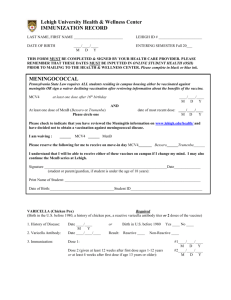
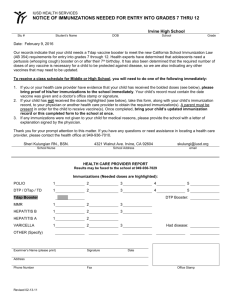
Hepatitis B Vaccine (Engerix -B)
advertisement

Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March SECTION 8 – BIOLOGICAL PRODUCTS TABEL OF CONTENTS DIPHTHERIA - TETANUS- ACELLULAR PERTUSSIS - HEPATITIS B- POLIO- HAEMOPHILUS INFLUENZAE TYPE B ADSORBED (DTAP- HB- IPV- HIB) (INFANRIX HEXA) ............................................. 3 DIPHTHERIA -TETANUS - ACELLULAR PERTUSSIS-POLIO-HAEMOPHILUS INFLUENZAE TYPE B ADSORBED (DTAP-IPV-HIB) (PEDIACEL) ............................................................................................................. 4 DIPHTHERIA-TETANUS- ACELLULAR PERTUSSIS - POLIO ADSORBED (DTAP-IPV) (QUADRACEL) 5 HAEMOPHILUS B CONJUGATE VACCINE (ACT-HIB ) ...................................................................................... 6 HEPATITIS A VACCINE: INDICATIONS .................................................................................................................... 7 HEPATITIS A VACCINE (INACTIVATED VIRAL) (HAVRIX ) ........................................................................... 8 HEPATITIS A VACCINE (INACTIVATED VIRAL) (VAQTA ) ........................................................................... 10 HEPATITIS B VACCINE PRE-EXPOSURE INDICATIONS ................................................................................... 11 HEPATITIS B VACCINE (ENGERIX-B) .................................................................................................................. 12 HEPATITIS B VACCINE PRE-EXPOSURE (RECOMBIVAXHB) (10 MCG/1.0 ML) ....................................... 13 HEPATITIS B VACCINE POST-EXPOSURE INDICATIONS ................................................................................. 15 HEPATITIS B IMMUNE GLOBULIN (HBIG) (BAYHEP B ) ............................................................................... 17 HEPATITIS B VACCINE POST EXPOSURE (RECOMBIVAXHB) (10 MCG/1.0 ML) ..................................... 19 HEPATITIS B VACCINE PROGRAM FOR CHRONIC KIDNEY DISEASE CLIENTS ...................................... 20 HUMAN PAPILLOMAVIRUS VACCINE (GARDASIL)........................................................................................ 21 SEASONAL TRIVALENT INFLUENZA VACCINE (INACTIVATED SPLIT VIRION OR SUBUNIT) ............ 23 INFLUENZA VACCINE (INACTIVATED SPLIT VIRION) (FLUVIRAL) ......................................................... 24 JAPANESE ENCEPHALITIS VACCINE (IXIARO) ............................................................................................... 25 MEASLES/MUMPS/RUBELLA VACCINE (LIVE ATTENUATED VIRAL) MMRII & PRIORIX............. 26 MUMPS, MEASLES AND RUBELLA ALGORITHM DETERMINING IMMUNITY/VACCINATION REQUIREMENTS OF ADULTS.................................................................................................................................... 28 MENINGOCOCCAL C CONJUGATE (MCC) VACCINE (NEIS VAC-C®) ........................................................... 29 MENINGOCOCCAL QUADRIVALENT CONJUGATE VACCINE (MENACTRA).......................................... 31 PNEUMOCOCCAL CONJUGATE VACCINE (PREVNAR®13)............................................................................... 33 COMPLETING A PNEUMOCOCCAL CONJUGATE VACCINE SERIES ............................................................ 35 RECOMMENDATIONS FOR PNEUMOCOCCAL IMMUNIZATION WITH 13-VALENT PNEUMOCOCCAL CONJUGATE VACCINE (PCV 13) AND 23-VALENT PNEUMOCOCCAL POLYSACCHARIDE VACCINE (PPV 23) FOR CHILDREN AT HIGH RISK OF PNEUMOCOCCAL DISEASE ................................................... 36 PNEUMOCOCCAL POLYSACCHARIDE VACCINE (PNEUMOVAX 23) ......................................................... 37 PNEUMOCOCCAL POLYSACCHARIDE VACCINE (PNEUMO 23) ................................................................. 39 POLIO VACCINE (INACTIVATED) (IMOVAX ®POLIO) (VERO CELL ORIGIN) ........................................... 41 Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 2 RABIES VACCINE PRE-EXPOSURE [HUMAN DIPLOID CELL VACCINE (HDCV)] (INACTIVATED) IMOVAX RABIES ........................................................................................................................................................ 43 RABIES VACCINE PRE-EXPOSURE [PURIFIED CHICK EMBRYO CELL VACCINE] (PCECV .................. 45 RABIES POST-EXPOSURE PROPHYLAXIS INSTRUCTIONS .............................................................................. 47 RABIES INVESTIGATION FORM............................................................................................................................... 48 RELEASE OF BIOLOGICALS FOR RABIES POST-EXPOSURE PROPHYLAXIS (RPEP) .............................. 49 HUMAN RABIES IMMUNE GLOBULIN (RABIG) (HYPERRAB™ S/D) .............................................................. 50 RABIES VACCINE POST-EXPOSURE [HUMAN DIPLOID CELL VACCINE (HDCV)] (INACTIVATED) IMOVAXRABIES ......................................................................................................................................................... 52 RHO (D) IMMUNE GLOBULIN (RHIG) (WINRHO ) ............................................................................................. 54 TETANUS-DIPHTHERIA (TD) ADSORBED .............................................................................................................. 55 TETANUS-DIPHTHERIA-ACELLULAR PERTUSSIS (TDAP) (ADACEL) ....................................................... 56 TETANUS-DIPHTHERIA-ACELLULAR PERTUSSIS (TDAP) (BOOSTRIX) ................................................... 58 TETANUS IMMUNE GLOBULIN (TIG) (HYPERTETS/D) .................................................................................. 60 TETANUS PROPHYLAXIS IN WOUND MANAGEMENT ...................................................................................... 62 TUBERCULIN SKIN TEST (MANTOUX) TUBERSOL ........................................................................................ 63 TYPHOID VACCINE (SALMONELLA TYPHI VI CAPSULAR POLYSACCHARIDE)(TYPHERIX) ........... 64 VARICELLA VACCINE (LIVE ATTENUATED VIRAL) VARIVAX III AND VARILRIX........................... 65 VARICELLA ZOSTER VACCINE (LIVE ATTENUATED VIRAL) (ZOSTAVAX) ........................................... 68 YELLOW FEVER (YF-VAX) ..................................................................................................................................... 70 Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 3 Diphtheria - Tetanus- Acellular Pertussis - Hepatitis B- Polio- Haemophilus Influenzae Type b Adsorbed (DTaP- HB- IPV- Hib) (INFANRIX hexa) Supplier: GlaxoSmithKline Inc INDICATIONS (1) Primary series for infants starting at 2 months of age (2) Primary series for high risk infants who have received a birth dose of HBIg and/or Hepatitis B vaccine INITIAL SERIES (1) & (2) Dose 1: 0.5ml IM Dose 2: 0.5ml IM Dose 3: 0.5ml IM Give each dose 2 months apart (3) Primary series for previously unimmunized infants and (3) See Section 3, 1.2 children who are late starting immunization and can complete a SCHEDULE B primary INFANRIX hexa series before 7 years of age REINFORCEMENTS (1) & (2) Booster dose at 18 months of age: 0.5 ml IM of DTaP-IPV-Hib (PEDIACEL) (3) Booster dose 6-12 months after dose 3: 0.5ml IM of DTaP-IPV-Hib ((PEDIACEL) if child is 6 years of age and no Hib dose has been given at 15 months of age, or 0.5 ml IM of DTaP-IPV (QUADRACEL) if child is 6 years of age and a Hib dose has been given at 15 months of age, or 0.5ml IM of Tdap if the child is 7 years of age at time of booster dose. Also give a dose of IPV if child did not receive their 3rd dose of an IPV-containing vaccine after their 4th birthday. CONTRAINDICATIONS 1. History of anaphylactic reaction to a previous dose of DPT, DTaP, IPV, Hib or HB - containing vaccine or to any INFANRIX hexa vaccine component, or to latex. 2. History of Guillain-Barré syndrome (GBS) within 8 weeks of receipt of a tetanus-containing vaccine. 3. INFANRIX hexa is not indicated for children 7 years of age. VACCINE COMPONENTS Aluminum hydroxyphosphate sulfate, L-histidine, polysorbate 80, trace amounts of polymyxin and neomycin ADVERSE EVENTS Local: redness, swelling, pain. Systemic: fever > 38.3° C, anorexia, restlessness, irritability, persistent or unusual crying. SPECIAL CONSIDERATIONS INFANRIX hexa™ contains only a single dose of HB vaccine (as Engerix) and is not indicated for infants and children requiring a double dose of hepatitis B vaccine INFANRIX hexa and PEDIACEL are NOT interchangeable in a primary series. Clients started on PEDIACEL should finish primary series with PEDIACEL Hypotonic-hyporesponsive episodes are not a contraindication to diphtheria, tetanus or acellular pertussis-containing vaccines, and continued immunization with all antigens is recommended. While the number of Hib doses varies with age of presentation, give INFANRIX hexa as indicated above, even when doing so provides “extra” Hib doses for age. Community Nursing Yukon Immunization Program Biological Products March 2011 Page 4 Diphtheria -Tetanus - Acellular Pertussis-Polio-Haemophilus Influenzae Type b Adsorbed (DTaP-IPV-Hib) (PEDIACEL) Supplier: sanofi pasteur INDICATIONS INITIAL SERIES REINFORCEMENTS CONTRAINDICATIONS VACCINE COMPONENTS ADVERSE EVENTS SPECIAL CONSIDERATIONS (1) Primary series and booster for infants and children 2-59 months of age who have had one or more doses of PEDIACEL (2) Primary series for high risk infants who have had doses of hepatitis B vaccine at birth and 1 month of age (3) Booster dose at 18 months of age for infants who have received a primary Infanrix hexa series or a primary PEDIACEL series Dose 1: 0.5ml IM Dose 2: 0.5ml IM Dose 3: 0.5ml IM Give doses 1, 2 and 3 2 months apart + Dose 4: 0.5ml IM Give dose 4 twelve months after 3rd dose School-entry booster is: 0.5 ml IM of DTaP-IPV (QUADRACEL) 1. History of anaphylactic reaction to a previous dose of DPT, DTaP, IPV or Hib--containing vaccine or to any PEDIACEL vaccine component 2. Children 7 years of age. 3. History of Guillain-Barré syndrome (GBS) within 8 weeks of receipt of a tetanus-containing vaccine. Neomycin, streptomycin, polymyxin B, aluminum phosphate, 2phenoxyethanol, polysorbate 80, tetanus protein, formaldehyde and bovine serum. Local: redness, tenderness, swelling. Systemic: irritability, crying, fever >38.3°C, drowsiness, decreased activity and decreased appetite, vomiting and diarrhea. Hypotonic-hyporesponsive episodes are not a contraindication to diphtheria, tetanus or acellular pertussis-containing vaccines, and continued immunization with all antigens is recommended If the child’s immunization schedule is delayed, so that the child requires fewer doses of Hib vaccine, administer QUADRACEL rather than PEDIACEL. If required, this dose can be given as early as 6 months following dose number 3. For protection against Hib, do not give this dose before 15 months of age. Dose number 5 should be given 30 to 54 months after dose number 4 and no sooner than age 4 (the minimum interval between dose 4 and 5 is six months). A 5th dose is not necessary if the 4th dose was given after the 4th birthday. Community Nursing Yukon Immunization Program Biological Products March 2011 Page 5 Diphtheria-Tetanus- Acellular Pertussis - Polio Adsorbed (DTaP-IPV) (QUADRACEL) Supplier: sanofi pasteur INDICATIONS DOSE (1) 0.5 ml IM School Entry Booster (2) 0.5 ml IM Used to complete the primary series and booster for children in whom Hib is not indicated (see routine Hib schedule). CONTRAINDICATIONS 1. History of anaphylactic reaction to a previous dose of DPT, DTaP or IPV-containing vaccine or to any QUADRACEL vaccine component 2. Children ≥ 7 years of age. 3. History of Guillain-Barré syndrome(GBS) within 8 weeks of receipt of a tetanus – containing vaccine. (1) (2) VACCINE COMPONENTS ADVERSE EVENTS Neomycin, polymyxin B, aluminum phosphate, 2-phenoxyethanol, tween 80, formaldehyde and bovine serum. Minor local: redness, tenderness, swelling, pain Minor systemic: fever > 38.3° C, anorexia, vomiting, irritability, drowsiness, listlessness, fretfulness, persistent or unusual crying SPECIAL CONSIDERATIONS Hypotonic-hyporesponsive episodes are not a contraindication to diphtheria, tetanus or acellular pertussis-containing vaccines, and continued immunization with all antigens is recommended. Not necessary if the 4th dose of PEDIACEL, or QUADRACEL was given after the 4th birthday. An interval of 8 weeks is preferred between doses 1, 2, and 3. An interval of 12 months is preferred between doses 3 and 4 (minimum interval between dose 3 and dose 4 is six months.) Dose number 5 should be given 30 to 54 months after dose number 4 and no sooner than age 4 (the minimum interval between dose 4 and 5 is six months). Community Nursing Yukon Immunization Program Section 8- Biological Products 2011 March Page 6 Haemophilus B Conjugate Vaccine (Act-HIB ) Supplier: sanofi pasteur INDICATIONS (1) All children 2-59 months of age AGE AT PRESENTATION INITIAL SERIES 0.5 ml IM (3 doses) 2 – 6 months 2 months apart 0.5 ml IM (2 doses) 7 – 11 months 2 months apart 0.5 ml IM (1 dose) 12 – 14 months 15 – 59 months 0.5 ml IM (1 dose) (2) (3) REINFORCEMENTS 0.5 ml IM at 18 months 0.5 ml IM at 18 months 0.5 ml IM at 18 months None required Unimmunized persons > 5 years of age with the following conditions: anatomic or functional asplenia; sickle cell disease; immunosuppression related to disease (e.g., congenital immunodeficiency states such as complement, properdin or factor D deficiency; malignant neoplasm including leukemia and lymphoma; HIV infection) or therapy (e.g., high dose, systemic steroids; or severe rheumatoid arthritis requiring immunosuppressive therapy); candidates or recipients of solid organ or islet cell transplants, or cochlear implants: 0.5 ml IM (1 dose) No reinforcement required Re-immunization following receipt of a hematopoietic stem cell transplant (HSCT) 0.5 ml IM (3 doses) History of anaphylactic reaction to a previous dose of a HibCONTRAINDICATIONS containing vaccine or to any component of Act-HIB . VACCINE COMPONENTS Tetanus protein and Trometamol. ADVERSE EVENTS Minor Local: redness, tenderness, swelling, pain. Minor Systemic: fever > 38.3° C, fussiness, irritability, lethargy, loss of appetite. It is preferable to use the same Hib product for all doses of the primary series. Using different Hib products during the primary series is acceptable if it is not possible to continue with the initial product. Children who had Hib disease prior to 24 months of age may not have mounted an adequate immune response for protection against Hib disease and should receive vaccine according to the schedule consistent with their age. If series is interrupted, complete series according to age at which child re-presents. The booster recommended at 18 months may be given as early as 15 months provided there is a 2 month interval following the previous dose. At 15 months of age and older, a single dose of any Hib product is all that is required for protective antibody levels. Give vaccine at least 14 days prior to elective splenectomy, or if not possible, 14 or more days post-splenectomy. If there is concern that the patient may not present later for immunization, give vaccine before discharge. One Hib dose is recommended for children and adult asplenics > 5 years of age, regardless of previous Hib immunization. Contact the Vaccine Program Manager prior to immunization for this indication. Community Nursing Yukon Immunization Program Biological Products March 2011 Page 7 Hepatitis A Vaccine: Indications Recommended and provided free to: Individuals with haemophilia A or B receiving plasma-derived replacement clotting factors and testing negative for anti-HAV IgG/HAV total (combined IgM & IgG) negative. Previously unimmunized anti-HCV positive individuals who are anti-HAV IgG/HAV total negative. Previously unimmunized individuals chronically infected with hepatitis B virus who are anti-HAV IgG/HAV total negative. Individuals with other chronic liver disease (including cirrhosis and liver transplant candidates or recipients, liver damage from hemachromatosis) who are anti-HAV IgG/HAV total negative. Users of illicit injection drugs; persons sharing illicit drug snorting, smoking or injecting equipment. Men who have sex with men. Individuals with sexual life-style risks of infection where there is a likelihood of oral-anal contact. Individuals who are HIV positive. Inmates of correctional facilities in which there is epidemiological evidence of sustained Hepatitis A infection (on order of Medical Officer of Health only). Haematopoietic stem cell transplant (HSCT) recipients. Individuals receiving chronic blood transfusions. Contacts of a confirmed case of hepatitis A: Household, Close non-household, Daycare, Drug-sharing, Sexual contacts, Other food handlers at the same establishment if the case is a food handler, Patrons of involved food-handling establishment at risk of hep A as assessed by Public Health staff. Recommended but not provided free to: Travelers, military personnel, and others who will work or live in countries with intermediate or high endemic rates of HAV infection, especially when travel or work will involve rural or primitive conditions. Persons with multiple sex partners. Food handlers. Employees who have been directed to receive this immunization, as per employer direction, must pay upfront for the immunization, ie Department of Highways & Public Works, City of Whitehorse Zookeepers, veterinarians, and researchers who handle non-human primates; certain workers involved in research on hepatitis A virus or the production of hepatitis A vaccine One dose of vaccine is to be provided when it is within 14 days after the last exposure to the case while case was in the infectious period. If a client received 1 dose of hepatitis A vaccine more than 6 months previously, provide a 2nd dose of hepatitis A vaccine. Travelers who opt not to undergo HAV immunization may consider Ig prophylaxis. That is, those who do not have evidence of past hepatitis A infection. Those who have started a vaccine series who now have positive serology should complete the series regardless of the interval between dose 1 & 2. Those who have not started a vaccine series with a positive anti-HAV IgG or HAV total are considered to have lab evidence of immunity against Hepatitis A. For individuals who are HIV positive, please contact YCDC for most recent CD4 counts prior to immunization. Community Nursing Yukon Immunization Program Biological Products March 2011 Page 8 Hepatitis A Vaccine (Inactivated Viral) (Havrix ) Supplier: GlaxoSmithKline See Hepatitis A Vaccine Indications INDICATIONS 6 months up to and including 18 years of age: INITIAL SERIES USING HAVRIX presentation of 720 ELU per 0.5ml Dose 1: 0.5 ml IM Dose 2: 0.5 ml IM 6 to 12 months after dose 1 19 years and older: USING HAVRIX presentation of 1440 ELU per 1.0 ml Dose 1: 1.0 ml IM Dose 2: 1.0 ml IM (1440 ELU presentation) or 0.5 ml IM (720 ELU presentation) 6 to 12 months after dose 1 REINFORCEMENTS Currently no recommendation for booster dose(s). CONTRAINDICATIONS History of an anaphylactic reaction to a previous dose of any hepatitis A vaccine, to any component of HAVRIX vaccine or to latex (prefilled syringe presentation only). VACCINE COMPONENTS Formaldehyde, aluminum hydroxide, 2-phenoxyethanol, polysorbate 20, neomycin B sulphate, potassium chloride, disodium phosphate, monopotassium phosphate, bovine serum albumin, amino acids. ADVERSE EVENTS Tend to be mild and transient. Local: Soreness and redness at injection site Systemic: Headache, fatigue, fever, malaise, and gastrointestinal symptoms SPECIAL CONSIDERATIONS Active immunization with hepatitis A vaccine is the first choice for protection against hepatitis A for travellers. Given the good serologic response to vaccine after the primary dose, simultaneous administration of Ig is not indicated even if the vaccine is given immediately before departure. Ig may be used for infants 6 months of age and individuals for whom the vaccine is contraindicated. Post – vaccination testing is not indicated following a Hepatitis A vaccine series Community Nursing Yukon Immunization Program Biological Products March 2011 Page 9 Hepatitis A Vaccine (Inactivated Viral) (Havrix ) Supplier: GlaxoSmithKline The hepatitis A vaccines HAVRIX, VAQTA, AVAXIM, AVAXIM Pediatric, and ViVAXIM are interchangeable at any scheduled dose for children or adults, using the age-specific dosage for the particular product. HAVRIX is licensed for persons 1 year of age. However, numerous studies have demonstrated the immunogenicity and safety of hepatitis A vaccine for infants at 6 months of age. Immune response may be blunted in some children less than 6 months of age due to interference with maternally derived antibody. As maternal hepatitis A antibody status is usually not known, contact the Vaccine Program Manger to discuss giving Ig to infants 6 months of age who are at risk for hepatitis A. Studies have shown that 720 ELISA units provides an effective booster dose in those ≥19 years of age For individuals who are HIV positive, please contact YCDC for most recent CD4 counts prior to immunization. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 10 Hepatitis A Vaccine (Inactivated Viral) (Vaqta ) Supplier: Merck Frosst INDICATIONS See Hepatitis A Vaccine Indications INITIAL SERIES 6 months up to and including 17 years of age: Dose 1: 0.5 ml (25U) IM Dose 2: 0.5 ml (25U) IM 6 to 18 months after dose 1 18 years of age: Dose 1: 1.0 ml (50U) IM Dose 2: 1.0 ml (50U) IM 6 months after dose 1 REINFORCEMENTS Currently no recommendation for booster dose(s) CONTRAINDICATIONS History of anaphylactic reaction to a previous dose of any hepatitis A vaccine or to any component of VAQTA vaccine or to latex. VACCINE COMPONENTS Bovine albumin, formaldehyde, neomycin B sulphate, aluminum hydroxide, sodium borate. ADVERSE EVENTS Tend to be mild and transient. Local: Soreness and redness at injection site Systemic: Headache, fatigue, fever, malaise and gastrointestinal symptoms SPECIAL CONSIDERATIONS Active immunization with hepatitis A vaccine is the first choice for protection against hepatitis A for travellers. Given the good serologic response to vaccine after the primary dose, simultaneous administration of Ig is not indicated even if the vaccine is given immediately before departure. Ig may be used for infants 6 months of age and individuals for whom the vaccine is contraindicated. Post – vaccination testing is not indicated following a Hepatitis A vaccine series The hepatitis A vaccines HAVRIX, VAQTA, AVAXIM, AVAXIM Pediatric, and ViVAXIM are interchangeable for children or adults at any scheduled dose, using the age-specific dosage for the particular product. Vaqta does not contain a preservative; use immediately and discard any remainder. Vaqta is licensed for persons 1 year of age. However, numerous studies have demonstrated the immunogenicity and safety of hepatitis A vaccine for infants at 6 months of age. Immune response may be blunted in some children less than 6 months of age due to interference with maternally-derived antibody. As maternal hepatitis A antibody status is usually not known, contact the vaccine program manager to discuss giving Ig to infants 6 months of age who are at risk for hepatitis A. For individuals who are HIV positive, please contact YCDC for most recent CD4 counts prior to immunization. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 11 Hepatitis B Vaccine Pre-exposure Indications Provided free to: All children ≤ 19 years of age. All Community Nursing personnel and Yukon Communicable Disease Control personnel All Yukon EMS personnel in Whitehorse and the rural communities (complete log & submit March 31 of each year to CN financial admin assistant, and immunizations will be paid for by EMS). Household contacts of acute Hepatitis B cases or Hepatitis B chronic carriers. Sexual contacts of acute Hepatitis B cases or Hepatitis B chronic carriers. Users of illicit injectable drugs and their sexual partners. Persons sharing illicit drug snorting, smoking or injecting equipment. Males who have sexual contact with other males. Individuals who are HIV positive Persons with multiple sexual partners or recent history of a sexually transmitted infection (STI). Anti-HCV positive individuals who do not have past or current evidence of hepatitis B infection. Individuals with significant chronic liver disease (including cirrhosis, candidates or recipients of liver transplant, and liver damage from hemachromatosis) who do not have past or current evidence of hepatitis B infection. Hemophiliacs and others receiving repeated infusions of blood or blood products. Individuals with chronic kidney disease (predialysis, hemodialysis, and peritoneal dialysis clients) and candidates or recipients of a kidney transplant. Previously unimmunized residents and staff of developmentally challenged known hepatitis B carriers whose behavior or medical condition increases risk to others Previously unimmunized children and staff in childcare settings in which there is a child infected with hepatitis B (upon order of Medical Health Officer). Recommended but not provided free to: All Health Care Workers All employees who have been directed to receive this immunization, as per employer direction, must pay upfront for the immunization ie City of Whitehorse, Department of Highways & Public Works Persons visiting countries with high HBV endemicity areas and/or having sexual or blood contact with local residents regardless of length of stay. Starting in 1994 YT has had either a school based or infant hepatitis B immunization program; therefore many individuals born in 1983 through present day are immunized. If no records are available and the client is unable to recall receiving hepatitis B vaccine, proceed with hepatitis B vaccination as per indication. Prevaccination testing for HBsAg, anti-Hbc and anti-HBs is recommended for persons at high risk of having been infected (i.e., IDU, STW, individuals with HCV or chronic liver disease, and persons born in countries of high hepatitis B prevalence). Post vaccination serology is recommended for those with chronic liver disease. not routinely recommended. Serology to determine protective status for hepatitis B is prudent in those with chronic liver, chronic renal & HIV infection. If anti-HBs is < 10IU/L but is detectable, provide one dose of vaccine and retest 4 weeks after this dose. If level is ≥ 10 following this dose, no further vaccine is required. When anti-HBs is <10 IU/L after this one dose, complete the second vaccine series and retest 4 weeks after the last dose. Do not complete more than 2 complete Hepatitis B series. Hemodialysis clients require a specific hepatitis B vaccine dosage and series. See Section 5, Immunization of Special Populations, Chronic Kidney Disease. For individuals who are HIV positive, please contact YCDC for most recent CD4 counts prior to immunization. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 12 Hepatitis B Vaccine (Engerix-B) Supplier: GlaxoSmithKline Pediatric presentation 10 mcg/0.5 ml; adult presentation 20mcg/1.0 ml INDICATIONS INITIAL SERIES (1) See Hepatitis B Vaccine Preexposure Indications (2) See Hepatitis B Vaccine Postexposure Indications (3) Use when there is a contraindication to RecombivaxHB or when RecombivaxHB is not available (1) (2) & (3) Infants from birth, children, and adolescents to 19 years of age inclusive (except the routine infant program and neonates who will be contacts of chronic carriers)0.5 ml IM (10 mcg) at 0, 1 and 6 months (4) Adolescents 11 years of age, but 15 years of age at the initiation and completion of series. REINFORCEMENTS CONTRAINDICATIONS VACCINE COMPONENTS ADVERSE EVENTS Eligible adults 20 years of age 1.0 ml IM (20 mcg) at 0, 1 and 6 months (4) 1.0 ml IM (20 mcg) at 0 and 6 months (Use adult single dose formulation) None History of anaphylactic reaction to a previous dose of any hepatitis B vaccine or to any component of Engerix-B. Aluminum hydroxide, and traces of yeast. Thimerosal Fever ( 37.7C) and mild short-term soreness at injection site. Engerix-B & RecombivaxHB are interchangeable at any dose, using age-specific dosage and recommended schedule for the respective product. There must be a minimum of 6 months between doses 1 and 2 whenever both products are used in a 2-dose series. The single dose pediatric formulation (10 mcg/0.5 ml vial) and the adult single dose (20 mcg/1.0 ml) formulation are thimerosal-free. A minimum of 1 month must pass between dose 1 and 2. Dose 3 must be given at least 4 months after the 1st dose and 2 months after the 2nd dose. If the immunization series is interrupted after the 1st dose, the 2nd dose should be administered as soon as possible. If only the 3rd is delayed, administer as soon as possible. Hemodialysis clients require a specific hepatitis B vaccine dosage and series (see Hepatitis B Vaccine Program for Chronic Kidney Disease Clients). Serology to determine protective status for hepatitis B is prudent in those with chronic liver, chronic renal & HIV infection. If anti-HBs is < 10IU/L but is detectable, provide one dose of vaccine and retest 4 weeks after this dose. If level is ≥ 10 following this dose, no further vaccine is required. When anti-HBs is <10 IU/L after this one dose, complete the second vaccine series and retest 4 weeks after the last dose. Do not complete more than 2 complete Hepatitis B series. High risk infants who receive a birth dose of Hepatitis B vaccine and/or HBIg can complete their vaccine series with INFANRIX hexa at 2, 4 and 6 months of age. Infants who have been given doses of Hepatitis B vaccine at birth and 1 month of age should be given PEDIACEL vaccine at 2, 4 and 6 months of age, and a 3rd dose of Hepatitis B vaccine at 6 months of age. These infants weighing < 2000 grams at birth will require a 4th dose of Hepatitis B vaccine at 8 months of age. There must be a minimum of 6 months between doses 1 and 2. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 13 Hepatitis B Vaccine Pre-Exposure (RecombivaxHB) (10 mcg/1.0 ml) (Pediatric presentation: 5 mcg/0.5 ml, thimerosal free) Supplier: Merck Frosst INDICATIONS INITIAL SERIES (1) Infants, including infants weighing (1) Give 0.5ml IM (5mcg) at birth < 2000 grams at birth, whose father or other primary caregiver Give INFANRIX hexa at 2 - 4 - 6 months or household contact has chronic hepatitis B infection. Use thimerosal free vaccine. (2) Infants who are part of the routine (2) 0.5 ml IM (5 mcg) at 2-4-6 months. Hepatitis B program and receiving PEDIACEL in the primary series Use thimerosal free vaccine. (3) 0.5 ml IM (5 mcg) at 0-1-6 months (3) Infants and children and adolescents to19 years of age inclusive (except the routine infant program, neonates who will be contacts of chronic carriers). Use thimerosal free vaccine. (4) Adolescents 11years of age, but (4) 1.0 ml IM (10 mcg) at 0 and 6 months 15 years of age at time of initiation & completion of series. Use thimerosal free vaccine. (5) 1.0 ml IM (10 mcg) at 0-1-6 months. (5) Eligible adults 20 years of age. (6) See Hepatitis B Vaccine Preexposure Indications (7) See Hepatitis B Vaccine Postexposure Indications REINFORCEMENTS None. CONTRAINDICATIONS History of anaphylactic reaction to a previous dose of any hepatitis B vaccine, to any component of RecombivaxHB or to latex. Aluminum hydroxide, formaldehyde, yeast, and thimerosal when the 3 mL vial presentation is used. Fever ( 37.7 C) and mild short-term soreness at injection site. VACCINE COMPONENTS ADVERSE EVENTS Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 14 Hepatitis B Vaccine Pre-Exposure (RecombivaxHB) (10 mcg/1.0 ml) (Pediatric presentation: 5 mcg/0.5 ml, thimerosal free) Supplier: Merck Frosst Engerix-B & RecombivaxHB are interchangeable at any dose, using age-specific dosage and recommended schedule for the respective product. There must be a minimum of 6 months between doses 1 and 2 whenever both products are used in a 2-dose series. A minimum of 1 month must pass between dose 1 and 2. Dose 3 must be given at least 16 weeks after the 1st dose and 8 weeks after the 2nd dose. If the immunization series is interrupted after the 1st dose, the 2nd dose should be administered as soon as possible. If only the 3rd is delayed, administer as soon as possible. If years have lapsed between the 1st and 2nd dose, it may be prudent to assess antibody response post series, especially if the client is at significant risk. Hemodialysis clients require a specific hepatitis B vaccine dosage and series (see Hepatitis B Vaccine Program for Chronic Kidney Disease Clients) A 0.5 ml (5mcg) Recombivax HB dose represents a double dose for infants and children < 11 years of age. Infants who have been given doses of Hepatitis B vaccine at birth and 1 month of age should be given PEDIACEL vaccine at 2, 4 and 6 months of age, and a 3rd dose of Hepatitis B vaccine at 6 months of age. These infants weighing < 2000 grams at birth will require a 4th dose of Hepatitis B vaccine at 8 months of age. While a second dose can be given 4 – 6 months following the first dose, the dose is suggested at 6 months for consistent timing with other vaccine programs administered in the school setting. Serology to determine protective status for hepatitis B is prudent in those with chronic liver, chronic renal & HIV infection. If anti-HBs is < 10IU/L but is detectable, provide one dose of vaccine and retest 4 weeks after this dose. If level is ≥ 10 following this dose, no further vaccine is required. When anti-HBs is <10 IU/L after this one dose, complete the second vaccine series and retest 4 weeks after the last dose. Do not complete more than 2 complete Hepatitis B series. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 15 Hepatitis B Vaccine Post-Exposure Indications Provided free to: Infant born to known HBsAg + mother. Give HBIg and hepatitis B vaccine at birth. Infant born to a mother who is at high risk for hepatitis B infection (intravenous drug use or sex trade work) and her infectious status at delivery is unknown or negative (possible window period); give HBIg and hepatitis B vaccine at birth. Infants born to mother who has risk factors (other than IDU and/or STW) for hepatitis B infection and her infectious status at delivery is unknown or negative (possible window period). Give hepatitis B vaccine at birth. Infant whose father or other primary care giver or household contact has chronic hepatitis B infection. Give hepatitis B vaccine at birth. Infants from birth to 12 months of age if father or other primary caregiver are at high risk for hepatitis B infection and their infectious status is unknown or negative (possible window period). Give hepatitis B vaccine at birth. Infant < 12 months of age whose mother has acute hepatitis B. Household contacts (including infants) of acute case or chronic carrier. Sex with a person who has acute or chronic hepatitis B infection. Percutaneous or mucosal exposure in the community (i.e. sexual assault, needle sticks) and household contacts with percutaneous or mucosal exposure (i.e. sharing of toothbrushes or razors) of acute or chronic hepatitis B infection. Refer to Yukon Immunization Program, Section 16, Blood & Body Fluid Management for complete guidelines to assess need for HBIg and hepatitis B vaccine. These guidelines do not include post exposure to newborns. For newborn exposure see, Hepatitis B Vaccine Post Exposure (RecombivaxHB). Post-vaccination testing (HBsAg and anti-HBs) of infants must be performed 1 month after completion of the hepatitis B vaccine series. If HBsAg is found, the infant is likely to become a chronic carrier. If the infant is negative for HBsAg and anti-HBs, a 2nd series of hepatitis B vaccine should be given and serological testing repeated 1 month post-series. See . For steady long-term sexual partners of chronic HBV carriers, test for HBsAg, anti-HBc and anti-HBs prior to administering HBIG. If the client is susceptible to HBV, give HBIg as soon as possible and no later than 14 days of last sexual exposure. See . Post-vaccination testing should be performed 1 month after completion of the hepatitis B vaccine series for steady sexual partners of HBV chronic carriers, household contacts of acute and chronic carriers, sexual assault victims and those with percutaneous or mucosal exposures. See . Yukon & HBIg availability HBIG for post exposure prophylaxis is located in the following rural Community Health Centres throughout the territory: Beaver Creek, Dawson City, Haines Junction, Mayo, Old Crow, Ross River, Watson Lake When you receive the HBIg there will be a transfer log enclosed. It must be completed and faxed to the WGH Lab when either a client has received HBIg or the Lot has expired. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 16 Hepatitis B Vaccine Post-Exposure Indications Yukon & HBIg availability In the event a community not listed above requires HBIg, please contact the nearest community to you that has HBIg and make arrangements to have the HBIg brought to your community. For communities with close proximity to Whitehorse there are two routes that can be followed. If a nurse is traveling to the community within 48 hrs contact the Lab and Community Nursing staff will pick up the HBIg and give it to the nurse. In the case where there is no staff traveling to the community, the client may come to WGH Emergency to receive the HBIg. See Section 16, Blood & Body Fluid Management, How to Access HBIg. HBIg is automatically sent to the Whitehorse General Hospital Lab about 6 to 8 weeks prior to EDC. (Since most Yukon babies are born in WGH). Watson Lake Hospital must secure the HBIg from the Whitehorse General Hospital Lab). If any other health facility requires HBIg, call the Lab at Whitehorse General Hospital. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 17 Hepatitis B Immune Globulin (HBIg) (BayHep B ) Supplier: Bayer INDICATIONS (1) Infant born to known HBsAg positive woman DOSAGE (1) Give HBIg 0.5 ml IM immediately after birth, along with first dose of hepatitis B vaccine series. (2) Infant born to woman at high risk for hepatitis B infection (i.e., intravenous drug use, sex trade work)) whose infectious status is unknown or negative (possible window period) (2) Give HBIg 0.5 ml IM immediately after birth, along with first dose of hepatitis B vaccine series. (3) Infant 12 months of age has mother with acute hepatitis B infection (3) Consider the immune status of the infant and history of hepatitis B immunization and give HBIg 0.06ml/kg of body weight IM and hepatitis B vaccine as required (4) Percutaneous or mucosal exposure to HBsAg positive source (4) Give HBIg 0.06 ml/kg of body weight and hepatitis B vaccine IM as required, considering the client’s immune status and history of hepatitis B immunization. (5) Sex with a person who has acute or chronic hepatitis B infection (5) REINFORCEMENTS CONTRAINDICATIONS Give HBIg 0.06 ml/kg of body weight IM as soon as possible following the last sexual exposure, along with hepatitis B vaccine series An at-risk known non-responder to two series of vaccine requires 2 doses of HBIG one month apart None Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 18 Hepatitis B Immune Globulin (HBIg) (BayHep B ) Supplier: Bayer PRECAUTIONS Human Ig products are among the safest blood-derived products available. The method of preparation includes one or more steps that exclude or inactivate hepatitis B, C and HIV; therefore the risk of transmission is extremely low. However, it is possible that unknown infectious agents may be present in such products. Regarding HBIg and the administration of live vaccines see CIG (2006), p 54, Guidelines for the interval between Administration of Immune Globulin Preparations or Blood Products and MMR or Varicella Virus. For full Hepatitis B Post-Exposure Prophylaxis guidelines see Section 16, Blood & Body Fluid Exposure Management. Give HBIg with caution (i.e., in a setting capable of managing anaphylaxis) if the person has a history of anaphylactic reaction following receipt of any human Ig product, or a history of anaphylactic reaction to latex (assess risks versus benefits). Clients with severe thrombocytopenia or coagulation disorders that contraindicate IM injections should not be given HBIg unless the benefits outweigh the risks. HBIg does not contain preservatives. Vials are single dose use; discard unused contents. HBIg must be given at a separate anatomic site from hepatitis B vaccine. The preferred site for the administration of HBIg is the ventrogluteal area, which may be used in those > 7 months of age. However, the vastus lateralis is most often used in infants and children up to 5 years of age. ADVERSE EVENTS Local pain and tenderness at injection site, urticaria and angioedema may occur. There is no upper limit to the volume of HBIg that can be administered. Provide a written record to a client who receives any immune globulin product. There is no outer time limit for administering HBIg in infants 12 month’s of age, when the infant’s exposure to the known risk factor(s) is ongoing. For infants < 8.3 kg, give 0.5 ml HBIg. HBIg dose for all clients 8.3kg is 0.06ml/kg. Give HBIg as soon as possible, preferably within 48 hours of the exposure. For a percutaneous exposure, HBIg may be given up to 7days following the exposure. If the client presents 7 days following a percutaneous exposure, give Hepatitis B vaccine only. For permucosal or sexual exposures, HBIg may be given up to 14 days following the last exposure. If the client presents 14 days following a permucosal or sexual exposure, give Hepatitis B vaccine only. See Section Hepatitis B Post-Exposure Prophylaxis table located in, Section 16, Blood & Body Fluid Management. See CIG (2006) for maximum volume to be administered per site according to age. For steady, long term sexual partners of chronic hepatitis B carriers, test for HBsAg, antiHBc and anti-HBs as per scope of practice. See Section 16, Blood & Body Fluid Management for complete guidelines See Section 16, Blood & Body Fluid Management for complete guidelines Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 19 Hepatitis B Vaccine Post Exposure (RecombivaxHB) (10 mcg/1.0 ml) (Pediatric presentation: 5 mcg/0.5 ml, thimerosal free) Supplier: Merck Frosst INDICATIONS INITIAL SERIES (1) Infants born to HBsAg positive mothers (2) Infant weighing 2000 grams at birth and requiring a birth dose of hepatitis B vaccine (3) Infant whose mother is at high risk and infectious status unknown (4) Infant whose caregiver or household contact is a chronic hepatitis B carrier (1) (2) (3) & (4) POST EXPOSURE SCHEDULE FOR OTHER INDICATIONS (1) Infants and children ≤15 years of age. Use thimerosal free vaccine. 0.5 ml IM (5 mcg) at 0-1-6 months. Give 0.5 ml IM (5 mcg) at birth (must be given within 12 hours along with HBIg) Use thimerosal free vaccine Give Infanrix hexa at 2-4-6 months. (2) Adolescents 16 and 20 years of age. 0.5 ml IM (5 mcg) at 0-1-6 months. SPECIAL CONSIDERATIONS (3) Adults 20 years of age. 1.0 ml IM (10 mcg) at 0-1-6 months. Routine information regarding RecombivaxHB vaccine is located on the pre-exposure vaccine page (e.g. vaccine interchangeability, contraindications, precautions, schedule variations, etc). Hemodialysis clients require a specific dose and series (See Hepatitis B Vaccine Program for Chronic Kidney Disease Clients) See Hepatitis B Vaccine Post-Exposure Indications and Blood & Body Fluid Management for complete guidelines to assess need for HBIg, hepatitis B vaccine, and serologic testing for all other groups (i.e., baseline and post exposure). Post-vaccination testing (HBsAg and anti-HBs) should be performed 1 month after completion of the hepatitis B vaccine series. If HBsAg is found, the child is likely to become a chronic carrier. If the infant is negative for HBsAg and anti-HBs, a 2nd series of hepatitis B vaccine should be given and serological testing repeated 1 month post 2nd series. Engerix-B & RecombivaxHB are interchangeable at any dose, using age-specific dosage and recommended schedule for the respective product. There must be a minimum of 6 months between doses 1 and 2 whenever both products are used in a 2-dose series Infants who have been given doses of Hepatitis B vaccine at birth and 1 month of age should be given PEDIACEL vaccine at 2, 4 and 6 months of age, and a 3rd dose of Hepatitis B vaccine at 6 months of age. These infants weighing < 2000 grams at birth will require a 4th dose of Hepatitis B vaccine at 8 months of age. Post-exposure vaccine schedules are individualized based on a number of factors (e.g. immune status of client and history of hepatitis B immunization) See Section Hepatitis B PostExposure Prophylaxis table located in, Section 16, Blood & Body Fluid Management. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 20 Hepatitis B Vaccine Program for Chronic Kidney Disease Clients Chronic hemodialysis clients are at high risk for HBV infection because the process of hemodialysis requires vascular access for prolonged periods. In an environment where multiple clients receive dialysis concurrently, repeated opportunities exist for person-to-person transmission of infectious agents, directly or indirectly via contaminated devices, equipment and supplies, environmental surfaces or hands of personnel. Furthermore, hemodialysis clients are immunosuppressed, which increases their susceptibility to infection. ELIGIBILITY All predialysis, hemodialysis and peritoneal dialysis clients in hospital, community, home or selfcare settings are eligible for this program. Vaccine administration often occurs at the dialysis facility; please verify if this has occurred prior to immunization and enter the appropriate immunization records into iPHIS. PRE-DIALYSIS AND DIALYSIS CLIENTS Engerix-B Schedule Dose Volume Schedule 0, 1 and 6 40 mcg 2.0 ml 0, 1, 2 and 6 months months 7 – 19 0, 1 and 6 20mcg 1.0 ml 0, 1, 2 and 12 10 mcg 1.0 ml years months months Birth – 6 0.5 ml 0, I and 6 0, 1, 2 and 12 5 mcg 20 mcg 1.0 ml years months months Post-vaccination serology: measure anti-HBs 1 month after completion of a primary series. If anti-HBs is 10 IU/L, the client is a non-responder. Provide a second vaccine series and assess anti-HBs. If anti-HBs is 10 IU/L, the client, as a non-responder to 2 vaccine series, is susceptible to hepatitis B. There is no benefit to further vaccination. If an exposure to blood or body fluids occurs, the client will require post-exposure prophylaxis. Age 20 years RECOMBIVAX HB Dose Volume 40 mcg 1.0 ml All doses of hepatitis B vaccine should be administered in the deltoid by the IM route, or for infants <12 months of age, in the vastus lateralis. Pre-dialysis clients and dialysis clients receive the same dose volume of hepatitis B vaccine because there is no discrete level of renal function that correlates well with vaccine immunogenicity. Special formulation for adult dialysis clients. Use adult formulation (10mcg/1.0ml). Use thimerosal-free RecombivaxHB or pediatric Engerix-B formulation. Dosage for this age group is based on NACI guidelines. NOTE: If a client has received Engerix-B vaccine as dose 1, the client will require a 4 dose series regardless of which vaccine is used to complete the series. If a client has received RecombivaxHB vaccine as dose 1, the client will only require a 3 dose series regardless of which vaccine is used to complete the series. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 21 Human Papillomavirus Vaccine (GARDASIL) [Quadrivalent (Types 6, 11, 16, 18) Recombinant] Supplier: Merck Frosst INDICATIONS INITIAL SERIES Recommended and provided free to: (1) Girls in grade 6 starting 2011-2012 school year (extended dose schedule) (1) 2 doses in grade 6: Dose1: 0.5 ml IM Dose 2: 0.5 ml IM (minimum of 6 months after dose one) Dose 3: 0.5 ml IM in grade 11 (60 months) (2) Girls aged 9 years to ≤ 13 years at time of initiation of immunization series (extended dose schedule) (3) Girls in grade 6, 7 & 8 2010-2011 school year (2) 2 doses: Dose1: 0.5 ml IM Dose 2: 0.5 ml IM (minimum of 6 months after dose one) Dose 3: 0.5 ml IM in grade 11 (60 months) (3) (4) & (5) Females or males (4) Other females 14 years to ≤ 26 years of age at initiation of series. 3 doses: 0.5 ml IM 0.5 ml IM at 2 months 0.5 ml IM at 6 months Recommended but NOT provided free: (5) Males 9 years to ≤ 26 years of age at initiation of immunization series. REINFORCEMENTS The duration of vaccine protection is unclear. Current studies (with five-year follow up) indicate that the vaccine is effective for at least five years. This information will be updated as additional data regarding duration of immunity become available. CONTRAINDICATIONS 1. History of anaphylactic reaction to a previous dose of HPV vaccine, or to any component of GARDASIL 2. Pregnancy. Although the vaccine has not been causally associated with adverse outcomes of pregnancy or adverse events to the developing fetus, the data on vaccination in pregnancy are limited. Administer vaccine series after completion of the pregnancy. If a woman is found to be pregnant after initiating the vaccine series, delay completion of the series until after pregnancy. If a vaccine dose has been administered during pregnancy, there is no indication for any intervention. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 22 Human Papillomavirus Vaccine (GARDASIL) [Quadrivalent (Types 6, 11, 16, 18) Recombinant] Supplier: Merck Frosst SPECIAL Women for whom HPV vaccine is recommended may be immunized CONSIDERATIONS even if already sexually active, or if they have had previous Pap abnormalities (including cervical cancer), genital warts, or known HPV infection. This is because the likelihood that they have been infected with all four types of HPV contained in the vaccine is low and they stand to benefit from immunization. Sexually active vaccine recipients should continue to be routinely screened for cervical cancer. VACCINE Amorphous aluminum hydroxyphosphate sulfate, L-histidine, COMPONENTS polysorbate 80, sodium borate, yeast. ADVERSE EVENTS Local: mild to moderate pain, redness, swelling Systemic: headache HPV vaccine was offered in the 2009-2010 & 2010-2011 school years for females in grades 6, 7 & 8. 2010-2011 is the last year of the grade 7 & 8 program. Grade 6 girls who are known to have immune system defects associated with solid organ transplant, stem cell transplant, or HIV infection should receive HPV vaccine in the three dose schedule at 0, 2 and 6 months. The immunosuppressed state results in a less robust immune response, and those with such conditions are at risk of persistent HPV infection and associated HPV disease if they become infected. Currently, routine HPV testing is not recommended before or after immunization. In addition, serologic tests are not routinely available in Canada. Females who are immunocompromised, either from disease or medication, can receive this vaccine; however, the immune response to vaccination and vaccine efficacy might be less than in immunocompetent females. Gardasil™ vaccine can be administered at the same visit as other age-appropriate vaccines, using a separate needle and syringe for each injection. If the schedule is interrupted, the vaccine series does not need to be restarted. If the series is interrupted after any dose, the subsequent dose should be given as soon as possible. The minimum interval schedule between dose one and dose two is 4 weeks, and between dose two and dose three is 12 weeks The minimum interval schedule should not be followed on a routine basis; it should only be used at the client – specific level based on health care provider assessment. The preferred schedule is 0 – 2 – 6 months. In some areas in Canada a 0-6-12 month dosing schedule was used to accommodate pandemic influenza mass immunization. General principles for vaccine series are that longer intervals between doses are not known to result in lower response rates to the series. Advise vaccine recipients that there are no data to suggest the vaccine will have any therapeutic effect on existing cervical lesions (i.e., vaccine does not prevent the consequences of current HPV infection). Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 23 Seasonal Trivalent Influenza Vaccine (Inactivated Split Virion or Subunit) Recommended and provided free to all Yukoners. Special attention should be given to encourage immunization in these high risk groups: (1) People at high risk: People ≥ 65 years of age People of any age who are residents of long-term care facilities Adults (including pregnant women) and children with the following chronic health conditions: - Cardiac or pulmonary disorders (e.g., bronchopulmonary dysplasia, cystic fibrosis, asthma) - Diabetes and other metabolic diseases - Cancer; immunodeficiency (including human immunodeficiency virus [HIV] infection); immunosuppression due to underlying disease or therapy (e.g., severe rheumatoid arthritis requiring immunosuppressive therapies) - Chronic kidney disease - Chronic liver disease, including hepatitis C - Anemia and hemoglobinopathy - Conditions that compromise the management of respiratory secretions and are associated with an increased risk of aspiration (e.g., cognitive dysfunction, spinal cord injury, seizure disorder, and neuromuscular disorders) Children and adolescents (age 6 months to 18 years) with conditions treated for long periods with acetylsalicylic acid Adults who are morbidly obese (BMI ≥40) Aboriginal peoples (on and off reserve) for the 2010 – 2011 influenza season Healthy children age 6 to 23 months Pregnant women. Especially those who will be in their 3rd trimester during the influenza season (typically spanning November to April) Inmates of provincial correctional institutions People working with live poultry (Immunization may reduce the potential for human-avian reassortment of genes should such workers become coinfected with human and avian influenza.) (2) People capable of transmitting influenza to those at high risk: Healthcare workers (HCW) and other personnel who have significant contact with people in the high-risk groups previously described The HCW groups include independent health care practitioners and their staff in community settings. Household contacts (including children) of people at high risk whether or not those high-risk people have been immunized Those who provide care or service in potential outbreak settings housing high risk persons (e.g., crew on ships) Household contacts of children age 0 to 23 months Those providing regular child care to children age 0 to 23 months, whether in or out of the home (3) People who provide essential community services: First responders: police, fire fighters, ambulance Corrections Officers Large cohort studies of health databases have demonstrated that there is no association between childhood vaccination with thimerosal-containing vaccines and neurodevelopmental outcomes, including autistic-spectrum disorders. This includes persons carrying out paid or unpaid work in a health care facility; including persons who volunteer or undergo training in a health care facility for any period of time between November and April. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 24 Influenza Vaccine (Inactivated Split Virion) (FLUVIRAL) Supplier: GlaxoSmithKline Inc. INDICATIONS See Seasonal Trivalent Influenza Vaccine DOSE BY AGE GROUP Age Group Dosage No. Of Doses 6-35 months 0.25 ml IM 1 or 2 3-8 years 0.5 ml IM 1 or 2 9 years 0.5 ml IM 1 REVACCINATIONS Yearly CONTRAINDICATIONS 1. PRECAUTIONS VACCINE COMPONENTS ADVERSE EVENTS SPECIAL CONSIDERATIONS History of anaphylactic reaction to a previous dose of any type of influenza vaccine 2. History of anaphylactic reaction to any component of FLUVIRAL 3. History of anaphylactic reaction to eggs 4. History of Guillain-Barré syndrome (GBS) within 8 weeks of receipt of a previous dose of influenza vaccine 5. Infants less than 6 months of age Severe oculo-respiratory syndrome (ORS) after a previous dose of influenza vaccine. Egg protein, formaldehyde, thimerosal (50 μg per 0.5 mL, = 0.01% w/v), sodium deoxycholate Transient injection site reactions Fever, malaise, myalgia, and fatigue 6-12 hours following vaccination and lasting ~1 - 2 days, especially in individuals receiving influenza vaccine for the 1st time About 1 in 20 people may have cough, sore throat, hoarseness or red eyes, sometimes called “oculo-respiratory syndrome.” Generalized itching may occur, but is uncommon. Discard multi-dose vials 28 days after first entry. Children under 9 years of age who have not previously received seasonal trivalent influenza vaccine require 2 doses given 4 weeks apart. This applies regardless of whether the child received monovalent pH1N1 vaccine in 2009-10. If the child has received one or more doses of seasonal trivalent influenza vaccine in any previous season, only a single dose is required this season. ORS consists of bilateral red eyes or facial swelling or respiratory symptoms such as cough, wheeze, sore throat, chest tightness, difficulty breathing, difficulty swallowing, hoarseness, or sore throat beginning within 24 hours of vaccination. Most people who have had ORS after a previous dose of influenza vaccine do not experience it again. About 5 - 34% experience another episode but it is usually milder. If a client has received influenza vaccine without difficulty following an episode of severe ORS, they may be revaccinated with the vaccine prepared for this season. Severe symptoms of ORS include wheezing, chest tightness/discomfort, difficulty breathing or severe throat constriction/difficulty swallowing. When a client has had severe ORS following influenza vaccine and not received influenza vaccine since, this is considered to be a precaution to future receipt of influenza vaccine. Such individuals who wish to receive influenza vaccine should consult with their primary care physician and MOH for an expert review to distinguish between severe ORS and any anaphylaxis risk. Consult the National Advisory Committee on Immunization Statement on Influenza Vaccination for the current season. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 25 Japanese Encephalitis Vaccine (IXIARO) Supplier: Novartis INDICATIONS (1) Those ≥ 18 years of age who are traveling to endemic regions INITIAL SERIES (1) 1st Dose: 0.5 mL IM deltoid Day- 0 2nd Dose: 0.5 mL IM deltoid Day-28 series needs to be completed at least one week before travel to the high risk area REINFORCEMENTS None at this time CONTRAINDICATIONS VACCINE COMPONENTS ADVERSE EVENTS hypersensitive to Ixiaro or to any ingredient in the formulation or component of the container. Individuals who show hypersensitivity reactions after receiving the first dose of the vaccine should not be given the second dose individuals with the following conditions should be considered as relative contraindications and thorough assessment should be undertaken including risks and benefits. Consider discussion with the clients physician and/or MOH - Pregnant or breastfeeding women - Persons with a bleeding disorder - Immunosuppressed persons due to disease or therapy < 18 years of age Adjuvant/Preservative: aluminum hydroxide Others: sodium chloride, potassium dihydrogen phosphate, disodium hydrogen phosphate. Local: injection site pain, erythema, hardening, swelling and itching Systemic: myalgia, vertigo,fever, headache, rash. G.I: nausea, diarrhea and vomiting allergic reactions usually occur within 3 days but some reactions can occur up to 10 days after getting the vaccine; for this reason counsel clients that they are not to travel to another country for 10 days after you receive the vaccine due to the possibly of delayed reactions. See Section 5, Immunization of Special Populations, International Travelers. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 26 Measles/Mumps/Rubella Vaccine (Live Attenuated Viral) MMRII & Priorix Suppliers: Merck Frosst, MMRII ; GlaxoSmithKline, Priorix INDICATIONS INITIAL SERIES (1) Infants at 12 months of age (1) Dose 1: 0.5 ml SC Dose 2: 0.5 ml SC at 18 months of age (2) Adult HSCT recipients (2) Dose 1: 0.5 ml SC Dose 2: 0.5 ml SC (6 – 12 months later) (3) Infants from 6 months but 12 months of age, if travelling to endemic areas (3) One dose of 0.5 ml SC (upon return, give 2 additional doses at routine times) (4) All individuals who require protection against measles, mumps, OR rubella (4) Dose 1: 0.5 ml SC Dose 2: 0.5 ml SC (1 month later) CONTRAINDICATIONS 1. History of anaphylactic reaction to a previous dose of a measles/mumps/rubella-containing vaccine, to any component of MMRII or Priorix, or to latex when administering Priorix with the pre-filled syringe (latex is present in the pre-filled syringe of diluent for Priorix). 2. Consult the appropriate physician (i.e., either the primary care physician most familiar with the client’s current medical status or a medical specialist) and consult the Vaccine Program Manager or MOH prior to administration to persons whose immune status may be suppressed as the result of disease or therapy. 3. Pregnancy. Counsel female recipients to avoid pregnancy for 1 month following immunization. Risk is theoretical and not observed. Inadvertent immunization during pregnancy is not considered a medical indication for therapeutic abortion. 4. Recent administration of an immune globulin preparation or blood product (see CIG, 2006, Recent Administration of Human Immune Globulin Products, http://www.phacaspc.gc.ca/publicat/cig-gci/pdf/cig-gci-2006-part-5_e.pdf) 5. Physician-diagnosed significant thrombocytopenia after first dose of a MMR vaccine. 6. For high risk/immunocompromised clients only: separate the administration of MMR and varicella vaccine by least 4 weeks. 7. Family history of congenital immunodeficiency. See Yukon Immunization Program Manual, Section 4, Contraindications and Routine Precautions for Immunization. VACCINE COMPONENTS Components of MMRII are neomycin, sorbitol, sucrose, sodium phosphate, human albumin, fetal bovine serum, and hydrolyzed gelatin. Components of Priorix are neomycin sulphate, lactose, amino acids, human albumin, mannitol, and sorbitol. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 27 Measles/Mumps/Rubella Vaccine (Live Attenuated Viral) MMRII & Priorix Suppliers: Merck Frosst, MMRII ; GlaxoSmithKline, Priorix PRECAUTIONS Measles/mumps/rubella immunization should be given on the same day or delayed until 4 weeks after administration of any other live vaccine. Anti-Rho (D) / Rho (D) immune globulin may interfere with response to the rubella component of the vaccine. Rubella-susceptible women who receive anti-Rho(D) / Rho (D) immune globulin post-partum should either be given MMR vaccine at the same time and tested 2 months later for rubella immunity, or should be immunized with MMR vaccine 2 months post-partum, with follow-up ensured. Do TB skin testing on the same day as MMR immunization, or delay TB skin testing for 4 weeks. ADVERSE EVENTS Local - Tenderness, redness, swelling, induration, wheal and flare reaction, urticaria Systemic – Moderate fever, rash, malaise, headache, and nausea, myalgia, and paraesthesia; thrombocytopenia; encephalitis. Acute transient arthritis or arthralgia is uncommon in children, but frequency and severity increases with age. 25% of post-pubertal females may experience arthralgia, and 10% may have transient arthritis-like signs and symptoms. SPECIAL Consult the appropriate physician (i.e., either the primary care physician most CONSIDERATIONS familiar with the client’s current medical status or a medical specialist) regarding the appropriateness of MMR vaccine administration to persons whose immune status may be suppressed as the result of disease or therapy(e.g., chronic renal disease / dialysis; HIV/AIDs (if no significant compromise); solid organ transplant candidate; hyposplenia/asplenia; ≥ 3 months after being cured of a malignant disease and the end of immunosuppressive treatment; and high doses of oral corticosteroid therapy) Administer the entire volume of reconstituted product, which may be 0.5 – 0.7 ml 2nd dose must be given at least 1 month after 1st dose. Second dose is provided for protection against measles and, for some age groups, mumps. Wait at least 24 months after ablative therapy before administering MMR and then only if the recipient is deemed to be immunocompetent by the transplant specialist. MMR should not be given to those with chronic graft-versus-host disease (GVHD) or those taking immunosuppressive therapy for chronic GVHD. Consult the Vaccine Program Manager prior to immunization for this indication. Those born prior to 1957 are considered to have acquired natural immunity to measles, mumps, and rubella, if not in a high risk group ONLY. All those borne on or after January 1, 1970 require documentation of 2 doses of a live MMR vaccine at ≥12 months of age and given at least 4 weeks apart. DOB prior to 1970 assumes immunity to measles and mumps, with the exception of those at high risk including: HCWs, travellers to endemic areas, military recruits and students attending a post secondary institution. In this population additional assessments are required. See Mumps Measles and Rubella Algorithm Determining Immunity/Vaccination Requirements of Adult, on following page. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 28 Mumps, Measles and Rubella Algorithm Determining Immunity/Vaccination Requirements of Adults Born Before 1970 (DOB 1900-1969) Asses risk status Not at high risk Documented 1 dose of rubella containing vaccine and/or history of disease Consider immune to mumps, measles & rubella At high risk Assessment of immune status required Born After 1970 (DOB 1970-present) Assessment of Immunization Status Documented 2 doses of MMR vaccine Documented 1 dose of MMR vaccine Give 1 dose of MMR vaccine No documentation of previous doses of MMR vaccine Check serology for measles, mumps and rubella AND Give 1 dose of MMR vaccine Box A Measles: Lab evidence of immunity (IgG positive) or, After 2 documented MMR vaccines no further vaccination is warranted regardless of serology history of lab-confirmed disease AND Mumps: labconfirmed infection AND Rubella: Lab evidence of immunity (IgG>10 IU/mL) or, lab evidence of acute infection (IgM) Consider immune to mumps, measles & rubella Negative or indeterminate status in ANY one of the following: Measles, Mumps, or Rubella - as defined in Box A Consider non immune Give 2nd dose of MMR vaccine A birth date prior to 1970 is not definitive for immunity against mumps or measles. Further assessment is required if the client is in a high risk group including: travelers to endemic areas, health care workers, military recruits, students at post-secondary institutions. Additional assessment may include history of disease, exposure to clinical illness after exposure to a confirmed case, clinical history of illness in conjunction with serology and assessment of immunization status. MMR vaccine must be given ≥ 12 months of age at least 4 weeks apart If current screening results are “indeterminate”, with a documented prior history of Rubella “immune” (IgG>10IU/mL) client is considered immune to rubella. If DOB prior to 1957, assume immunity to mumps, measles and rubella. If not at high risk ONLY. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 29 Meningococcal C Conjugate (MCC) Vaccine (Neis Vac-C®) Supplier: GlaxoSmithKline INDICATIONS INITIAL SERIES (1) Two-dose program for infants (1) Dose 1: 0.5 ml IM at 2 months of age or age at presentation. (When age of presentation is 12 months, one dose only is required.) Dose 2: 0.5 ml IM at 12 months of age (at least 2 months after 1st dose) (2) Children not previously vaccinated or who received their last dose of any MCC vaccine when they were less than 12 months of age (2) One dose: 0.5 ml IM at 12 months of age (3) Medically high risk children 2 months to < 12 months of age (4) Close contacts of a case of invasive meningococcal group C disease that meet the criteria for chemoprophylaxis who have NOT been previously vaccinated with MCC vaccine as directed by YCDC (5) Medically high risk children 2 – 10 years of age who have NOT been previously vaccinated with any MCC vaccine (3) & (4) Age at presentation: 2 months to < 12 months of age: Dose 1: 0.5 ml IM Dose 2: 0.5 ml IM at least 2 months after 1st dose Dose 3: 0.5 ml IM at 12 months of age (at least 2 months after 2nd dose) 12 months of age (any MCC vaccine may be used): One dose: 0.5 ml IM (5) One dose: 0.5 ml IM (6) Children up to 19 years of age who are previously unimmunized. (6) One dose: 0.5 ml IM (7) Grade 6 students starting 2011-2012 school year (7), (8) & (9) One dose: 0.5 ml IM (8) Grade 9 students in 2011/2012, 2012/2013 & 2013/2014 school years (9) Students attending post secondary education outside of YT not previously immunized. CONTRAINDICATIONS VACCINE COMPONENTS History of anaphylactic reaction to a previous dose of any meningococcal vaccine or to any component of Neis Vac-C vaccine. Aluminum hydroxide, tetanus toxoid Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 30 Meningococcal C Conjugate (MCC) Vaccine (Neis Vac-C®) Supplier: GlaxoSmithKline ADVERSE EVENTS All: redness, swelling and pain at injection site; headache, fever Infants and toddlers: crying, irritability, drowsiness, somnolence/impaired sleeping Infants: vomiting/nausea/diarrhea/loss of appetite SPECIAL CONSIDERATIONS Upon storage, a white deposit and clear supernatant can be observed. Shake the vaccine well in order to obtain a homogenous suspension. There must be an interval of at least 6 months since the prior administration of a meningococcal polysaccharide vaccine and the administration of Neis Vac-C. Meningococcal C conjugate vaccines are interchangeable for those 12 months of age. If an infant has a history of receiving their last dose before 12 months of age, give an additional dose at 12 months of age. Administer concurrently with chemoprophylaxis or as soon as possible. A MCC vaccine is preferred in this situation as it provides longer duration of protection and induction of immunologic memory than does a meningococcal C-containing polysaccharide vaccine and is less expensive than Menactra. See Meningococcal Quadrivalent Conjugate Vaccine (Menactra) for list of medical indications. Medically high risk children < 2 yrs old: give MCC 1st, followed by Menactra after 2nd birthday. Medically high risk children 2 yrs to 10 years of age (inclusive): give Menactra first, followed by MCC vaccine one month later. A grade 6 or 9 student is considered up-to-date for MCC vaccine if they have a dose of MCC vaccine on or after their 10th birthday. The interval between MCC doses is a minimum of 8 weeks. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 31 Meningococcal Quadrivalent Conjugate Vaccine (Menactra) (Groups A, C, Y, W-135) Supplier: sanofi pasteur INDICATIONS (1) Provided free to medically high risk individuals 2 years of age: Functional or anatomic asplenia Congenital immunodeficiency states (e.g., complement, properdin or factor D deficiency, primary antibody deficiencies) Hematopoietic Stem Cell Transplant Solid organ transplant (candidate or recipient) Islet cell transplant (candidate or recipient) Refer to Yukon Immunization Program Manual, Section 5, for more information on specific medical conditions. Note: Children 2 – 10 years of age (inclusive) with a medical indication (as specified above) who have NOT been previously vaccinated with MCC vaccine: Administer Menactra followed by MCC vaccine one month later (2) Close contacts ( 2 years of age) of a case of invasive meningococcal disease (serogroups A, Y, or W-135) that meet the public health criteria for chemoprophylaxis (3) Individuals who have previously been vaccinated with Menomune and for whom there is a need for re-vaccination due to: high risk medical status continuing outbreak exposure, or expected ongoing exposure during travel Administer Menactra as follows: First dose of Menomune (polysaccharide A/C/Y/W-135) received at: 3 – 12 months of age 13 – 23 months of age 2 – 5 years of age 6 years of age Immunize with Menactra when 2 years of age and it is: 6 months since last dose of Menomune 1 year since last dose of Menomune 2 years since last dose of Menomune 5 years since last dose of Menomune (4) Recommended, but NOT provided free to: research, industrial, and clinical laboratory personnel who are routinely exposed to N. meningitidis military recruits travellers for whom meningococcal vaccine is indicated Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 32 Meningococcal Quadrivalent Conjugate Vaccine (Menactra) (Groups A, C, Y, W-135) Supplier: sanofi pasteur DOSE Persons 2 years of age: One dose: 0.5 ml IM REINFORCEMENTS Medically high risk persons: (dose: 0.5 ml IM) First dose received at ≥ 7 years of age: give 5 years after 1st dose First dose received at ages 2 – 6 years: give 3 years after 1st dose Thereafter, re-immunize every 5 years as long as medical condition exists. SPECIAL CONSIDERATIONS If a Grade 6 or 9 child received Menactra when they were 2 – 10 years of age, and have not received a dose of MCC vaccine on or after their 10th birthday, administer MCC vaccine. CONTRAINDICATIONS (1) (2) Known history of Guillain-Barré syndrome (GBS). History of anaphylactic reaction to a previous dose of any meningococcal or diphtheriacontaining vaccine, to any component of Menactra or to latex (if using the vial presentation). The pre-filled syringe presentation does not contain latex. VACCINE COMPONENTS Sodium phosphate, dibasic, anhydrous; sodium phosphate, monobasic. ADVERSE EVENTS Local pain, redness, swelling, headache, malaise, chills, fever. Give vaccine at least 14 days prior to elective splenectomy, or if not possible, 14 or more days post-splenectomy. When there is concern that the patient may not present later for immunization, give vaccine before discharge. The recommended interval between the administration of any meningococcal C conjugate vaccine and Menactra is one month (regardless of which vaccine was given first). Administer vaccine concurrently with chemoprophylaxis or as soon as possible. Any prior history of GBS is a relative contraindication to Menactra vaccine. Immunization may be considered if the benefit of vaccination outweighs the potential risk of recurrence of GBS if the vaccine is given. Discuss with the Vaccine Program Manager/ MOH. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 33 Pneumococcal Conjugate Vaccine (Prevnar®13) Supplier: Wyeth, a Pfizer Company INDICATIONS (1) Healthy infants and children 2 to 59 months of age to start or complete a pneumococcal conjugate vaccine series INITIAL SERIES (1) Healthy children: (2) Children 2 months to 59 months of age who are at high risk of pneumococcal disease due to: Sickle cell disease and other hemoglobinopathies Immunosuppression related to disease [e.g., malignant neoplasm (including leukemia and lymphoma); HIV; multiple myeloma] or therapy (e.g., high dose, systemic steroids or severe rheumatoid arthritis requiring immunosuppressive therapy) Congenital immunodeficiencies involving any part of the immune system, including B-lymphocyte (humoral) immunity, T-lymphocyte (cell-mediated) immunity, complement system (properdin or factor D deficiencies) or phagocytic function. Receipt of hematopoietic stem cell transplant (HSCT) Solid organ or islet cell transplant (candidate or recipient) Chronic heart or lung disease (except asthma, unless management involves ongoing high dose oral corticosteroid therapy) Chronic liver disease including cirrhosis, chronic hepatitis B, chronic hepatitis C Chronic kidney disease Diabetes, cystic fibrosis or chronic CSF leak Chronic neurological conditions that may impair clearance of oral secretions Cochlear implant (candidate or recipient) Anatomic or functional asplenia (children up to and including 16 years of age) (2) Children medically at high risk: (3) All children to 59 months of age and asplenics ≤ 16 years of age who have completed a PVC 7 or PCV 10 vaccine series Dose 1: 2 months of age: 0.5 ml IM Dose 2: 4 months of age: 0.5 ml IM Dose 3: 12 months of age: 0.5 ml IM (at least 8 weeks after second dose). Dose 1: 2 months of age: 0.5 ml IM Dose 2: 4 months of age: 0.5 ml IM Dose 3: 6 months of age: 0.5 ml IM Dose 4: 12 months of age: 0.5 ml IM (at least 8 weeks after third dose) (3) One dose 0.5 ml IM at least 8 weeks after a previous PCV7 or PCV10 dose Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 34 Pneumococcal Conjugate Vaccine (Prevnar®13) Supplier: Wyeth, a Pfizer Company CONTRAINDICATIONS VACCINE COMPONENTS ADVERSE EVENTS History of an anaphylactic reaction to a previous dose of any pneumococcal vaccine, or to any component of Prevnar®13. Diphtheria toxoid, succinic acid, polysorbate 80, aluminum phosphate Redness, swelling, tenderness at injection site; fever, irritability, drowsiness, restless sleep, decreased appetite, vomiting, diarrhea High risk children should receive one dose of pneumococcal polysaccharide vaccine at 2 years of age, and at least 8 weeks after the final dose of pneumococcal conjugate vaccine. Unimmunized asplenics identified at 5-16 years of age require two doses of vaccine, 8 weeks apart. Give vaccine at least 14 days prior to elective splenectomy, or, if not possible 14 days post-splenectomy. If there is concern that the patient may not present later for immunization, give at hospital discharge. Give vaccine before initiation of immunosuppression therapy, and early in the course of HIV infection. If HIV positive contact YCDC, for most recent CD4 counts. A complete series for a child is: three (PVC7 or PCV10) primary doses given at appropriate intervals and a 4th dose given on or after 12 months of age and at least 8 weeks after previous dose, or a delayed or interrupted schedule that has been completed at a later age according to the information in table “Completing a Pneumococcal Conjugate Vaccine Series.” Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 35 Completing a Pneumococcal Conjugate Vaccine Series Age at presentation for immunization History of prior doses of PCV7, PCV10 or PCV13 given 3 to 11 months 12 to 23 months Completion of series requires Booster dose Healthy and High Risk Healthy Infant High Risk Infant 0 doses 2 doses 3 doses 1 dose 1 dose 2 doses 2 doses 0 doses 1 dose 0 doses 2 doses 2 doses No booster dose 1 dose < 12 months 2 doses 2 doses No booster dose 1 dose ≥ 12 months 1 dose 1 dose No booster dose One dose at 12 months of age 2 doses < 12 mos. 1 dose 2 doses No booster dose 1 dose < 12 mos. & 1 dose 1 doses No booster dose 1 dose ≥ 12 mos 24 to 59 months 0 doses 1 dose 1 dose No booster dose Any age- appropriate series incomplete by 24 1 dose 1 dose No booster dose months Complete PCV7 or PCV10 1 doses 1 dose No booster dose series When an infant has received one or two doses of vaccine, and is subsequently diagnosed with a high risk medical condition, use the table to complete the immunizations as “high risk.” When a high risk condition is diagnosed after an infant has completed the 3 dose schedule for healthy children, further immunization will be determined on a case-by-case basis. High risk children should receive one dose of pneumococcal polysaccharide vaccine at 2 years of age, and at least 8 weeks after their final pneumococcal conjugate vaccine dose. When there is a delay in initiating or completing the vaccine series, use the minimum interval of 4 weeks between vaccine doses given in infancy. See Section 3 Immunization Schedules, 3.0 Minimum Intervals between Vaccine Doses. At least 8 weeks after the previous dose. 8 weeks between doses. A complete series is: three (PVC7 or PCV10) primary doses given at appropriate intervals and a 4th dose given on or after 12 months of age and at least 8 weeks after previous dose, or a delayed or interrupted schedule that has been completed at a later age according to the information in this table. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 36 Recommendations for Pneumococcal Immunization With 13-Valent Pneumococcal Conjugate Vaccine (PCV 13) and 23-Valent Pneumococcal Polysaccharide Vaccine (PPV 23) for Children at High Risk of Pneumococcal Disease Age: Previous doses PCV 13 Recommendations: 23 months None PCV 13 as per primary series schedule 24 to 59 months None 2 doses of PCV 13, followed by one dose of PPV 23, 8 weeks after the dose of PCV 13. Once-only revaccination with PPV 23, 3 years after the first dose of PPV 23 2 doses of PCV 13, followed by one dose of PPV 23, 8 weeks after the dose of PCV 13. Once-only revaccination with PPV 23, 3 years after the first dose of PPV 23 One dose of PPV 23 at 24 months of age, Once-only revaccination with PPV 23, 3 years after the first dose of PPV 23 Two doses of PCV 13, 8 weeks apart, and 8 weeks after the administration of PPV 23. Once-only revaccination with PPV 23, 3 years after the first dose of PPV 23 ≤ 2 doses PCV13 before 24 months PCV 13 series completed One dose of PPV 23 For list of children at high-risk for pneumococcal disease, see Pneumococcal Conjugate Vaccine (Prevnar®13) PPV 23 is provided free for high risk children. Children who have completed a PCV13 vaccine series before they are 2 years of age, and who are among the high risk groups for pneumococcal disease, should receive one dose of pneumococcal polysaccharide vaccine at 2 years of age, no sooner than 8 weeks after the last dose of PCV 13. If high risk children 2 years of age received pneumococcal polysaccharide vaccine first, offer pneumococcal conjugate vaccine at least 8 weeks after the polysaccharide vaccine. For list of high-risk conditions for which revaccination with PPV23 is recommended, see Pneumococcal Polysaccharide Vaccine (Pneumo 23). Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 37 Pneumococcal Polysaccharide Vaccine (Pneumovax 23) Supplier: Merck Frosst Recommended and provided free to: INDICATIONS All persons 65 years of age All residents of Extended or Intermediate Care Facilities INITIAL SERIES REINFORCEMENT All persons 2 years of age with: Anatomic or functional asplenia Sickle cell disease Immunosuppression related to disease (e.g., malignant neoplasm (including leukemia and lymphoma); HIV; multiple myeloma) or therapy (e.g., high dose, systemic steroids or severe rheumatoid arthritis requiring immunosuppressive therapy) Congenital immunodeficiency states (e.g., complement, properdin or factor D deficiency) Chronic heart or lung disease Chronic kidney disease Chronic liver disease including cirrhosis, chronic Hepatitis B, Hepatitis C Receipt of hematopoietic stem cell transplant (HSCT) Solid organ or islet cell transplant (candidate or recipient) Diabetes Alcoholism Cystic fibrosis Chronic CSF leak Cochlear implant (candidate or recipient) Homelessness and/or illicit drug use Smokers Adults and children 2 years of age: 1 dose: 0.5 ml SC or IM HSCT Recipients ≥ 2 years of age: 2 doses: 0.5 ml SC or IM 7 months apart (See Section 6, Immunization of special populations) Revaccination is not routinely recommended. A once-only revaccination should be offered to those who have: Anatomic or functional asplenia Sickle cell disease Immunosuppression related to disease (e.g., HIV, lymphoma, Hodgkin’s, multiple myeloma, severe rheumatoid arthritis), or therapy (e.g., high dose, systemic steroids) Congenital immunodeficiency states (as above) Chronic kidney disease Chronic liver disease including cirrhosis, chronic hepatitis B, and chronic hepatitis C For individuals 10 years old at time of initial vaccination: 1 dose of 0.5 ml SC or IM 5 years after the initial immunization. For children 10 years old at time of initial vaccination: 1 dose of 0.5 ml SC or IM 3 years after the initial immunization. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 38 Pneumococcal Polysaccharide Vaccine (Pneumovax 23) Supplier: Merck Frosst CONTRAINDICATIONS VACCINE COMPONENTS PRECAUTIONS History of an anaphylactic reaction to a previous dose of a pneumococcal vaccine or to any component of Pneumovax 23™ vaccine Phenol, monosodium and disodium phosphate Adverse reaction may intensify if revaccination occurs within 2 years Do not administer Pneumovax23 and ZOSTAVAX at the same time due to the possibility of an inferior immune response to ZOSTAVAX. Separate these vaccines by 4 weeks. Hodgkin’s Disease: Do not administer to clients with Hodgkin’s disease less than 10 days prior to or during immunosuppressive therapy. Following intense chemotherapy with or without radiation, the immune response may be depressed for 2 years. During the 2 years following completion of treatment, the antibody response may improve as the interval between treatment and pneumococcal vaccination increases. ADVERSE EVENTS Local: Soreness and erythema; rarely severe arthus reaction Systemic: Occasionally low grade fever Give vaccine at least 14 days before splenectomy, or, if not possible 14 days post-splenectomy. If there is concern that the patient may not present later for immunization, give at hospital discharge. Give vaccine before initiation of immunosuppression therapy, and early in the course of HIV infection. Contact YCDC for most recent CD4 counts prior to immunization. Except asthma, unless management involves ongoing high dose oral corticosteroids Homelessness to be defined by local jurisdiction. Crack cocaine smokers have been shown to be at increased risk of invasive pneumococcal disease. Pneumococcal polysaccharide vaccine can be given simultaneously with influenza, Hib, and meningococcal vaccines, using separate syringes/needles at separate sites. Children who are among the high risk groups for pneumococcal disease and who have completed the PCV vaccine series before they are 2 years of age, should receive one dose of pneumococcal polysaccharide vaccine at 2 years of age, no sooner than 8 weeks after the last dose of PCV. If high risk children 2 years of age received pneumococcal polysaccharide vaccine first, offer pneumococcal conjugate vaccine at least 8 weeks after the polysaccharide vaccine. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 39 Pneumococcal Polysaccharide Vaccine (Pneumo 23) Supplier: sanofi pasteur INDICATIONS Recommended and provided free to: All persons 65 years of age. All residents of Extended or Intermediate Care Facilities INITIAL SERIES REINFORCEMENT All persons 2 years of age with: Anatomic or functional asplenia Sickle cell disease Immunosuppression related to disease [e.g., malignant neoplasm (including leukemia and lymphoma); HIV; multiple myeloma) or therapy (e.g., high dose, systemic steroids or severe rheumatoid arthritis requiring immunosuppressive therapy) Congenital immunodeficiency states (e.g., complement, properdin or factor D deficiency) Chronic heart or lung disease Chronic kidney disease Chronic liver disease including cirrhosis, chronic Hepatitis B, Hepatitis C Receipt of hematopoietic stem cell transplant (HSCT) Solid organ or islet cell transplant (candidate or recipient) Diabetes Alcoholism Cystic fibrosis Chronic CSF leak Cochlear implant (candidate or recipient) Homelessness and/or illicit drug use Smokers Adults and children 2 years of age: 1 dose: 0.5 ml SC or IM HSCT Recipients ≥ 2 years of age: 2 doses: 0.5 ml SC or IM 7 months apart (See Section 6, Immunization of special populations) Revaccination is not routinely recommended. A once-only revaccination should be offered to those who have: Anatomic or functional asplenia Sickle cell disease Immunosuppression related to disease (e.g., HIV, lymphoma, Hodgkin’s, multiple myeloma, severe rheumatoid arthritis), or therapy (e.g., high dose, systemic steroids) Congenital immunodeficiency states (as above) Chronic kidney disease Chronic liver disease including cirrhosis, chronic hepatitis B, and chronic hepatitis C For individuals 10 years old at time of initial vaccination: 1 dose of 0.5 ml SC or IM 5 years after the initial immunization. For children 10 years old at time of initial vaccination: 1 dose of 0.5 ml SC or IM 3 years after the initial immunization. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 40 Pneumococcal Polysaccharide Vaccine (Pneumo 23) Supplier: sanofi pasteur CONTRAINDICATIONS History of an anaphylactic reaction to a previous dose of a pneumococcal vaccine or to any component of Pneumo 23™ vaccine VACCINE Phenol, monosodium and disodium phosphate COMPONENTS PRECAUTIONS Adverse reaction may intensify if revaccination occurs within 2 years Do not administer Pneumo23™ and ZOSTAVAX at the same time due to the possibility of an inferior immune response to ZOSTAVAX. Separate these vaccines by 4 weeks. Hodgkin’s disease: Do not administer to clients with Hodgkin’s disease less than 10 days prior to or during immunosuppressive therapy. Following intense chemotherapy with or without radiation, the immune response may be depressed for 2 years. During the 2 years following completion of treatment, the antibody response may improve as the interval between treatment and pneumococcal vaccination increases. ADVERSE EVENTS Local: Soreness and erythema; rarely severe arthus reaction Systemic: Occasionally low grade fever Give vaccine at least 14 days before elective splenectomy, or, if not possible 14 days post-splenectomy. If there is concern that the patient may not present later for immunization, give at hospital discharge. Give vaccine before initiation of immunosuppression therapy, and early in the course of HIV infection. Contact YCDC for most recent CD4 counts prior to immunization. Except asthma, unless management involves ongoing high dose oral corticosteroid therapy. Homelessness to be defined by local jurisdiction. Crack cocaine smokers have been shown to be at increased risk of invasive pneumococcal disease. Pneumococcal polysaccharide vaccine can be given simultaneously with influenza, Hib, and meningococcal vaccines, using separate syringes/needles at separate sites. Children who are among the high risk groups for pneumococcal disease and who have completed the PCV vaccine series before they are 2 years of age, should receive one dose of pneumococcal polysaccharide vaccine at 2 years of age, no sooner than 8 weeks after the last dose of PCV. If high risk children 2 years of age received pneumococcal polysaccharide vaccine first, offer pneumococcal conjugate vaccine at least 8 weeks after the polysaccharide vaccine. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 41 Polio Vaccine (Inactivated) (Imovax ®Polio) (vero cell origin) Supplier: sanofi pasteur INDICATIONS Provided free to: 1) Infants and children 4 years of age who do not require diphtheria, pertussis, tetanus, or Hib. INITIAL SERIES (1) Infants and children < 4 years of age: Dose 1: 0.5 ml SC Dose 2: 0.5 ml SC give 4 to 8 weeks after dose 1 Dose 3: 0.5 ml SC give 6-12 months after dose 2 Dose 4: 0.5 ml SC at school entry (this dose not necessary if dose 3 was given on or after the 4th birthday) (2) Children 7 years and ≤ 17 years of age who do require polio immunization (2) Individuals 4 years of age: Dose 1: 0.5 ml SC Dose 2: 0.5 ml SC give 4 to 8 weeks after dose 1 Dose 3: 0.5 ml SC give 6-12 months after dose 2 Note: Give 1 dose 0.5 ml SC to children 7 years of age who have not received a polio booster on or after their 4th birthday (3) Adults who have previously received less than a full primary course of IPV or OPV regardless of interval since the last dose, should receive the remaining doses (3) Use schedule (2) as appropriate based on previous doses received. (4) Previously unimmunized children and adult solid organ transplant (SOT) candidates and recipients (4) Use schedule (1) or (2) above as appropriate for age (5) HSCT recipients: Individuals ≥ 7 years of age who are receiving Tdap concurrently (5) Dose 1: 0.5ml SC (12 months after HSCT) Dose 2: 0.5ml SC (2 months after dose 1) Dose 3: 0.5ml SC (12 months after dose 1) Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 42 Polio Vaccine (Inactivated) (Imovax®Polio) (vero cell origin) Supplier: sanofi Pasteur REINFORCEMENTS No additional doses of IPV are recommended for travellers < 18 years of age who have completed an IPV or OPV vaccine series. A single booster dose (10 years after the primary series) is recommended for individuals 18 years of age who are at increased risk of exposure to wild polioviruses and who completed an IPV or OPV series in childhood such as travelers to areas of countries where wild polioviruses are circulating- this is NOT publicly funded and at cost to the client. CONTRAINDICATIONS History of anaphylactic reaction to any polio-containing vaccine, or to any IPV vaccine component. VACCINE COMPONENTS 2-phenoxyethanol, formaldehyde, residual calf serum protein, neomycin, streptomycin, polymyxin B, Medium199 Hanks ADVERSE EVENTS Minor local reactions, fever. Routine polio immunization is not considered necessary for previously unimmunized adults in Canada who do not intend to travel to areas in which polio outbreaks occur except for those in Indication (3) & (4) above. Previously unimmunized travelers who will depart in less than 4 weeks should receive a single dose of IPV. The remaining doses of vaccine should be given later at the recommended intervals. Please contact the medical specialist most familiar with the client’s care and vaccine program manager prior to immunization for this indication. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 43 Rabies Vaccine Pre-exposure [Human Diploid Cell Vaccine (HDCV)] (Inactivated) Imovax Rabies Supplier: sanofi Pasteur INDICATIONS PRE-EXPOSURE PROPHYLAXIS: Recommended but not provided free to the following persons at risk of contact with the rabies virus: High Risk: Rabies research lab workers Rabies biologicals production workers Moderate Risk: Rabies diagnostic lab workers Spelunkers Veterinarians and staff, and animal control workers in rabies epizootic areas Hunters and trappers in high risk areas such as the far north Low Risk: Vets and staff, and animal control and wildlife workers in areas of low rabies disease (enzootic) Vet students and animal health tech students (however, vaccine is provided free to this group) Children and travelers visiting foreign epizootic areas INITIAL SERIES PRE-EXPOSURE PROPHYLAXIS: 1.0ml IM (2.5 IU) at dosage intervals of 0 - 7 - 21 days For infants and children 12 months of age, the site for immunization is the anterolateral thigh. For infants ≥12 months of age and adults, the preferred site is the deltoid muscle. DO NOT GIVE RABIES VACCINE IN THE GLUTEAL REGION. ROUTE While NACI considers the IM route of administration as the gold standard, consideration may be given to using the ID route of administration for pre-exposure immunization provided there is an opportunity to assess the neutralizing antibody level at least 1 month after administration, so that adequate protection can be ensured. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 44 Rabies Vaccine Pre-exposure [Human Diploid Cell Vaccine (HDCV)] (Inactivated) Imovax Rabies Supplier: sanofi Pasteur REINFORCEMENTS As required 1.0 ml IM. An acceptable antibody level is 0.5 IU/ml. High risk: test clients every 6 mos. and boost when level falls below 0.5 IU/ml. Moderate risk: test clients every 2 years and boost when level falls below 0.5 IU/ml. Low risk: testing not required and no routine booster for clients. CONTRAINDICATIONS 1. Persons with an anaphylactic reaction to a previous dose of rabies vaccine, Imovax Rabies, any component of Imovax Rabies, or to latex. 2. Severe allergic or neuroparalytic reactions during the course of a rabies vaccine series pose a serious dilemma. The risk of exposure to rabies must be carefully considered before a decision is made to discontinue rabies vaccine. VACCINE Human albumin, neomycin sulfate, phenol red, and beta COMPONENTS propiolactone. PRECAUTIONS Persons receiving high doses of steroids or immunosuppressive therapy should receive vaccine by the IM route and have a rabies antibody titre upon completion to ensure an adequate response has developed. If titre is inadequate, give one booster dose and retest. Persons taking chloroquine should receive vaccine by the IM route or be vaccinated by the ID route at least 1 month prior to their taking chloroquine. There are insufficient data regarding concurrent use of mefloquine with rabies immunization. ADVERSE EVENTS Fever, nausea, headache, muscle aches, abdominal pain, fatigue, and dizziness. Pain, redness, swelling and itching at injection site. Three cases of neurologic illness resembling Guillain-Barré syndrome (GBS) were reported in the early 1980s; all cases resolved without sequelae within 12 weeks. SPECIAL Imovax Rabies is pink to red in color following reconstitution. Also, it CONSIDERATIONS does not contain any preservative and should be used immediately after reconstitution or discarded. Whenever possible the immunization series should be completed with the same product. However, if this is not feasible, Imovax and RabAvert are interchangeable in terms of indications for use, immunogenicity, efficacy, and safety. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 45 Rabies Vaccine Pre-exposure [Purified Chick Embryo Cell Vaccine] (PCECV) (RabAvert) Supplier: Novartis INDICATIONS PRE-EXPOSURE PROPHYLAXIS: Recommended but not provided free to the following persons at risk of contact with the rabies virus: High Risk: Rabies research lab workers Rabies biologicals production workers Medium Risk: Rabies diagnostic lab workers Spelunkers Veterinarians and staff, and animal control workers in rabies epizootic areas Hunters and trappers in high risk areas such as the far north Low Risk: Vets and staff, and animal control and wildlife workers in areas of low rabies disease (enzootic) Vet students and animal health tech students (however, vaccine is provided free to this group) Children and travelers visiting foreign epizootic areas INITIAL SERIES PRE-EXPOSURE PROPHYLAXIS: ROUTE REINFORCEMENTS 1.0 ml IM (2.5 IU) at dosage intervals of 0 - 7 - 21 days In infants and children 12 months of age, the site for immunization is the anterolateral thigh. For children 12 months of age and adults, the preferred site is the deltoid muscle. DO NOT GIVE RABIES VACCINE IN THE GLUTEAL REGION. NACI considers the IM route of administration as the gold standard, consideration may be given to using the ID route of administration for pre-exposure immunization provided there is an opportunity to assess the neutralizing antibody level at least 1 month after administration, so that adequate protection can be ensured. As required 1.0 ml IM. An acceptable antibody level is 0.5 IU/ml. High risk: test clients every 6 mos. and boost when level falls below 0.5 IU/ml. Moderate risk: test clients every 2 years and boost when level falls below 0.5 IU/ml. Low risk: testing not required and no routine booster for clients. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 46 Rabies Vaccine Pre-exposure [Purified Chick Embryo Cell Vaccine] (PCECV) (RabAvert) Supplier: Novartis Use the longer of the 2 needles supplied (21g x 1.5”) to RECONSTITUTION withdraw the entire contents of the sterile diluent into the syringe. Insert the needle at a 45 angle and slowly inject the entire contents of the diluent into the vaccine vial. Mix gently to avoid foaming. Unscrew the syringe from the needle to eliminate negative pressure. Reinsert the syringe into the needle. Withdraw the total amount of reconstituted vaccine into the syringe. Replace the long needle with the smaller needle (25g x 1”) for IM injection. Persons with a history of anaphylaxis to a previous dose of CONTRAINDICATIONS 1. rabies vaccine, RabAvert, eggs or egg products, or to any component of RabAvert. 2. Severe allergic or neuroparalytic reactions during the course of a rabies vaccine series pose a serious dilemma. The risk of exposure to rabies must be carefully considered before a decision is made to discontinue rabies vaccine. VACCINE Polygeline (processed bovine gelatin stabilizer), human serum COMPONENTS albumin, ovalbumin (egg white albumin), neomycin, chlortetracycline, amphotericin B, potassium glutamate, sodium EDTA. PRECAUTIONS Persons receiving high doses of steroids or immunosuppressive therapy should receive vaccine by the IM route and have a rabies antibody titre upon completion to ensure an adequate response has developed. If titre is inadequate, give one booster dose and retest. Persons taking chloroquine should receive vaccine by the IM route or be vaccinated by the ID route at least 1 month prior to their taking chloroquine. There are insufficient data regarding concurrent use of mefloquine with rabies immunization. ADVERSE EVENTS Fever, nausea, headache, muscle aches, abdominal pain, fatigue, and dizziness. Pain, redness, swelling and itching at injection site. Three cases of neurologic illness resembling Guillain-Barré syndrome (GBS) were reported in the early 1980s; all cases resolved without sequelae within 12 weeks. SPECIAL RabAvert does not contain a preservative and should be used CONSIDERATIONS immediately after reconstitution or discarded. Whenever possible the immunization series should be completed with the same product. However, if this is not feasible, RabAvert and Imovax are interchangeable in terms of indications for use, immunogenicity, efficacy, and safety. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 47 RABIES POST-EXPOSURE PROPHYLAXIS INSTRUCTIONS STEP 1 Was the person exposed i.e. bitten, scratched or in contact with saliva from a possibly rabid animal? Wound Management: The first and immediate action Immediate and thorough washing of the wounds and scratches with soap and water may reduce the risk of rabies and will reduce the risk of bacterial wound infection. Wash and flush the wound and scratches with copious amounts of water under moderate pressure, with a mild soap, for 5 to 10 minutes. As appropriate, follow-up wound care in situations of potential rabies exposure should be undertaken in consultation with a physician: Consideration can be given to disinfecting the wound with either 70% ethanol, tincture of aqueous solution of iodine, or povidone iodine. Decisions on primary versus delayed suturing of animal bites require medical assessment, and depend on multiple factors including type of animal, time since injury, location of wound, presence of crushed tissue or puncture wounds, and underlying medical status of the individual. If RPEP is advised, sutures, if required, should be placed after local infiltration of RabIg. They should be loose and not interfere with free bleeding and drainage. Tetanus toxoid containing vaccine should be administered as required. See Section 8, Biological Products, Tetanus Prophylaxis in Wound Management. Assess risk of rabies - refer to the current edition of the Canadian Immunization Guide for further rabies information. STEP 2 Risk of rabies - CALL YCDC OR MOH FOR DIRECTION The provision of Rabies Post Exposure Prophylaxis (RPEP) must be authorized by the MOH: Monday- Friday (0830-1630) After hours and Weekends: Yukon Communicable Disease Control #4 Hospital Road, Whitehorse, Yukon Y1A 3H8 Dr. Brendan E. Hanley MD CCFP (EM) MPH Chief Medical Officer of Health, Yukon #4 Hospital Road, Whitehorse, Yukon Y1A 3H8 Telephone: Local (867) 667-8323 Within Yukon 1-800-661-0408 Fax: (867) 667-8349 Cell: (867) 332-1160 STEP 3 Complete the Rabies Investigation Form- See following page and Fax to YCDC YCDC 2011 Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 48 Rabies Investigation Form Victim’s Name: YHIS #: Address: DOB: Y______M____D ___ Physician/NP: Gender: Male______Female_____ Bylaw informed on: Date:______________ Time:________ RCMP informed on: Date:______________Time:____ General Information Location of incident: Date of Incident: Y____M____D____ Time of Incident: Biting Provoked: Yes______ No_______ Severity of wound: Site:__________ Number of wounds:_____________ Sutures Required: Yes Any other pertinent details: Wound management description: Other circumstances about incident: No Immunization History of Client Tetanus updated: Yes________ No___________ History of Pre-exposure rabies vaccination: Yes____ No____ Known titre level: Yes____No____ Details: Rabies Immune Globulin advised: Yes____ No____ RIG administered: Yes____No____ If yes: Dose____________ Site________________ Post Exposure Vaccine advised: Yes____ No____ Animal Information Animal species: Bat Cat Dog Other (describe)___________________ unknown Animal type: Household pet – indoor Household pet – outdoor Stray Wild Unknown Animal immunized against rabies? Yes: Y____M____D__ No Unknown Veterinarian: Animal behavior at time of exposure: Animal description: Breed:_______________ Size:______________ Color:_______________ Collar, tags: Yes No Brief Description: Owner’s Name: Telephone: Address: Location of animal: Report Attending Physician/Nurse: Telephone: This Form is be Faxed to YCDC, (867) 667-8349 **Only Animal & Owner information can be released to Bylaw or RCMP unless victim consents. YCDC 2005 Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 49 Release of Biologicals for Rabies Post-Exposure Prophylaxis (RPEP) The MOH must authorize all releases of RPEP How to access RPEP Monday-Friday (0800-1600hrs) The MOH or assigned designate will call the WGH Pharmacy to request the release of the products: WGH Pharmacy (request Rabies Vaccine and RabIg) Phone 867-393-8737. Afterhours, the MOH or assigned designate is to phone WGH Admitting and Discharge – request that the Pharmacist on call be paged Phone: 867-393-8700 Administration Arrangements - Location of Exposed Person Whitehorse: o In Whitehorse, the administration of initial dose of vaccine along with RabIg should occur in the WGH ER or as arranged by YCDC. WGH ER - phone 867-393-8926 o Subsequent doses of vaccine will be arranged through YCDC - Potential sites include: YCDC, Whitehorse Health Centre or WGH ER. Communities: o Old Crow Health Centre has a stock of RPEP (Vaccine and RabIg) o All other communities: arrangements will be made in collaboration with the nurse to have RPEP sent as soon as possible to the community from WGH hospital, where the administration of RPEP will be done by the Primary Health Care or Community Health Nurse at the rural Community Health Centre. Arrangements for administration could also include having the client come into Whitehorse. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 50 Human Rabies Immune Globulin (RabIg) (HYPERRAB™ S/D) Supplier: Talecris Biotherapeutics, Inc. INDICATIONS INITIAL SERIES REINFORCEMENTS RABIES POST-EXPOSURE PROPHYLAXIS (RPEP): As determined by Yukon Medical Officer of Health. Rabies Vaccine is given in conjunction with Rablg. Rabies vaccine and Rablg must be administered with separate needles and syringes at separate anatomical sites If a rabies vaccine series has been started or completed elsewhere and it was not given in accordance with the current WHO standards, or if the vaccine was a nerve tissue vaccine (Semple vaccine), administer Rablg (on day 0) in conjunction with another full course of rabies vaccine. Note: Do not give Rablg if clients were previously immunized in accordance with the WHO standards or have documented seroconversion (i.e. level ≥ 0.5 IU/ml) within the past 2 years RABIES POST-EXPOSURE PROPHYLAXIS: The recommended dosage for children and adults is the same: 20 IU/kg of body weight. Because of interference with active antibody production, do not exceed recommended dose. The does of Rablg is calculated as: [20 IU/kg x weight in kg] = ml 150 IU/ml Rablg is supplied in 2 ml vials, each 1.0 ml = 150 IU Infiltrate as much Rablg as possible deep into and around the wound(s) in order to neutralize the virus. When more than one wound site exists, each site should be infiltrated with a portion of the Rablg, using a separate syringe and needle for each infiltration. If there are extensive wounds, where the calculated dose of Rablg (by weight) is not adequate in volume to infiltrate all wounds, dilute the Rablg 2-3 fold in normal saline to create an adequate volume to infiltrate all wounds. When there is no wound site, the preferred site for the administration of Rablg is the ventrogluteal area, which may be used in those > 7 months of age. However, the vastus lateralis is most often used in infants and children up to 5 years of age. None Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 51 Human Rabies Immune Globulin (RabIg) (HYPERRAB™ S/D) Supplier: Talecris Biotherapeutics, Inc. CONTRAINDICATIONS 1. PRECAUTIONS ADVERSE EVENTS There are no contraindications to Rablg given for post-exposure purposes. If client has a history of anaphylactic reaction following receipt of any human Ig product, to any of the components of RabIg (glycine) or to latex, administer RabIg in an emergency room setting. Human Ig products are among the safest blood-derived products available. The method of preparation includes one or more steps that exclude or inactivate hepatitis B, C and HIV; therefore the risk of transmission is extremely low. However, it is possible, that unknown infectious agents may be present in such products. Regarding RabIg and the administration of live vaccines (MMR & Varicella) see CIG Guildines for the Interval Between Administration of Immune Globulin Preparations or Blood Products and MMR or Vaccines. Persons with IgA deficiency have the potential for developing antibodies to IgA and could have an anaphylactic reaction to subsequent blood products that contain IgA. Administer RabIg in an emergency room setting. Fever, headache, malaise, rash, chills. Local tenderness, soreness or stiffness at the injection site SPECIAL RabIg contains no preservatives. CONSIDERATIONS Vials are single dose use: discard unused contents Since vaccine induced antibodies begin to appear within one week, there is no value in administering Rablg more than 8 days after initiation of vaccine. Provide a written record to a client who receives any immune globulin product. When notification of an exposure is delayed, RPEP may be started as late as 6 or more months after an exposure. The deltoid should not be used for Rablg administration. Both deltoid sites should be reserved for administration of rabies vaccine. See CIG, for maxiumum volume to be administered per site according to age. See Release of Biologicals for Rabies Post-Exposure Prophylaxis (RPEP), for information on how obtain Rablg in you community. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 52 Rabies Vaccine Post-exposure [Human Diploid Cell Vaccine (HDCV)] (Inactivated) ImovaxRabies Supplier: sanofi pasteur INDICATIONS Post-Exposure Prophylaxis: As determined by Yukon Medical Officer of Health. If a rabies vaccine series has been started or completed elsewhere and it was not given in accordance with current WHO standards, or if the vaccine was a nerve tissue vaccine (Semple vaccine), administer another full course of rabies vaccine. Administer RabIg on day 0 of vaccine series. SERIES Unimmunized: (1) 1.0 ml IM on days 0 – 3 – 7 – 14 - 28 Day 0: 1.0 ml IM as soon as possible after exposure PLUS RabIg Days 3, 7, 14 and 28: 1.0 ml IM Previously immunized: (1) Completion of a course of pre/post-exposure prophylaxis with rabies vaccine 2 years previously that used a WHO approved rabies vaccine and schedule OR (2) Completion of a course of rabies pre/post exposure prophylaxis that used a non-WHO approved vaccine or schedule OR completion of a course of rabies pre/post exposure prophylaxis > 2 years previously that used a WHO approved vaccine and schedule AND expedited rabies antibody titre result ≥ 0.5 IU/ml Give rabies vaccine on day 0 (as soon as possible after exposure) & on day 3: 1.0 ml IM (DO NOT GIVE RabIg) CONTRAINDICATIONS (3) Completion of a course of rabies pre/post exposure prophylaxis that used a non-WHO approved vaccine or schedule OR completion of a course of rabies pre/post exposure prophylaxis > 2 years previously that used a WHO approved vaccine and schedule AND expedited rabies antibody titre result < 0.5IU/ml Give rabies vaccine on day 0 (as soon as possible after exposure) & on days 3, 7, 14, 28: 1.0 ml IM (DO NOT GIVE RabIg) 1. There are NO contraindications to rabies vaccine given for postexposure purposes. 2. DO NOT GIVE RABIES VACCINE IN THE GLUTEAL REGION. 3. Rabies vaccine and RabIg must NOT be administered in the same anatomical site. Use separate needles and syringes for each product. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 53 Rabies Vaccine Post-exposure [Human Diploid Cell Vaccine (HDCV)] (Inactivated) Imovax Rabies Supplier: sanofi pasteur VACCINE Human albumin, neomycin sulfate, phenol red and beta propiolactone. COMPONENTS PRECAUTIONS Administer vaccine in an emergency room setting if history of an anaphylactic reaction to a previous dose of rabies vaccine, Imovax Rabies, to any of the components of ImovaxRabies or to latex. Persons receiving high doses of steroids or immunosuppressive therapy should receive vaccine by the IM route and have a rabies antibody titre upon completion to ensure an adequate response has developed. If titre is inadequate, give one booster dose and retest. There are insufficient data regarding concurrent use of mefloquine with rabies immunization. ADVERSE EVENTS Fever, nausea, headache, muscle aches, abdominal pain, fatigue, and dizziness. Pain, redness, swelling and itching at injection site. Three cases of neurologic illness resembling Guillain-Barré syndrome (GBS) were reported in the early 1980s; all cases resolved without sequelae within 12 weeks. SPECIAL Imovax Rabies is pink to red in color following reconstitution. Also, it CONSIDERATIONS does not contain any preservative and should be used immediately after reconstitution or discarded. Whenever possible the immunization series should be completed with the same product. However, if this is not feasible, ImovaxRabies and RabAvert are interchangeable in terms of indications for use, immunogenicity, efficacy, and safety. In infants and children 12months of age, the site for immunization is the anterolateral thigh. For children ≥12 months of age and adults, the preferred site is the deltoid. Have serum sample taken and administer first dose of rabies vaccine while awaiting results. It is very likely the rabies antibody titre result will not be available by day 7: administer 3rd dose of rabies vaccine on day 7. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 54 Rho (D) Immune Globulin (RhIg) (WinRho ) Supplier: Cangana Corporation INDICATIONS 1) Recommended for the prevention of Rh immunization of Rho (D) negative woman at risk of developing Rh antibodies, to prevent haemolytic disease of the newborn. The reduction of Rh alloimmunization is from 13% to 1 to 2 %. DOSE Dose 1: 300 μg IM 28 weeks of gestation Dose 2: 300 μg IM within 72hours after delivery CONTRAINDICATIONS Do not give Ig intravenously Rho (D) positives individuals including babies Rho (D) negative women who are Rh immunized as evidenced by standard manual Rh antibody screening tests. Individuals with a history of anaphylactic or other severe systemic reaction to immune globulins. PRECAUTIONS Human Ig products are amongst the safest blood-derived products available. As the method of preparation includes one or more steps that exclude or inactivate hepatitis B, C and HIV, the risk of transmission is considered to be extremely low. However, it is possible that unknown infectious agents may be present in such products. Persons with severe thrombocytopenia or coagulation disorders that contraindicate IM injections should not be give IM Ig unless the benefits outweigh the risks. Give Ig with caution (i.e., in a setting capable of managing anaphylaxis) if the client has a history of anaphylactic reaction following receipt of any human Ig product, or history of anayphylactic reaction to glycine or to latex (assess risks versus benefits). Persons with IgA deficiency have the potential for developing antibodies to IgA and could have an anaphylactic reaction to subsequent administration of blood products that contain IgA. Therefore, Ig should only be given to such persons if the expected benefits outweigh the risks. Ig contains no preservatives. Vials are single use. Once entered, discard any unused contents. The preferred site for the administration of Ig is the ventrogluteal area. Should either be given at the same time as MMR or the MMR should be deferred 3 months post injection of the Rho (D) Immune Globulin. If administration of Ig is necessary less than 14 days after MMR or varicella vaccine, repeat vaccine as per recommended intervals as in CIG. ADVERSE EVENTS Local: pain and injection site tenderness A Physician’s order by prescription is always required. Order through Whitehorse General Hospital Lab on a stores order form, (and phone Lab and give the patient's name, estimated date of confinement, whether the request is for the 28 week or post-delivery injection, and the name of attending physician) See product monograph for further information. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 55 Tetanus-Diphtheria (Td) Adsorbed Supplier: sanofi pasteur INDICATIONS (1) Booster dose for persons 7 years of age if both diphtheria and tetanus are required, but Pertussis is not required. (2) Adults 18 years of age who have not been immunized, including immigrants with unknown immunization status (1) 0.5 ml IM every 10 years DOSE (2) REINFORCEMENTS CONTRAINDICATIONS VACCINE COMPONENTS PRECAUTIONS Administer one dose of Tdap followed by two doses of Td: 1st Td: 0.5 ml IM 1 month after Tdap 2nd Td: 0.5 ml IM 6 – 12 months after 1st Td dose Every 10 years Adults who have not received one dose of acellular pertussis (Tdap) should receive a single dose of Tdap instead of Td (see Tetanus-Diphtheria-acellular Pertussis) 1. History of anaphylactic reaction to a previous dose of any tetanus or diphtheria-containing vaccine, or to any Td vaccine component. 2. When a contraindication exists to tetanus toxoid and a client sustains a major or unclean wound TIG should be given (see Tetanus Immune Globulin (TIg) (HYPERTET S/D). 3. History of Guillain-Barré syndrome (GBS) occurring within 8 weeks of receipt of a tetanus – containing vaccine. Aluminum phosphate and formaldehyde. Persons who experience a major local reaction or high fever following a dose of Td should not be given another dose for at least 10 years. When travel to a developing country is planned 5 years after the last Td dose, it may be prudent to offer an early booster, since some developing countries may not be able to guarantee the safe administration of a booster dose if required. ADVERSE EVENTS Discomfort, pain, swelling, redness at injection site. SPECIAL For wound prophylaxis, Td and Tetanus Immune Globulin should CONSIDERATIONS be administered using separate syringes and different sites. Tetanus toxoid should not be given routinely to clients who have received a booster dose in the previous 5 years. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 56 Tetanus-Diphtheria-acellular Pertussis (Tdap) (ADACEL) Supplier: sanofi pasteur INDICATIONS (1) Reinforcing dose for all grade 9 students INITIAL SERIES (1) & (11) One dose: 0.5 ml IM (2) Children and adolescents from 7 years to 17 years of age (inclusive) who have not received any doses of tetanus or diphtheria (2) (3) & (4) Dose 1: 0.5 ml IM Dose 2: 0.5 ml IM 1 month later Dose 3: 0.5 ml IM 6 to 12 months after dose 2 (5) Children and adolescents from 7 years to 17 years of age (inclusive) whose 3 dose primary series of tetanus or diphtheria or pertussis vaccine is incomplete (5) (6) Children and adolescents from 7 years to 17 years of age (inclusive) who have received 3 – 4 doses of tetanus/diphtheria/pertussis-containing vaccine at < 7 years of age, but have not received the school entry booster (7) Adults 18 years of age who have not been immunized, including immigrants with unknown immunization status (6) One to two doses of Tdap (0.5 ml IM) at time of presentation to complete the primary series of 3 doses, followed by another dose of 0.5 ml IM in grade 9 One dose of Tdap (0.5 ml IM) at time of presentation, followed by another dose of 0.5 ml IM in grade 9 (8) HSCT recipients ≥ 7 to <18 years of age (8) (3) Children and adolescents from 7 years to 17 years of age (inclusive) who have not received any doses of pertussis vaccine (4) Immigrants from 7 years to 17 years of age (inclusive) with unknown immunization status (9) HSCT recipients ≥ 18 years of age (7) One dose of Tdap (0.5ml IM) followed by two doses of Td Three doses of Tdap (0.5ml IM) at 0, 1, and 12 months. (9)& (10) One dose of Tdap (0.5ml IM) followed by two doses of Td/IPV (10) Solid organ transplant candidates or recipients ≥ 7 years of age who have not been previously immunized. (11) All adults who have not received a dose of acellular pertussis ≥ 14 years of age. REINFORCEMENTS Publicly funded as per indication (11). Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 57 Tetanus-Diphtheria-acellular Pertussis (Tdap) (ADACEL) Supplier: sanofi pasteur CONTRAINDICATIONS 1. History of an anaphylactic reaction to a previous dose of any tetanus, diphtheria, or pertussis-containing vaccine or to any component of ADACEL vaccine. 2. History of Guillain-Barré syndrome (GBS) occurring within 8 weeks of receipt of a tetanus – containing vaccine. 3. < 4 years of age and ≥ 65 years of age. Aluminum phosphate, 2-phenoxyethanol. VACCINE COMPONENTS ADVERSE EVENTS Minor local: redness, tenderness, swelling, induration, pain Minor systemic: headache, decreased energy, generalized bodyache, nausea, diarrhea, fever, sore or swollen joints There should be a minimum of 2 years since receipt of a previous booster dose of a tetanus/diphtheria –containing vaccine. The exception to this, for Grade 9 Tdap program only, is a minimum interval of 6 months. This recommendation is based on unpublished data. In studies related to the interval between the grade 9 Tdap booster and a previous dose of a tetanus-containing vaccine, there were a small number of students with an interval of ~ 6 months since receipt of a tetanus-containing vaccine. Following administration of the grade 9 tetanus booster they did not experience any marked local reactions. For clients ≥ 65 years of age, see BOOSTRIX. Give Tdap to high school students who missed their grade 9 booster. For example, if the student had received one dose of a tetanus/diphtheria/pertussis – containing vaccine, give two doses of ADACEL, separated by a period of 6 - 12 months. If the student had received two doses of a tetanus/diphtheria/pertussis – containing vaccine, give one dose of ADACEL The high school Tdap booster given at age 14-16 years is considered a dose of acellular pertussis in adulthood. At this time, an additional dose of acellular pertussis is not recommended. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 58 Tetanus-Diphtheria-acellular Pertussis (Tdap) (BOOSTRIX) Supplier: GlaxoSmithKline INDICATIONS Provided free: (1) Reinforcing dose for all grade 9 students INITIAL SERIES (1) & (11) One dose: 0.5 ml IM (2) Children and adolescents from 7 years to 17 years of age (inclusive) who have not received any doses of tetanus or diphtheria (2) (3) & (4) Dose 1: 0.5 ml IM Dose 2: 0.5 ml IM 1 month later Dose 3: 0.5 ml IM 6 to 12 months after dose 2 (5) Children and adolescents from 7 years to 17 years of age (inclusive) whose 3 dose primary series of tetanus or diphtheria or pertussis vaccine is incomplete (5) (6) Children and adolescents from 7 years to 17 years of age (inclusive) who have received 3 – 4 doses of tetanus/diphtheria/pertussis-containing vaccine at < 7 years of age, but have not received the school entry booster (7) Adults 18 years of age who have not been immunized, including immigrants with unknown immunization status (6) One to two doses of Tdap (0.5 ml IM) at time of presentation to complete the primary series of 3 doses, followed by another dose of 0.5 ml IM in grade 9 One dose of Tdap (0.5 ml IM) at time of presentation, followed by another dose of 0.5 ml IM in grade 9 (8) HSCT recipients ≥ 7 to <18 years of age (8) (3) Children and adolescents from 7 years to 17 years of age (inclusive) who have not received any doses of pertussis vaccine (4) Immigrants from 7 years to 17 years of age (inclusive) with unknown immunization status (9) HSCT recipients ≥ 18 years of age (7) One dose of Tdap (0.5ml IM) followed by two doses of Td Three doses of Tdap (0.5ml IM) at 0, 1, and 12 months. (9)& (10) One dose of Tdap (0.5ml IM) followed by two doses of Td/IPV (10) Solid organ transplant candidates or recipients ≥ 7 years of age who have not been previously immunized. (11) All adults who have not previously received a dose of acellular pertussis after 14years. REINFORCEMENTS Publicly funded as per indication (11) Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 59 Tetanus-Diphtheria-acellular Pertussis (Tdap) (BOOSTRIX) Supplier: GlaxoSmithKline CONTRAINDICATIONS 1. History of an anaphylactic reaction to a previous dose of any tetanus, diphtheria, or pertussis-containing vaccine or to any component of BOOSTRIX vaccine. 2. History of Guillain-Barré syndrome (GBS) occurring within 8 weeks of receipt of a tetanus – containing vaccine. 3. < 4 years of age. Aluminum phosphate, 2-phenoxyethanol. VACCINE COMPONENTS ADVERSE EVENTS Minor local: redness, tenderness, swelling, induration, pain Minor systemic: headache, decreased energy, generalized bodyache, nausea, diarrhea, fever, sore or swollen joints There should be a minimum of 2 years since receipt of a previous booster dose of a tetanus/diphtheria –containing vaccine. The exception to this, for Grade 9 Tdap program only, is a minimum interval of 6 months. This recommendation is based on unpublished data. In studies related to the interval between the grade 9 Tdap booster and a previous dose of a tetanus-containing vaccine, there were a small number of students with an interval of ~ 6 months since receipt of a tetanus-containing vaccine. Following administration of the grade 9 tetanus booster they did not experience any marked local reactions. Approved for use in those ≤ 4 years of age with no upper age limit. Give Tdap to high school students who missed their grade 9 booster. For example, if the student had received one dose of a tetanus/diphtheria/pertussis – containing vaccine, give two doses of Tdap separated by a period of 6 - 12 months. If the student had received two doses of a tetanus/diphtheria/pertussis – containing vaccine, give one dose of Tdap. The high school Tdap booster given at age 14-16 years is considered a dose of acellular pertussis in adulthood. At this time, an additional dose of acellular pertussis is not recommended. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 60 Tetanus Immune Globulin (TIg) (HYPERTETS/D) Supplier: Talecris Biotherapeutics, Inc. INDICATIONS 1) TIg is indicated for prophylaxis against tetanus following a major or unclean wound in individuals whose immunization history is incomplete or uncertain (See Tetanus Prophylaxis in Wound Management.) 2) TIg is indicated when a contraindication to a tetanus toxoidcontaining vaccine exists and an individual sustains a major or unclean wound. 3) DOSE TIg is indicated in individuals known to have a significant immune deficiency state (i.e. HIV) regardless of their immunization history, following any major or unclean wound. Give 250 units IM (entire syringe) to adults and children who require TIg. TIg is supplied in a 250 unit single dose pre-filled disposable syringe. REINFORCEMENTS The syringe fill volume for each lot is adjusted to ensure a potency of 250 IU/syringe. The actual fill volume for HyperTet syringes typically ranges between 0.75 ml and 1.3 ml. The needle on the pre-filled syringe is fixed and cannot be changed. None if Td vaccine is given concurrently with TIg. CONTRAINDICATIONS TIg should not be given intravenously. Provide a written record to a client who receives any immune globulin product. See CIG, for maximum volume to be administered per site according to age If a contraindication to a tetanus toxoid-containing vaccine exists or a client refuses a tetanus toxoid-containing vaccine, and a client sustains a major or unclean wound, consider offering a 2nd dose of TIg 30 days post the 1st dose of TIg. Tetanus Immune Globulin does not interfere with the development of active immunity from a tetanus toxoid-containing vaccine Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 61 Tetanus Immune Globulin (TIg) (HYPERTETS/D) Supplier: Talecris Biotherapeutics, Inc. PRECAUTIONS ADVERSE EVENTS Human Ig products are among the safest blood-derived products available. The method of preparation includes one or more steps that exclude or inactivate hepatitis B, C and HIV; therefore the risk of transmission is considered to be extremely low. However, it is possible that unknown infectious agents may be present in such products. Regarding TIg and administration of live vaccines (MMR & Varicella) see Immune Globulin Preparations or Blood: Timing Intervals For Vaccines Containing Live Measles, Mumps, Rubella, or Varicella Virus in CIG. Give TIg with caution (i.e., in a setting capable of managing anaphylaxis) if the client has a history of anaphylactic reaction following receipt of any human Ig product, or a history of anaphylactic reaction to latex (assess risks versus benefits). Persons with IgA deficiency have the potential for developing antibodies to IgA and could have an anaphylactic reaction to subsequent administration of blood products that contain IgA. Therefore, TIg should only be given to such persons if the expected benefits outweigh the risks. In clients who have severe thrombocytopenia or any coagulation disorder that would contraindicate IM injections, TIg should be given only if the expected benefits outweigh the risks. TIg must be given at separate anatomic sites from a tetanus toxoid-containing vaccine. The preferred site for the administration of TIg is the ventrogluteal area, which may be used in those > 7 months of age. However, the vastus lateralis is most often used in infants and children up to 5 years of age. Local tenderness, erythema and stiffness of local muscles that may persist for several hours. Systemic reactions include mild fever or malaise. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 62 Tetanus Prophylaxis in Wound Management History of Tetanus Immunization Clean, minor wounds All other wounds Tetanus ToxoidContaining Vaccine TIg Tetanus ToxoidContaining Vaccine TIg Uncertain or 3 doses Yes No Yes Yes Primary immunization complete No No No No Such as, but not limited to, wounds contaminated with dirt, feces, soil, and saliva; puncture wounds; tearing away of body parts or structures; and wounds resulting from missiles, crushing, burns and frostbite. May have been given as Td, Tdap, or Td/IPV. Monovalent tetanus toxoid is not available in Canada. For additional information on the primary immunization schedule, refer to the Td, Tdap, or Td/IPV vaccine pages. Wound management for children 7 years of age would be based on specific spacing and doses required as per INFANRIX hexa, PEDIACEL® and QUADRACEL vaccine pages. Yes, if > 10 years since last tetnus containing booster. Yes, if > 5 years since last tetnus containing booster. No, unless individuals are known to have a significant humoral immune deficiency state (e.g., HIV, agammaglobulinemia), since immune response to tetanus toxoid may be suboptimal. In adults, if a tetanus toxoid containing vaccine is required it may be administered as Tdap (if not previously administered ≥ 14 years of age) or as Td. See individual product information in this section. Note: Tetanus-diphtheria (Td) / Tetanus-diphtheria- acellular pertussis (Tdap) vaccine and Tetanus Immune Globulin (TIg) should be administered using separate syringes and different sites. If a contraindication exists for a tetanus toxoid-containing vaccine, TIg would be given where tetanus immunization is required. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 63 Tuberculin Skin Test (Mantoux) Tubersol Supplier: sanofi pasteur INDICATIONS Recommended and provided free to everyone. Target groups include: Suspected cases of TB Individuals referred for medical diagnostic reason Contacts of a known case of TB HIV positive individuals and persons at significant risk for HIV infection International travelers who will be residing in countries where TB is endemic and travelers returning from prolonged visits to endemic areas. Establishment of a baseline prior to possible exposure to TB (as a requirement for an educational program, volunteer position or employment) Self-referral INITIAL SERIES PPD 5 TU 0.1 ml ID in anterior forearm (flexor or dorsal surface) between the wrist and the elbow For contact tracing, if the initial skin test is negative, a second test should be given 8 – 12 weeks after the last date of contact REINFORCEMENTS 2 – STEP TESTING: A second test, done 7 - 21 days after the first test, may be required in certain situations see Yukon Health & Social Services Tuberculosis Manual, YCDC. A small percentage of persons will only react after a second test or will react to a greater degree (so called “boosting” effect). Intradermally ROUTE CONTRAINDICATIONS 1. History or documentation of previous positive reaction to tuberculin testing (because of the severity of the reaction at the test site: vesiculation, ulceration or necrosis) 2. Documentation of previous active TB 3. History of an anaphylactic reaction to a previous test using Tubersol or a similar product, or to any component of Tubersol 4. Individual with severe burns or eczema 5. Individuals with severe viral infections or live-virus vaccination in the past 4 weeks (to avoid negative reactions). Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 64 Typhoid Vaccine (Salmonella Typhi Vi Capsular Polysaccharide)(Typherix) Supplier: GlaxoSmithKline INDICATIONS Routine vaccination is not recommended in Canada. Recommended but not provided free to: Travelers 2 years of age to countries where typhoid fever is endemic or epidemic, or where sanitary conditions may be doubtful and where travellers may be exposed to potentially contaminated food and water. INITIAL SERIES Adults and children 2 years of age: One dose: 0.5 ml IM REINFORCEMENTS Adults and children 2 years old every 2 years as required: 0.5 ml IM History of anaphylactic reaction to a previous dose of any typhoid vaccine or to any component of Typherix or to latex. Sodium phosphate dihydrate, disodium phosphate dihydrate, phenol. CONTRAINDICATIONS VACCINE COMPONENTS PRECAUTIONS ADVERSE EVENTS An adequate immune response may not be achieved in clients receiving immunosuppressive treatment or in clients who are immunocompromised. Soreness, redness and swelling at the injection site Headache and fever. The typhoid vaccines Vivotil, Typhim Vi, Typherix, and ViVAXIM are interchangeable for children or adults at any scheduled dose, using the age-specific dosage for the particular product. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 65 Varicella Vaccine (live attenuated viral) Varivax III and Varilrix Supplier: Varivax III, Merck Frosst Canada; Varilrix, GlaxoSmithKline INDICATIONS Recommended and provided free to: (1) All infants at 12 months of age (including infants with a history of varicella disease occurring at < 12 months of age). (2) Susceptible children, adolescents, and adults at opportune health encounters. With special attention to: children and adults on low dose steroid therapy (< 2 mg prednisone/kg daily to a maximum of 20 mg/day for < 2 weeks), and those taking inhaled or topical steroids household contacts of immunocompromised individuals health care workers AND susceptible individuals at high risk of severe varicella disease: Individuals with cystic fibrosis Individuals on chronic salicylate therapy (those 18 years of age must be able to discontinue it for 6 weeks post vaccination) (3) Susceptible Immunocompromised CHILDREN and ADULTS. Before vaccination of the following clients, receive approval from the appropriate physician (i.e., either the primary care provider most familiar with the client’s current medical status or a medical specialist). Refer to Yukon Immunization Program, Section 5, subsection 1.4 Immunization With Live Vaccines, for those who are immunosupressed; use Varilrix® ONLY: with chronic kidney disease (and not receiving immunosuppressant therapy) undergoing hemo or peritoneal dialysis (and not receiving immunosuppressant therapy) Asplenia Candidates for solid organ transplant, isolated immunodeficiency diseases, asymptomatic HIV, HSCT, acute lymphocytic leukemia in remission and those cured of a malignant disease and the end of immunosuppressive treatment. Discuss immunization with Vaccine Program Manger, and medical specialist prior to immunization. Also see Yukon Immunization Manual, Section 5 Immunization of Special Populations. ≥ 1 month after completion of high doses (>2mg/kg or >20 mg/day) oral corticosteroid therapy more than 14 days duration Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 66 Varicella Vaccine (live attenuated viral) INITIAL SERIES 12 months to 12 years of age: One dose: 0.5 ml SC 13 years of age: Two doses - dose 1: 0.5 ml SC dose 2: 0.5 ml SC 4 weeks later REINFORCEMENTS Not indicated at this time CONTRAINDICATIONS 1. 2. 3. 4. 5. 6. 7. 8. 9. Children/adults with: T-cell or combined T-and B-cell immunodeficiencies (SCID) Total lymphocyte count < 1.2 x 109/L or presenting other evidence of lack of cellular immune competence Advanced HIV (AIDS) Malignant solid tumours Conditions requiring chronic immunosuppressive therapy Acute lymphocytic leukemia (ALL) not in remission Acute myelogenous leukemia (AML) Adult solid organ transplant recipients Children or adults with chronic inflammatory diseases (e.g., inflammatory bowel disease, collagen-vascular disease) receiving significant immunosuppressive therapy. However, they may be immunized at least 6 to 12 weeks after they have completed or temporarily stopped the immunosuppressive therapy. History of an anaphylactic reaction to a previous dose of any varicella vaccine, or to any component of VarivaxIII or Varilrix®. Pregnancy. Women of childbearing age should avoid pregnancy for 1 month following vaccination. Active untreated TB. For high risk/immunocompromised clients only - concurrent administration with another live vaccine. Separate the administration of varicella vaccine and another live vaccine by at least 4 weeks (expert opinion, BC Children’s Hospital, based on concerns about adverse events with concurrent administration). Recent administration of an immunoglobulin preparation or blood product. See CIG, P 53-56, 2006 Family history of congenital immunodeficiency. See Yukon Immunization Program Section 4, Contraindications and Routine Precautions for Immunization. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 67 Varicella Vaccine (live attenuated viral) VACCINE COMPONENTS VarivaxIII: Hydrolyzed beef gelatin, neomycin, monosodium L-glutamate, sucrose, sodium phosphate dibasic, urea, potassium phosphate monobasic, potassium chloride, fetal bovine serum. Varilrix®: Amino acids, human albumin, lactose, neomycin sulphate, and polyalcohols. PRECAUTIONS Those 18 years of age should avoid taking salicylates for 6 weeks following immunization. Do TB skin testing on the same day as varicella immunization or delay TB skin testing for 4 weeks. Varicella immunization for immunocompetent clients should be given on the same day or delayed until 4 weeks after administration of any other live vaccine. ADVERSE EVENTS Generally mild and include injection site reactions, non-injection site rash, and low-grade fever. SPECIAL CONSIDERATIONS Administer vaccine immediately after reconstitution. Discard if not used within 30 minutes of reconstitution. Assess varicella susceptibility before immunization. A varicella susceptible individual is defined as an individual: with a history of varicella disease at <12 months of age with no history of varicella disease at > 12 months of age, no history of herpes zoster, and no history of varicella immunization. For persons 13 years of age with negative or unknown history of prior varicella infection, have serology done for VZV IgG (use BCCDC Laboratory Services requisition). Whenever possible, vaccine should be given at least 14 days prior to elective splenectomy, or if not possible, 14 or more days post-splenectomy. However, vaccine is indicated whenever an individual with functional or anatomic asplenia is identified. Use same brand of varicella vaccine for dose 2. There is no data on the interchangeability of Varivax III and Varilrix. Varicella-susceptible women who receive RhIg post-partum should be given the first dose of varicella vaccine 2 months after delivery. Also at 2 months after delivery, prior rubellasusceptible women should be tested for rubella immunity as they should have been immunized against rubella immediately post-partum. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 68 Varicella Zoster Vaccine (live attenuated viral) (ZOSTAVAX) Supplier: Merck Frosst INDICATIONS Recommended but not currently provided free to: Individuals > 60 years of age INITIAL SERIES One dose: entire contents of vial (approximately 0.65ml) SC REINFORCEMENTS Not indicated at this time. CONTRAINDICATIONS 1. History of anaphylactic reaction to a previous dose of varicella zoster vaccine, or to any component of ZOSTAVAX 2. Immune suppression related to disease[e.g., malignant neoplasm (including leukemia and lymphoma), HIV/AIDS] 3. Immune suppression related to therapy (e.g., high dose systemic corticosteroid therapy, chemotherapy, radiation therapy, certain medications for treatment of rheumatoid arthritis) 4. Congenital immunodeficiency 5. Active untreated tuberculosis 6. Pregnancy and breastfeeding PRECAUTIONS 1. Delay immunization of individuals with severe acute illness until recovery. 2. Varicella Zoster immunization should be given on the same day or delayed until 4 weeks after administration of any other live vaccine. 3. Do TB skin testing on the same day as VZV immunization, or delay TB skin testing for > 4 weeks. 4. ZOSTAVAX has not been studied in individuals who have previously experienced an episode of herpes zoster. While these individuals are at risk for further episodes, the efficacy of ZOSTAVAX in this population is not known. 5. ZOSTAVAXand a pneumococcal polysaccharide 23 valent vaccine should not be given at the same time due to the possibility of an inferior immune response to ZOSTAVAX. Separate these vaccines by 4 weeks. 6. Antiviral medications active against VZV (i.e., acyclovir, famciclovir, valacyclovir taken less than 2 days before or within 14 days after immunization may decrease vaccine effectiveness. 7. Delay ZOSTAVAX™ administration for 3 months after a dose of intravenous immunoglobulin (IVIG). Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 69 Varicella Zoster Vaccine (live attenuated viral) (ZOSTAVAX) Supplier: Merck Frosst VACCINE COMPONENTS Neomycin, hydrolyzed porcine gelatin, sucrose, sodium chloride, monosodium L-glutamate monohydrate, sodium phosphate dibasic, potassium phosphate monobasic, potassium chloride, MRC-5 cells, bovine calf serum. ADVERSE EVENTS Local: Mild to moderate pain, redness, swelling, itchiness, varicella-like rash at the injection site Systemic: Headache, fever SPECIAL CONSIDERATIONS 1. ZOSTAVAX™ should be stored FROZEN at an average temperature of -15°C or colder until it is reconstituted for injection. Do not freeze reconstituted vaccine. The diluent should be stored separately at room temperature (20 to 25°C) or in the refrigerator (2 to 8°C). Do not store the diluent in a freezer. 2. It is recommended that the vaccine be administered immediately after reconstitution to minimize loss of potency. Discard reconstituted vaccine if it is not used within 30 minutes. ZOSTAVAX™ is indicated for the prevention of herpes zoster in patients with prior chickenpox infection. There is no known safety risk associated with vaccination of healthy individuals who are varicella-susceptible. If individual is known to be serologically varicella susceptible, they should be immunized with 2 doses of varicella vaccine. The efficacy of protection has not been assessed beyond 4 years and it is not known whether booster doses of vaccine are beneficial. Consult client’s medical specialist regarding the appropriateness of zoster vaccine administration to persons whose immune status may be suppressed as the result of disease or therapy (e.g., chronic renal disease/dialysis; solid organ transplant candidate; hyposplenia/asplenia; ≥ 3 months after being cured of a malignant disease and the end of immunosuppressive treatment). ZOSTAVAX™ and trivalent influenza vaccine may be given at the same time or be separated by any interval. Co-administration of ZOSTAVAX™ with other vaccines has not been studied. Individuals who inadvertently receive systemic anti-viral therapy active against VZV within 2 days before and 14 days after ZOSTAVAX™ immunization may benefit from a second dose of vaccine 42 days later and after discontinuing antiviral therapy. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 70 Yellow Fever (YF-VAX) Supplier: sanofi pasteur INDICATIONS Recommended but not provided free to: (1) International travelers ≥ 9 months & ≤ 60 years of age, visiting yellow fever endemic areas Single dose of 0.5 mL sc REINFORCEMENTS Booster every 10 years CONTRAINDICATIONS 1. 2. 3. 4. 5. PRECAUSIONS VACCINE COMPONENTS ≤ 9 months of age ≥ 60 years of age Severe egg allergy Immunosuppressed persons due to disease or therapy History of thymoma or other thymus disorders 6. Post vaccine encephalitis, Guillain-Barre syndrome, autoimmune central or peripheral nervous system involvement. 7. History of anaphylactic reaction to Yellow Fever vaccine or any of it’s components including latex 8. Pregnancy individuals with the following conditions should be considered as relative contraindications and thorough assessment should be undertaken including risks and benefits - Breastfeeding women No adjuvants, no preservatives Contains residual egg proteins, sorbitol, gelatin, sodium chloride ADVERSE EVENTS 5 - 10 days after injection possible: 2%-5% mild headaches, myalgia, fevers, or other minor symptoms for 5 – 10 days. Severe reactions following yellow fever vaccine increases with age. Risk between 60-69 years old is 4/100,000 doses and ≥ 70 years old is 7.5/100,000 doses. These serious reactions include YEL-AVD, Multi organ failure and YELAND. Community Nursing Yukon Immunization Program Section 8 – Biological Products 2011 March Page 71 Yellow Fever (YF-VAX) Supplier: sanofi pasteur Only administered at Whitehorse Health Centre. See discussion in Yukon Immunization Manual, Section 5 Immunization of Special Populations. Requires completion of the International Certificate of Vaccination or Prophylaxis for Yellow Fever, or medical exemption for Yellow Fever Immunization required regions. Freeze dried product, requiring reconstitution Give Varicella or M.M.R. on the same day or 4 weeks apart from vaccine administration. PPD ≥ 6 weeks after live vaccine. Live vaccines can be given any time after PPD. No time restriction on oral cholera and oral typhoid YEL-AVD: Yellow Fever Associated Viscerotropic disease & YEL-AND: Yellow Fever Associated Neurotropic disease. Administration of Yellow Fever Vaccine to breastfeeding females is a relative precaution due to a theoretical risk of transmission of the 17D vaccine virus from nursing mother to infant. If travel to an endemic area is required the vaccination with YF vaccine is a lesser risk than that of acquiring the disease. Under extreme risk situations and after careful examination of associated risks & benefits, immunization under these situations may be recommended with consultation of a physician and/or MOH.