed that they may be at risk of contracting the infection. They
should be advised to seek medical care urgently if they develop fever and respiratory
symptoms within ten days of their last contact with a case.
Provide reassurance.
Record name and contact details.
Contact tracing
The aim of contact tracing is to identify individuals who had close contact with a SARS case,
to advise them of that contact, and to give them advice about personal isolation and
observation for symptoms of SARS, particularly fever.
When a case of suspect or probable SARS is identified, the Department of Health should
undertake contact tracing, in a similar manner to that undertaken for other infectious
diseases.
In the majority of cases, transmission of SARS appears to occur through either droplet spread
or direct contact. The level of exposure that needs to be identified when contact tracing
is close contact2.
Figure 5 Risk assessment algorithm for contacts / travellers during
potential incubation period
CONTACT
Within 14
days
TRAVELLER FROM
AFFECTED AREA
Within 14 days
No
Home isolation
for duration of
incubation period
Yes
Possible case of SARS,
isolate and transport using
barrier nursing techniques
No
No isolation; personal
surveillance for fever
during incubation
period
FEVER
WITH NO
OBVIOUS
CAUSE?
FEVER
WITH NO
OBVIOUS
CAUSE?
2
close contact means having cared for, having lived with, or having had direct contact
with respiratory secretions and body fluids of a person with SARS.
PPHSN. SARS Guidelines
09/04/2003
18
Contacts of probable cases
Give information on SARS to the contact
Place under active surveillance for 14 days and ideally insist on “home isolation”.
Give the contact a mask to wear if they develop respiratory symptoms, while waiting
for clinical assessment.
Ensure contact is visited or contacted daily by a member of the public health care team
Record temperature twice daily (the earliest symptom of SARS is fever):
o If contact develops any symptoms, contact to be assessed at health care facility
o The most consistent first symptom that is likely to appear is fever.
(NB in Hong Kong and Singapore the authorities are recommending that the children of probable
cases be kept away from school for 10 days from the date the parent was hospitalised as a
precaution.)
Contacts of suspected cases
Give information on SARS to the contact
Place under passive surveillance for 14 days
Give the contact a mask to wear if they develop respiratory symptoms, while waiting
for clinical assessment.
Contact is free to continue with usual activities; however:
o Contact to self-report to public health authority if contact develop any symptoms
o The most consistent first symptom which is likely to appear is fever
Provide advice in the event of fever or respiratory symptoms to:
o immediately report to doctor/physician/health authority
o not report to work until advised by health authority
o avoid public places until advised by health authority
o minimize contact with family members and friends
Contacts of suspected cases on aircraft
If a passenger or member of aircrew has suspected/probable SARS on arrival and the immediate
medical assessment of the ill passenger excludes SARS as a possible cause of his/her illness,
the passenger should be referred to local health care facilities for any necessary follow up. If
however, the initial medical assessment conducted in the airport concludes that the passenger is
a suspect or probable case of SARS the following action should be taken:
All close contacts3 of the ill passenger should be identified during the flight.
All passengers should provide, to the health authorities, identification and details of their
place(s) of residence for the next 14 days.
National health or port authorities may consider routinely collecting a copy of the passenger
seating list of every flight arriving from SARS affected areas.
All passengers should be given information about SARS and advised to seek immediate
medical attention if they develop any symptoms of SARS within 14 days of the flight.
When seeking medical attention they should ensure that all those treating them are aware
that they have been in contact with a suspect case of SARS.
All passengers should be allowed to continue to travel so long as they are well. They must
be informed that they may be refused permission to continue their journey if they
develop fever and/or other symptoms.
If over time it becomes apparent that the suspect case is a probable case of SARS, the health
authority where the case is being cared for should inform other health authorities in those
areas in which the close contacts reside so that active surveillance of each close contact is
undertaken until 14 days after the flight. Health authorities may consider extending active
surveillance to other passengers as well.
3
For the purposes of air travel, a close contact is defined as:
passengers sitting in the same seat row or 4 rows in front or behind the sick passenger
all flight attendants on board
anyone having intimate contact, providing care or otherwise having contact with respiratory
secretions of the ill passenger
anyone on the flight living in the same household as the ill passenger
If it is a flight attendant who is considered to be a SARS case, all passengers are
considered to be contacts
PPHSN. SARS Guidelines
09/04/2003
19
REDUCING THE RISK OF IMPORTING SARS THROUGH INTERNATIONAL TRAVEL (updated
09.04.2003)
Key points
On 2 April 2003 WHO recommended that "persons travelling to Hong Kong and Guangdong
Province of China consider postponing non-essential travel." An earlier WHO
recommendation suggested that countries where there had been cases of SARS enhance
screening at departure points to prevent suspect cases from travelling.
Countries should develop national SARS-related travel policies.
Countries should develop information sheets (such as a health alert card) for international
travellers. This should detail the incubation period for SARS, and explain what they should
do and who they should report to if they develop a fever.
Airlines should develop polices to prepare for and manage a potential case of SARS
detected in-flight, and how to manage other passengers on the same flight.
WHO recommendations to limit the spread of SARS by international travel
WHO released its first SARS-related travel advice on 15 March 2003
(http://www.who.int/csr/sarsarchive/2003_03_15/en/). It provided advice to travellers who
developed SARS-like symptoms, and recommendations to airlines on what to do if a possible
SARS case was identified in-flight.
On 27 March 2003, WHO recommended new measures to prevent travel-related spread of
SARS (http://www.who.int/csr/sarsarchive/2003_03_27/en/). These included a screening
process to identify people with possible SARS symptoms leaving an affected area. Individual
countries, as they make their own travel advice, may wish to take into account national
considerations. Information updates on affected areas and the number of SARS cases,
deaths and evidence of local transmission are issued daily by WHO
(http://www.who.int/csr/sars).
On 2 April, 2003, WHO recommended that "that persons travelling to Hong Kong and
Guangdong Province of China consider postponing non-essential travel."
(http://www.who.int/csr/sarsarchive/2003_04_02/en/). This recommendation is based on
concerns about more general community transmission of SARS in these regions. This is a
temporary recommendation and it will be reassessed in the light of the evolution of the SARS
outbreak in currently affected areas. Other areas of the world could become subject to
recommendations if the situation demands. This recommendation applies only to travellers
entering Hong Kong SAR and Guangdong province and not to passengers directly transiting
through international airports within those areas.
Travellers' Alert
All travellers, including airline/ship crews, should be aware of the main symptoms and signs of
SARS. They should seek immediate medical attention should fever occur, and ensure that
information about their recent travel is passed on to health care staff. Travellers who develop
these symptoms are advised not to undertake further travel until they have recovered.
Many countries are now distributing SARS health alert cards (for an example see ANNEX
5). These cards briefly describe the symptoms of SARS, advise travellers to seek immediate
medical care when showing these symptoms, specify the potential incubation period (14
days), and give a contact address and telephone number/hotline of a SARS referral centre.
Cards may also contain advice for physicians.
Some countries distribute SARS health alert cards to passengers arriving from SARS-affected
areas which combine this health alert information with a short questionnaire on the traveller's
health status (in this case the card has a perforation to allow the health questionnaire to be
collected by quarantine staff, while the health alert information remains with the traveller) (for
PPHSN. SARS Guidelines
09/04/2003
20
an example see ANNEX 5). This approach is designed to identify suspect SARS cases on
arrival. These cases would be referred to airport/port health authorities for assessment and
management (Figure 3).
The PPHSN SARS Task force has also produced a travel advisory that goes further than
WHO (see ANNEX 3). This careful attitude helps to avoid SARS long-distance spread through
travel to and from infected zones and prevents the importation of SARS "home" (lots of close
contacts...). This is particularly important in places where control measures may not be easy
to implement (and SARS importation may have serious public health consequences).
Advice to airline staff and national airport health authorities
See “In-flight care of suspected case of SARS”, page 11.
See “Contacts of suspected cases on aircraft “, page 19.
In order to respond to these recommendations, airlines will have to ensure that flights with
passengers from affected areas are provided with sufficient gloves, face masks and
disinfectant, and they should ideally ensure that a seat in an isolated area can be made
available when needed. Airlines must also make sure that flight attendants are properly
trained.
Disinfection of aircraft
See WHO Guide to Hygiene and Sanitation in Aviation (http://www.who.int/csr/ihr/guide.pdf).
Although these recommendations are mainly directed to air travel, the same procedures are
recommended for international travel from affected areas by sea, rail or road.
PPHSN. SARS Guidelines
09/04/2003
21
REFERENCES AND FURTHER SOURCES OF INFORMATION (updated 09.04.2003)
http://www.spc.int/phs/PPHSN/Outbreak/SARS_Outbreak.htm
http://www.who.int/csr/sars/en/
http://www.wpro.who.int/sars/
http://www.cdc.gov/ncidod/sars/
http://www.info.gov.hk/dh/ap.htm
http://www.phls.co.uk/topics_az/SARS/menu.htm
http://www.moh.govt.nz/sars
http://www.sante.gouv.fr/htm/dossiers/pneumapathies/
PPHSN. SARS Guidelines
09/04/2003
22
ANNEXES (updated 09.04.2003)
ANNEX 1 – List of Key Contacts (updated 09.04.2003)
ANNEX 2 – PPHSN Reporting Form (updated 09.04.2003)
ANNEX 3 – PPHSN Advice To Governments Regarding Travelers Arriving From SARS
Affected Areas (new)
ANNEX 3B – List Affected Areas 09 April 2003 – SARS (updated 09.04.2003)
ANNEX 4 – SARS Patient Management Flow Chart (example) (updated 09.04.2003)
ANNEX 5 – Advice to arriving travellers (2 examples, incl. The Solomon Islands)
ANNEX 6 – Health Advice on the Prevention of Respiratory Tract Infections
(example from Hong Kong MOH)
ANNEX 7 – Health Advice on the Prevention of Respiratory Tract Infections in Public Places
(example from Hong Kong MOH)
ANNEX 8 – New Zealand infection control advice for managing patients with SARS (updated
4th April)
ANNEX 9 – PPHSN country checklist and assessment form 31st March 2003(new)
ANNEX 10 – WPRO SARS Preparedness Kit contents list (and instructions on use) (updated
09.04.2003)
ANNEX 11 – WPRO example of instructions for home isolation of close contacts(new)
ANNEX 11B – WPRO example of Advice for a traveller from an affected area with NO known
contact with a SARS case (new)
HISTORY OF GUIDELINE (updated 09.04.2003)
Compiled by:
Dr Kevin Carroll
on behalf of PPHSN
Reviewed by:
Dr Tom Kiedrzynski
Epidemiologist (Ag)
Secretariat of the Pacific Community, PPHSN-CB Focal Point
The PPHSN SARS Task Force consists of:
Dr Alain Berlioz, Pharmacist-biologist, New Caledonia Pasteur Institute
Dr Mary Beers Deeble, Senior Lecturer, Director, MAE, NCEPH, ANU
Dr Kevin Carroll, MO/Epidemiologist, WHO South Pacific
Dr Rob Condon, Public Health Physician/Epidemiologist, SARS Outbreak Response Group, WPRO
Dr Tom Kiedrzynski, Notifiable Disease Specialist/Epidemiologist (Ag), SPC
Dr Kamal Kishore, Senior Lecturer, Medical Microbiology, FSMed
Dr Joe Koroivueta, Consultant Virologist, Fiji MoH
Dr Ilisapeci Kubuabola, MAE student, Fiji MOH
Dr Michael O'Leary, Regional Medical Epidemiologist, CDC/PIHOA
Dr Hitoshi Oshitani, Regional Adviser, Communicable Surveillance and Response, SARS Outbreak
Preparedness Group, WPRO
Dr Salanieta Saketa, National Epidemiologist/MO, Fiji MoH
Revision date(s)
06.04.2003
Review date
09.04.2003
PPHSN. SARS Guidelines
09/04/2003
23
ANNEX 1
CONTACTS (updated 09.04.2003)
PPHSN-CB Focal Point
Dr Tom Kiedrzynski
Epidemiologist (Ag)
Secretariat of the Pacific Community, PPHSN-CB Focal Point
SPC PO Box D5
98848 Noumea cedex
New Caledonia
Tel:
+(687) 26 20 00 or 01 43
Fax:
+(687) 26 38 18
Out of hours
+(687) 25 92 36
E-mail: tomk@spc.int
WHO South Pacific
Dr Kevin Carroll
MO/Epidemiologist
WHO South Pacific
PO Box 113
Suva, Fiji
Tel
+(679) 3304 600
Fax
+(679) 3300 462
Out of hours
+(679) 99202971
Email carrollk@sp.wpro.who.int
Emergency Hotline to WPRO
WHO WPRO Outbreak Ops Room
After Hours Duty Officer
Dr. Hitoshi Oshitani
Dr. Robert Condon
+63-2-528 9833; +63-2-528 9781
+63-2-528 9782; +63-2-528 9650
+63-920 640 9696
+63-918 921 4217
+63-919 3922023
Institute Pasteur
Alain Berlioz-Arthaud,
Laboratoire de Biologie Medicale,
Institut PASTEUR de NouvelleCaledonie,
BP 61,
98845 Noumea,
New Caledonia.
Tel : +(687) 27.02.85
Fax : +(687) 27.33.90
Email : aberlioz@pasteur.nc
WHO Collaborating Centre for Reference and Research on Influenza, Australia
Ian Barr
WHO Collaborating Centre for Reference and Research on Influenza
45 Poplar Road, Parkville.
Victoria, Australia 3052
Tel
Fax
Email
+(61) 3 9389 1761
+ (61) 3 9389 1881
Ian.Barr@csl.com.au
PPHSN. SARS Guidelines
09/04/2003
24
Clinical Virology, Communicable Disease Programme, Institute of
Environmental Science and Research (ESR)
Dr. Sue Huang; Dr. Fiona Thomson-Carter
34 Kenepuru Drive, PO Box 50-348,
Porirua,
Wellington 6004,
New Zealand
Tel: +(64)-4-914-0700
Fax: +(64)-4-914-0770
Email: Sue.Huang@esr.cri.nz; Fiona.Thomson-Carter@esr.cri.nz
PPHSN. SARS Guidelines
09/04/2003
25
ANNEX 2
PPHSN Reporting Form
Severe acute respiratory syndrome (SARS) outbreak
PPHSN Reporting Form
Severe acute respiratory syndrome (SARS) outbreak
Report of suspected or probable cases
This form is to be used for reporting suspected or probable cases of respiratory illness,
which may be associated with the outbreaks of SRAS. The cases to be reported are those
conforming to the case definitions provided by the WHO and reproduced at the bottom of
this form.
Please return this form to
PPHSN-CB Focal Point at SPC
Fax: +(687) 26 38 18
e-mail: phs.cdc@spc.int
AND/OR
WHO South Pacific
Fax: +(679) 330 04 62
e-mail: CarrollK@sp.wpro.who.int
PPHSN case definitions for hospital based surveillance
Suspected case
A person presenting to a health care facility after 1st February 2003 with a history of:
High fever (>38 o C)
And:
One or more respiratory symptoms (cough, shortness of breath, difficulty breathing)
And one or more of the following:
Close contact*, within 14 days of onset of symptoms, with a person who has been diagnosed
with SARS.
History of travel, within 14 days of onset of symptoms to an area in which there are reported
foci of transmission of SARS (see ANNEX 3B).
* Close contact means having cared for, having lived with, or having had direct contact with respiratory secretions
and body fluids of a person with SARS.
Probable Case
A suspect case with chest x-ray findings of pneumonia or Adult Respiratory Distress
Syndrome
OR
A person with an unexplained respiratory illness resulting in death, with an autopsy
examination demonstrating the pathology of Respiratory Distress Syndrome without an
identifiable cause.
Note
In addition to fever and respiratory symptoms, SARS may be associated with other symptoms including: headache,
muscular stiffness, loss of appetite, malaise, confusion, rash, and diarrhea.
Reporter details
PPHSN. SARS Guidelines
09/04/2003
1
Name of person completing this form: _ _ _ _ _ _ _ _ _ _ _ _ _
Date of report to PPHSN _ _/ _ _ /_ _ _
Name of reporter: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Position: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Institution/Organisation: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Country:____________ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Contact telephone number: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
E-mail: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Mobile phone number: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Fax no. _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Patient details
Name: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Sex:
Female
Male
Date of birth:
Surname: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
_ _/ _ _/ _ _ _ _
Country of residence
(If different from home address)
___________
Home address: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
City/town: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Postcode: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Country: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Home telephone: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
PPHSN. SARS Guidelines
09/04/2003
Mobile phone: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
2
Patient history
In the last 10 days, has the patient been in contact
with anyone who is a suspect or probable case of
SARS?
Yes
No
If yes:
Type of contact: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
(e.g. family member, friend, etc)
Name of the SARS
contact:
_____________________________________
Place of the contact: _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Has the patient traveled since 1 November 2002 in
one of the countries reported in the ANNEX 3B?
Yes
No
If yes
Country visited
Length of the stay
From
1
2
3
4
To
_____ _____ _____ ____
__/__/____
__/__/____
_____ _____ _____ ____
__/__/____
__/__/____
_____ _____ _____ ____
__/__/____
__/__/____
_____ _____ _____ ____
__/__/____
__/__/____
Date of return to (name country)
Country of departure
____________
PPHSN. SARS Guidelines
09/04/2003
__/__/____
Airport of arrival in
Country
___________
3
Clinical details
Date of onset of illness
Clinical
diagnosis
_ _/ _ _ / _ _ _ _
Pneumonia
Fever 38C
Yes
No
ARDS
Cough
Yes
No
Other: _ _ _ _ _ _ _ _ _
Myalgia
Yes
No
Fully recovered (symptom free)
Recovering
Stable
Getting worse
Not very ill
Moderately ill
Severely ill
Died
Current status:
Shortness of
breath/difficulty breathing
Yes
No
Severity of illness:
Other, please specify:
____________
Admitted to hospital?
Yes
__/__/__
No
Admission status:
Currently admitted
Date of
admission
_ _ / _ _/ _ _ _ _
Hospital
_________________
Transferred to other
hospital
Date of
admission
_ _ / _ _/ _ _ _ _
Hospital
_________________
Discharged
Date of
discharge
_ _ / _ _/ _ _ _ _
PPHSN. SARS Guidelines
09/04/2003
(Name and country)
(Name and country)
4
Tests performed and laboratory results
Chest X-ray
____________________________
Date
_ _/ _ _/ _ _ _ _
Results:
Normal
Abnormal:
____________________________
____________________________
Date
_ _/ _ _/ _ _ _ _
Results:
Normal
Abnormal:
____________________________
____________________________
Date
_ _/ _ _/ _ _ _ _
Results:
Normal
Abnormal:
____________________________
Cell blood
count
Date
_ _/ _ _ /_ _
Result
Normal
Thrombocytopenic
Leucocytopenic
Date
_ _/ _ _ /_ _
Result
Normal
Thrombocytopenic
Leucocytopenic
Date
_ _/ _ _ /_ _
Result
Normal
Thrombocytopenic
Leucocytopenic
(If performed)
PPHSN. SARS Guidelines
09/04/2003
5
ANNEX 3
Advice To Governments Regarding Travelers Arriving From SARS Affected Areas
As of 2nd April 2003 there has been a cumulative total of 2223 cases of SARS with 78 deaths. Over 80%
of these cases have been reported from China and Hong Kong. Singapore, Vietnam, Taiwan and Canada
are also affected, with local transmission.
There has been considerable debate on PACNET about the need for more stringent travel advisories – to
deter individuals from traveling to affected countries. WHO first advice was issued on 15 th March, and
stated that individuals are NOT advised not to travel to affected areas still stands. WHO has since
updated this travel advice twice. The first amended guidance of 27th March reads as follows:
“WHO recommends that passengers departing for international destinations from an affected area should
be interviewed by a health care worker in the port of departure prior to check-in. The interview should
assess whether the passenger:
(1) Currently has or has experienced in the past 48 hours any symptoms of SARS and
(2) Has had any contact with suspect or probable SARS cases
(3) Has a fever (body temperature may be checked if appropriate)
Persons meeting the SARS case definitions should be referred to a health care facility. Persons with only
fever should be instructed to postpone travel until the fever has subsided and to seek further medical
attention if symptoms of SARS develop."
However these are only recommendations and they are being implemented in a patchy and
incomplete fashion in the principal countries and areas affected.
On 2nd April, a second amendment was published by WHO. WHO recommends that persons traveling to
Hong Kong Special Administrative Region of China and Guangdong Province, China consider postponing
all but essential travel. This updated travel advice comes as a result of new developments in the multicountry outbreak of SARS.
Countries and Territories may find that because of their particular situations (especially their limited
capacity to deal with the clinical and public health implications of imported cases), it may be necessary to
advise their citizens not to travel to ALL areas with local transmission of SARS. As on 2nd April, these
areas are Guangdong, Hong Kong Special Administrative Region of China and Shanxi in China, Taiwan,
Toronto in Canada, Singapore and Hanoi in Vietnam.
It is also imperative that Governments of Pacific Island Countries prepare themselves for the importation
of cases of SARS.
In response to the exceptional situation that exists, and the vulnerability of many Pacific Island Countries
and Territories the PPHSN SARS Task Force recommends that the following action be taken for travelers
from these areas reporting active transmission of SARS:
It is recommended that all travelers arriving from, or having been in the last 14 days in, the affected areas
(particularly Hong Kong and China) should be provided with written advice regarding SARS. All
passengers with fever or respiratory symptoms should be medically assessed on their arrival. If any are
found to satisfy the suspected or probable SARS case definition, they should be taken care of as
described in the PPHSN SARS interim guidelines.
For close contacts3 of suspect and probable cases and asymptomatic travelers arriving from the worstaffected areas:
3
All close contacts of the ill passenger should be identified during the flight. For the purposes of air travel a close contact is defined
as:
passengers sitting in the same seat row or 2 rows in front or behind the sick passenger
all flight attendants on the flight
PPHSN. SARS Guidelines
09/04/2003
1. They should provide contact details for the next 14 days.
2. They should avoid public and crowded places (including all types of gatherings: functions,
celebrations, church etc).
For close contacts of suspected and probable cases, “Voluntary quarantine” at home or at
a designated facility, with minimum contact with other people including members of their own
family and relatives until 14 days has passed since the last contact with the case is
recommended IF feasible (it might be difficult to enforce or unrealistic in some places).
“Voluntary quarantine” should also be considered for travelers coming from the areas with active
local transmission4.
3. They should be provided with a mask to use should they develop a cough and while awaiting
medical assessment.
4. Their family (and relatives) must receive proper explanations/health education messages about
the risk of SARS, and what they should do as soon as they become sick (at least with fever).
5. They should be kept under surveillance. The most consistent first symptom that is likely to
appear is fever. If possible they should record their body temperature twice daily. At NO stage
should they take any drug to bring the temperature down (eg Paracetamol).
There are 2 options for their surveillance:
Passive surveillance can be used if resources to carry out active surveillance are not
available.
o If they develop a fever with or without a cough they should contact the designated
health worker/medical facility immediately (preferably by phone if possible) for advice
and assessment. They will be assessed as for a suspected case of SARS.
Active surveillance is the preferred option:
o In addition to the advice above, a designated health worker contacts them daily or
twice daily to interview them about symptoms.
6. Ideally Ministries of Health should set up dedicated SARS telephone “hotlines”. All
individuals under passive or active surveillance should be able to ring for advice 24 hrs a
day.
This advice has been prepared by the PPHSN SARS Taskforce:
The members of the Task force are:
Dr Alain Berlioz, Pharmacist-biologist, New Caledonia Pasteur Institute
Dr Mary Beers Deeble, Senior Lecturer, Director, MAE, NCEPH, ANU
Dr Kevin Carroll, MO/Epidemiologist, WHO South Pacific
Dr Rob Condon, Public Health Physician/Epidemiologist, SARS Outbreak Response Group, WPRO
Dr Tom Kiedrzynski, Notifiable Disease Specialist/Epidemiologist (Ag), SPC
Dr Kamal Kishore, Senior Lecturer, Medical Microbiology, FSMed
Dr Joe Koroivueta, Consultant Virologist, Fiji MoH
Dr Ilisapeci Kubuabola, MAE student, Fiji MOH
Dr Michael O'Leary, Regional Medical Epidemiologist, CDC/PIHOA
Dr Hitoshi Oshitani, Regional Adviser, Communicable Surveillance and Response, SARS Outbreak
Preparedness Group, WPRO
Dr Salanieta Saketa, National Epidemiologist/MO, Fiji MoH
anyone having intimate contact, providing care or otherwise having contact with respiratory secretions of the sick
passenger
any one on the flight living in the same household as the ill passenger
If it is a flight attendant who is considered to be a suspect or probable SARS case all the passengers are considered to be contacts.
4
See above
PPHSN. SARS Guidelines
09/04/2003
ANNEX 3B
Affected Areas* - Severe Acute Respiratory Syndrome (SARS)
Last revised by WHO – 09 April 2003
Country
Area
Canada
Toronto
Singapore
Singapore
China
China
Guangdong Province, Hong Kong Special
Administrative Region of China, Shanxi
province
Taiwan
Viet Nam
Hanoi
*An "Affected Area" is defined as a region at the first administrative level where the country is
reporting local transmission of SARS.
PPHSN. SARS Guidelines
09/04/2003
ANNEX 4
SARS Patient Management Flow Chart (Example)
Patient arrival at hospital
Contacts
Give information on SARS to the
contact
Contact of Suspect case
Patient Triaged on arrival
Using SARS case definitions
No
Reassurance
Advice
Usual care
•Place under passive surveillance for 14
days.
•Contact is free to continue with usual
activities; however:
Contact to self-report to public health
authority if contact develop any
symptoms
The most consistent first symptom that
is likely to appear is fever
Potential
Case of
SARS
Contact of Probable case
•Place under active surveillance for 14
days.
•Home isolation:
If contact develops any symptoms,
contact to be assessed at health
care facility
The most consistent first symptom that
is likely to appear is fever.
Yes
Place mask on Patient
and transfer to isolation area
HCWs should wear mask or N95 respirator mask
PRIOR to entering room to examine patient
SUSPECTED case
Of SARS
(WHO definition)
No
Yes
Yes
CXR and FBC, other specimen collection
Reassurance
Advice
Usual care
No
PROBABLE case of SARS (WHO definition)
Yes
Inform Public health
authorities
PPHSN. SARS Guidelines
09/04/2003
Admit to designated
isolation facility.
Treat as indicated
Contact tracing
Advice to contacts
Health Education
Public health
authorities
informed
ANNEX 5
Advice To Arriving Travelers (examples)
During your recent travel if you have traveled through the affected areas listed below
during the past 10 days, you may have been exposed to cases of severe acute respiratory
syndrome. The usual incubation period for this illness is 2-7 days. You should monitor
your health. If you become ill with fever accompanied by cough or difficulty in breathing,
and you have been in one of the affected areas during the past 10 days you should seek
medical advice (please see list below). To help the doctor make a diagnosis, tell him or
her about your recent travel to these regions and whether you were in contact with
someone who had these symptoms. Please save this card and give it to your physician if
you become ill.
Affected Areas* - Severe Acute Respiratory Syndrome (SARS)
Country
Area
Canada
Toronto
Singapore
Singapore
China
Guangdong Province, Hong Kong Special
Administrative Region of China, Taiwan
Province
Viet Nam
Hanoi
Last revised 24 March 2003
*An "Affected Area" is defined as a region at the first administrative level where the country is reporting
local transmission of SARS.
List of Medical Practioners/Facilities where Assistance Can Be Obtained
Name
PPHSN. SARS Guidelines
09/04/2003
Address
Telephone
Fax
SOLOMON ISLANDS - MINISTRY OF
HEALTH AND MEDICAL SERVICES
ADVISORY ON
SEVERE ACUTE RESPIRATORY
SYNDROME (SARS)
The Centre for Disease Control and
Prevention (CDC) and the World Health
Organization (WHO) have received reports
of patients with severe acute respiratory
syndrome (SARS) from Canada, China,
Hong Kong Special Administrative Region
of China, Indonesia, Philippines, Singapore,
Thailand, Vietnam, Germany and the United
Kingdom. The cause of these illnesses is
unknown and is being investigated. Early
manifestations in these patients have
included influenza-like symptoms such as
fever, muscle pains, headache, sore throat,
dry cough, shortness of breath, or difficulty
breathing.
Based on currently available evidence, close
contact with an infected person is needed for
the infective agent to spread from one person
to another.
This illness can be severe and, due to global
travel, has spread to several countries in a
relatively short period of time. Therefore,
there is cause for concern.
PPHSN. SARS Guidelines
09/04/2003
WHO has not recommended restricting
travel to any destination in the world.
However, all travelers should be aware of the
main symptoms and signs of SARS. People
who have these symptoms and within the
previous 10 days have been in close contact
with a person who has been diagnosed with
SARS, or a history of travel to areas where
cases of SARS have been spreading (see
list), should seek medical attention and
inform health authorities of recent travel.
Travelers who develop these symptoms are
advised not to undertake further travel until
fully recovered.
Please note that this situation is rapidly
evolving and that the advice given will be
constantly changing as more evidence about
the causation and options for treatment
becomes available.
The public is advised to consult the home
page of the WHO SARS website:
http://www.who.int/csr/sars/en/ for daily
updates on the outbreak and relevant press
releases.
This advisory is given by the Ministry of Health
in collaboration with Immigration, Quarantine
and Travel Agencies in Solomon Islands, aimed
at preventing introduction of SARS into the
country and ensuring the health and well being of
the local population and visiting friends.
To ensure that appropriate health measures are
provided in case of an emergency, please respond to
the following questions:
Have you been to the following places / countries
within the last 10 days?
Guangdong Prov., China
Hongkong, SAR, China
Singapore
Hanoi, Vietnam
ROC / Taiwan
Toronto, Canada
Yes / No
Yes / No
Yes / No
Yes / No
Yes / No
Yes / No
If “Yes” are you experiencing the following
symptoms?
High Fevers
Coughs
Breathing Difficulties
Yes / No
Yes / No
Yes / No
If “Yes” to any of the above locations AND “Yes” to
any of the above symptoms, please report to the
Quarantine Desk at the arrival lounge.
If you state “Yes” to any of the above locations and
“No” to all of the above symptoms, you are advised to
report to the nearest hospital or see your doctor in the
event that you start to have these symptoms within the
next 7 days and present this advisory.
Full Name……………………………….…………….
Passport No.…………………………………………..
Nationality:……………………………………………
Address in Solomon Islands:
………………………………………………………
………………………………………………………
ANNEX 6
Health Advice on the
Prevention of Respiratory Tract Infections
(Hong Kong MOH)
Background
In view of a recent outbreak of febrile respiratory illness among health care staff in
Prince of Wales Hospital, the Department of Health is conducting a detailed
investigation with the Hospital Authority and the Hong Kong University and Chinese
University of Hong Kong to identify the cause of infection. The situation will be
monitored closely.
The Department of Health has informed the World Health Organization (WHO) about
the latest developments. Hong Kong is working closely with the WHO on disease control
and prevention.
Advice applicable to all
As a precautionary measure, members of the public are advised to take precautionary
measures to prevent respiratory tract infections:
o
Build up good body immunity. This means taking a proper diet, having regular
exercise and adequate rest, reducing stress and avoiding smoking
o
Maintain good personal hygiene, and wash hands after sneezing, coughing or
cleaning the nose
o
Maintain good ventilation
o
Avoid visiting crowded places with poor ventilation
o
Consult their doctor promptly if they develop respiratory symptoms
For schools and pre-school institutions
Child Care Centres / Kindergartens / Schools are advised to refer to the 'Guidelines on
Prevention of Communicable Diseases in Child Care Centres / Kindergartens / Schools'
published by the Department of Health in 2000 for general information on the
prevention of communicable diseases in school and institutional settings. This is
downloadable from the DH's website http://www.info.gov.hk/dh. Specific advice in the
school and institutional setting that helps to prevent respiratory tract infections
includes :
o
Cleanse used toys and furniture properly
o
Keep hands clean and wash hands properly
o
Cover nose and mouth when sneezing or coughing
o
Wash hands when they are dirtied by respiratory secretions e.g. after sneezing
o
Use liquid soap for hand washing and disposable towel for drying hands
o
Do not share towels
For other institutional settings
A 'Guidelines on Prevention of Communicable Diseases in Residential Care Homes for
the Elderly and People with Disabilities' published by the Department of Health is also
available for general information on the prevention of communicable diseases in the
PPHSN. SARS Guidelines
09/04/2003
particular institutional setting. This is downloadable from the DH's website
http://www.info.gov.hk/dh.
For health care workers in clinic setting
There is as at date no unusual upsurge of pneumonia cases in the community.
All clinic staff should enforce strict infection control measures appropriate for their
particular setting, especially observance of good personal hygiene.
If staff fall sick, they should report to their seniors and take sick leave as appropriate.
Where considered necessary, for example, treating or nursing a patient with respiratory
symptoms, staff may wear masks.
The Department of Health will continue to monitor the situation of the pneumonia cases
and issue advice accordingly.
Patients with respiratory symptoms are advised to wear mask to reduce the chance of
spread of the infection.
Caring for sick family members with respiratory illness
Patients should consult a doctor if they are unwell.
They should follow instructions given by the doctor including the use of drugs as
prescribed and taking adequate rest as appropriate.
Adhere to good personal hygiene practices.
Ensure adequate ventilation.
Patients should put on masks to reduce the chance of spread of infection to carers.
Carers may also put on masks to reduce the chance of acquiring infection through the
airways.
Advice to relatives visiting patients with pneumonia
Visitors to warded patients are advised to take due precautions in infection control, e.g.
wearing face mask and gowns and to wash hands thoroughly afterwards before coming
into contact with other people.
Notification of infections
If unusual patterns of illnesses/sick leave in any setting are detected, please notify
the respective Regional Office of the Department of Health. The contact numbers are
as follows :
PPHSN. SARS Guidelines
09/04/2003
ANNEX 7
Health Advice on the Prevention of
Respiratory Tract Infections in Public Places
(Hong Kong MOH)
Members of the public are advised to avoid frequenting crowded public places to
prevent the spread of respiratory tract infections. When visiting crowded places such as
cinemas and restaurants, the following precautionary measures should be taken :
Maintain good personal hygiene. Cover nose and mouth when sneezing or coughing
Dispose of used tissue paper properly
Keep hands clean. Wash hands when they are dirtied by respiratory secretions e.g.
after sneezing
Do not share towels
Consult your doctor promptly if you develop respiratory symptoms, and follow
instructions given by your doctor including the use of drugs as prescribed and
adequate rest as appropriate
Patients should put on masks to reduce the chance of spread of infection
Workers in public places should take the following precautionary measures to
reduce the chance of spread of infection :
Maintain good personal hygiene. Cover nose and mouth when sneezing or coughing
Wash hands after sneezing, coughing or cleaning the nose
Consult your doctor promptly if you develop respiratory symptoms
Allow plenty of fresh air into the indoor environment
If the facilities are mechanically ventilated, ensure frequent air exchanges and
proper maintenance and cleansing of the system
Ensure that toilet flushing apparatus is functioning properly
Provide toilets with liquid soap and disposable tissue towels or hand dryers
Cleanse and disinfect the facilities (including furniture and toilet facilities) regularly
(at least once a day), using diluted household bleach (i.e. adding 1 part of household
bleach to 99 parts of water), rinse with water and then mop dry
If the facilities are contaminated with vomitus, wash / wipe with diluted domestic
bleach (mixing 1 part of bleach with 49 parts of water) immediately
PPHSN. SARS Guidelines
09/04/2003
Infection Control ~ Doing it Right, Each Time
Prepared by the Infection Control team, C&C DHB, 04 April 2003.
ANNEX 8
New Zealand MOH
Infection Control advice for the management of patients with
suspected Severe Acute Respiratory Syndrome (SARS)* (updated 4th
April)
For detailed case definitions (of “suspect” and “probable” SARS patients) and clinical management
recommendations please consult the bulletin sent electronically to all C&C DHB staff on 18 March.
Immediately notify the Clinical Microbiologist/Infectious Diseases physician on call of any new
suspected cases.
SARS – should be suspected in patients presenting with symptoms of atypical pneumonia and a
history within the last 10 days of recent travel or stay in South-East Asia or recent close contact
with unwell travellers to that region or other areas of reported transmission of SARS.
At this stage the causative organism is believed to be a coronavirus. Specific screening/diagnostic tests
are being developed and will soon be available locally; specific treatments are under investigation but at
present treatment is supportive – the emphasis must therefore be on minimizing contact by good infection
control procedures as detailed below.
Peak infectivity occurs as patients develop obvious respiratory symptoms including cough. It is
especially important at this stage for staff to use eye protection in addition to other personal
protective clothing/equipment detailed below and to avoid any aerosol-generating procedures (eg use
of nebulisers) with suspected or probable SARS patients.
To minimise exposure of other patients, staff and hospital visitors, the World Health Organisation
and the US Centers for Disease Control & Prevention advise:
1. That all suspected SARS patients are managed in isolation using:
Standard (blood/body fluid) Precautions especially use of barrier protection when dealing
with any blood or body fluids; use of masks (see airborne precautions below) plus eye
protection (such as goggles or visor or use of a mask with attached eyeguard) when in close
proximity to patients who are coughing (ie. all cases who meet the ”probable” SARS case
definition) and for all “suspect” SARS patients when procedures are done which are likely to
generate splashes or sprays of respiratory secretions (eg. taking respiratory samples or
suctioning) and scrupulous handwashing after removing gloves (see contact precautions below)
plus
• Airborne Precautions placement of the patient in a negative pressure air-conditioned room and use of
respiratory protection – particulate filter respirator masks (TB masks - Tecnol PCM 2000 mask) - by all
staff and visitors,
plus
• Contact Precautions use of non-sterile gloves and disposable, impervious isolation gown by all staff
and visitors for any contact with the patient, the patient’s body fluids, with patient care equipment or with
used linen or with waste
2. Patient masking for transport (ambulance or internal trolley transport) and short visits to other
clinical departments (eg. Radiology)
• Patient movement outside negative pressure rooms should be avoided as much as possible.
• A standard surgical mask (eg. Tecnol Procedure mask 6001 or any other droplet containing mask)
must be placed over the patient’s mouth and nose for transport through corridors and public areas
PPHSN. SARS Guidelines
09/04/2003
(eg. between clinical areas such as Emergency Department and Radiology / wards /units) or for
investigation in departments such as Radiology.
• Attending staff do not then require masks but should continue use of gloves and gown for direct
contact with the patient, with blood or body fluids or with patient equipment.
• Receiving departments should be advised of the patient’s isolation status when transfer or investigations
are ordered and patients must be escorted during transport between negative pressure areas to ensure
that appropriate precautions are maintained.
• See Equipment and Cleaning details below for advice on necessary equipment and
environmental surface cleaning and decontamination following procedures on suspected SARS patients.
3. Emergency Dept. and Ward management details
Isolation room details
• The patient must be isolated in a negative pressure single room – eg. rooms A3 or C7 in the Emergency
Dept. or a room (preferably with attached ensuite bathroom) within the airborne isolation area in Ward 17.
• The isolation room door must be kept closed at all times except when required by entry or exit of
personnel.
• A laminated “STOP” isolation sign (as distributed by the Infection Control Officers) must be placed on
the door or where it will be visible to all who enter the room
• The patient should leave the room only when clinically necessary (see point 2. above).
• Microshield 4 antiseptic handwash should be used for all handwashing within the room and at
adjacent washbasins outside the room (eg. in the anteroom) immediately following removal of protective
clothing on exiting the isolation room.
Handwashing is the most important hygiene measure for preventing the spread of infection.
Gloves are not a substitute for handwashing. Hands must be washed and gloves replaced before and
after significant contact with the patient, after activities involving handling of contaminated items and after
removal of gloves.
• All staff and visitors must put on mask, gowns and gloves as specified before entering the isolation
room.
• On leaving the isolation room, staff and visitors should remove gown, gloves and mask (in that order,
masks should be handled only strings); place them into a yellow Biohazard waste bin and immediately
wash their hands. (In Ward 17 this is done in the ante-room to the isolation rooms; in the Emergency
Dept. this must be done immediately outside the isolation room and then the nearest washbasin must be
used for handwashing.). These are single use items - fresh gowns, gloves and masks must be put on for
any subsequent entry into the isolation room.
• Provide patients with ample supplies of disposable tissues and teach them to cover their mouth and
nose when coughing or sneezing. Tissues must be handled and disposed of as Biohazard waste.
• Patient notes, including medicine and observation charts (and clinical staff’s pens) must not be kept or
taken into the room.
• Patient samples/specimens should be handled in the usual manner (placed in a Biohazard specimen
bag for transport to the laboratory accompanied by a completed request form)
Staff allocation
• The primary focus must be appropriate, skilled response to the clinical needs of the patient
• The nurse allocated to direct patient care on each shift is responsible for directing other health care
workers and visitors on the nature of the precautions required
• The number of staff allocated to the patient should be as small as possible to decrease the possibility of
transmission to other patients within the ward or to other areas of the hospital.
eg. Blood tests are to be taken by the Medical Officer ordering the test rather than being put out for
Phlebotomy service staff
• Whenever possible, care is provided by nurses/staff usually working in the ward
• If care cannot be provided from within the ward, the Coordinator Central Nursing, her deputy or the after
hours manager is contacted for assistance by the nurse in charge and consultation must include the
Clinical Microbiologist/Infectious Diseases physician on call
• A nurse employed by the Casual Resource may look after the patient only if s/he has the skills and
knowledge necessary to care safely and confidently for the patient, and the Central Nursing Coordinator
and the nurse agree to the assignment.
PPHSN. SARS Guidelines
09/04/2003
Equipment and supplies
• Disposable equipment should be used wherever possible in the treatment of patients with suspected
SARS.
• A range of sizes of non-sterile gloves must be available inside and at the entrance to the isolation room.
Gloves must be changed as clinically indicated and removed and disposed of in the Biohazard waste
each time personnel leave the isolation room.
• Disposable, impermeable isolation gowns are recommended (eg. Baxter yellow disposable isolation
gowns). Gowns are single use items and may not be kept for reuse – they must be removed and
disposed of in the Biohazard waste when personnel leave the isolation room and a new gown must be
worn for re-entry.
• Masks:
Particulate filter respirator (Tb) masks must be available (eg. Tecnol PCM 2000 mask), preferably
the fluid repellent orange version (PCM 2000 reorder number 47707 – available from Supply
Dept.) and in the fluid repellent orange version with attached eyeguard (PCM 2000 reorder
number 47757 – available as a buy-in, 15/box).
Standard surgical masks (eg. Tecnol Procedure mask 6001 – available from Supply Dept.) must
be available for use by the patient to prevent dispersal of respiratory droplets if the patient must
leave the isolation room.
Masks are single use items and must be removed and disposed of in the Biohazard waste each
time staff and visitors leave the isolation room and a new mask must be worn for re-entry.
• Equipment and supplies necessary for patient treatment, safety and comfort must be available in the
isolation room but storage of supplies and equipment within the room must be kept to a minimum and be
replenished daily if necessary.
• All non-disposable equipment (eg. blood pressure cuffs, stethoscopes, tympanic membrane
thermometers and including mobile units such as X-ray machines, IV pumps etc.) that is taken into the
room must be decontaminated immediately after removal from the isolation room and before it may be
reused in the care of other patients. At a minimum, items will require cleaning by surface wiping with a
disposable cloth, detergent and water (or specialist products if these are normally used) and usual
disinfection and sterilisation processes should be used for items normally reprocessed by these methods.
• It is recommended that some dedicated items of non-disposable equipment (eg. blood pressure cuffs)
are left in the room for the duration of the patient’s isolation so that discharge/terminal cleaning only is
likely to be required.
• Bedpans and urinals should be emptied and reprocessed (immediately after use ie. Should not be left
unprocessed on communal dirty benches in utility rooms) by the usual method in ward sanitisers. The
isolation nurse may need assistance from other nursing staff outside the isolation room to facilitate this
(these staff should use gloves, disposable aprons and facial protection when handling used toilet items
and plan the transfer of items so that minimal contamination of environmental surfaces occurs).
• Metal surgical instruments requiring sterilisation in the Sterile Production Centre can be placed in a clear
plastic bag, the opening secured and then returned in the usual container to SPC for routine
decontamination (full body and facial protective equipment is worn routinely in the SPC decontamination
area).
• A designated sharps container must be available in the room plus phlebotomy equipment if required
(tourniquet, vacutainer collection system, A.N.D. disposal unit for vacutainer needles, etc).
• The wash bowl is kept in the room for the duration of the isolation. It is cleaned with hot soapy water
after use, dried, then stored, inverted, off the floor. Bowls used to clean patients after incontinence
episodes are to be emptied in the sluice room, rinsed and wiped over with 1% Chlorine solution then
sanitised in the usual manner.
Food service
• Usual meal trays, plates and cutlery may be used. Menus and trays do not need special marking or
bagging as isolation items.
• After use, waste food should be disposed of within the isolation room and the trays and utensils should
be returned directly (with assistance from staff working outside the isolation area) to the Food Services
trolley for return to the kitchen for reprocessing. Staff in this area routinely wear protective clothing and
the usual machine dishwashing process is adequate to decontaminate the trays and utensils.
PPHSN. SARS Guidelines
09/04/2003
Linen and waste handling
• A linen skip (with a cloth linen bag lined with a hot water soluble alginate liner) and a Biohazard yellow
waste bag must be present in the isolation room.
• All waste (except sharps which must go into the sharps container) produced in the room must go into
the Biohazard waste bag.
• Care should be taken not to shake or flap the bedlinen. Change the bedlinen completely each morning
shift and carefully scoop and fold used linen to place it in the used linen container.
• Linen and waste bags are to be replaced at least daily and when two thirds full.
• Nursing staff are responsible for the closure and replacement of bags. Double bagging and labelling are
not required.
Visitors
• Visitors other than close family members should be discouraged as the causative organism and
infectivity of SARS is not yet clear and specific treatments have not yet been identified.
• Request visitors not to visit other patients in hospital if they are visiting patients with suspected SARS.
• All visitors must wear full protective clothing (gown, gloves and mask) to enter the isolation room. (See
procedures detailed for staff).
• Nursing staff are responsible for ensuring that visitors comply with isolation procedures and should
explain and assist as necessary.
Daily cleaning
• The isolation room must be cleaned daily.
• Under the direction of the Team Leader, Clinical Coordinator or deputy, the cleaner must be directed
and shown how to use full protective clothing (gown, gloves and mask).
• The room (and ensuite) must be cleaned last of all the rooms on the ward. Disposable cleaning cloths
must be used.
• The cleaner must dust to a height of 6 feet the door, bed frame, bed light, window sills and furniture,
shelves and ledges, trolleys and equipment. Dust must not be shaken out of cleaning cloths but must be
contained by folding inwards.
• Locker tops, washbasins, taps and door handles must be cleaned with clean cloths, fresh hot water and
detergent.
• The floor must be wet mopped with clean hot water and detergent.
• Isolation bathroom areas must be cleaned following the isolation room, using the same precautions.
• Dispose of all cleaning cloths in the Biohazard bag in the isolation room. The mop head must be placed
in an alginate liner bag before being sent to the Laundry for routine laundering – special labelling is not
required.
• The bucket is to be washed thoroughly with hot water and detergent and turned upside down to dry.
• The cleaner must be shown how and where to take off protective clothing in a safe manner, dispose of it
into a Biohazard container and instructed to wash their hands immediately.
Terminal cleaning (on patient discharge)
• Infection Control advice must be sought for the decontamination complex equipment.
• Nursing staff are responsible for supervising the safe stripping and cleaning of the isolation room and
bathroom including instructing and supervising the cleaner in putting on protective clothing.
• Strip the bed of linen. Check for breaks in the impervious covering of the pillow and mattress.
Only when breaks are detected - dispose of these items as Biohazard waste (pillows can be placed in a
Biohazard waste bag; if mattresses are to be disposed of they must be contained within clean large
plastic bags, clearly labelled as intended for Biohazard waste and Orderlies should be contacted to collect
and place them directly into a large yellow Biohazard waste bin for transport to the Infectious Waste
room.)
• Dispose of disposable equipment (used or unused stock) and other waste into the Biohazard waste bag.
• Leave the waste and linen bags to be tied off by the cleaner once cleaning is completed so that cleaning
cloths and protective clothing can be discarded safely.
• The cleaner must clean all the surfaces including isolation bathrooms and floors as listed in the daily
cleaning requirements with clean disposable cloths, clean hot water and detergent.
• All cleaning cloths must be disposed of into the Biohazard waste bag. Mop heads must go to the
Laundry as detailed above in Daily cleaning and the bucket must be cleaned as above.
• Curtains:
PPHSN. SARS Guidelines
09/04/2003
In the Emergency Department, ask the cleaner to check the curtains for soiling; if present, ask for
the curtains to be changed.
In the ward or unit setting, ask the cleaner to change the curtains. (New curtains must not be put
up until the room has been fully cleaned and aired for 1 hour following completion of cleaning).
• The cleaner must be shown how and where to take off protective clothing in a safe manner, dispose of it
into a Biohazard container and instructed to wash their hands immediately.
• The rooms should be left with the door closed for 1 hour before the bed is remade, curtains are rehung
and the room is re-occupied. This is to allow for sufficient air changes to occur to ensure removal all
possibly contaminated air.
This information is subject to change and updating as further information and direction comes to
hand from WHO, CDC and the NZ Ministry of Health.
For further infection control advice
• Please contact an Infection Control Officer (Clo Taylor on ext/page 5925 or Viv McEnnis on ext/page
6514).
References
1. Garner JS, Hospital Infection Control Practices Advisory Committee “Guidelines for Isolation
Precautions in Hospitals” Infection Control & Hospital Epidemiology 1996; 17: 53-80.
2. US Centers for Disease Control and Prevention information – Severe Acute Respiratory Syndrome
“Interim Information and Recommendations for Health Care Providers” 15 March 2003.
3. NZ Ministry of Health – information distributed electronically on 18 March 2003 and sourced from WHO
and CDC.
PPHSN. SARS Guidelines
09/04/2003
ANNEX 9
PPHSN country checklist and assessment form 31st March 2003
The EpiNet national/territorial focal points should liase with their health authorities to complete the following information
about preparedness to deal with cases of SARS.
Overview
This one page checklist is meant as a guide for countries in the Pacific Island Region to assist with their response and
preparedness planning for SARS. Please tick whatever was achieved. Details in this document may change as more clinical,
epidemiological, and laboratory information about SARS becomes available. Please tick whatever was
Preparation of a strategic country plan (adapting PPHSN updated SARS guidelines)
1.
With the EpiNet national/territorial team, task force established to oversee the development of a
comprehensive local SARS response strategy (could be the EpiNet team itself).
2.
Comprehensive local strategy developed (using available resources from PPHSN and WHO) to manage the
response to SARS and prevent its further spread when cases appear.
3.
Contact maintained with relevant hospitals, clinical services, doctors, nurses, other healthcare workers, and
laboratories, and all of them kept informed of the local SARS preparedness and response strategy.
4.
Contact maintained —through WHO country representative if applicable—with the PPHSN Coordinating Body
Focal Point (SPC) or WHO Suva Office, kept informed of development/adaptation and implementation of strategic
country plan.
If difficulties encountered to achieve the preparation of a strategic country plan, please explain:
Supplies – stockpiling of barrier nursing supplies
1.
Awareness of the local or regional storage sites of the initial WHO stockpile of barrier nursing supplies, and contact
identified when/if these are needed.
2.
Budget resources and/or donor support identified for the acquisition of a local stockpile of barrier nursing material.
3.
Local inventory of barrier nursing supplies in the event of SARS cases being identified, performed.
4.
Consider requirements beyond the time covered using the initial WHO stockpile kit – estimated to be 3 to 4 days.
Required volume of equipment ordered from suppliers of barrier nursing material in the event of local SARS cases.
If difficulties encountered to achieve the stockpiling of barrier nursing supplies, please explain:
PPHSN. SARS Guidelines
09/04/2003
Enhanced Surveillance
1.
Current surveillance case definitions and guidelines for reporting suspect or probable SARS cases distributed to
clinical facilities likely to see potential SARS patients. Updated SARS case definitions are available from the WHO
website—see http://www.who.int/csr/sars/en/) or from the PPHSN SARS guidelines on PPHSN SARS webpage—
see http://www.spc.int/phs/PPHSN/Outbreak/SARS_Outbreak.htm
2.
Sensitivity of local surveillance for the detection of new SARS cases maximised – for example, by establishing
active surveillance for SARS cases via a local networking (eg teleconference by HF radio) with major hospitals and
peripheral health car facilities.
3.
In regions or countries without previous SARS cases, suspect or probable SARS cases should be notified
immediately to the WHO country offices, the PPHSN Coordinating Body Focal point (SPC) or WHO Suva Office,
who can assist with planning the local response. This should preferably be done using PacNet or PacNet-restricted.
4.
System for monitoring and investigating rumours and anecdotal reports of local SARS cases established. Details
provided to the WHO country office, the PPHSN Coordinating Body Focal point (SPC) or WHO Suva Office.
5.
Sensitive suspect case definition should be used by countries at low risk, but with health infrastructure inadequate
to respond to a potential local SARS transmission, and planned control measures immediately implemented upon
identification of a suspect case, in consultation with the WHO country office, the PPHSN Coordinating Body Focal
point (SPC) or WHO Suva Office if needed . The WHO WPRO SARS response team should be notified
immediately, preferably through PacNet and PacNet-restricted.
If difficulties encountered to implement enhanced surveillance, please explain:
Procedures for passengers arriving from affected areas and community control measures (for
updated affected areas see http://www.who.int/csr/sarsareas/en/)
1.
All passengers having been in the previous 10 days in the affected areas informed about SARS symptoms and
where to present for further evaluation if they develop these.
2.
Local surveillance procedures augmented by developing a process for the identification of symptomatic arrivals
from affected regions. Local planned infection control procedures should then be implemented, which may include
isolation for up to ten days.
3.
Procedures to identify contacts of probable SARS cases developed and locally developed adequate control
measures implemented. Daily clinical review for fever and/or respiratory symptoms in these contacts undertaken.
If difficulties encountered to implement procedures for passengers arriving from affected areas and community control measures,
please explain:
PPHSN. SARS Guidelines
09/04/2003
Hospital Infection Control
1.
A local facility identified and prepared to accept suspected or probable SARS cases. If multiple facilities can be
identified in a region, where practical these should be as few as possible and geographically dispersed (i.e. not all
located in the capital city).
2.
Planned local infection control strategy implemented, including isolation and barrier nursing, upon the identification
of suspect or probable cases of SARS.
3.
Local management of suspected SARS cases implemented if possible. Transfer over long distances should be
avoided due to the difficulty in maintaining respiratory isolation and barrier nursing techniques.
4.
Preparedness exercise for 1 - an arriving airline passenger with suspected SARS, and 2 – someone presenting at
a peripheral health facility (ie at least different from the hospital supposed to deal with SARS) with suspected SARS,
carried out under proper supervision.
If difficulties encountered to implement Hospital Infection Control procedures, please explain:
Laboratory Specimens
1.
2.
3.
Your regional SARS reference laboratory identified.
Collection and transport of clinical specimens from suspect or probable SARS cases coordinated with your regional
SARS reference laboratory, and the local WHO country office, the PPHSN Coordinating Body Focal point (SPC) or
WHO Suva Office kept informed (they are the ones who could assist if you experience difficulties in shipping eg
needed supplies or import permits/clearance).
Collection of specimens should allow for the exclusion of common/usual respiratory pathogens.
If difficulties encountered to implement laboratory specimen shipment procedures, please explain:
Additional information
Please complete the following table as well:
Action.
Details.
WHO Country
Point of first contact for national
Focal Point
and WPRO SARS
National Focal
Point
MOH/DOH designated SARS
focal point / coordinator
(preferably the EpiNet team
Focal Point or a member of the
team)
Designated
SARS Isolation
Facility (s)
Hospital with isolation
(preferably intensive care)
facilities designated by MOH
/DOH for SARS admissions
PPHSN. SARS Guidelines
09/04/2003
Status / contact details (tel/fax –office and after hours), email
WR or CLO in countries where present, otherwise the PPHSN
Coordinating Body Focal point (SPC) or WHO Suva Office.
Designated
SARS
laboratories
Laboratories with appropriate
infection control capability
designated by MOH /DOH for
SARS specimen processing
and/or trans-shipment. The labs
listed in the next column are
those who explicitly agreed to
do the above. The form needs
yet to include at least one
additional lab for the Northern
part of the Pacific Island region.
Institute Pasteur
Alain Berlioz-Arthaud
Laboratoire de Biologie Medicale,
Institut PASTEUR de Nouvelle Caledonie,
BP 61, 98845 Noumea, New Caledonia.
Tel: +(687) 27.02.85
Fax : +(687) 27.33.90
Email : aberlioz@pasteur.nc
WHO Collaborating Centre for Reference and Research on Influenza
Ian Barr
WHO Collaborating Centre for Reference and Research on Influenza
45 Poplar Road, Parkville, Victoria, Australia 3052
Tel: +(61) 3 9389 1761
Fax: +(61) 3 9389 1881
Email:
Ian.Barr@csl.com.au
Clinical Virology, Communicable Disease Programme, Institute of
Environmental Science and Research (ESR)
Dr. Sue Huang; Dr. Fiona Thomson-Carter
34 Kenepuru Drive, PO Box 50-348, Porirua,
Wellington 6004, New Zealand
Tel: +(64)-4-914-0700
Fax: +(64)-4-914-0770
Email: Sue.Huang@esr.cri.nz; Fiona.Thomson-Carter@esr.cri.nz
Immediately
identifiable
requirements
from PPHSN (if
any).
Anything you think you urgently
need.
PPHSN. SARS Guidelines
09/04/2003
The following information has been prepared to assist WHO WRs and CLOs when liasing with
national health authorities regarding public health response to the current outbreak of Severe Acute
Respiratory Syndrome (SARS). The PPHSN SARS Task Force thinks that this information should
also be obtained from countries without WHO offices so that arrangements can be made to enhance
our preparedness. The PPHSN SARS Task Force has already circulated interim guidelines about
SARS, which will be updated continuously and circulated, as knowledge about this disease
increases.
WPRO has provisionally categorized member countries based on 3 levels of risk and 3 levels of
capability to respond to the outbreak.
Risk Categories
R1
countries where cases have been reported
R2
where traffic risks exist between these and R1 countries
R3
all other WPR countries
Capability to Respond Categories
C1 countries needing the most assistance from WHO in terms of emergency supplies,
enhanced surveillance and technical assistance
C2 countries with limited national resources and requiring some emergency assistance
C3 countries not requiring much assistance except for technical advice and international
network coordination
Category
C1
R1
Vietnam
C2
China
R2
Cambodia
Lao PDR
Northern Mariana Islands
Samoa *
Tonga *
R3
Mongolia
American Samoa
Cook Islands
Federated States of
Micronesia
Kiribati
Marshall Islands
Nauru
Niue
Palau
Papua New Guinea
Pitcairn
Solomon Islands
Tokelau
Tuvalu
Vanuatu
Wallis and Futuna
French Polynesia
New Caledonia
Malaysia
Philippines
Macao SAR
Republic of Korea
Brunei Darussalaam
Fiji *
Guam
C3
Singapore
Australia
Japan
New Zealand
* These countries are now R2 given the Rugby Teams that will be/are coming back from the worst-affected
areas in East Asia.
This assessment is current as of 31 March 2003. Revisions may be necessary as the SARS epidemic
evolves, and will be included as necessary in subsequent updates.
Do the NHA agree with this first assessment?
YES / NO
If NO, please specify why: ……………………………………………………………………………………………
………………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………………
……………………………………………………………………………………………………………………………..
PPHSN. SARS Guidelines
09/04/2003
A kit of supplies developed to address initial requirements for management of an outbreak of SARS in select
countries has been dispatched to the WR offices in Laos, Mongolia, Cambodia, Papua New Guinea, Fiji (2
kits), Samoa, the WHO CLO offices in Kiribati, Solomon Islands, Tonga and Vanuatu, and for the Northern
Pacific Guam PHL. A list of contents is in the 2nd attachment.
Daily Updates
Please advise whether
you receive the daily (or so) updates through PacNet:
YES / NO
you can access the WHO daily epidemiologic update
via the internet (http://www.who.int/csr/sars/):
YES / NO
you would like to receive daily updated in a different way or format YES / NO
If YES please specify:
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
After completion of the form
Please keep a copy with the SARS or EpiNet Focal Point and return the completed form by email or fax to:
PPHSN-CB Focal Point
Dr Tom Kiedrzynski
Epidemiologist (Ag)
Secretariat of the Pacific Community, PPHSN-CB Focal Point
SPC PO Box D5
98848 Noumea cedex
New Caledonia
Tel:
+(687) 26 20 00 or 01 43
Fax:
+(687) 26 38 18
Out of hours
+(687) 259236
E-mail: tomk@spc.int
OR
WHO South Pacific
Dr Kevin Carroll
MO/Epidemiologist
WHO South Pacific
PO Box 113
Suva, Fiji
Tel
+(679) 3304 600
Fax
+(679) 3300 462
Out of hours +(679) 99202971
Email: carrollk@sp.wpro.who.int
PPHSN. SARS Guidelines
09/04/2003
ANNEX 10
INSTRUCTIONS FOR USE OF WHO COUNTRY OFFICE SARS
OUTBREAK STOCK.
The WHO Country Office SARS Outbreak Stock is designed to provide essential personnel protective equipment
(PPE) for barrier nursing and collection of clinical specimens from suspected SARS cases. It is based on estimated
needs for maximum 50 health workers per day for 3-4 days, and high-level protection for 6-8 procedural / laboratory
workers for a similar period. This will be adequate for a small SARS outbreak or isolation of suspected SARS patients
until larger stocks can be accessed.
The stock is intended as an interim measure only to assist preparedness for a SARS outbreak. Countries should
compile larger stocks of equipment as soon as possible, or ensure rapid access to larger stocks.
Storage / positioning of the stock.
The stock should be stored where it can be readily accessed at all times for despatch to a facility / transport
where suspected SARS patients are involved, including after-hours.
The WR, CLO or recipient of the kit should decide this in consultation with the national health authorities.
USE OF THE EQUIPMENT.
In all cases, certain principals apply:
PPE reduces but does not completely eliminate the possibility of infection.
Exposure to the infected patient should be kept to an absolute minimum necessary for the level of care required.
Visits by non-staff should be avoided where possible.
PPE is only effective if used correctly and at all times where contact is possible.
Any contact between contaminated (used) PPE and surfaces / clothing / people outside the isolation area must be
avoided.
Used PPE must be sealed in appropriate disposal bags and incinerated or decontaminated.
The use of PPE does not reduce the importance of basic hygiene measures such as hand-washing.
Masks (2 types are provided):
N95 masks are recommended for general use in the isolation room where close contact with the patient and direct
contamination with saliva / sputum (cough, sneezing etc) is not likely. Ideally, masks should be splash-proof (e.g.
3M 1860 model) if available. Change mask after 4-6 hours.
The patient wear an N95 mask at all times when staff / other people are in room.
HEPA (P100, N100) masks are recommended for use during procedures (e.g. intubation, collection of respiratory
or blood specimens) and for laboratory use, where splash of respiratory secretions is likely.
Disposable masks should be discarded after 4-6 hours use. They should not be stored in bags and re-used, shared,
or hung around neck etc. (patient's mask may be reused by patient).
It is essential that the mask makes a complete seal on the face (see attached fitting instructions) at all times. Care
should be taken to ensure seal is complete before approaching patient.
Masks can not be worn with beards / unshaven faces.
If a mask is splashed, wet, it should be changed using strict hand-washing and gloves.
Goggles / eye-wear.
Goggles should be worn at all times during patient contact.
They should be cleaned thoroughly in alcohol-based disinfectant solution prior to re-use.
UVEX goggles may be worn with glasses.
Safety glasses have been included in the stock, they are not a good substitute for goggles and should only be
used if extreme heat and humidity prevents goggles from being tolerated.
GENERAL NOTES ON USE OF PPE EQUIPMENT
(see accompanying notes on patient isolation).
Decide where the patient(s) is to be isolated.
The isolation facility should be arranged as follows:
Isolation room. Patient care room, with no air flow to other rooms.
Changing room. Separate areas in room for storage of outside clothes, and removal of PPEs.
General access area (i.e. rest of hospital).
Further details on choosing and setting up isolation rooms are under preparation, but it is important that appropriate
sites be designated now.
PPHSN. SARS Guidelines
09/04/2003
Specify who should wear PPEs
All doctors, nurses and health care workers who provide direct patient care to SARS cases (keep to minimum
necessary for patients' condition)
All support staff including medical aides, cleaners, laundry staff (keep to minimum necessary for patients'
condition, designated SARS laundary staff etc.)
All laboratory staff who handle patient specimens from suspect cases (keep to minimum necessary for laboratory
procedures)
Family members who care for SARS patients (minimum visiting, avoid close contact)
Putting on the PPEs before entering isolation area.
Wear scrub suit or old set of thin clothes before entering the designated changing room or area
Put on the shoe covers or boots with trousers tucked inside
Put on the outer laboratory gown or coveralls
Put on the impermeable apron
Put on gloves with gown sleeve cuff tucked into glove.
Put on the mask and goggles.
(Boots are provided for heavily contaminated / wet flooring and floor cleaning. They should be cleaned as the
goggles are).
Taking off the PPEs and leaving area.
Wash gloved hands in >60% alcohol handwash solution (Sterillium). (Disinfect boots with 1% bleach)
Using gloved hands, remove aprons, gowns, and shoe covers without contaminating clothing underneath. Place in
biohazard disposal bag.
Remove gloves.
Wash hands in >60% alcohol solution.
Remove goggles and place in receptacle for cleaning with alcohol (note: personnel cleaning goggles should use
same PPE procedure).
Remove head cover and mask, place in biohazard disposal bag.
Wash hands to elbows thoroughly in >60% alcohol hand cleansing solution, followed by soapy water.
Change into street clothing and wash hands in soapy water before leaving facility.
*****
More details on isolation procedures and care of isolated patients can be found in:
WHO: Hospital Infection Control Guidance. Care for patients with SARS.
CDC: Severe Acute Respiratory Syndrome (SARS).Updated Interim Domestic Infection Control Guidance in the
Health Care and Community Setting for Patients with Suspected SARS.
WHO-CDC: Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting. (Refer chapters
3-7 & 9).
These have been sent on 20 Mar 03.
Collection of pathology specimens and use of drugs, and general notes on isolation and use of PPE, will be
detailed in a later bulletin. Doxycyclin is provided as a useful drug in some instances of atypical pneumonia, but
is not a specific treatment for SARS.
Countries to receive WHO country Office SARS Outbreak Stock:
Cambodia, Fiji (2), Guam, Kiribati, Laos, Mongolia, Myanmar, Papua New Guinea, Philippines, Samoa, Solomon
Islands, Tonga, Vanuatu (modified kit to Macao, Brunei).
PPHSN. SARS Guidelines
09/04/2003
WPRO SARS Preparedness Kit contents list.
The list below is designed to provide essential equipment for barrier nursing and pathology
collection for suspected SARS cases. It is based on estimated needs for maximum 50 health
workers per day for 3-4 days, and high-level protection for 6-8 procedural / laboratory workers for
a similar period.
INFECTION CONTROL EQUIPMENT
Coveralls
Disposable Aprons (yellow)
Shoe covers
Hair cover (bouffant)
Safety glasses
Non-fog goggles
UVEX goggles
HEPA (P100, N100) Mask
Reusable HEPA half-face
mask (P100, N100)
HEPA mask replaceable
filter
N95 particulate mask
Disposable gloves
Surgical gloves
Anti-microbial waterless
hand-wash
Anti-microbial waterless
hand-wash refills
Absorbent laboratory mat
Aprons: impermeable
Rubber boots
30
200
200 pair
200
30
50
10
30
10
10 large, 10 medium, 10 small (includes hood) polypropylene
40 pair
Not yet in all kits
200
500 pair
150
10
bottles
10
bottles
2 rolls
200
10 pairs
Biohazard disposal bags
100
LABORATORY EQUIPMENT
Sterile cotton swab sticks
1 box
Vacutainer 5 ml EDTA
1 box
Vacutainer 5ml plain
1 box
Vacutainer needles
200
Vacutainer adapters
200
Syringe 5ml
100
Butterfly needles
50
Sterile screw-top plastic
25 ml
specimen containers
SPECIMEN SHIPPING
Bio-bottles 0.5L shipping
2
containers
Cryogenic vials 5ml
100
Cooler, large capacity
1
Ice packs
12
Ziplock bags
200
DRUGS
Doxycyclin
100mg
PPHSN. SARS Guidelines
09/04/2003
Polypropylene
Not adequate eye protection: see notes above.
2-lens
Can be worn with glasses/spectacles
Disposable
Not yet in all kits
100 large, 200 medium, 200 small
> 60% alcohol, with emollient ('Sterillium 1000ml) dispensor
(Sterillium 1000 ml)
3 x 50ft
2 L, 4 M, 4 S
autoclavable
(1000)
(50)
(100)
100
For transport of field specimens
300 tabs
Annex 11
Example of instructions for a close contact (with no fever) of a known, probable or suspect case of
SARS. This should be treated as a guideline only that countries may wish to consider adapting for
local use, and not as an official WHO recommendation.
Someone in this category who remains without a fever, should be instructed to:
Maintain home-based personal isolation during the incubation period;
Remain at home from work or school;
Not leave the house for the period of isolation;
Not answer the door (arrange for other family members to do this);
Not have visitors to the house;
Minimise contact with other household members, but if close contact cannot be avoided, wear
a mask;
Sleep in a separate room away from others. Use separate utensils and dishes for meals, and
wash these separately from other utensils and dishes;
Take his or her temperature daily with a provided thermometer and record the results;
Take his or her temperature if feeling feverish or unwell;
Monitor self for appearance of possible early symptoms of SARS, such as muscle aches and
pains, headache, dizziness, and loss of appetite, tiredness, confusion, rash, and diarrhoea.
Respiratory symptoms of SARS usually occur after these early prodromal symptoms and may
include cough, sore throat, and shortness of breath;
Continue to monitor his or her temperature if respiratory symptoms develop;
Avoid others, cover face or wear a mask if coughing or sneezing;
Wear a mask at all times to limit the spread of respiratory droplets, if possible;
Maintain daily telephone contact with the Department of Health SARS team to report
symptoms of SARS and other problems.
Responsibilities of the health worker:
Teach the contact how to use the thermometer;
Provide the contact with written details of the duration of his or her potential incubation period;
Tell the contact how to maintain daily contact with the designated health worker, or the person
responsible for monitoring him or her during the incubation period. This may include telephone
contact, or a home visit by a health worker;
Ensure the contact is well prior to entering the house without PPE on;
Tell the contact not to travel to a clinic or hospital without talking to the health worker, to avoid
further disease transmission in the community;
Provide contacts with an emergency 24-hour contact number that they can call in the event of fever.
Make arrangements for the transport of a febrile contact to a designated hospital or health care
facility, equipped to triage and manage possible SARS cases;
Supply contacts with a small number of masks and instructions on how to properly fit the mask;
Tell the contacts when the end of their incubation period is over, and give instructions about reentering the community, and returning to work or school.
What the contact should be given:
A thermometer;
A simple chart to record temperatures;
A small supply of masks (these can be surgical masks where N95 masks are not available);
Written details of their potential incubation period and the process for confirming they are out of the
incubation period;
Details of their health worker or another contact person, whom they should talk to once daily;
Details of the 24 hour SARS emergency number to call if they develop a fever; A written copy
of advice about home-based isolation and personal surveillance for fever.
A written copy of advice about home-based isolation and personal surveillance for fever.
PPHSN. SARS Guidelines
09/04/2003
Annex 11B
Example of advice for a traveller from an affected area with NO known contact with a SARS case.
Transmission of SARS to people who have short or casual contact with a case appears uncommon.
While people in this category remain without a fever, they should be instructed to:
o Maintain personal surveillance for fever during the incubation period:
o Monitor self for appearance of fever and respiratory symptoms;
o Asymptomatic casual contacts of a suspect or probable case of SARS need not be isolated
if they remain well.
A traveller in this category should be given the following information/advice:
Information for calculating the potential incubation period (last day in affected area + 14 days);
Travellers from a SARS affected area who develop a fever should be told not to travel to a clinic or
hospital for review without first discussing it with a health worker (SARS hotline);
Details of an emergency 24-hour SARS contact number should be provided in case a traveller
develops a fever;
Where possible, there should be procedures in place to transport a febrile traveller to a designated
hospital or health care facility, equipped to triage and manage possible SARS cases.
PPHSN. SARS Guidelines
09/04/2003